Abstract
Purpose
Positive airway pressure (PAP) is the standard and most effective treatment for obstructive sleep apnea (OSA). It provides a continuous stream of air under positive pressure through the nose, mouth, or both, which prevents collapse of the upper airway. This allows the patient to breathe freely during sleep. The success of PAP therapy depends largely on the selection of the proper interface (mask). The choice and application of the interface in patients with OSA is a great challenge that greatly affects the long-term compliance to PAP therapy.
Methods
This article discusses the different types of masks that can be used in patients with OSA, including the differences between nasal, oro-nasal, and total face masks, breathing during wakefulness and sleep, and the impact of interface type on upper airway patency and mask fitting. We also discuss the steps to be considered in choosing the proper interface and potential problems that may arise during long-term use.
Results and conclusion
Current evidence suggests that the nasal mask is better tolerated, requires lower pressure to eliminate obstructive respiratory events, and is associated with a better sleep quality and better PAP therapy compliance. Nevertheless, the best mask is the one that patient will wear.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Positive airway pressure (PAP) continues to be the most effective treatment for obstructive sleep apnea (OSA) [1]. Studies have shown that PAP can effectively reduce upper airway obstruction leading to an improvement of daytime sleepiness and sleep quality [2]. Moreover, observational studies have shown a reduction in the risk of cardiovascular events in patients with OSA treated with PAP compared to those who are untreated [3]. However, despite the advancement in PAP technology and the wide variety of mask choices in the market, the success of PAP therapy depends on patients’ cooperation and staff expertise. Lack of patient acceptance and inadequate adherence remain the major causes of treatment failure. Nevertheless, patients’ acceptance of PAP therapy depends largely on the selection of the proper interface.
Review method
The literature search began on the August 1, 2016 with key word searches of “sleep apnea,” “CPAP,” “positive airway pressure,” “interface,” “mask,” and “nasal pillows” using PubMed, Google Scholar, and Medline. The reference lists of identified articles were also searched for any additional sources. Publications were then filtered based on whether or not they reported original findings, provided background information, or contained relevant theoretical speculation of the effect of different interfaces on the areas addressed in this review. Most of the studies that investigated the interface used in patients receiving PAP have small sample sizes.
This article discusses the different types of masks that can be used in patients with OSA, breathing during wakefulness and sleep, and the impact of interface type on upper airway patency and mask fitting. We also discuss the steps to be considered in choosing the proper interface and potential problems that may arise during long-term use.
Types of interfaces for PAP
The availability of several types of interface makes the choice of the appropriate interface for patients with OSA a great challenge. Choosing the right mask for patients with OSA involves patient preference, and finding the right size and fit of the mask. There are five available types of masks that can be used to deliver PAP therapy in a sleep laboratory setting:
-
1.
Nasal masks. This type of mask covers the nose only while resting on the upper lip, sides of the nose and on the nasal bridge.
-
2.
Oro-nasal (full-face) masks. This type of mask covers the nose and mouth while resting on the chin, sides of the nose and mouth, and on the nasal bridge.
-
3.
Nasal pillows. This type of mask rests on the inside rim of the nostrils. They are a good option for people who find nasal or oro-nasal mask too intrusive and who have skin breakdown on nasal bridge.
-
4.
Oral masks. This type of mask fits in the mouth between the teeth and lips. It also has a tongue guide to prevent obstruction of the passage of air by the tongue. This type is not common in practice. Major limitations of this type of mask include upper airway dryness and rain-out associated with heated humidification [4].
-
5.
Total face masks. This type of mask covers the entire face. It is a comfortable alternative for patients who may not be able to obtain a good seal with other masks such as nasal masks, nasal pillows, and full-face masks, and is preferably indicated for those with facial deformities and those suffering from skin breakdown around the facial area.
Masks are made of a variety of materials, but the commonly used material is silicone; some manufacturers produce gel masks as well. The advantage of gel masks is that they adapt to the contours of the face.
The main two modes of PAP therapy used in patients with OSA are continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BPAP). For all modes of PAP therapy, a good fit interface is much needed, and this greatly contributes to the adherence of patients to therapy.
Breathing during wakefulness and sleep
Human beings are obligate nose breathers during wakefulness. During sleep, we also breathe mainly through the nose, and nasal breathing is not affected by sleep stage or body position in normal subjects [5]. In patients with OSA and snoring, a multilevel anatomic obstruction is often present. As the nose is the first anatomical boundary of the upper airway, nasal obstruction may contribute to sleep disordered breathing (SDB). A number of pathophysiological mechanisms can potentially explain the role of nasal pathology in SDB. These include the Starling resistor model, an unstable oral airway, the nasal ventilatory reflex, and the role of nitric oxide (NO) [6].
To understand the concept of treating OSA with nasal CPAP, we need to understand the Starling resistor model. The Starling resistor model consists of a tube passing through a sealed box [7]. The tube consists of two rigid segments with a collapsible segment interposed in between, within the box. In humans, the rigid tube is represented by the nose and trachea, and the collapsible segment is the muscular pharynx. As long as pressure inside the pharynx (Pin) is greater than the surrounding tissue pressure (Pout) (composed of pharyngeal muscles and pharyngeal and submucosal fat, mucosal edema), the pharynx will not collapse [8]. The pressure at which complete collapse of the pharynx occurs is called pharyngeal critical closing pressure, at which Pin falls below Pout. The fundamental concept of treating OSA with nasal CPAP is that nasal CPAP increases the pressure inside the pharynx above the pharyngeal critical closing pressure and thereby keeps the pharynx open (Fig. 1).
The Starling resistor model consists of a tube passing through a sealed box. The tube consists of two rigid segments with a collapsible segment interposed in between, within the box. In humans, the rigid tube is represented by the nose and trachea and the collapsible segment is the muscular pharynx. As long as pressure inside the pharynx (Pin) is greater than the pressure outside when the surrounding tissue pressure (Pout), the pharynx does not collapse
However, the correlation between the degree of nasal obstruction and the severity of SDB is not linear [6]. The presence of nasal obstruction either due to anatomical factors, inflammatory diseases, or nasal valve incompetence, may lead to mouth breathing during daytime or mouth opening at night due to increased nasal resistance [9]. Upper airway dynamics differ when we breathe through the nose than when we breathe through the mouth. Namely, upper airway resistance and propensity to develop OSA is higher when breathing through the mouth compared to breathing through the nose [10].
Mouth opening is common in patients with OSA during sleep, especially during NREM sleep, while the muscle atonia accompanied by REM sleep decreases mouth opening [11]. Mouth opening leads to decreased distance between the hyoid bone and mandible, which leads to shortening of genioglossus muscle fibers and puts them on an unfavorable position on the length-tension curve, which diminishes the upper airway dilator muscle tone [12]. This mouth opening in patients with OSA at night should not be confused with daytime mouth breathing due to nasal obstruction; these are distinct [13]. For instance, mouth opening at night may happen without any nasal obstruction and in the absence of daytime mouth breathing. During airway collapse, there is an increase in negative intrathoracic pressure, which pulls the jawbone down due to thoracic traction. This is known as the tracheal tug, which leads to mouth opening and an increased breathing effort [14].
The mask of choice for patients with OSA with nighttime mouth opening is not necessarily the oro-nasal mask; rather, nasal CPAP may be optimal, as it has been shown to decrease mouth opening episodes as well as the amplitude of mouth opening movements in patients with OSA [15]. Similarly, Ruhle et al. [16] demonstrated reduced mouth opening and a decrease in the number of oral breaths with nasal CPAP. Keeping this in mind will prevent over prescription of oro-nasal masks in patients with OSA with nighttime mouth opening; as there are differences in patient tolerance and CPAP pressures needed between nasal masks and oro-nasal masks.
Mask type and upper airway obstruction
As patients with OSA have an element of upper airway obstruction during sleep, it is important to discuss the effect of different routes of interfaces on upper airway patency. Several studies have assessed the impact of different interfaces on the success of treatment in patients with OSA in this context. We will now review studies that have assessed the effect of each type of interface on upper airway dynamics.
Upper airway resistance and propensity to develop OSA is higher when breathing occurs through the mouth as compared to breathing through the nose. Mouth opening is associated with a significant reduction in the retropalatal and retroglossal cross-sectional areas in awake subjects, as well as a reduction in the positive pharyngeal critical closing pressure during natural sleep [17].
While nasal CPAP enhances the Starling resistor model by increasing the pressure inside the pharynx above the pharyngeal critical closing pressure and thereby keeping the pharynx open, the oro-nasal mask violates the Starling resistor model as pressure applied simultaneously through the mouth and nose may lead to a collapse of the upper airway [18]. Figure 2 illustrates the effects of mask type on upper airway collapse.
This illustration demonstrates the relationship between the Starling resistor concept and mask type. There are two rigid segments (nose and trachea) with a collapsible segment interposed in between (pharynx). Level I, the nose (upstream); level II, the pharynx (collapsible segment); and level III, the trachea (downstream). a Upper airway obstruction during inhalation due to negative airway pressure. b The use of PAP through a nasal mask enhances the Starling resistor model by increasing the pressure inside the pharynx above the pharyngeal critical closing pressure and thereby keeping the pharynx open. c The use of PAP through an oro-nasal mask violates the Starling resistor model as pressure applied simultaneously through the mouth and nose may lead to displacement of the tongue and soft palate posteriorly and obstruction of the upper airway
In one study, the upper airway was investigated in 18 patients with severe OSA and treated with nasal CPAP [19]. When the CPAP flow route was shifted from the nasal to the oro-nasal or oral route, there was a significant and progressive reduction in the distance between epiglottis and tongue base, and the retroglossal area, respectively. This demonstrated that patients showed upper airway obstruction during oro-nasal CPAP, despite predominantly breathing through the nose preceding the obstructive event. The authors speculated that positive pressure applied through the mouth pushed the tongue posteriorly, despite undetectable flow. Moreover, the authors proposed that oro-nasal CPAP applies equal positive pressure in both nasopharyngeal and oropharyngeal compartments, which eliminates the pressure gradient, and hence allows gravity to displace the soft palate and tongue backwards, resulting in upper airway obstruction. Similar results have been reported by Smith et al., who showed that oro-nasal CPAP was unable to open the upper airway, even with a CPAP pressure above the pharyngeal critical closing pressure that was obtained when the nasal mask was applied [20]. Body position has also been shown to influence the effectiveness of PAP therapy via oro-nasal masks. For example, the interaction between the supine position and the oro-nasal interface results in posterior tongue displacement and airway obstruction [21].
Figure 3 shows two histograms of the same patient during CPAP titration while on the nasal mask and the oro-nasal mask. The pressure needed to eliminate obstructive respiratory events and desaturation was lower during nasal mask use compared to oro-nasal mask use (9 cm H2O vs 13 cm H2O, respectively). Sleep efficiency, slow wave sleep, and REM sleep were greater during nasal mask titration.
Two histograms of the same patient during CPAP titration while on the nasal mask and oro-nasal mask. The pressure needed to eliminate obstructive respiratory events and desaturation was lower with the nasal mask compared to the oro-nasal mask (9 cm H2O vs 13 cm H2O, respectively). Sleep efficiency, slow wave sleep, and REM sleep were greater during nasal mask titration
Nasal pillow masks versus nasal masks
Three studies in the literature have made a direct comparison between nasal masks and nasal pillow masks. A six-week randomized crossover study involving 39 patients with OSA concluded that the nasal pillow mask is well tolerated and an effective way of delivering therapy in patients that require CPAP ≤14 cm H2O [22]. This study also reported that the use of nasal pillow mask was associated with less adverse effects and better perceived sleep quality in the first 3 weeks of CPAP treatment. Another study found that nasal pillow masks are as effective as nasal masks at CPAP pressure ≥12 cm H2O, and can be considered to treat patients with OSA that require high PAP [23]. The authors also found no difference between the two masks in subjective ratings of comfort, seal, red marks, and side effects such as jetting and nose and mouth dryness. Finally, in a 4-week randomized crossover study, 21 patients with OSA were assigned to a nasal pillow mask and a standard nasal mask [24]. The study showed that the Epworth Sleepiness Scale (ESS) and quality of life improved equally with both interfaces; however, nasal pillow masks exerted less pressure on the face of most subjects, resulting in a greater perception of comfort. Nevertheless, there was no clear preference of either interface at the end of the study. The authors therefore concluded that patients should be assessed individually for the use of nasal pillow masks [24]. Side effects such as nasal dryness, nosebleeds, and headaches were more common with nasal pillow use compared to nasal mask use [24].
Nasal masks versus oro-nasal masks
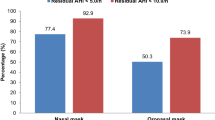
Studies comparing the nasal mask, oro-nasal mask, and nasal pillow mask in patients with moderate and severe OSA have shown that higher CPAP pressures were required by the oro-nasal mask compared to the nasal mask. CPAP pressure was not significantly different between nasal masks and nasal pillow masks. Leaks were significantly higher with oro-nasal mask compared to nasal pillows, but leaks were not significantly different between oro-nasal and nasal mask [25]. A follow-up study showed that changing from a nasal to an oro-nasal mask without changing CPAP pressure settings resulted in a higher residual AHI [26]. Another study concurred with the above findings, and showed that CPAP pressure is higher with the oro-nasal mask compared to the nasal mask or nasal pillow mask [27]. Moreover, the oro-nasal mask had a negative influence on the adherence to CPAP therapy [27], which confirmed results of an earlier study that showed higher CPAP adherence with the nasal mask compared to the oro-nasal mask [28]. Furthermore, normalized respiratory disturbance index, decreased arousal index, and increased slow wave and REM sleep have been shown in patients with OSA who switched from an oro-nasal to a nasal mask [29]. One of the proposed reasons for poor performance of the oro-nasal mask compared to the nasal mask is the backward protrusion of the chin and tongue by the oro-nasal mask [30]. The second reason for the poor performance of the oro-nasal mask may be the simultaneous application of pressure to the oropharynx and nasopharynx, which may not generate a pressure gradient. Gravity may further displace the tongue and soft palate backward causing upper airway obstruction [19]. Together, these studies suggest that the nasal mask should be the first choice, even if the patient experiences nighttime mouth opening [29].
Oral masks versus nasal masks
A limited number of studies with small number of patients have evaluated oral masks in patients with OSA. A study conducted with 7 patients with OSA reported there to be a similar pressure flow relationship between oral and nasal masks, meaning that CPAP delivered through oral route can keep the upper airway patent [31]. Another study reported there to be no differences in CPAP pressure and subjective CPAP compliance between oral masks and nasal or oro-nasal masks [4]. Similarly Anderson et al. [32] and Khanna et al. [33] reported there to be no difference in short-term compliance to CPAP treatment between oral and nasal masks. However, oral mask users suffered more from dry mouth and rain out [31]. Other common side effects of oral masks include dental pain, orthodontic problems, nasal leaks, initial hypersalivation, and Aerophagia [4, 31–33]. Although this preliminary data suggest that oral masks are effective in treating OSA, these masks are not commonly used in practice.
Chinstrap
Some patients complain of mouth leak while on nasal masks. Chin strap has been used in such cases. A retrospective analysis of 124 patients showed that a chinstrap in combination with nasal CPAP had a positive effect on leak and adherence to CPAP therapy [34]. Another study that aimed to determine whether a chinstrap is an effective alternative to CPAP in patients with OSA revealed that a chinstrap alone is not effective [35]. Currently, no good data are available to support the beneficial effects of chin strap on mouth leak and PAP tolerance. Nevertheless, chin strap may be tried in patients on nasal masks who complain of mouth leak.
Type of mask and effect on adherence to PAP therapy
A few studies have been conducted to assess the impact of the type of mask used on adherence to PAP therapy in patients with OSA. In a large-scale study of patients with OSA (n = 2311) assessed the impact of mask type on CPAP adherence. A multivariate analysis revealed that non-adherence to CPAP therapy was associated with the use of oro-nasal masks (OR = 2.0; 95%CI = 1.6; 2.5) [27]. Moreover, side effects such as ocular irritation, mouth dryness, choking sensation, and psychological inconvenience were more common with oro-nasal mask use compared to nasal mask use. In a randomized trial that included 20 patients with OSA, CPAP adherence was greater with nasal masks use than with oro-nasal masks, and the overall comfort was better with nasal masks [28]. Another randomized crossover 4-week study compared nasal pillow masks with nasal masks in 21 patients with OSA [24]. The authors found no differences between nasal pillow masks and nasal masks with regard to CPAP adherence. In a third randomized crossover study with 39 patients with OSA, minutes of use per night did not differ in nasal pillow mask users compared to nasal mask users [22]. Combined, these studies seem to show that nasal masks and nasal pillow masks are associated with a better adherence to PAP therapy than oro-nasal masks.
Fitting the mask
In terms of mask fit, mask comfort, and mask satisfaction, patients generally prefer nasal masks to oro-nasal masks. Correct mask fitting is essential for the success of PAP therapy. Therefore, most masks come with a fitting gauge to assure the choice of the correct size mask to improve acceptance and avoid complications. If a significant leak is detected or the patient does not tolerate the mask, the interface should be changed to avoid PAP failure. However, when a different mask is used, trigger sensitivity, pressurization level, and compatibility with the circuitry must be checked [36]. Once the patient is stable and mouth leaks are not present, nasal masks can be tried, as these are less claustrophobic and have a lower risk of skin problems. Straps should not be over tightened as this can cause pressure ulcers. In general, when the headgear is fixed, it should be possible to permit two fingers beneath it (the two-finger rule) [37].
A PAP trial can be helpful in determining which interface is suitable and preferred by the patient who is about to undergo a sleep study. In this procedure, patients are given an introduction and education on what is PAP and how it works. Patients then try several types of interface and choose the one that is most comfortable. The choice of interface is also influenced by the shape of the patient’s face, mouth/nose breathing pattern, patient preference, and experience of the staff. This procedure helps to reduce anxiety of patients, which leads to a better acceptance during PAP titration and hence a better long-term compliance with PAP therapy. Figure 4 shows a proposed algorithm for the choice of interface during PAP titration in patients with OSA.
Summary
The best mask is the one that patient will wear. It is important to let the patient try different types of masks and to choose the most comfortable, and avoid switching from one type of interface to another as this may lead to variability in the effective pressure needed to eliminate respiratory events. Aside from patient preference, current evidence suggests that the nasal mask is better tolerated, requires lower pressure to eliminate obstructive respiratory events, and is associated with a better sleep quality and better PAP therapy compliance. Therefore, nasal masks or nasal pillow masks should be the first choice. Oro-nasal masks may be tried if the nasal mask is not tolerated, or mouth leak is persistent even with the use of a chinstrap. If all have been tried and are still ineffective, total face masks may be tried.
References
Sullivan CE, Issa FG, Berthon-Jones M, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1(8225):862–865
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Journal of clinical sleep medicine : JCSM: official publication of the American Academy of Sleep Medicine 5(3):263–276
Kakkar RK, Berry RB (2007) Positive airway pressure treatment for obstructive sleep apnea. Chest 132(3):1057–1072
Beecroft J, Zanon S, Lukic D, Hanly P (2003) Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest 124(6):2200–2208
Gleeson K, Zwillich CW, Braier K, White DP (1986) Breathing route during sleep. Am Rev Respir Dis 134(1):115–120
Georgalas C (2011) The role of the nose in snoring and obstructive sleep apnoea: an update. Eur Arch Otorhinolaryngol 268(9):1365–1373
Schwartz AR, Smith PL, Wise RA, Gold AR, Permutt S (1985) Induction of upper airway occlusion in sleeping individuals with subatmospheric nasal pressure. J Appl Physiol 64(2):535–542
Ayappa I, Rapoport DM (2003) The upper airway in sleep: physiology of the pharynx. Sleep Med Rev 7(1):9–33
Pevernagie DA, De Meyer MM, Claeys S (2005) Sleep, breathing and the nose. Sleep Med Rev 9(6):437–451
Fitzpatrick MF, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS (2003) Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J 22(5):827–832
Miyamoto K, Ozbek MM, Lowe AA, Sjoholm TT, Love LL, Fleetham JA, Ryan CF (1999) Mandibular posture during sleep in patients with obstructive sleep apnoea. Arch Oral Biol 44(8):657–664
Meurice JC, Marc I, Carrier G, Series F (1996) Effects of mouth opening on upper airway collapsibility in normal sleeping subjects. Am J Respir Crit Care Med 153(1):255–259
Fitzpatrick MF, Driver HS, Chatha N, Voduc N, Girard AM (1985) Partitioning of inhaled ventilation between the nasal and oral routes during sleep in normal subjects. J Appl Physiol 94(3):883–890
Van de Graaff WB (1988) Thoracic influence on upper airway patency. J Appl Physiol (1985) 65(5):2124–2131
Bachour A, Maasilta P (2004) Mouth breathing compromises adherence to nasal continuous positive airway pressure therapy. Chest 126(4):1248–1254
Ruhle KH, Nilius G (2008) Mouth breathing in obstructive sleep apnea prior to and during nasal continuous positive airway pressure. Respiration; international review of thoracic diseases 76(1):40–45
Jefferson Y (2010) Mouth breathing: adverse effects on facial growth, health, academics, and behavior. Gen Dent 58(1):18–25 quiz 26-17, 79-80
Andrade RG, Piccin VS, Nascimento JA, Viana FM, Genta PR, Lorenzi-Filho G (2014) Impact of the type of mask on the effectiveness of and adherence to continuous positive airway pressure treatment for obstructive sleep apnea. Jornal brasileiro de pneumologia: publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia 40(6):658–668
Andrade RG, Madeiro F, Piccin VS, Moriya HT, Schorr F, Sardinha PS, Gregorio GM, Genta PR, Lorenzi-Filho G (2016) Impact of acute changes in CPAP flow route in sleep apnea treatment. Chest
Smith PL, Wise RA, Gold AR, Schwartz AR, Permutt S (1985) Upper airway pressure-flow relationships in obstructive sleep apnea. J Appl Physiol 64(2):789–795
Nascimento JA, de Santana CT, Moriya HT, Fernandes PH, de Andrade RG, Genta PR, Lorenzi-Filho G, Nakagawa NK (2016) Body position may influence oronasal CPAP effectiveness to treat OSA. J Clin Sleep Med 12(3):447–448
Massie CA, Hart RW (2003) Clinical outcomes related to interface type in patients with obstructive sleep apnea/hypopnea syndrome who are using continuous positive airway pressure. Chest 123(4):1112–1118
Zhu X, Wimms AJ, Benjafield AV (2013) Assessment of the performance of nasal pillows at high CPAP pressures. J Clin Sleep Med 9(9):873–877
Ryan S, Garvey JF, Swan V, Behan R, McNicholas WT (2011) Nasal pillows as an alternative interface in patients with obstructive sleep apnoea syndrome initiating continuous positive airway pressure therapy. J Sleep Res 20(2):367–373
Ebben MR, Oyegbile T, Pollak CP (2012) The efficacy of three different mask styles on a PAP titration night. Sleep Med 13(6):645–649
Ebben MR, Narizhnaya M, Segal AZ, Barone D, Krieger AC (2014) A randomised controlled trial on the effect of mask choice on residual respiratory events with continuous positive airway pressure treatment. Sleep Med 15(6):619–624
Borel JC, Tamisier R, Dias-Domingos S, Sapene M, Martin F, Stach B, Grillet Y, Muir JF, Levy P, Series F, Pepin JL, Scientific Council of The Sleep Registry of the French Federation of (2013) Type of mask may impact on continuous positive airway pressure adherence in apneic patients. PLoS One 8(5):e64382
Mortimore IL, Whittle AT, Douglas NJ (1998) Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax 53(4):290–292
Westhoff M, Litterst P (2015) Obstructive sleep apnoea and non-restorative sleep induced by the interface. Sleep & breathing = Schlaf & Atmung 19(4):1317–1325
Schorr F, Genta PR, Gregorio MG, Danzi-Soares NJ, Lorenzi-Filho G (2012) Continuous positive airway pressure delivered by oronasal mask may not be effective for obstructive sleep apnoea. Eur Respir J 40(2):503–505
Smith PL, O’Donnell CP, Allan L, Schwartz AR (2003) A physiologic comparison of nasal and oral positive airway pressure. Chest 123(3):689–694
Anderson FE, Kingshott RN, Taylor DR, Jones DR, Kline LR, Whyte KF (2003) A randomized crossover efficacy trial of oral CPAP (Oracle) compared with nasal CPAP in the management of obstructive sleep apnea. Sleep 26(6):721–726
Khanna R, Kline LR (2003) A prospective 8 week trial of nasal interfaces vs. a novel oral interface (Oracle) for treatment of obstructive sleep apnea hypopnea syndrome. Sleep Med 4(4):333–338
Knowles SR, O’Brien DT, Zhang S, Devara A, Rowley JA (2014) Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med 10(4):377–383
Bhat S, Gushway-Henry N, Polos PG, DeBari VA, Riar S, Gupta D, Lysenko L, Patel D, Pi J, Chokroverty S (2014) The efficacy of a chinstrap in treating sleep disordered breathing and snoring. J Clin Sleep Med 10(8):887–892
Brill A-K (2014) How to avoid interface problems in acute noninvasive ventilation. Breathe 10:231–242
Meduri GU, Abou-Shala N, Fox RC, Jones CB, Leeper KV, Wunderink RG (1991) Noninvasive face mask mechanical ventilation in patients with acute hypercapnic respiratory failure. Chest 100(2):445–454
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by a grant from the National Plan for Science and Technology Program by the King Saud University Project in Saudi Arabia. The sponsor had no role in the design or conduct of this research.
Conflict of interest
TS is an employee of Philips/Respironics. He declares that he has no proprietary or financial interests that could be construed or considered to be a potential conflict of interest that might have influenced the views expressed in this manuscript. All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Rights and permissions
About this article
Cite this article
BaHammam, A.S., Singh, T., George, S. et al. Choosing the right interface for positive airway pressure therapy in patients with obstructive sleep apnea. Sleep Breath 21, 569–575 (2017). https://doi.org/10.1007/s11325-017-1490-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1490-9