Abstract
Purpose
Mask type (nasal versus oronasal) can affect the optimal pressure required to correct the apnea/hypopnea index (AHI) in obstructive sleep apnea (OSA) subjects treated with CPAP. Our objective was to evaluate if mask type influenced CPAP titration outcomes in OSA patients.
Methods
A retrospective study of individuals with a baseline AHI ≥ 15.0/h, who received an auto-adjusting CPAP titrating device (S9 AutoSet ResMed®) in a sleep-lab setting. The mask type oronasal (OM) or nasal (NM) was always selected by the patients. Optimal pressure requirements, leak, and residual AHI were compared based on mask type.
Results
Overall, 436 patients were included: 283 with NM (64.9%) and 153 with OM (35.1%). At baseline, NM and OM cohorts had similar AHI (p = 0.160). Patients allocated to the OM cohort had a higher 95th percentile pressure, a higher 95th percentile leak, and a higher residual AHI than those with a NM: pressure requirement: 12.9 cm H2O (IQR: 10.6–15.0) versus 10.7 cm H2O (IQR: 9.2–12.3); leak: 21.6 L/min (IQR: 9.6–37.2) versus 9.6 L/min (IQR: 3.6–19.2); and residual AHI: 4.9/h (IQR: 2.4–10.2) versus 2.2/h (IQR: 1.0–4.4), respectively (p < 0.001 for all).
Conclusions
CPAP mask type based on individual preferences exerts profound effects on optimal CPAP pressures and efficacy. Patients titrated with OM showed higher pressure requirements, had higher a leak, and higher residual AHI when compared to NM, which may adversely impact treatment adherence and other health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is an extremely prevalent disease characterized by recurrent upper airway obstructive episodes during sleep, causing intermittent hypoxemia and sleep fragmentation [1,2,3]. This disorder is associated with several significant comorbidities, such as cardiovascular and cerebrovascular disease, metabolic syndrome, neurocognitive and mood deficits, and an increased risk of motor vehicle accidents [4,5,6,7].
Currently, continuous positive airway pressure (CPAP) is recommended, as the first choice, for treating patients diagnosed with moderate to severe OSA [apnea/hypopnea index (AHI) ≥ 15.0/h] [8]. The proposed idea for treatment with CPAP would be that, when applied with a mask interface, it would act as a pneumatic splint to maintain the patency of the upper airway [8]. In OSA patients, regular CPAP treatment can effectively reduce excessive daytime sleepiness, improve cognitive function, improve quality of life, reduce blood pressure in hypertensive individuals, and reduce the risk of cardiovascular complications [9,10]. However, treatment effectiveness depends on the regular use of CPAP. Predictors of adherence to CPAP therapy include OSA severity, degree of daytime sleepiness, socioeconomic status, and the level of understanding of the patient concerning therapy and mask type [11].
The pressure required for CPAP treatment is usually titrated, either automatically or manually, aiming to find the minimum and optimal CPAP level that will correct obstructive events, restore normal arterial oxygen saturation and reduce sleep fragmentation [8,12,13]. During titration, it is also possible to select the best interface for the patient [14]. The adequate selection of mask interface is a key determinant of treatment efficacy and compliance. Although several studies demonstrate the effectiveness of CPAP in correcting respiratory events in patients suffering from OSA, many patients do not tolerate CPAP and do not adhere to treatment, with compliance being surprisingly and consistently low all around the world [15,16,17]. There are various possible reasons for this low adherence, and the discomfort caused by mask type is one of the most frequently mentioned by patients [18,19,20].
Generally, nasal masks (NM) are the most used interface. Oronasal masks (OM) are frequently recommended for patients who have excessive mask leaks from mouth breathing and, recently, nasal pillows have also gained popularity, since they provide the opportunity to reduce mask size [21]. Therefore, it is intuitive to assume that the type of interface can have a decisive impact on adherence to CPAP treatment. However, CPAP titration effectiveness (pressure requirement, leak, and residual events) according to the type of mask used in the titration shows contradictory results [19,20,21,22,23,24,25,26,27,28,29,30,31,32].
Notwithstanding, there is only a scarce number of studies comparing CPAP titration effectiveness based on mask type (OM or NM) as chosen by the patient. In the present study, our main objective was to evaluate parameters obtained during CPAP titration (pressure requirement, leak, and residual AHI) in patients grouped according to the mask type selected by them: NM or OM.
Materials and methods
Study design
This cross-sectional study was carried out between January 2017 and June 2018. The eligibility criteria were: adult patients (age ≥ 18 years) diagnosed with moderate to severe OSA (AHI ≥ 15.0/h) and referred for in-lab titration. The exclusion criteria were as follows: 1) individuals who were already on regular CPAP treatment, 2) no baseline full in-lab polysomnography (PSG) available, and 3) those who underwent bilevel positive airway pressure (BiPAP) titration. All subjects were grouped into two independent cohorts selected from the mask type (NM or OM) used during the titration. The choice of the mask was always based on the patient's preference, with no interference from the sleep technicians.
Ethical considerations
The study protocol was approved by the Research Ethics Committee of the Federal University of Rio de Janeiro (#666.608) and waived the patient-consent requirement, because no intervention was performed. The anonymity of each participant was strictly preserved.
Data acquisition
Gender, age, body-mass index (BMI), neck circumference (NC), and Epworth Sleepiness Scale (ESS) were systematically collected. BMI was calculated by dividing the weight in kilograms by the square of the height in meters (kg/m2), while NC (in cm) was measured using a flexible tape with all subjects in the upright sitting position, with the upper edge of the tape measure placed immediately below the laryngeal prominence and applied perpendicularly to the long axis of the neck. Subjective sleepiness was assessed using ESS, an 8-item questionnaire, with four-point scales (from zero to three) [33]. Score ≥ 11 points (final score from 0 to 24 points) was considered as excessive daytime somnolence [33].
Overnight in-lab polysomnography
All sleep tests were conducted in a Brazilian single-center: SleepLab - Sleep Laboratory, Rio de Janeiro. All participants underwent an attended, in-lab full PSG (EMBLA® S7000, Embla Systems, Inc., Broomfield, CO, USA) consisting of the recording of electroencephalography, electrooculography, electromyography (chin and legs), electrocardiography, airflow, thoracic and abdominal impedance belts, oxygen saturation (SpO2), microphone for snoring, and sensors for body position. Polysomnographic data were scored manually following the latest 2012 American Academy of Sleep Medicine (AASM) guidelines [34] by two board-certified sleep physicians. Polysomnographic data included AHI and oxygen saturation (SpO2) values (baseline, average, and lowest). Obstructive apneas were defined as a decrease of at least 90% of airflow from baseline with persistent respiratory effort, lasting at least 10 seconds, while hypopneas were classified with a decrease of at least 30% of pre-event during ≥ 10 seconds associated with ≥ 3% oxygen desaturation or an arousal. AHI was calculated as the number of apnea plus hypopnea/total sleep time (in hours).
Overnight in-lab titration
All participants were subjected to an auto-adjusting CPAP titrating with humidification (S9 AutoSet ResMed®, Sydney, Australia) in a sleep laboratory setting. All masks were selected from the available commercial line produced by ResMed® (Sydney, Australia), with the appropriate size to provide a balance between fit, comfort, and sealing of the mask. After the patient chose the type of mask (NM or OM), sleep technicians adjusted the interface, providing support to the patient during the night. The S9 AutoSet ResMed® device was programmed to apply a minimum pressure of 4.0 cm H2O and a maximum pressure of 20.0 cm H2O, with expiratory pressure relief (EPR) of 3.0 cm H2O. The auto-adjusting CPAP data were downloaded using ResScan® software: CPAP pressures (50th, 95th, and maximum), leak (50th, 95th, and maximum), and residual AHI were recorded into the database.
Statistical analysis
Data analysis was carried out using SPSS for Windows statistical software (version 21.0; Chicago, IL, USA). Results are summarized as the median and interquartile range (IQR) or as number (n) and percentage (%) for quantitative and qualitative variables, respectively. Comparisons between groups were performed using the Chi-square test for dichotomous variables and Mann–Whitney nonparametric test for continuous variables. Multivariate logistic regression was developed with clinical and polysomnographic parameters, being residual AHI < 5.0/h or < 10.0/h used as outcome. All statistical tests were two-tailed and statistical significance was set at p < 0.05.
Results
Of a total of 571 consecutive individuals who were referred for auto-adjusting in-lab titration, 135 patients (23.6%) were subsequently removed for the following reasons: 93 with no baseline PSG available, 17 with mild OSA diagnosis, 15 referred for BiPAP titration, and 10 already receiving regular CPAP treatment. Therefore, 436 participants were allocated into two independent cohorts: NM (n = 283; 64.9%) or OM (n = 153; 35.1%). Our sample included predominantly men (65.8%), with a median age of 56.0 years (IQR: 46.0–66.0) and a median BMI of 29.5 kg/m2 (IQR: 26.4–33.0). As shown in Table 1, all clinical and polysomnographic data were similar in the two datasets, except for age (p = 0.019) and average SpO2 (p = 0.009). Interestingly, both NM and OM cohorts had similar median baseline AHI values: 40.2/h (IQR: 28.5–58.3) versus 44.4/h (IQR: 31.0–65.1), respectively (p = 0.160); Table 1.
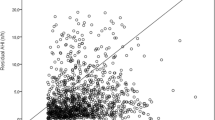
Table 2 summarizes the pressure requirements, leaks, and residual events data obtained by CPAP titration. All values related to optimal CPAP pressures, leak, and residual events were significantly higher in subjects with OM compared to those who chose the NM (p < 0.001 for all comparisons). Figure 1 reports the percentage of individuals who achieved a residual AHI < 5.0/h or < 10.0/h, through CPAP titration, based on the choice of mask. This percentage was always significantly higher for participants who chose the NM over the OM; both with p < 0.001. The chance of subjects who chose NM over OM to have a residual AHI < 5.0h or < 10.0/h was as follows: unadjusted odds ratio (OR): 3.377 [95% confidence interval (CI) 2.215-5.150] and unadjusted OR: 4.655 (95% CI: 2.606-8.316), respectively.
Frequency (%) of patients with OSA showing residual apnea/hypopnea index (AHI) < 5.0/h or < 10.0/h in a cohort of individuals who preferred a nasal mask compared to those who preferred an oronasal mask. This percentage was always significantly higher for individuals who chose the NM over the OM (both with p < 0.001)
Multivariate stepwise logistic regression (Table 3) revealed that BMI, baseline AHI, and mask type were independently associated with residual AHI < 5.0/h: adjusted OR: 0.911 (95% CI 0.852–0.975), adjusted OR: 1.021 (95% CI 1.009–1.033), and adjusted OR: 4.097 (95% CI 2.550–6.584), respectively. Also, lowest SpO2 and mask type emerged as independent parameters for residual AHI < 10.0/h: adjusted OR: 0.945 (95% CI 0.905–0.988) and adjusted OR: 4.671 (95% CI 2.483–8.784). For both outcomes (residual AHI < 5.0 or < 10.0/h), the mask type shows the greatest degree of association: regression coefficient (β) of 1.410 and 1.541, respectively; Table 3.
Discussion
The main findings of the present study were that patients who underwent in-lab CPAP titration with OM required higher levels of therapeutic CPAP pressures, and exhibited greater leak and residual AHI than individuals who chose NM. Besides, the percentage of individuals with residual AHI < 5.0/h or < 10.0/h, i.e., therapeutic success, was significantly higher in individuals who preferred NM compared to those with OM, showing a better correction of respiratory parameters in the NM cohort over the OM cohort. Corroborating these findings, individuals titrated with NM were ~4 times more likely to exhibit a residual AHI < 5.0/h or < 10.0/h than individuals who preferred to be titrated with OM.
These findings highlight that NM should, whenever possible, be the first option of mask type in an auto-adjusting CPAP titration, with the ulterior intent to achieve improved adherence to CPAP treatment. Several studies show that the chosen interface is crucial for adequate adherence to the treatment offered [16,21,22,23]. However, a prior study reported that adherence to CPAP did not differ between different types of masks, although the residual AHI was lower with the use of NM compared to OM [24]. Moreover, patients reported greater comfort, better sleep quality, and a greater preference for NM [24].
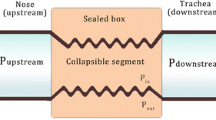
Many OSA patients have nasal obstruction, and may, therefore, be intolerant to NM. NM completely covers the nose, while the pillow mask consists of two intranasal pillows that can be used as an alternative to NM, because they are smaller and more comfortable. OM covers the nose and mouth, allowing the individual to breathe through both the mouth and the nose. Although OM is a larger and more uncomfortable mask, it can be a possible and feasible alternative in subjects with nasal obstruction. Conversely, the reasons why an OM can induce upper airway obstruction are not fully understood. One possibility is that OM can push the tongue and soft palate, inducing obstruction and increased upper airway resistance [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35].
The comparison of titration effectiveness from the interfaces (NM or OM) is rarely made using the patient's choice as the allocation procedure. This was the reason why we opted for a real-life study, in which the sleep-lab technicians who supervised the exams did not influence on the choice of the interface type. Our study found that the vast majority of participants chose NM over OM. Most studies comparing mask type claim that NM is usually associated with better outcomes (therapeutic pressure, leak, and residual events) [25,26,27,28,29,30], but there are some studies with contradictory results [31,32].
In a study with 55 individuals randomly assigned to one of three masks (nasal pillows, NM, and OM) who underwent a CPAP titration, OM required significantly higher pressures in subjects with moderate to severe OSA [26]. Similarly, 109 patients with moderate to severe OSA were studied using an autotitrating device [30]. The therapeutic CPAP level was also significantly higher when administered via OM, leading to an increased number of residual events (both p < 0.05) [30].
However, when 60 participants already using CPAP were randomly allocated to a NM or an OM with Auto‐CPAP titration for 2 weeks, and were then switched to the alternative mask for another 2 weeks, there were no differences in median 95th percentile pressures (NM: 11.5 cm H2O versus OM: 11.7 cm H2O; p = 0.115) or median residual AHI (NM: 4.9 events/h versus OM: 5.3 events/h; p = 0.234) [31]. Similarly, a randomized crossover study with 24 participants with moderate to severe OSA, therapeutic level of CPAP, as determined during titration, was similar for NM and OM [32]. Despite this, residual AHI was on average, 5.7 events/h higher with the use of an OM versus a NM (p = 0.01) [32].
Among the several studies comparing different mask types in the context of OSA treatment, the approaches were very heterogeneous, making comparisons between them quite challenging if not impossible. Moreover, as they are frequently controlled, i.e., patients were not allowed to select their mask, this can limit the generalization of their findings. In contrast, our study did not apply any interference in the choice of the mask by the researcher or sleep technician. This choice was exclusively the result of the individual patient preference, which can translate into a greater generalization of our data. Also, as it was a real-life study, we were able to include a considerable number of participants, increasing the robustness of our findings.
Limitations and strengths
Our study has some limitations that deserve comment. First, the patients were all referred to a single sleep laboratory, which may limit the reproducibility of our findings in other settings. Second, the possibility of selection bias is plausible and should be considered. Also, we did not obtain adherence measures as a follow-up to the titration procedures to examine whether mask choice and our findings affected treatment adherence. Despite these limitations, our study included an adequate sample size of consecutively enrolled individuals. Besides, all participants underwent full PSG performed in our laboratory and were diagnosed with moderate to severe OSA, according to the AASM guidelines [34].
Conclusions
In a real-world setting, the present study showed that the choice of mask type significantly influences the main outcomes obtained by a CPAP titration. The CPAP pressure requirements were higher when administered through OM compared to NM. Also, the choice of OM led to more residual events and leak than with NM. Hypothetically, all of these factors may negatively impact treatment adherence.
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2003) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K et al (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 13:479–504
Sánchez-de-la-Torre M, Campos-Rodriguez F, Barbé F (2013) Obstructive sleep apnoea and cardiovascular disease. Lancet Respir Med 1:61–72
Peled N, Kassirer M, Shitrit D, Kogan Y, Shlomi D, Berliner AS et al (2007) The association of OSA with insulin resistance, inflammation and metabolic syndrome. Respir Med 101:1696–1701
Boland LL, Shahar E, Iber C, Knopman DS, Kuo TF, Nieto FJ et al (2002) Measures of cognitive function in persons with varying degrees of sleep-disordered breathing: the Sleep Heart Health Study. J Sleep Res 11:265–272
Mulgrew AT, Nasvadi G, Butt A, Cheema R, Fox N, Fleetham JA et al (2008) Risk and severity of motor vehicle crashes in patients with obstructive sleep apnoea/hypopnoea. Thorax 63:536–541
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 15:335–343
Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ (2006) Continuous positive airway pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001106.pub3
Sharma SK, Agrawal S, Damodaran D, Sreenivas V, Kadhiravan T, Lakshmy R et al (2011) CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med 365:2277–2286
Kohler M, Smith D, Tippett V, Stradling JR (2010) Predictors of long-term compliance with continuous positive airway pressure. Thorax 65:829–832
Gao W, Jin Y, Wang Y, Sun M, Chen B, Zhou N et al (2012) Is automatic CPAP titration as effective as manual CPAP titration in OSAHS patients? A meta-analysis. Sleep Breath 16:329–340
Morgenthaler TI, Aurora RN, Brown T, Zak R, Alessi C, Boehlecke B et al (2008) Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine Report. Sleep 31:141–147
Chai CL, Pathinathan A, Smith B (2006) Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005308.pub2
Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE (2011) A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 15:343–356
Borel JC, Tamisier R, Dias-Domingos S, Sapene M, Martin F, Stach B et al (2013) Type of mask may impact on continuous positive airway pressure adherence in apneic patients. PLoS ONE 8:e64382
Schwab RJ, Badr SM, Epstein LJ, Gay PC, Gozal D, Kohler M et al (2013) An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med 188:613–620
Andrade RGS, Viana FM, Nascimento JA, Drager LF, Moffa A, Brunoni AR et al (2018) Nasal vs oronasal CPAP for OSA treatment: a meta-analysis. Chest 153:665–674
Madeiro F, Andrade RGS, Piccin VS, Pinheiro GDL, Moriya HT, Genta PR et al (2019) Transmission of oral pressure compromises oronasal CPAP efficacy in the treatment of OSA. Chest 156:1187–1194
Andrade RG, Piccin VS, Nascimento JA, Viana FM, Genta PR, Lorenzi-Filho G (2014) Impact of the type of mask on the effectiveness of and adherence to continuous positive airway pressure treatment for obstructive sleep apnea. J Bras Pneumol 40:658–668
Massie CA, Hart RW (2003) Clinical outcomes related to interface type in patients with obstructive sleep apnea/hypopnea syndrome who are using continuous positive airway pressure. Chest 123:1112–1118
Beecroft J, Zanon S, Lukic D, Hanly P (2003) Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest 124:2200–2208
Goh KJ, Soh RY, Leow LC, Toh ST, Song PR, Hao Y et al (2019) Choosing the right mask for your Asian patient with sleep apnoea: a randomized, crossover trial of CPAP interfaces. Respirology 24:278–285
Rowland S, Aiyappan V, Hennessy C, Catcheside P, Chai-Coetzer CL, McEvoy RD et al (2018) Comparing the efficacy, mask leak, patient adherence, and patient preference of three different CPAP interfaces to treat moderate-severe obstructive sleep apnea. J Clin Sleep Med 14:101–108
Ebben MR, Narizhnaya M, Segal AZ, Barone D, Krieger AC (2014) A randomised controlled trial on the effect of mask choice on residual respiratory events with continuous positive airway pressure treatment. Sleep Med 15:619–624
Ebben MR, Oyegbile T, Pollak CP (2012) The efficacy of three different mask styles on PAP titration night. Sleep Med 13:645–649
Schorr F, Genta PR, Gregório MG, Danzi-Soares NJ, Lorenzi-Filho G (2012) Continuous positive airway pressure delivered by oronasal mask may not be effective for obstructive sleep apnoea. Eur Respir J 40:503–505
Ng JR, Aiyappan V, Mercer J, Catcheside PG, Chai-Coetzer CL, McEvoy RD et al (2016) Choosing an oronasal mask to deliver continuous positive airway pressure may cause more upper airway obstruction or lead to higher continuous positive airway pressure requirements than a nasal mask in some patients: a case series. J Clin Sleep Med 12:1227–1232
Bakker JP, Neill AM, Campbell AJ (2012) Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath 16:709–716
Bettinzoli M, Taranto-Montemurro L, Messineo L, Corda L, Redolfi S, Ferliga M et al (2014) Oronasal masks require higher levels of positive airway pressure than nasal masks to treat obstructive sleep apnea. Sleep Breath 18:845–849
Shirlaw T, Duce B, Milosavljevic J, Hanssen K, Hukins C (2019) A randomised crossover trial comparing nasal masks with oronasal masks: No differences in therapeutic pressures or residual apnea-hypopnea indices. J Sleep Res 28:e12760
Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J (2011) Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep 34:951–955
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. J Clin Sleep Med 8:597–619
Liang Y, Kimball WR, Kacmarek RM, Zapol WM, Jiang Y (2008) Nasal ventilation is more effective than combined oral-nasal ventilation during induction of general anesthesia in adults subjects. Anesthesiology 108:998–1003
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by Ethics Committee of the Federal University of Rio de Janeiro (number: 666.608).
Informed consent
This was a retrospective data analysis study and it did not need informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duarte, R.L.M., Mendes, B.A., Oliveira-e-Sá, T.S. et al. Nasal versus oronasal mask in patients under auto-adjusting continuous positive airway pressure titration: a real-life study. Eur Arch Otorhinolaryngol 277, 3507–3512 (2020). https://doi.org/10.1007/s00405-020-06242-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06242-x