Abstract
Obstructive sleep apnea (OSA) is a common breathing disorder during sleep, characterized by recurrent upper airway obstruction resulting in physiologic perturbations and frequent nocturnal arousals. Nocturnal noninvasive ventilatory (nNIV) techniques utilizing positive airway pressure (PAP) devices delivered through a comfortable mask interface have provided effective and acceptable treatment for this disorder. Despite excellent clinical outcomes with PAP, lack of adherence remains a major issue in clinical sleep medicine. Innovations in the delivery of PAP have attempted to address a major cause of noncompliance—patient discomfort with PAP. In the following review, new delivery modes of PAP in patients with OSA is presented along with relevant data regarding their efficacy in altering patient adherence patterns and clinical outcomes. The methods of PAP delivery to be discussed include continuous PAP (CPAP), bi-level PAP (BPAP), autotitrating PAP (APAP), pressure relief (PR), and auto-bi-level PAP (Auto-BPAP).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Obstructive sleep apnea
- Continuous positive airway pressure
- Bi-level positive airway pressure
- Autotitrating positive airway pressure
- Pressure relief
The advent of positive airway pressure (PAP) for the treatment of obstructive sleep apnea (OSA) as a form of “nocturnal non-invasive ventilation” (nNIV) enabled clinicians to finally offer patients with this debilitating disease a viable and acceptable treatment modality. Previously, the only effective treatment for OSA was tracheostomy [1], a method of mechanically bypassing the upper airway, thereby avoiding the consequences of repetitive upper airway closure during sleep. Obviously, tracheostomy was not readily accepted by patients with OSA. With the seminal publication by Colin Sullivan and colleagues in 1981 [2], a new era of treatment for OSA with PAP therapy was begun. During the next three decades, technological advances resulted in the development of a plethora of PAP delivery modes (Fig. 9.1), which have complicated and may potentially improve the treatment of OSA.
Pressure versus time relationships among different types of positive airway pressure (PAP) devices. (CPAP continuous positive airway pressure, BPAP bi-level positive airway pressure, APAP autotitrating positive airway pressure, PR pressure relief (A—CPAP with PR; B—BPAP with PR); Auto-BPAP—Auto bi-level positive airway pressure (A—Auto-BPAP with fixed pressure support (PS); B—Auto-BPAP with independent inspiratory and expiratory PAP (IPAP and EPAP)). ↑—initiation of inspiratory phase; ↓—initiation of expiratory phase)
Continuous Positive Airway Pressure
The first publication demonstrating the effective use of continuous positive airway pressure (CPAP) therapy in patients with OSA was in 1981 by Colin Sullivan and colleagues [2]. In their initial study, Sullivan et al. developed both a nasal interface, which was made from soft plastic tubes fit into each nostril and sealed by silicone rubber, and a “vacuum cleaner blower motor” connected by a wide-bore tube that could control the level of pressure delivered via mechanical narrowing of the free end of the tube. Five patients with generally severe OSA characterized by a mean apnea index of 62 events per hour during non-rapid eye movement (NREM) sleep and 64 events per hour during rapid eye movement (REM) sleep were fitted with a nasal interface and underwent polysomnography (PSG) with CPAP applied. The patients demonstrated complete cessation of obstructive events and marked improvement in sleep continuity, with CPAP pressures ranging from 4.5 to 10 cm H2O. Each patient remained awake and alert for the entirety of the following day, in stark contrast to their daytime hypersomnolence prior to using CPAP.
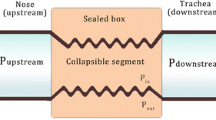
Despite early contradictory reports of the effectiveness of CPAP therapy [3, 4], it has become the standard of care for the management of OSA. CPAP consistently shows improvements in the apnea–hypopnea index, Epworth sleepiness scale (ESS), multiple sleep latency test (MSLT), maintenance of wakefulness test (MWT), and quality of life parameters as compared with placebo or conservative management in a recent systematic review [5]. CPAP is the standard of care therapy for moderate to severe OSA and should be considered in patients with mild OSA, particularly in those with daytime symptoms and/or other significant comorbidities [6]. The generally accepted mechanism by which CPAP resolves obstructive events is by acting as a pneumatic splint, maintaining patency of the upper airway in the setting of decreased intraluminal pressure during inspiration [7].
Nonadherence to CPAP therapy is a major challenge in the management of OSA. Adherence rates have been estimated to range from 46 to 83 % when adherence is defined as CPAP use of at least 4 h per night [8]. Current recommendations to improve compliance with PAP include close follow-up, the utilization of heated humidification, and CPAP educational programs [6]. Device manufacturers and the medical community have approached the problem of CPAP nonadherence by developing alternate modes of delivering PAP (bi-level PAP, autotitrating PAP) and pressure waveform modification (C-Flex, Bi-Flex, expiratory pressure relief (PR)) . The remainder of this chapter discusses these differing modalities in an evidence-based manner in order to provide the practitioner a working knowledge of the current technology of PAP therapy.
Bi-level Positive Airway Pressure
The first description of bi-level PAP (BPAP) in 1990 [9] investigated the potential of providing differential pressures during inspiration and expiration with the hope of lowering positive pressure during the expiratory phase in order to improve comfort while still maintaining airway patency. Thirteen patients underwent a full night diagnostic PSG, a CPAP titration PSG, and BPAP titration PSG. BPAP was titrated based on the respiratory events: inspiratory PAP (IPAP) was increased for desaturation events while expiratory PAP (EPAP) was increased for apneic events. CPAP and BPAP were equally effective in resolving OSA. Final mean pressures were 14 cm H2O for CPAP and 14/8.9 cm H2O (IPAP/EPAP) for BPAP, confirming that despite a lower mean airway pressure, obstructive events were prevented. Some individuals required oxygen supplementation during the CPAP study, while the same individuals did not with BPAP study.
In randomized controlled trials evaluating CPAP versus BPAP in newly diagnosed patients with OSA, BPAP was not found to improve compliance with therapy. Reeves-Hoche and colleagues randomized patients with OSA (apnea-hypopnea index (AHI) ≥ 10 events/h) to 12 months of CPAP or BPAP therapy following in-laboratory PAP titration [10]. BPAP titration differed from the study by Sanders et al. in that CPAP was initially increased to resolve apneas followed by an independent increase in IPAP to eliminate hypopneas and snoring. There was no difference in the mean machine timer hours over the 12-month period. Of note, dropout was higher in the group randomized to CPAP. In a second study, 27 PAP naïve patients were randomized to CPAP or BPAP with Bi-Flex (Respironics) after separate titration nights with each device and followed for 1 month [11]. There were no observed differences in compliance, and the improvement in the ESS and the functional outcomes of sleep questionnaire (FOSQ) were similar between the groups. Because of these findings, BPAP is not recommended as a first-line PAP therapy for OSA, although it could be considered as an optional therapy in patients with CPAP intolerance due to high pressures [6]. The use of BPAP in patients with coexisting hypoventilation syndromes is not included in this review or in these recommendations.
Although PAP naïve OSA patients do not demonstrate improved usage patterns with BPAP when compared with CPAP use, failure of CPAP therapy, either during the titration study night or on follow-up after PAP has been used in the home, may be an indication to consider BPAP therapy. In a two-phase intervention trial of OSA patients with poor CPAP compliance, Ballard and colleagues demonstrated that compliance may be improved with BPAP therapy [12]. Of 204 patients with OSA, 24 % became compliant (≥ 4 h of nightly CPAP use) after phase 1 of the trial, which consisted of educational measures, mask adjustment or replacement, therapy for nasal symptoms, and initiation of heated humidification. If these measures failed to increase CPAP adherence , patients underwent a “split-night” titration trial with 4 h of CPAP and 4 h of Bi-Flex (BPAP with pressure modification, to be discussed later). The patients were then randomized to home CPAP or Bi-Flex therapy for 3 months. The Bi-Flex group demonstrated greater compliance (49 % vs. 28 %; p = 0.03) and a higher increase in mean FOSQ scores from baseline compared with CPAP treatment.
Based on these findings, routine administration of BPAP after a diagnosis of OSA does not improve treatment adherence and hence, cannot be recommended. However, if a patient demonstrates treatment noncompliance with CPAP despite behavioral and medical optimization (education, humidification, mask fitting, nasal steroids for rhinitis, etc.), second-line therapy, of which BPAP is an option, should be considered. The choice of which second-line modality (BPAP, oral appliance, surgery) to pursue depends on the patient characteristics and preferences. If BPAP therapy is pursued, a formal in-laboratory titration should be performed to ensure pressure optimization and improved patient comfort. Of note, differences in BPAP titration techniques and pressure modifications (Bi-Flex vs. BPAP without pressure modification) may result in variable outcomes and different rates of improvement in adherence.
Autotitrating Positive Airway Pressure
The purported utility of BPAP therapy for OSA was to decrease expiratory pressure, and therefore mean airway pressure, against which an individual must breathe, thereby increasing comfort with the device and subsequent improvement in compliance. Another strategy for improved compliance that was and is still being explored relies on varying the delivered pressure throughout sleep via device-specific algorithms, which fluctuates between higher and lower pressures to relieve flow limitation and obstruction, as changes in position and sleep stage may require. The characterization of flow limitation was a crucial first step in this process [13]. Condos and colleagues demonstrated that upper airways resistance is increased when the contour of the flow-time curve is flattened. Automated analysis of the flow-time curves could then be used to guide computer-generated adjustment of pressure in the setting of obstructive respiratory events. Current autotitrating positive airway pressure (APAP) technology relies on the determination of obstructive events characterized by flow limitation (flattening of the flow-time curve), apneas (no or markedly reduced flow over time), and snore (measured via vibration sensors). In addition, current devices use the forced oscillation technique (FOT) [14] to help determine whether reduction in flow is obstructive (i.e., non-patent airway) or nonobstructive. If events are obstructive, delivered pressure will be increased, while raising pressures during non-obstructive events (central apneas or hypopneas) can be avoided. The FOT is a measure of mechanical impedance of the respiratory system that is determined by applying high frequency, low amplitude pressure waves via the mask interface; patterns of FOT help determine if the airway is open (patent) or closed (obstructed) [15].
APAP and CPAP demonstrate equal efficacy in relieving obstructive respiratory events and improving daytime functional parameters. In the first randomized controlled trial of APAP versus CPAP, 16 patients with OSA were randomized to fixed CPAP with pressure determined from full PSG (Peff) or APAP (minimum pressure—(Peff − 2 cm H2O), maximum pressure—(Peff + 4 cm H2O)) [16]. Sleep and respiratory parameters were similar with CPAP and APAP therapy (AHI, total sleep time, sleep architecture). Following 3 weeks of PAP therapy, patients in both groups demonstrated equal improvement in ESS, MWT, and the trail making test (a test of cognitive impairment) compared with baseline; no differences between the groups were detected. Subjects randomized to APAP spent 49 % of the time requiring pressure below Peff, suggesting that APAP use at home may deliver pressures lower than that determined during a titration study for a significant portion of the night and thereby improve tolerance of PAP. Along these lines, another study of 15 patients with generally severe OSA demonstrated a positive correlation between the polysomnographically determined Peff and the time spent below Peff on APAP [17]; patients with more severe OSA may benefit to a greater extent with APAP due to spending a greater duration of the night at pressure levels below Peff.
Although there is some evidence that APAP improves compliance compared with fixed pressure CPAP, the evidence depends on the study type and the improvement is of questionable clinical importance. A Cochrane Collaboration review demonstrated a statistical improvement of 0.21 h of machine usage time in crossover studies comparing APAP to fixed CPAP [18]. Although statistically significant, an overall increase of 13 min per night is not likely to result in improvements in clinically meaningful outcomes. Crossover trials generally show equivalent residual AHI between APAP and fixed CPAP [19–23], equal improvement in ESS scores from baseline [19–21, 24–26], and a reduction in delivered pressure with APAP treatment [20, 22, 23]. Although there was a general patient preference for APAP treatment [21, 22], this was not a universal finding with some patients preferring fixed CPAP [20]. Similarly, improvement in machine usage was not a universal finding; among parallel studies or the first arm of crossover studies, a statistically significant difference in machine usage was not seen (mean increase in machine usage with APAP—0.22 h (− 0.05, 0.49; 95 % CI)) [18].
It is clear from the above discussion that APAP compared with CPAP therapy in an unselected patient population showed minimal to no improvement in treatment adherence and conflicting data on patient preference. However, several groups observed APAP treatment in patients with CPAP intolerance or those with high pressure variability to determine if these subgroups of OSA patients may benefit from APAP therapy. In one study, 27 patients with an AHI ≥ 20 and a high variability index, which was a calculated value based on the variability of pressures required during a 2-week run-in period on APAP, were randomized to 8 weeks of CPAP or APAP followed by crossover to the other treatment [27]. Machine usage time was not significantly different between the groups; however, mean pressure and ESS scores were lower in the APAP group and a greater number of participants chose APAP over CPAP when simply asked which device they preferred. Another study looked at a mixed population of patients in which CPAP was not the optimal treatment, as defined by patients with CPAP intolerance, CPAP requirements ≥ 12 cm H2O, or central respiratory events accounting for ≥ 10 % of events [22]. Patients were randomized in a crossover fashion to either BPAP or APAP for 6 weeks each. Both modalities significantly improved respiratory parameters (although mean residual AHI while on PAP in each group was > 5) and sleep quality. Patients again preferred APAP treatment as a long-term therapy for their sleep-disordered breathing . Although the heterogeneity of this study population prevents any firm conclusions, the search for subpopulations that may benefit from APAP therapy, as illustrated in these two studies, is an important strategy in improving patient’s acceptance of PAP therapy, thereby improving overall outcomes.
APAP devices rely on brand-specific proprietary algorithms that use a variety of methods for detecting respiratory events and adjust pressure settings differentially. An early trial evaluated devices guided by “flow limitation (APAPfl)” versus “FOT (APAPfot)” for determining the presence of respiratory events [28]. In a group of 30 patients with moderate to severe OSA (AHI ≥ 20 events per hour) treated with each device in a “split-night” setting (4 h/device), there was a trend towards lower AHI in the APAPfl group, higher overall pressure in the APAPfl group, and greater pressure variability in the APAPfot group. Although based on this study it is unclear which detection system is more accurate in identifying obstructive respiratory events, most current devices use a combination of flow limitation and forced oscillation in order to identify both obstructive and non-obstructive events. Several studies have compared devices produced by competing manufacturers [29, 30]. It is apparent from these studies that there is variability in delivered pressure and respiratory parameters between the various devices but the clinical significance is unclear.
Although the concept of APAP was well conceived in attempting to lower average positive pressure and improving patient compliance with PAP devices, the evidence does not support this. Overall usage of APAP was slightly increased when all studies are taken into account, although these results were highly dependent on the type of study and the patient population studied. In an attempt to combine other technology with APAP , two recent studies looked at APAP with expiratory PR (which will be discussed in the next section) to further improve patient comfort [31, 32]. When compared with fixed CPAP, APAP with expiratory PR (see the following section) was essentially equivalent with respect to sleep/respiratory parameters and outcomes. Consistent with prior studies, the patients in one study were satisfied with both regimens but preferred APAP treatment [32], while in the other study, patients were less satisfied and felt they derived less benefit with APAP therapy [31]. Without clear and convincing evidence supporting the superiority of APAP over CPAP, this treatment modality cannot be recommended at this time except on an individual basis.
Pressure Relief
Many device manufacturers have developed technologies to decrease applied positive pressure during the expiratory phase in order to improve compliance with the device by encouraging more physiologic transitions between inspiration and expiration. Brand-specific algorithms differ in the degree and timing of such Pressure Relief (PR) [33, 34]. The pressure decrement is either flow based (pressure drop proportional to patient’s flow amplitude) or prespecified (i.e., 1 cm H2O, 2 cm H2O or 3 cm H2O) . Likewise, the pressure decrement is either in the early portion of the expiratory phase (returning to set pressure prior to inhalation) or throughout the entire expiratory phase. PR may be utilized in most modes of PAP, including CPAP, APAP, and BPAP. Although when in CPAP or APAP mode PR appears to be very similar to a bi-level mode of ventilation, the main difference is that the pressure differential between IPAP and EPAP is usually lower than 3 cm H2O in PR mode and PR can be set in a stepwise manner (increase settings for more PR) as compared with the completely independently set IPAP and EPAP of BPAP therapy.
Similar to findings with APAP, there was no major difference in adherence when CPAP with PR was used compared with CPAP alone in clinical trials. This was confirmed in a systematic review [18] and meta-analysis [35]. Several randomized controlled trials comparing CPAP with PR versus standard CPAP demonstrated equal compliance between the two devices [36–41]. In one trial [41], low compliers, defined as those using standard CPAP for < 4 h per night, demonstrated improved compliance using CPAP with PR compared with standard CPAP. Another trial demonstrated improved compliance with CPAP with PR [42]; however, this trial was limited by non-blinded patients. In patients with severe OSA defined as AHI > 30/h or AHI 20–30/h with ESS > 12, there was a trend towards improved compliance (4.7 vs. 3.0 h per night, p = 0.15) in one study [39]. Overall, it is apparent that PR does not improve compliance with PAP therapy based on the current literature, although certain patient populations (low compliance, severe OSA) may achieve better compliance from this modality. Further research into these patient populations is needed.
PR did not improve subjective sleepiness scores (ESS and Stanford sleepiness scale (SSS)) when compared with standard CPAP [36, 37, 42]. Conversely, one study demonstrated improved ESS in patients treated with standard CPAP when compared with CPAP with PR [39]. When objective measures were assessed, studies found no differences in psychomotor vigilance testing (PVT) and modified MWT results between those randomized to CPAP with PR or standard CPAP [36, 39]. Although vigilance measures and objective sleepiness would not be expected to change if compliance was similar between the groups, Marshall et al found a trend towards increased compliance in the CPAP with PR group (4.7 vs. 3 h, p = 0.15) without improvement in PVT or modified MWT measures [39]. Despite a lack of benefit seen with PR technologies, patients frequently preferred this modality over fixed CPAP [37, 38].
Auto-Bi-level Positive Airway Pressure
The most recent foray into technologies to improve compliance and comfort with PAP devices is auto-BPAP. Similar to the situation with APAP , algorithms and device settings are different among different manufacturers. One manufacturer’s device analyzes the flow-time curve and adjusts pressure based on the presence of flow limitation, apnea events, and snoring events [43]. Clinical inputs include EPAP minimum, IPAP maximum, and pressure support (PS). The device initiates PAP at the minimum EPAP setting, with IPAP delivered at EPAP + PS. IPAP is then increased when respiratory events (flow limitation, apnea, snore) are detected, delivering an appropriate pressure to resolve the events, with EPAP now delivered at IPAP—PS. For example, if EPAPmin is set at 4 cm H2O and IPAPmax at 25 cm H2O with a PS of 4 cm H2O, the patient will initially receive an EPAP of 4 cm H2O and IPAP of 8 cm H2O. If obstructive respiratory events are detected and the device increases pressure to an IPAP of 18 cm H2O, EPAP will now be 14 cm H2O. Another manufacturer’s technology differs in that the device adjusts EPAP and IPAP independently, with increases in EPAP based on detection of apnea and snore events and changes in IPAP based on detection of hypopnea and respiratory effort-related arousal events [44]. Clinical inputs for the device with independently adjusted IPAP and EPAP are as follows: EPAPmin, IPAPmax, PSmin, and PSmax. PR technology is also available with both devices described above.
In the only trial of auto-BPAP versus standard CPAP in patients with moderate to severe OSA requiring PAP for the first time, 35 patients were randomized and evaluated after using their respective device after 12 weeks [45]. Sleep parameters and AHI were not significantly different between the groups. ESS and the Pittsburgh Sleep Quality Index were improved in both groups but not significantly different between groups. Likewise, compliance with therapy was not significantly different between the groups. The final pressures in each group were 9.5 cm H2O in the CPAP group and ~ 12/9 cm H2O in the auto-BPAP group.
Although there was no benefit regarding AHI, subjective sleepiness levels, or compliance in using auto-BPAP in PAP naïve patients with OSA, several investigators have observed the utility of this modality in patients noncompliant with CPAP, intolerant of CPAP, or failed CPAP titration. In an observational cohort study, patients noncompliant with CPAP (CPAP use < 4 h for ≥ 70 % of nights over the preceding 3 months) were initiated on auto-BPAP with PR and followed at 10 weeks [46]. Although the residual AHI was lower with auto-BPAP, both modalities (CPAP and auto-BPAP) resulted in AHI below five events per hour. Sleep parameters were not significantly different among devices. ESS and some domains of the FOSQ were improved with auto-BPAP. Most interesting, compliance was improved as compared with baseline and even more so in the subgroup of patients who initially required CPAP ≥ 10 cm H2O. In patients who failed CPAP use due to pressure intolerance, single night comparisons of standard BPAP versus auto-BPAP showed no significant differences in AHI or sleep parameters [47]. Finally, in a randomized controlled trial of 47 patients who initially failed CPAP titration (defined as sleep efficiency ≤ 70 %, ≥ 20 arousals per hour, aborted titration, or “persistent sleep disruption despite therapeutic CPAP therapy and low probability of CPAP compliance in the judgment of the reviewing physician”), patients were prescribed either CPAP or auto-BPAP with PR [48]. At 30 and 90 day follow-up, there were no significant differences in compliance, Epworth Sleepiness Scale (ESS) scores, Functional Outcomes of Sleep Questionnaire (FOSQ) scores. Although there may be a role for auto-BPAP, particularly in patients who are CPAP intolerant and require higher pressures, further studies are indicated.
Summary
The development of PAP as a therapy for OSA has provided patients with this disorder a noninvasive, effective treatment modality. CPAP remains the gold standard treatment among nocturnal PAP modalities. Due to poor compliance with standard CPAP therapy, technological innovation has resulted in the development of multiple devices that alter pressure delivery designed to improve patient comfort and subsequently patient compliance. This has not been demonstrated in clinical studies. BPAP did not show improved compliance in PAP naïve patients, although it may be beneficial in patients with CPAP noncompliance. APAP demonstrated a slight improvement in compliance, although the improvement was not clinically meaningful. PR technologies did not improve PAP compliance. Similarly, auto-BPAP did not improve compliance rates in PAP naïve patients, although this technology is in its infancy.
Interestingly, specific subgroups of patients may actually benefit from these new technologies, such as those intolerant to CPAP, patients with high pressure requirements, and patients who did not achieve satisfactory results on the initial titration studies. The identification of patient populations that will require these technologies will be a fruitful line of inquiry as we strive towards an effective therapy for all patients with OSA. Regardless of the deficiencies in the current literature, a logical stepwise approach to management of poorly compliant patients actively on CPAP therapy should be undertaken: (1) education, mask adjustment, treatment of nasal symptoms, and initiation of heated humidification, (2) initiation of PR (most standard CPAP devices have this capability), (3) trial of APAP therapy, (4) in-laboratory bi-level titration with initiation of BPAP if study results are adequate or initiation of auto-BPAP if titration is not optimal. Although not formally studied, this stepwise approach utilizes the spectrum of current technologies in a practical way to assist patients in their pursuit of an effective therapy.
References
Guilleminault C, et al. Obstructive sleep apnea syndrome and tracheostomy. Long-term follow-up experience. Arch Intern Med. 1981;141:985–8.
Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1:862–5.
Rapoport DM, Sorkin B, Garay SM, Goldring RM. Reversal of the “Pickwickian syndrome” by long-term use of nocturnal nasal-airway pressure. N Engl J Med. 1982;307:931–3. doi:10.1056/NEJM198210073071507.
Wagner DR, Pollak CP, Weitzman ED. Nocturnal nasal-airway pressure for sleep apnea. N Engl J Med. 1983;308:461–2.
Giles TL, et al. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;(1):CD001106, doi:10.1002/14651858.CD001106.pub3.
Kushida CA, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80.
Basner RC. Continuous positive airway pressure for obstructive sleep apnea. N Engl J Med. 2007;356:1751–8. doi:10.1056/NEJMct066953.
Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi:10.1513/pats.200708-119MG.
Sanders MH, Kern N. Obstructive sleep apnea treated by independently adjusted inspiratory and expiratory positive airway pressures via nasal mask. Physiologic and clinical implications. Chest. 1990;98:317–24.
Reeves-Hoche MK, et al. Continuous versus bilevel positive airway pressure for obstructive sleep apnea. Am J Respir Crit Care Med. 1995;151:443–9. doi:10.1164/ajrccm.151.2.7842204.
Gay PC, Herold DL, Olson EJ. A randomized, double-blind clinical trial comparing continuous positive airway pressure with a novel bilevel pressure system for treatment of obstructive sleep apnea syndrome. Sleep. 2003;26:864–9.
Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med: JCSM. 2007;3:706–12.
Condos R, et al. Flow limitation as a noninvasive assessment of residual upper-airway resistance during continuous positive airway pressure therapy of obstructive sleep apnea. Am J Respir Crit Care Med. 1994;150:475–80. doi:10.1164/ajrccm.150.2.8049832.
Dubois AB, Brody AW, Lewis DH, Burgess BF Jr. Oscillation mechanics of lungs and chest in man. J Appl Physiol. 1956;8:587–94.
Farre R, Montserrat JM, Navajas D. Assessment of upper airway mechanics during sleep. Respir Physiol Neurobiol. 2008;163:74–81. doi:10.1016/j.resp.2008.06.017.
Meurice JC, Marc I, Series F. Efficacy of auto-CPAP in the treatment of obstructive sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1996;153:794–8. doi:10.1164/ajrccm.153.2.8564134.
Boudewyns A, et al. Two months follow up of auto-CPAP treatment in patients with obstructive sleep apnoea. Thorax. 1999;54:147–9.
Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2009:CD003531, doi:10.1002/14651858.CD003531.pub3.
Galetke W, Anduleit N, Richter K, Stieglitz S, Randerath WJ. Comparison of automatic and continuous positive airway pressure in a night-by-night analysis: a randomized, crossover study. Respiration. 2008;75:163–9. doi:10.1159/000097767.
Hussain SF, Love L, Burt H, Fleetham JA. A randomized trial of auto-titrating CPAP and fixed CPAP in the treatment of obstructive sleep apnea-hypopnea. Respir Med. 2004;98:330–3.
Nussbaumer Y, Bloch KE, Genser T, Thurnheer R. Equivalence of autoadjusted and constant continuous positive airway pressure in home treatment of sleep apnea. Chest. 2006;129:638–43. doi:10.1378/chest.129.3.638.
Randerath WJ, Galetke W, Ruhle KH. Auto-adjusting CPAP based on impedance versus bilevel pressure in difficult-to-treat sleep apnea syndrome: a prospective randomized crossover study. Med Sci Monit. 2003;9:CR353–C358.
Teschler H, Wessendorf TE, Farhat AA, Konietzko N, Berthon-Jones M. Two months auto-adjusting versus conventional nCPAP for obstructive sleep apnoea syndrome. Eur Respir J. 2000;15:990–5.
d’Ortho MP, et al. Constant vs. automatic continuous positive airway pressure therapy: home evaluation. Chest. 2000;118:1010–7.
Hudgel DW, Fung C. A long-term randomized, cross-over comparison of auto-titrating and standard nasal continuous airway pressure. Sleep. 2000;23:645–8.
Hukins C. Comparative study of autotitrating and fixed-pressure CPAP in the home: a randomized, single-blind crossover trial. Sleep. 2004;27:1512–7.
Noseda A, et al. Constant vs auto-continuous positive airway pressure in patients with sleep apnea hypopnea syndrome and a high variability in pressure requirement. Chest. 2004;126:31–7. doi:10.1378/chest.126.1.31.
Pevernagie DA, et al. Efficacy of flow- vs impedance-guided autoadjustable continuous positive airway pressure: a randomized cross-over trial. Chest. 2004;126:25–30. doi:10.1378/chest.126.1.25.
Hertegonne KB, Rombaut B, Houtmeyers P, Van Maele G, Pevernagie DA. Titration efficacy of two auto-adjustable continuous positive airway pressure devices using different flow limitation-based algorithms. Respiration. 2008;75:48–54. doi:10.1159/000103515.
McCoy R, Diesem R. 1–15 (ResMed) ResMed white paper, A Bench Comparison of Three Auto-Adjusting Positive Airway Pressure Devices: Response to Apnea, Hypopnea, Flow Limitation and Simulated Snore Robert McCoy BS RRT FAARCRyan Diesem BAValley Inspired Products Inc. 18 March 2011.
Kushida CA, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34:1083–92. doi:10.5665/SLEEP.1166.
Mulgrew AT, Cheema R, Fleetham J, Ryan CF, Ayas NT. Efficacy and patient satisfaction with autoadjusting CPAP with variable expiratory pressure vs standard CPAP: a two-night randomized crossover trial. Sleep Breath = Schlaf & Atmung. 2007;11:31–7, doi:10.1007/s11325-006-0078-6.
ResMed (personal communication, ResMed technical support staff).
Respironics. http://flexfamily.respironics.com/.
Bakker JP, Marshall NS. Flexible pressure delivery modification of continuous positive airway pressure for obstructive sleep apnea does not improve compliance with therapy: systematic review and meta-analysis. Chest. 2011;139:1322–30. doi:10.1378/chest.10-2379.
Bakker J, Campbell A, Neill A. Randomized controlled trial comparing flexible and continuous positive airway pressure delivery: effects on compliance, objective and subjective sleepiness and vigilance. Sleep. 2010;33:523–9.
Dolan DC, et al. Longitudinal comparison study of pressure relief (C-Flex) vs. CPAP in OSA patients. Sleep Breath = Schlaf & Atmung. 2009;13:73–7, doi:10.1007/s11325-008-0199-1.
Leidag M, Hader C, Keller T, Meyer Y, Rasche K. Mask leakage in continuous positive airway pressure and C-Flex. J Physiol Pharmacol. 2008;59(Suppl 6):401–6.
Marshall NS, Neill AM, Campbell AJ. Randomised trial of compliance with flexible (C-Flex) and standard continuous positive airway pressure for severe obstructive sleep apnea. Sleep Breath = Schlaf & Atmung. 2008;12:393–6, doi:10.1007/s11325-008-0189-3.
Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130:1018–24. doi:10.1378/chest.130.4.1018.
Pepin JL, et al. Pressure reduction during exhalation in sleep apnea patients treated by continuous positive airway pressure. Chest. 2009;136:490–7. doi:10.1378/chest.08-2646.
Aloia MS, Stanchina M, Arnedt JT, Malhotra A, Millman RP. Treatment adherence and outcomes in flexible vs standard continuous positive airway pressure therapy. Chest. 2005;127:2085–93. doi:10.1378/chest.127.6.2085.
ResMed (personal communication, ResMed technical support staff).
Rush, K (personal communication).
Blau A, et al. Auto bi-level pressure relief-PAP is as effective as CPAP in OSA patients—a pilot study. Sleep Breath = Schlaf & Atmung. 2012;16;773–9, doi:10.1007/s11325-011-0574-1.
Gentina T, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy–a pilot study. Sleep Breath = Schlaf Atmung. 2011;15:21–7. doi:10.1007/s11325-009-0322-y.
Ball N, Gordon N, Casal E, Parish J. Evaluation of auto bi-level algorithm to treat pressure intolerance in obstructive sleep apnea. Sleep Breath = Schlaf & Atmung. 2011;15:301–9, doi:10.1007/s11325-010-0381-0.
Powell ED, Gay PC, Ojile JM, Litinski M, Malhotra A. A pilot study assessing adherence to auto-bilevel following a poor initial encounter with CPAP. J Clin Sleep Med: JCSM. 2012;8:43–7, doi:10.5664/jcsm.1658.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Weingarten, J. (2015). Use of nNIV in Obstructive Sleep Apnea: Modes, Flexes, and More. In: Basner, R., Parthasarathy, S. (eds) Nocturnal Non-Invasive Ventilation. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7624-6_9
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7624-6_9
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7623-9
Online ISBN: 978-1-4899-7624-6
eBook Packages: MedicineMedicine (R0)