Abstract
Purpose: Obstructive sleep apnea (OSA) is a chronic condition characterized by airway obstructive events with important neurocognitive and cardiovascular complications, leading to a compromised quality of life. Continuous positive airway pressure (CPAP) is the gold standard therapeutic intervention for this disorder. The success of CPAP therapy depends largely on the selection of the proper interface (mask). Finding the correct interface for each patient can be a great challenge that greatly affects the long-term compliance to therapy.
Methods: To elaborate this work, the author proceeded to a systematic review of common database focusing mainly on works published between 2017 and 2019. The purpose was to assemble scientific knowledge, background information, or contained relevant theoretical speculation about the role of different interfaces in CPAP treatment efficacy, adherence, side effects, comfort, and sleep quality in patients with OSA.
Conclusions: Interface selection is a key factor to CPAP compliance and should be based on individual patient preference and tolerance. Patient should participate in decision-making as the best mask is the one that he will wear. Unless patients have significant nasal problems, CPAP therapy is better tolerated and more effective if initially commenced with nasal mask.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Obstructive sleep apnea (OSA) is a chronic disorder caused by repeated upper-airway collapse during sleep resulting in recurrent nocturnal wake-ups, fragmented sleep, increased sympathetic nervous system activity with associated increased cardiovascular risk [1], and great impact in daily life including excessive daytime somnolence, reduced quality of life and increased risk of motor vehicle, as well as incident heart failure and stroke [2,3,4,5]. Given that only a few attempts have been made to screen the general population its real prevalence remains unknown. Last time it was revised was around 34% in men aged 30–70 years and 17% in women aged 30–70 years [1]. Continuous positive airway pressure (CPAP) is considered the gold-standard therapy for OSA and remains the most effective treatment [3, 5, 6]. CPAP can effectively reduce sleep-disordered breathing events, improve objective and subjective sleepiness, and enhance quality of life [2]. CPAP therapy in patients with OSA is also associated with a significant reduction in the cardiovascular risk [6]. Despite huge technology progress and the wide variety of masks available in the market, as the success of this treatment depends on the prolonged use of the CPAP, it is essential to have a good adherence and commitment with the treatment. The lack of patient acceptance and inadequate adherence remain the major causes of treatment failure. One of the most important factors contributing to patient’s acceptance of CPAP therapy is the selection of the proper interface. This fact makes it extremely important to find a mask with which the patient feels comfortable, which makes good sealing and associated with few side effects [2, 6].
There are three main groups of CPAP interfaces to deliver pressure to the patient: nasal, oral, and oronasal, although oral masks have not found widespread acceptance and are rarely used [3]. Many interface models have been released in the market these last years; however, it lacks guidelines and scientific knowledge to support decision-making. Moreover, there is a growing concern that oronasal interface may compromise CPAP effectiveness to treat OSA [7, 8]. A prior systematic review comparing CPAP interfaces has been published; however, because of limited available data at that time, the results were not clear [9].
The aim of this work was to perform a systematic review to better understand the role of interface in CPAP treatment efficacy, adherence, side effects, comfort, and sleep quality in patients with OSA.
2 Methodology
The literature search began on February 2019 and consisted of a systematic review of common database, mainly PubMed and Medline. The keywords used in this search were “sleep apnea,” “CPAP adherence,” “interface and CPAP,” “nasal mask,” and “oronasal mask.” The criteria followed for publication inclusion were based on publication date (between 2017 and 2019, mainly), whether, or not, they reported original findings, scientific knowledge, and background information or contained relevant theoretical speculation about the role of different interfaces on the areas addressed in this review. The reference lists of identified articles were also searched for any additional sources.
3 Interface Characteristics
As mentioned before, CPAP is the first-line treatment for OSA treatment. The importance of selection of the right mask for each patient is also more than established as a determinante factor in the compliance and efficacy of the treatment. The availability of several types of interface and the lack of studies supporting and guiding the decision-making process make the choice of the appropriate interface for patients with OSA a great challenge.
There are available a vast number of interfaces in the market, each one with its features. They can be arranged into six main categories of masks used to deliver CPAP therapy (Table 19.1) [6, 10]:
Human beings are obligate nose breathers during wakefulness. During sleep, humans also breathe mainly through the nose. Besides, in normal subjects, nasal breathing is not affected neither by sleep stage nor by body position [6, 11].
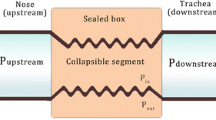
In patients with OSA and snoring, a multilevel anatomic obstruction is often present. Nasal obstruction may contribute to sleep disordered breathing (SDB) as it’s the first anatomical boundary of the upper airway. One of the pathophysiological mechanisms that can potentially explain the role of nasal pathology in SDB is the Starling resistor model. Through this model we can also understand the assumptions of CPAP therapy. The Starling resistor model consists of a tube passing through a sealed box. The tube consists of two rigid segments with a collapsible segment interposed in between corresponding to the muscular pharynx of the human’s airway. The fundamental concept of treating OSA with nasal CPAP is that nasal CPAP increases the pressure inside the pharynx above the pharyngeal critical closing pressure and thereby keeps the pharynx open (Fig. 19.1) [6].
The Starling resistor model consists of a tube passing through a sealed box. The tube consists of two rigid segments with a collapsible segment interposed in between. In humans, the rigid tube is represented by the nose and trachea and the collapsible segment corresponds to the muscular pharynx of the human’s airway. As long as the pressure inside the pharynx (Pin) is greater than the pressure outside of the surrounding tissue pressure (Pout), the pharynx does not collapse [6]
The presence of nasal obstruction, either due to anatomical factors, inflammatory diseases, or nasal valve incompetence, may also lead to mouth breathing during daytime or mouth opening at night due to increased nasal resistance, changing upper airway dynamics, and increasing the propensity to develop OSA [6].
Interestingly, the mask of choice for patients with OSA with nighttime mouth opening should not be necessarily the oronasal mask. Actually, nasal CPAP mask seems to be very efficient in decreasing mouth opening episodes as well as the amplitude of mouth opening movements in patients with OSA [6]. Ruhle et al. had already demonstrated a reduction in mouth opening events and a decrease in the number of oral breaths with nasal CPAP [12]. Moreover, nasal CPAP enhances the Starling resistor model by increasing the pressure inside the pharynx, above the pharyngeal critical closing pressure, thereby keeping the pharynx open, while oronasal mask violates the Starling resistor model as pressure applied simultaneously through the mouth and nose may lead to a collapse of the upper airway. In Fig. 19.2 is represented the same patient without and under CPAP therapy, with nasal mask and with oronasal mask.
This illustration demonstrates the relationship between the Starling model and mask type. There are two rigid segments (nose and trachea) with a collapsible segment interposed in between (pharynx). Level I, the nose (upstream); level II, the pharynx (collapsible segment); and level III, the trachea (downstream). (a) Upper airway obstruction during inhalation due to negative airway pressure. (b) The use of CPAP through a nasal mask enhances the Starling resistor model by increasing the pressure inside the pharynx above the pharyngeal critical closing pressure and thereby keeping the pharynx open. (c) The use of CPAP through an oronasal mask violates the Starling resistor model as pressure applied simultaneously through the mouth and nose may lead to displacement of the tongue and soft palate posteriorly and obstruction of the upper airway [6]
Another study achieved similar findings. Andrade et al. investigated the effect on upper airway of CPAP therapy with nasal and oronasal routes in patients with severe OSA. When the CPAP flow route was shifted from the nasal to the oronasal or oral route, there was a significant and progressive reduction in the distance between epiglottis and tongue base and the retroglossal area, respectively. They also realized that patients had upper airway obstruction during oronasal CPAP, despite maintaining predominant breathing through the nose preceding the obstructive event [6, 7]. But does this mean all patients should be advised to use nasal masks?
3.1 Adherence
Rowland et al. conducted a prospective study where they compared among other things CPAP adherence. In this study there was no statistically significant difference in CPAP adherence between interfaces. However, patient satisfaction and quality of sleep were higher with the nasal mask and nasal mask with chinstrap than with the oronasal mask. When they were asked about their preference, most chose nasal mask over the nasal mask with chinstrap and oronasal masks, as that was perceived to be easier to fit and keep in place, leak less, be quieter, and provide a more restful sleep [3].
The efficacy of intra-nasal compared with nasal interfaces for improving adherence to CPAP therapy was evaluated using meta-analyses of two crossover randomized controlled trials (RCTs) of 3- to 4-weeks duration [13, 14] involving newly treated participants with a range of CPAP pressures and one RCT [15] for 1-week periods in participants previously established on nasal CPAP treatment at ≥12 cmH2O for >6 months. There was no clinically significant difference in mean adherence and percent of nights of CPAP use with intra-nasal interfaces compared with nasal interfaces [16].
The efficacy of oronasal compared with nasal interfaces for improving adherence was evaluated in meta-analyses of three crossover RCTs of 3- to 4-week duration [3, 17] which demonstrated a clinically significant improvement in adherence of 0.6 h/night (95% CI: −0.2 to 1.3 h/night) with nasal interface compared with oronasal interface [16]. Another meta-analysis was performed of three nonrandomized studies in which participants were predominantly male without major medical comorbidities, with previously untreated moderate to severe OSA, treated for at least 3 weeks up to 24 months [18,19,20]. A clinically significant difference in adherence was also demonstrated with an improve of 0.7 h/night (95% CI: 0.2–1.2 h/night) in adherence of nasal interfaces. There was insufficient evidence to perform meta-analysis for the effects on adherence for oral versus nasal interfaces. Although it’s worth mentioning that the American Academy of Sleep Medicine commissioned a task force of content experts to conduct this review and accordingly to their clinical experience, most patients have difficulties using an oral interface over the long term [16].
3.2 Positive Pressure and Apnea Hypopnea Index (AHI)
An observational study conducted by Borel et al. associated oronasal mask use with higher treatment pressures when compared with nasal masks [18]. In contrast, observational crossover studies by Bakker et al., Teo et al., and Ebben et al. have demonstrated no differences between nasal and oronasal masks and the pressure prescribed. The interpretability of these studies is somewhat limited by their small sample sizes which not only limits the ability to explore relationships between mask types and pressure requirements but also reduces the array of craniofacial structures examined. Also, subjects were followed during a short number of nights for each mask type, making the results susceptible to night-to-night variability. Moreover, each study dictated a specific oronasal mask to be used in the study, so the lack of differences in therapeutic pressures may be unique to these particular models of masks. Shirlaw et al. conducted a randomized, crossover trial design with a greater number of subjects using both a nasal mask and an oronasal mask for a longer period of time (4 weeks). They found an equal proportion of noncompliance at time of recruitment, with 26% and 23% of subjects noncompliant with CPAP therapy (threshold of 4 h per night) for oronasal mask and nasal mask interfaces, respectively [2]. Actually, in their work, parameters such as positive airway pressure requirements (median and 95th percentile pressures), leak, and residual AHI were not statistically different between oronasal and nasal masks [2]. It should be emphasized that these similarities in pressure requirements between nasal and oronasal masks were not universal. Indeed, four subjects in this last study showed much higher pressures when using an oronasal mask. This would suggest that there are specific aspects that predispose them to higher pressure requirements while using an oronasal mask. As already mentioned, decreases in either the retroglossal or retropalatal area with use of an oronasal mask may explain this occurrence, but only partially [2]. Still, higher pressure requirement was not isolated to oronasal mask use. Some subjects required higher therapeutic pressures with a nasal mask compared to the oronasal mask [2].
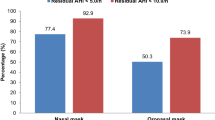
Patil et al. analyzed the efficacy of intra-nasal compared to nasal interfaces for the treatment of OSA in adults which was evaluated using a meta-analysis of three crossover RCTs. Of those, two studies of 3- to 4-week duration [13, 14] involve newly treated participants with a range of CPAP pressures. The other study analyzed a 1-week period [15] in participants previously treated with nasal CPAP treatment at ≥12 cmH2O for >6 months. There was no clinically significant difference in AHI in neither group. The authors also compared the efficacy of oronasal and nasal interfaces for the treatment of OSA in previously untreated adults. This was evaluated through a meta-analysis of two crossover RCTs: one of 3-week duration [17] and one of 4-week duration [3]. Concordantly with previous data, they found that residual AHI was higher with oronasal than with nasal interfaces, although this difference was not clinically significant. There was insufficient evidence to perform a meta-analysis on OSA severity for oral versus nasal interfaces, perhaps because it is not often used. Even though, one RCT employing a 4-week crossover design demonstrated no clinically significant differences in AHI with oral compared with nasal interfaces [16]. Further studies are needed to elucidate other contributory factors.
3.3 Leaks
It is possible to try to reduce mouth leaks by using a chinstrap that supports and restricts jaw movements, but there is limited data supporting the efficacy of this approach [3]. The oronasal mask covers both the nose and the mouth and allows the patient to breathe through the mouth while maintaining therapeutic CPAP pressure which, in theory, would eliminate mouth leaks [3]. However, theses masks, as they have a wider surface, can be more difficult to adapt to patients’ face, resulting in more leaks, patient discomfort, and reduced adherence [3, 18].
More recently, some studies have analyzed the relationship between mouth opening and body position, showing that mouth opening, and consequently leak, was more influenced by sleep stage than by body position [9, 21]. Lebret et al., in their work, found that lateral and prone positions increased the risk of unintentional leak, probably because of mask displacement or traction on the CPAP tube in these positions. Nasal obstruction may also be an independent determining factor of mouth opening that can lead to the use of an oronasal mask, although in their study, nasal obstruction and mouth opening were significantly greater in patients who used an oronasal mask. Moreover, the oronasal mask itself may promote mouth opening by displacing the jaw backward and downward [22,23,24,25]. Once more, the specific indications for oronasal masks are still debated and more studies are necessary. But, accordingly to Lebret et al.’s work, there is an overall equivalence between oronasal and nasal masks except for the specific situations of mouth opening and REM sleep, in which there were fewer leaks with oronasal interfaces. This suggests that oronasal masks could be an effective solution to reduce unintentional leak in such cases [23]. There was insufficient data comparing other interface models.
3.4 Sleepiness
Regarding self-reported sleepiness, once more there are insufficient data and are contradictory. BaHammam et al. reported that the use of nasal pillow mask was associated with less adverse effects and better perceived sleep quality in the first 3 weeks of CPAP treatment [6]. Later on the efficacy of intra-nasal was compared with nasal interfaces using a meta-analysis of two crossover studies, one employing a 3-week duration [13] and one employing a 4-week duration [14]. There was no clinically significant difference in self-reported sleepiness between intra-nasal and nasal interfaces as assessed with the Epworth Sleepiness Scale (ESS). The efficacy of oronasal versus nasal interfaces was evaluated using a meta-analysis of two RCTs [3]. The meta-analysis demonstrated no clinically significant difference in self-reported sleepiness between the interfaces as assessed with the ESS. There was insufficient evidence to perform meta-analysis for the effects on self-reported sleepiness for oral versus nasal interfaces. Actually, in concern of self-reported sleepiness no meta-analyses were able to demonstrate clinically significant differences in self-reported sleepiness between the different mask interfaces [16].
3.5 Quality of Life
When looking to quality of patient life accordingly to the type of interface used, there was insufficient evidence to perform a meta-analysis. Only one RCT [13] was identified that met inclusion criteria which assessed the effect of intra-nasal versus nasal interfaces on quality of life. The study took place over a period of 3 weeks each in a crossover RCT and accessed the effect of interface in quality of life with a questionnaire, but no clinically significant difference in quality of life was found comparing intra-nasal versus nasal interfaces [13, 16].
3.6 Other Side Effects
Since this is a therapy based in the delivery of positive pressure during a long period of time on a daily basis, side effects are expected and have been reported with all interfaces and, of course, may adversely impact adherence. Side effects may differ between interface type and between individuals for a given interface. A well-sealed interface is necessary for effective delivery of CPAP, and mask and/or mouth leak may adversely impact treatment efficacy. Improvements of air leak and other side effects through interface selection may have beneficial effects on treatment adherence and efficacy.
The nasal mask is most commonly used, although some studies report a high rate of side effects, sometimes in over 50% of individuals. In those, mouth and mask leaks are common and are associated with drying of the nasal and the oral mucosa, sore eyes, irritating noises and airstreams, and even increased arousals of patients [3].
For intra-nasal versus nasal interfaces, side effect data were reported from two crossover RCTs of 3-week and 4-week duration [13, 14] involving newly treated participants with a range of CPAP pressures or for 1-week periods [15] in participants previously established on nasal CPAP treatment at ≥12 cmH2O for >6 months. An overall multi-item side effect score favored intra-nasal interfaces in one study of newly treated participants, but there were no clinically significant differences in overall side effects between interfaces for the other two studies. Individual side effects including pressure sensation on the face, skin irritation, claustrophobia, and obtrusiveness were in general less for intra-nasal interfaces in the three studies, while nasal interfaces were scored as being less obtrusive. There were no clinically significant differences between interfaces for nasal or oral congestion or dryness. In one study, overall mask satisfaction scores were significantly higher for intra-nasal interfaces, while in the other two studies there was no clinically significant difference in preference between intra-nasal and nasal interfaces either for newly treated or previously treated participants. Overall, differences in side effects between the two interfaces were not clinically significant.
In a non-RCT of 2311 participants in whom 62% were using nasal and 26% oronasal interfaces, there were greater reports in symptoms of eye irritation, dry mouth, choking sensation, and psychologically perceived inconvenience with oronasal interfaces, while there were no clinically significant differences between oronasal and nasal interfaces in nasal congestion, headache, aerophagia, or family tolerance of treatment. [16]. In these non-RCT cohorts, oronasal interfaces were least often chosen by participants for long-term treatment compared with nasal and intra-nasal interfaces [18, 19]. Borel et al. also demonstrated lower compliance (based on average hours used per night) and a greater risk of noncompliance (based on the proportion of nights with 4 h or more usage) with oronasal masks compared with nasal masks [2]. Rowland et al. obtained similar results. Nasal interface was reported as more comfortable although it was associated with more complaints of nasal and throat dryness, nasal congestions, and rhinitis but not nasal stuffiness. In the other hand, self-reported mask leak, sore eyes, claustrophobia, and difficulty exhaling were clinically significant and more predominant with the oronasal interface. In their study mask noise and leak were also greater with oronasal masks which were also reported to be harder to fit and hold in place [3].
More recently in Shirlaw’s work, nasal masks generally appear to be more preferable than oronasal masks, based on the greater number of subjects withdrawing during the study because of intolerance of the oronasal mask and the preference for the nasal mask in the majority of subjects completing the trial [2].
In Patil et al. review, there were clinically important differences in side effects with oronasal compared with nasal interfaces, and these increased side effects appear to result in a patient preference for nasal over oronasal interfaces and ultimately in a significant reduction in adherence to CPAP with oronasal when compared to nasal CPAP [16].
Advantages and disadvantages of the three main types of interfaces are presented in Table 19.2:
As already mentioned above, the correct mask fitting is an essential step for the success of CPAP therapy. BaHammam et al. proposed a flow chart to support and guide the choice of the correct interface for each patient (Fig. 19.3).
4 Conclusions
The effectiveness of CPAP depends on the numbers of hours the patient really is under positive pressure therapy. Interface selection is a key factor to CPAP compliance and should be based on individual patient preference and tolerance. It is important to let the patient try different types of masks and to choose the most suitable. Published data suggest that unless patients have significant nasal problems, OSA therapy may be better tolerated and more effective if initially commenced with nasal mask. There is also increasing recognition about the different phenotypes underlying OSA and the route of breathing as important factors to be accounted for when choosing an interface. Further studies are needed to guide and substantiate medical decision. Nowadays, there are a huge number of interfaces available in the market. Their characteristics, advantages, and disadvantages should be compared. New studies should be developed, stronger studies with bigger samples and a longer duration. It is well known that as time goes on, the number of people who fail to comply CPAP therapy raises. Finally, studies should also be developed including hybrid masks, to help to clarify its position in interface choice algorithm.
5 Key Recommendations
-
The fundamental concept of CPAP therapy is that nasal CPAP increases the pressure inside the pharynx above the pharyngeal critical closing pressure maintaining the pharynx open.
-
Despite different airway delivery routes having little impact on CPAP efficacy, compatibility with a specific patient’s preferred method of breathing constitutes a significant factor in patient adherence.
-
There is no difference in therapeutic pressures when using either a nasal or oronasal mask.
-
There is no difference in the residual AHI between nasal and oronasal mask use.
-
Nasal masks are preferable based on better tolerability and compliance with therapy.
-
Oronasal mask itself may promote mouth opening by displacing the jaw backward and downward.
-
In specific situations of mouth opening and REM sleep, oronasal interfaces demonstrated fewer leaks when compared to nasal masks.
-
Regarding sleepiness no meta-analyses were able to demonstrate clinically significant differences in self-reported sleepiness between interfaces.
-
Difficulty with mask interface is common and none proved to be clearly superior.
-
An oronasal mask may be useful in patients with mouth leak or severe nasal congestion.
-
Changing mask type or improving fit can dramatically improve adherence and satisfaction.
References
Heinzer R, Andries D, Bastardot F, et al. Prevalence of sleep disordered breathing in middle-aged general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–8.
Shirlaw T, Duce B, Milosavljevic J, et al. A randomised crossover trial comparing nasal masks with oronasal masks: no differences in therapeutic pressures or residual apnea-hypopnea indices. J Sleep Res. 2019;28(5):e12760.
Rowland S, Aiyappan V, Hennessy C, et al. Comparing the efficacy, mask leak, patient adherence, and patient preference of three different CPAP interfaces to treat moderate-severe obstructive sleep apnea. J Clin Sleep Med. 2018;14(1):101–8.
Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–39.
Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29(3):381–401.
BaHammam A, Singh T, George S, et al. Choosing the right interface for positive airway pressure therapy in patients with obstructive sleep apnea. Sleep Breath. 2017;21(3):569–75.
Andrade R, Madeiro F, Piccin V, et al. Impact of acute changes in CPAP flow route in sleep apnea treatment. Chest. 2016;150(6):1194–201.
Andrade R, Madeiro F, Genta P, Lorenzi-Filho G. Oronasal mask may compromise the efficacy of continuous positive airway pressure on OSA treatment: is there evidence for avoiding the oronasal route? Curr Opin Pulm Med. 2016;22(6):2016.
Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;4:CD005308.
Doyle C. The engineering of masks for application in continuous positive airway pressure (CPAP) therapy. Newcastle upon Tyne: New Castle University; 2017.
Gleeson K, Zwillich C, Braier K, White D. Breathing route during sleep. Am Rev Respir Dis. 1986;134(1):115–20.
Ruhle K, Nilius G. Mouth breathing in obstructive sleep apnea prior to and during nasal continuous positive airway pressure. Respiration. 2008;76(1):40–5.
Massie C, Hart R. Clinical outcomes related to interface type in patients with obstructive sleep apnea/hypopnea syndrome who are using continuous positive airway pressure. Chest. 2003;123(4):1112–8.
Ryan S, Garvey J, Swan V, Behan R, McNicholas W. Nasal pillows as an alternative interface in patients with obstructive sleep apnoea syndrome initiating continuous positive airway pressure therapy. J Sleep Res. 2011;20(2):367–73.
Zhu X, Wimms A, Benjafield A. Assessment of the performance of nasal pillows at high CPAP pressures. J Clin Sleep Med. 2013;9(9):873–7.
Patil S, Ayappa I, Caples S, et al. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2019;15(2):301–34.
Ebben M, Narizhnaya M, Segal A, et al. A randomised controlled trial on the effect of mask choice on residual respiratory events with continuous positive airway pressure treatment. Sleep Med. 2014;15(6):619–24.
Borel J, Tamisier R, Dias-Domingos S, et al. Type of mask may impact on continuous positive airway pressure adherence in apneic patients. PLoS One. 2013;8(5):e64382.
Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200–8.
Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667–72.
Mador MJ, Krauza M, Pervez A, Pierce D, Braun M. Effect of heated humidification on compliance and quality of life in patients with sleep apnea using nasal continuous positive airway pressure. Chest. 2005;128(4):2151–8.
Lebret M, Arnol N, Martinot J, et al. Determinants of unintentional leak during CPAP treatment in obstructive sleep apnea syndrome. Chest. 2017;S0012-3692(17):31435–6.
Lebret M, Arnol N, Contal O, et al. Nasal obstruction and male gender contribute to the persistence of mouth opening during sleep in CPAP-treated obstructive sleep apnoea. Respirology. 2015;20(7):1123–30.
Borel J-C, Gakwaya S, Masse J-F, Melo-Silva CA, Sériès F. Impact of CPAP interface and mandibular advancement device on upper airway mechanical properties assessed with phrenic nerve stimulation in sleep apnea patients. Respir Physiol Neurobiol. 2012;183(2):170–6.
Andrade R, Viana F, Nascimento J, et al. Nasal vs oronasal CPAP for OSA treatment: a meta-analysis. Chest. 2018;153(3):665–74.
Dibra M, Berry R, Wagner M. Treatment of obstructive sleep apnea. Choosing the Best Interface Sleep Med Clin. 2017;12:543–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mestre, A.M., Ramos, A.L. (2020). Importance of Interface in the Effectiveness of CPAP. In: Esquinas, A.M., et al. Noninvasive Ventilation in Sleep Medicine and Pulmonary Critical Care. Springer, Cham. https://doi.org/10.1007/978-3-030-42998-0_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-42998-0_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-42997-3
Online ISBN: 978-3-030-42998-0
eBook Packages: MedicineMedicine (R0)