Abstract
Purpose
Obstructive sleep apnea syndrome (OSAS) is a common chronic disorder associated with hypoxia and endothelial and vascular dysfunction. Many studies have analyzed choroidal thickness measurements in patients with different severities of OSAS versus normal subjects by optical coherence tomography (OCT), but the results have been inconsistent. Therefore, a meta-analysis was performed to evaluate the choroidal thickness changes in OSAS measured by OCT.
Methods
Pertinent studies were retrieved by a comprehensive search of PubMed, Embase, Web of Science, and the Cochrane Library from inception to August 2015. For continuous outcomes, the weighted mean difference (WMD) and 95 % confidence interval (CI) were calculated by using a random effects model.
Results
Seven case-control studies were included in the final meta-analysis, containing a total of 784 eyes (558 in the OSAS group and 226 in normal controls). The results showed that subfoveal choroidal thickness (SFCT) was significantly reduced compared with normal controls, with pooled WMD −8.06 (95 % CI −15.72 to −0.41) for mild OSAS, −29.99 (95 % CI −52.40 to −7.58) for moderate OSAS, and −53.72 (95 % CI −88.95 to −18.48) for severe OSAS. Choroidal thickness at 1 mm temporal to the fovea and at 1 mm nasal to the fovea were also significantly lower than those in the normal controls (WMD = −28.94, 95 % CI −43.78 to −14.10 and WMD = −20.90, 95 % CI −36.62 to −5.18).
Conclusion
This meta-analysis suggests that choroidal thickness was reduced in OSAS. Considering the non-invasive nature of OCT, OCT could be a useful tool for grading the severity of OSAS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is a common chronic disorder characterized by repeated upper airway obstruction during sleep, causing periods of sympathetic activation, hypoxia, and hypercapnia. OSAS has been shown to be accompanied by a number of eye disorders, such as glaucoma (5.9–57 %) [1, 2], non-arteritic ischemic optic neuropathy (NAION, 28–71 %) [3–5], and floppy eyelid syndrome (20–32.6 %) [6]. Additionally, hypoxia may affect the endothelium and vascular resistance and further cause structural alterations of the choroid. The choroid is a highly vascularized tissue extending from the margins of the optic nerve head to the ora serrata. It plays an important role in the physiology of the eye. Nearly 90 % of the ophthalmic artery blood flow is distributed to the choroid. Besides providing oxygen and nutrients to the outer retina, the choroid regulates temperature and removes waste products from the retina [7]. It is also involved in aqueous circulation and ocular growth. Abnormal structure or function of the choroid is related to a variety of ocular and systemic diseases.
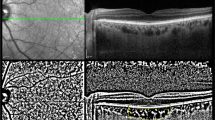
Optical coherence tomography (OCT) is a non-invasive, cross-sectional imaging method that is commonly used for retinal imaging. The newer OCT techniques have higher resolution, deeper tissue penetration, and faster acquisition speed. The emergence of enhanced depth imaging (EDI) with spectral domain OCT, polarization-sensitive OCT, and swept-source OCT enables better visualization of the choroid and evaluation of choroidal thickness in vivo. These possibilities have triggered a considerable scientific interest in the choroidal thickness in ocular and systemic diseases. Investigations focused on glaucoma and NAION have revealed reduction of choroidal thickness [8, 9].
Recently, several studies have reported measurements of the choroidal thickness with OCT in OSAS patients and normal controls. Some previous publications [10–13] reported that OSAS patients had abnormal choroidal structure alteration, while others [14, 15] did not. Results have been inconsistent and some studies are less convincing because of a small sample size. Therefore, a meta-analysis is useful to determine whether choroidal thickness (CT) is reduced in OSAS patients.
The aims of this study were to perform a meta-analysis and systemically evaluate CT measurements with OCT in a series of OSAS patients and in the normal control groups.
Materials and methods
This meta-analysis was performed according to the Cochrane Collaboration recommendations [16]. The results were reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [17] .
Search strategy
Pertinent studies were retrieved by a systemic search of PubMed, Embase, Web of Science, and the Cochrane Library from inception to August 28, 2015. The search strategy was constructed using the following terms: obstructive sleep apnea syndrome, OSAS, choroidal thickness, and choroid. No language was restricted. Furthermore, references of reviews and identified studies were screened for potentially relevant studies.
Study selection
The following inclusion criteria were adopted in the present meta-analysis: (1) case-control or cross-sectional studies; (2) OSAS was diagnosed with international diagnostic criteria and graded according to apnea-hypopnea index (AHI). Patients with OSAS were divided into mild (5–15 events per hour), moderate (15–30), and severe (≥30); (3) patients with OSAS were compared with normal controls; (4) choroidal thickness in all subjects were obtained by OCT; (5) studies provided data of choroidal thickness of both OSAS patients and normal controls; (6) at least one of the following outcomes was used: subfoveal choroidal thickness (SFCT), choroidal thickness at 1 mm temporal to the fovea (T1), and choroidal thickness at 1 mm nasal to the fovea (N1). Exclusion criteria included the following: (1) studies without normal controls; (2) abstracts from conferences, case reports, comments, or reviews; (3) data were not retrievable; and (4) duplicate articles. In studies of the same population, only the latest or the most complete studies were included. The screening processes were performed independently by two reviewers, and discrepancies were settled by discussion.
Data extraction
Two reviewers extracted the necessary information from the eligible studies by using a standardized form. Extracted data included the following: first author, year of publication, location, OCT type, mean age, sex, sample size, body mass index (BMI), systemic diseases, AHI, spherical equivalent, axial length, intraocular pressure (IOP), the matched or adjusting factors, and choroidal thickness parameters. Discrepancies between the reviewers’ results were resolved by discussion, and a third independent reviewer was requested when there was a discrepancy noted.
Quality assessment
The methodological quality of included studies was assessed by two reviewers based on guidance in Cochrane Handbook for Systematic Reviews of Interventions [16]. It recommends the Newcastle-Ottawa Scale (NOS) system for grading the quality of case-control studies in meta-analysis. The NOS evaluates three dimensions (selection, comparability, and exposure), and the maximum scores were 4 for selection, 2 for comparability, and 3 for outcome or exposure. The overall NOS score was 9, and studies with ≥6 were regarded as having adequate quality.
Statistical analysis
The weighted mean differences (WMDs) were used for comparisons of choroidal thickness between OSAS patients and normal controls. In the present study, all summary estimates and their 95 % confidence interval (CI) were pooled by using the random effects model to obtain more conservative conclusions. Statistical heterogeneity between studies was quantified with χ 2 test and I 2 statistics. For the χ 2 test, a P value <0.10 indicates significant heterogeneity; for the I 2 statistics, values of 25, 50, and 75 % represent mild, moderate, and severe heterogeneity, respectively [18]. Sensitivity analyses were performed by assessing the influences of individual studies on the pooled results. Funnel plots and Egger’s test were used to evaluate potential publication bias. All statistical analyses were performed by Stata SE 12.0 (StataCorp, College Station, TX), and the level of significance was set at 0.05, two sided, except when otherwise specified.
Results
Eligible studies
Figure 1 shows the process of study selection. The search strategy initially identified 32 articles. Eleven reports were duplicate studies and removed. After title and abstract screening, seven reports were excluded because they did not study OSAS patients, and six did not evaluate choroidal thickness. After review of full texts, one report was excluded because the report was a letter [19]. Ultimately, seven eligible studies were included in the final meta-analysis [10–15, 20].
Characteristics and quality of studies
All studies were case-control design including a total of 784 eyes (558 in the OSAS group and 226 in normal controls). Six studies [11–15, 20] were conducted in Turkey and one in China [10]. The mean age ranged from 42.3 to 58.6 years. Among the seven studies, six studies matched confounding factors in control subjects with OSAS patients: age, sex, and BMI were matched in four studies [11, 13, 15, 19]; age and IOP were matched in one study [12], and age and spherical equivalent (SE) were matched in another study [10]. Table 1 summarizes the main characteristics of the studies included. There were no significant differences in age, sex distribution, BMI, SE, axial length (AL), or IOP between patients with various degree of OSAS and normal controls. All studies set a strict inclusion and exclusion criteria, and patients with any systemic disease (such as hypertension, diabetes) that potentially affects CT were excluded. The inclusion and exclusion criteria of the included studies are summarized in Table 2. All studies had NOS scores ≥6 and the mean score was 7.3 (range 7 to 9), indicating the methodological quality was generally good.
Data synthesis and meta-analysis
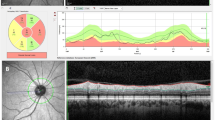
The meta-analysis of the SFCT comparison between OSAS patients and normal controls is depicted in Fig. 2. No significant heterogeneity was detected across articles comparing mild OSAS and controls (P = 0.845, I 2 = 0 %). The results showed that SFCT was reduced significantly compared with normal controls, with a pooled WMD of −8.06 (95 % CI −15.72 to −0.41) for mild OSAS, −29.99 (95 % CI −52.40 to −7.58) for moderate OSAS, and −53.72 (95 % CI −88.95 to −18.48) for severe OSAS. The SFCT reduction was more apparent as OSAS becomes more severe.
Three studies evaluated choroidal thickness at N1 between OSAS patients and normal controls. The meta-analysis of these data showed that there was no significant difference of N1 between mild OSAS and normal controls (WMD = −3.15, 95 % CI −17.58 to 11.28, P = 0.669). However, N1 in moderate OSAS (WMD = −19.13, 95 % CI −32.46 to −5.81, P = 0.005) and severe OSAS (WMD = −28.94, 95 % CI −43.78 to −14.10, P < 0.001) were significantly lower than the controls. The detailed results are presented in Fig. 3.
Analysis of T1 in three studies revealed mild between-study heterogeneity. There were no statistically significant differences in T1 between the patients with mild OSAS (WMD = 0.88, 95 % CI −14.51 to 16.27, P = 0.911) and moderate OSAS (WMD = −12.34, 95 % CI −26.00 to 1.32, P = 0.077) in comparison with controls. The detailed results are presented in Fig. 4.
Of the seven studies, two used Spectralis OCT (Heidelberg Engineering Inc.), three used RTVue-100 OCT (Optovue Inc.), and two used Topcan 3D-OCT 2000 (Topcon Inc.). Subgroup analyses according to the type of OCT were performed; the results showed that SFCT was thinner in patients with OSAS than in controls regardless of the type of OCT.
Five studies reported the relationship between choroidal thickness and AHI bivariate correlation analysis (Table 3). Only one study did not detect significant correlations between CT and AHI. Four studies (4/5) demonstrated a negative correlation between CT and AHI, which is consistent with the observation that CT was significantly decreased in OSAS patients compared with the normal controls.
Sensitivity analysis and publication bias
To further test the stability and reliability of our results, a sensitivity analysis was performed by sequentially excluding individual studies. Statistically similar results were obtained after omitting each single study, suggesting our primary results were robust. Funnel plots of SFCT were created to evaluate the potential publication bias, and the data points showed mild asymmetry, suggesting a publication bias (Fig. 5). In addition, Egger’s tests confirmed evidence of publication bias (P = 0.022 for mild OSAS vs control, P = 0.058 for moderate OSAS vs control, P = 0.038 for severe OSAS vs control).
Discussion
With the availability of EDI-OCT, we can image choroid non-invasively and precisely. Recent studies have demonstrated that CT measurements by OCT are highly reproducible and repeatable and have a very small range of variability [21–24]. Additionally, CT measurements obtained with different OCTs were highly correlated and could be used interchangeably [24]. It was suggested that variations in CT may indicate the presence of a disease, signal its progression, or provide insights into its prognosis. For example, CT was reported to decrease in NAION, glaucoma, and retinal vein occlusion, while it increased in carotid cavernous fistula, migraine, and central serous chorioretinopathy [25]. However, whether or not alternation of CT occurs in OSAS remains a subject of debate.
With the accumulation of a number of OCT studies, there is an opportunity to analyze the available data to resolve persistent clinical questions [18]. Based upon the published data from seven studies, our meta-analysis investigated how CT changed in different stages of OSAS. Our meta-analysis confirmed that CT changes can be detected using OCT in patients with OSAS. The pooled results demonstrated a significant reduction in SFCT in mild, moderate, and severe OSAS patients compared with normal controls. Further analysis in location at N1/T1 provided evidence that CT in severe or moderate OSAS was thinner than that in controls, while CT in mild OSAS was similar to that in controls. Thus, reduced CT could be an ocular marker of the severity of OSAS.
Reduction of CT in OSAS is biologically reasonable, though an exact mechanism remains unclear. It has been speculated that CT may be an indirect biomarker of choroidal circulation. The smooth muscles of the choroid vessel walls are innervated by sympathetic and parasympathetic nerves. Choroidal blood flow has been shown to have a capacity to autoregulate in order to maintain adequate oxygen saturation. Sogawa et al. [26] suggested that there were no significant correlations between the SFCT and the choroidal blood flow in healthy young subjects. But, Okamoto et al. [27] demonstrated that the reduction of SFCT after intravitreal bevacizumab injection in the eyes with central serous chorioretinopathy was caused by the reduction of choroidal blood flow. And several studies [28–30] have found that sildenafil citrate increases CT because of increased choroidal blood flow. Analysis of Doppler ultrasound variables and SFCT revealed an association between SFCT and internal carotid artery diameter and resistance index [31]. In OSAS, intermittent airway obstruction causes hypoxia and decreases the mean saturation of oxygen. Recurrent hypoxia and reperfusion episodes can lead to oxidative stress and inflammation, damage the vascular endothelium, decrease responsiveness to vasodilator agents, and activate the sympathetic system [32]. These serious conditions lead to vascular dysregulation, altered choroidal blood flow, and consequently reduced CT.
In this study, we did not find significant differences in T1/N1 between mild OSAS and controls. This may be explained by the autoregulation mechanism of the choroid. The sympathetic and parasympathetic fibers terminating on the choroid may remain balanced in some patients with mild OSAS. These results were consistent with the findings by Khayi et al. [33] that the regulation of choroidal blood flow was unaltered in men with OSAS who have no comorbidities. Tonini et al. [34] also reported that choroidal vascular reactivity to hyperoxia and hypercapnia in OSAS was similar to that in healthy subjects. The results of our study suggest that the choroidal blood flow is preserved in mild OSAS. On the other hand, patients with moderate or severe OSAS may have dominant sympathetic activity and decreased choroidal blood flow. More studies evaluating CT and choroidal blood flow in OSAS patients may be required to confirm this theory.
Difficulties in the meta-analysis are the heterogeneity of the existing studies and confounders. An important confounder in OCT measurement includes co-existing ocular conditions such as refractive error and glaucoma. Refractive error contributes to different retinal nerve fiber layer thickness and CT. The differences in IOP and SE between OSAS and controls were not statistically significant in four of seven studies, and the pooled measurements were similar when the combined data was restricted to these four studies. Hence, the results would not be biased by the IOP or SE. However, the potential effect of other confounding factors may have been present, as it is uncertain whether or not eyes with NAION, CCF, migraine, or retinal vein occlusion were truly excluded by these studies.
This meta-analysis has some limitations. First, CTs in the included studies were all obtained manually, a fact which may have introduced measurement bias. Although this is still the most commonly used method for determining CT, automated software will be required to obtain a more objective evaluation [35]. Second, the reported changes in CT as measured by the EDI-OCT are assumed to be generalized. It is possible that this might not be the case and that segmental changes in CT occurred and were overlooked. Third, this meta-analysis included studies published in indexed journals. We did not search for unpublished studies or original data. The funnel plot for publication bias was indeed significant, although this result may also indicate small-study effects. Further study may be warranted to analyze this. Fourth, OSAS duration, which has been shown to affect vascular autoregulation, may influence CT. Unfortunately, a subgroup analysis for this was unavailable because of lack of data. Finally, the included studies were performed in Turkey or China. The results of this study may not be generalizable to other populations. More studies with larger sample sizes and various ethnicities are needed.
In conclusion, the present meta-analysis showed that CT was significantly decreased in OSAS patients compared with the normal controls. The tendency of reduction of CT in severe OSAS was more obvious. OCT could be a useful tool for grading the severity of OSAS. These findings may be helpful for explaining the pathogenesis of OSAS and the mechanisms connecting OSAS and ocular diseases.
References
Quintyn JC (2013) Evaluation of the visual function in obstructive sleep apnea syndrome patients and normal-tension glaucoma by means of the multifocal visual evoked potentials. Graefes Arch Clin Exp Ophthalmol 251:1457
Sergi M, Salerno DE, Rizzi M, Blini M, Andreoli A, Messenio D, Pecis M, Bertoni G (2007) Prevalence of normal tension glaucoma in obstructive sleep apnea syndrome patients. J Glaucoma 16:42–46
Bilgin G, Koban Y, Arnold AC (2013) Nonarteritic anterior ischemic optic neuropathy and obstructive sleep apnea. J Neuroophthalmol 33:232–234
Palombi K, Renard E, Levy P, Chiquet C, Deschaux C, Romanet JP, Pepin JL (2006) Non-arteritic anterior ischaemic optic neuropathy is nearly systematically associated with obstructive sleep apnoea. Br J Ophthalmol 90:879–882
Arda H, Birer S, Aksu M, Ismailogullari S, Karakucuk S, Mirza E, Gumus K, Oner A (2013) Obstructive sleep apnoea prevalence in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 97:206–209
Muniesa M, Sanchez-de-la-Torre M, Huerva V, Lumbierres M, Barbe F (2014) Floppy eyelid syndrome as an indicator of the presence of glaucoma in patients with obstructive sleep apnea. J Glaucoma 23:e81–e85
Nickla DL, Wallman J (2010) The multifunctional choroid. Prog Retin Eye Res 29:144–168
Usui S, Ikuno Y, Miki A, Matsushita K, Yasuno Y, Nishida K (2012) Evaluation of the choroidal thickness using high-penetration optical coherence tomography with long wavelength in highly myopic normal-tension glaucoma. Am J Ophthalmol 153:10–16
Schuster AK, Steinmetz P, Forster TM, Schlichtenbrede FC, Harder BC, Jonas JB (2014) Choroidal thickness in nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 158:1342–1347
Xin C, Wang J, Zhang W, Wang L, Peng X (2014) Retinal and choroidal thickness evaluation by SD-OCT in adults with obstructive sleep apnea-hypopnea syndrome (OSAS). Eye (Lond) 28:415–421
Ekinci M, Huseyinoglu N, Cagatay HH, Keles S, Ceylan E, Gokce G (2014) Choroidal thickening in patients with sleep apnea syndrome. Neuro-Ophthalmology 38:8–13
Kara S, Ozcimen M, Bekci TT, Sakarya Y, Gencer B, Tufan HA, Arikan S (2014) Evaluation of choroidal thickness in patients with obstructive sleep apnea/hypopnea syndrome. Arq Bras Oftalmol 77:280–284
Karalezli A, Eroglu FC, Kivanc T, Dogan R (2014) Evaluation of choroidal thickness using spectral-domain optical coherence tomography in patients with severe obstructive sleep apnea syndrome: a comparative study. Int J Ophthalmol 7:1030–1034
Karaca EE, Ekici F, Yalcin NG, Ciftci TU, Ozdek S (2014) Macular choroidal thickness measurements in patients with obstructive sleep apnea syndrome. Sleep Breath 19:335–341
Zengin MO, Oz T, Baysak A, Cinar E, Kucukerdonmez C (2014) Changes in choroidal thickness in patients with obstructive sleep apnea syndrome. Ophthalmic Surg Lasers Imaging Retina 45:298–304
Higgins JP, Green S (2011) Cochrane Handbook for systematic reviews of interventions. Version 5.1.0 [updated March, 2011], Available from:www.cochrane-handbook.org; 2011. edn: The Cochrane Collaboration
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Wang W, Zhang X (2014) Choroidal thickness and primary open-angle glaucoma: a cross-sectional study and meta-analysis. Invest Ophthalmol Vis Sci 55:6007–6014
Bayhan HA, Aslan BS (2014) Choroidal thickness alterations in obstructive sleep apnea-hypopnea syndrome (OSAS). Eye (Lond) 28:1387
Bayhan HA, Bayhan SA, Intepe YS, Muhafiz E, Gurdal C (2015) Evaluation of the macular choroidal thickness using spectral optical coherence tomography in patients with obstructive sleep apnea syndrome. Clin Experiment Ophthalmol 43:139–144. doi:10.1111/ceo.12631
Shao L, Xu L, Chen CX, Yang LH, Du KF, Wang S, Zhou JQ, Wang YX, You QS, Jonas JB et al (2013) Reproducibility of subfoveal choroidal thickness measurements with enhanced depth imaging by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 54:230–233
Matsuo Y, Sakamoto T, Yamashita T, Tomita M, Shirasawa M, Terasaki H (2013) Comparisons of choroidal thickness of normal eyes obtained by two different spectral-domain OCT instruments and one swept-source OCT instrument. Invest Ophthalmol Vis Sci 54:7630–7636
Chhablani J, Barteselli G, Wang H, El-Emam S, Kozak I, Doede AL, Bartsch DU, Cheng L, Freeman WR (2012) Repeatability and reproducibility of manual choroidal volume measurements using enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci 53:2274–2280
Yamashita T, Yamashita T, Shirasawa M, Arimura N, Terasaki H, Sakamoto T (2012) Repeatability and reproducibility of subfoveal choroidal thickness in normal eyes of Japanese using different SD-OCT devices. Invest Ophthalmol Vis Sci 53:1102–1107
Laviers H, Zambarakji H (2014) Enhanced depth imaging-OCT of the choroid: a review of the current literature. Graefes Arch Clin Exp Ophthalmol 252:1871–1883
Sogawa K, Nagaoka T, Takahashi A, Tanano I, Tani T, Ishibazawa A, Yoshida A (2012) Relationship between choroidal thickness and choroidal circulation in healthy young subjects. Am J Ophthalmol 153:1129–1132
Okamoto M, Matsuura T, Ogata N (2015) Choroidal thickness and choroidal blood flow after intravitreal bevacizumab injection in eyes with central serous chorioretinopathy. Ophthalmic Surg Lasers Imaging Retina 46:25–32
Kim DY, Silverman RH, Chan RV, Khanifar AA, Rondeau M, Lloyd H, Schlegel P, Coleman DJ (2013) Measurement of choroidal perfusion and thickness following systemic sildenafil (Viagra((R))). Acta Ophthalmol 91:183–188
Orefice JL, Costa RA, Scott IU, Calucci D, Orefice F (2013) Spectral optical coherence tomography findings in patients with ocular toxoplasmosis and active satellite lesions (MINAS Report 1). Acta Ophthalmol 91:e41–e47
Vance SK, Imamura Y, Freund KB (2011) The effects of sildenafil citrate on choroidal thickness as determined by enhanced depth imaging optical coherence tomography. Retina 31:332–335
Agladioglu K, Pekel G, Citisli V, Yagci R (2015) Choroidal thickness and retinal vascular caliber correlations with internal carotid artery Doppler variables. J Clin Ultrasound 43(9):567–572
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Khayi H, Pepin JL, Geiser MH, Tonini M, Tamisier R, Renard E, Baguet JP, Levy P, Romanet JP, Chiquet C (2011) Choroidal blood flow regulation after posture change or isometric exercise in men with obstructive sleep apnea syndrome. Invest Ophthalmol Vis Sci 52:9489–9496
Tonini M, Khayi H, Pepin JL, Renard E, Baguet JP, Levy P, Romanet JP, Geiser MH, Chiquet C (2010) Choroidal blood-flow responses to hyperoxia and hypercapnia in men with obstructive sleep apnea. Sleep 33:811–818
Wang W, Zhou M, Huang W, Chen S, Ding X, Zhang X (2013) Does acute primary angle-closure cause an increased choroidal thickness? Invest Ophthalmol Vis Sci 54:3538–3545
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This is a meta-analysis; thus, requirements of ethics statement and consent statement are not needed.
Funding
The Chinese government provided financial support in the form of a grant from the National Natural Science Foundation of China (81570843).
The sponsor had no role in the design or conduct of this research.
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
This is a meta-analysis which does not involve human subjects; thus, the requirement of informed consent is not needed.
Rights and permissions
About this article
Cite this article
He, M., Han, X., Wu, H. et al. Choroidal thickness changes in obstructive sleep apnea syndrome: a systematic review and meta-analysis. Sleep Breath 20, 369–378 (2016). https://doi.org/10.1007/s11325-015-1306-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1306-8