Abstract
Our aim was to study the association of two potential serum biomarkers glial fibrillary acidic protein (GFAP) and epidermal growth factor receptor (EGFR) with prognostic markers such as IDH1 mutation, tumor burden, and survival in patients with high-grade gliomas (HGG). Additionally, our objective was to evaluate the potential of serum EGFR as a surrogate marker for EGFR status in the tumor. Pre-operative serum samples were prospectively collected from patients with primary (n = 17) or recurrent (n = 10) HGG. Serum GFAP and EGFR levels were determined by ELISA and studied for correlation with molecular markers including EGFR amplification, tumor volume in contrast-enhanced T1-weighted MRI, and progression-free survival (PFS). Pre-operative serum GFAP level of ≥0.014 ng/ml was 86 % sensitive and 85 % specific for the diagnosis of glioblastoma. High GFAP was related to the lack of IDH1 mutation (P = 0.016), high Ki67 proliferation index (P < 0.001), and poor PFS (HR 5.9, CI 1.2–29.9, P = 0.032). Serum GFAP correlated with enhancing tumor volume in primary (r = 0.64 P = 0.005), but also in recurrent HGGs (r = 0.76 P = 0.011). In contrast, serum EGFR levels did not differ between HGG patients and 13 healthy controls, and were not related to EGFR status in the tumor. We conclude that high serum GFAP associates with IDH1 mutation-negative HGG, and poor PFS. Correlation with tumor burden in recurrent HGG implicates the potential of serum GFAP for detection of tumor recurrence. Our results suggest that circulating EGFR is not derived from glioma cells and cannot be used as a marker for EGFR status in the tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-grade gliomas (HGGs, WHO grade III and IV) are aggressive brain tumors, which have a persistently dismal prognosis [1]. The gold standard for diagnosing HGG is histologic evaluation of tumor biopsy. However, inadequate amount of tissue or inherent sampling errors may limit its value [2]. Furthermore, assessing tumor progression with contrast enhanced magnetic resonance imaging (MRI) may be complicated by treatment-related changes such as pseudoprogression or pseudoresponse [3]. A readily achievable blood-based biomarker with diagnostic and prognostic value could bypass these limitations and provide complementary data in clinical decision-making [4].
Glial fibrillary acidic protein (GFAP) is an intermediate filament expressed almost exclusively in astrocytes where it acts as a member of the cytoskeleton [5]. Serum levels of GFAP are known to be elevated after stroke and traumatic brain injury [6, 7]. There is increasing evidence that blood levels of GFAP are also elevated in primary HGGs prior to surgical resection implicating that serum GFAP is a diagnostically relevant biomarker [8–10]. However, its prognostic value nor its association to established prognostic markers such as IDH1 mutation, have not been examined. Also, the previous studies have included only primary HGGs whereas the correlation between serum GFAP level and tumor burden in recurrent HGGs has not been studied.
Overexpression of epidermal growth factor receptor (EGFR), which is often related to amplification of the EGFR gene, is a hallmark in primary or de novo glioblastomas [11]. EGFR gene amplification is detected in about 40 % of primary glioblastomas and approximately half of these additionally demonstrate EGFRvIII mutation, which results in constitutive signaling activity. This renders EGFR and EGFRvIII attractive targets for therapy [12]. In addition, EGFR amplification carries a diagnostic and prognostic value with an association to glioblastoma and reduced overall survival [13]. EGFR expression and amplification are most commonly determined by immunohistochemistry and chromogenic in situ hybridization (CISH), respectively. Measuring serum levels of EGFR extracellular domain (ECD) has provided additional information on tumor aggressiveness and outcome in various types of malignancies [14–17]. Quaranta et al. found elevated serum EGFR levels also in patients with glioblastomas compared to anaplastic astrocytomas or controls [18]. However, the association of serum EGFR levels to EGFR overexpression and amplification status in tumor tissue or to other molecular markers has not previously been studied.
Our purpose was to study serum levels of GFAP and EGFR in patients with primary and recurrent HGGs, and to examine their association with tumor volumes in T1-weighted post-contrast MRI, prognostic molecular markers, and progression-free survival (PFS). In addition, we wanted to evaluate the potential of serum EGFR as an indicator of tumor EGFR expression by determining the association of serum EGFR levels to tumor EGFR immunohistochemistry and gene amplification.
Materials and methods
Study subjects and sample collection
Pre-operative blood samples were prospectively obtained from 27 patients with radiologically suspected primary (n = 17) or recurrent (n = 10) HGG who were scheduled for tumor resection between 2011 and 2013 (mean age 53 years; women 63 %). Mean interval between blood sampling and surgical resection was 18 days. Additionally, post-operative blood samples were collected 2–5 days after surgical resection from 20 of these patients. Patient characteristics are presented in Table 1. The study was approved by the local ethics committee, and all patients gave written informed consent before participation. Serum samples of 13 healthy subjects (mean age 54 years; women 69 %) without a history of cancer or neurological symptoms were used as controls. Pre-operative and control blood samples were collected in Vacuette Z Serum Clot Activator (Greiner Bio-One, Kremsmünster, Austria) and post-operative blood samples in Venosafe plastic tubes (Terumo Europe N.V.). After adequate coagulation, samples were centrifuged at 2500×g for 10 min within 2 h, and supernatants were stored at −70 °C.
Serum GFAP and EGFR measurements
Serum GFAP and EGFR levels were determined using commercially available sandwich enzyme-linked immunosorbent assay (ELISA) kits from BioVendor (Brno, Czech Republic) and OncogeneScience (Cambridge, USA), respectively. Both assays were performed according to the instructions by the manufacturer. Serum samples, quality controls and standards were diluted 1:3 for GFAP ELISA and 1:50 for EGFR ELISA. All standards and test specimens were run in duplicates with the volume of 100 µl pipetted into each ELISA well. A biotin-labelled anti-GFAP-antibody and an alkaline phosphatase-labelled anti-EGFR-antibody specifically recognizing the ECD of EGFR were employed as detector antibodies. The absorbance was measured by reading the plate at 450 nm for GFAP and at 650 nm for EGFR. Reported concentration values are the mean absorbances of the duplicates. The limit of detection defined as the mean absorbance of the blanks (calibrator diluent) + 3 SD (Ablank + 3 × SDblank) was measured and calculated as 0.014 ng/ml for GFAP. All values below this detection limit were defined as 0 ng/ml, which also was applied in case the other absorbance measurement of a duplicate was below the detection limit. Serum EGFR ELISA assays for HGG patients and control subjects were performed at separate times and, therefore, 24 samples from HGG patients were re-analyzed for serum EGFR to test the reliability of the measurement.
Immunohistochemistry and molecular markers
Formalin-fixed paraffin-embedded tumor tissues obtained during surgical resection were sectioned at 3 µm and used for analyses. GFAP, EGFR, and Ki67 were studied by immunohistochemistry using primary antibodies (clones EP671Y, 5B7, and 30-9, respectively; Ventana Medical Systems, Strasbourg, France). IDH1 mutation was studied by immunohistochemistry with an IDH1 R132H antibody (clone H09; Dianova, Hamburg, Germany), which detects the most common R132H mutation of the IDH1 gene [19]. Immunostainings were performed with BenchMark XT Autostainer and antibody detection with ultraVIEW Universal DAB Detection Kit (Ventana Medical Systems, Tucson, Arizona). EGFR amplification was studied by silver in situ hybridization [20] and 1p/19q codeletion by fluorescent in situ hybridization using Vysis 1p36/1q25 and 19q13/19p13 FISH probe kit (Abbot Laboratories, Abbott Park, IL). MGMT gene promoter methylation was analyzed by pyrosequencing [21]. EGFR immunohistochemistry was reported using a scoring system described previously by Ålgars et al. [20]. Three scoring parameters were used: the highest staining intensity (minimum 10 % of tumor area), the most common staining intensity, and the localization of staining (membranous, cytoplasmic, or both). Staining intensities were classified as: 0 (negative), 1 (weak), 2 (moderate), and 3 (strong).
Enhancing and necrotic tumor volumes in MRI
Tumor areas with contrast enhancement and necrosis were defined from pre-operative MRI acquired on clinical basis. Mean interval between MRI and blood sampling was 18 days. Tumor volume with gadolinium enhancement was delineated in T1-weighted post-contrast images (MRI-T1-Gad) using iPlan RT Treatment Planning Software (Brainlab, Munich, Germany) by thresholding the enhancing tumor volume on visual basis and then manually subtracting the hyperintense volume on pre-contrast T1-weighted images. Necrotic tumor volume was manually outlined in pre-operative MRI-T1-Gad with guidance from standard T2-weighted and FLAIR images. Enhancing residual tumor volumes were correspondingly delineated in post-operative MRI-T1-Gad performed 1–4 days after operation. Extent of tumor resection (EOR%) was calculated from tumor volumes with gadolinium enhancement in pre- and post-operative MRI-T1-Gad in those patients with available post-operative serum samples.
Statistical analysis
Data are presented as mean ± SD. Comparisons of serum protein levels between groups were made using Kruskal–Wallis test and Mann–Whitney U test with Bonferroni correction, or one-way ANOVA. Spearman’s correlation was used to compare serum protein levels and tumor volumes, GFAP IHC, and Ki67 proliferation index. Comparisons of serum protein levels according to molecular marker status was performed using Mann–Whitney U test or Independent-samples T test. EGFR IHC was compared to serum EGFR using Kruskal–Wallis test and to EGFR amplification using Crosstabs with Pearson χ 2. Receiver operating characteristic (ROC) curve analysis was used to evaluate the ability of serum GFAP and EGFR values to discriminate glioblastoma from anaplastic glioma and control subjects. A GFAP cut-off value was determined according to ROC curve analysis and the cutoff value was then applied in Kaplan–Meier curve with log-rank test. Univariate Cox regression model was used to analyze survival data for PFS. PFS was defined as the time from first surgical resection (also for recurrent HGGs) to first tumor progression in follow-up MRI, deterioration in clinical symptoms, or end of follow-up. Agreement between repeated EGFR ELISA measurements was assessed with intraclass correlation coefficient ICC(3,1) and Coefficient of Repeatability (CR). Difference between pre- and post-operative serum protein levels was evaluated using Wilcoxon signed-rank or paired-samples T test. Two-tailed P values <0.05 were regarded as significant. Statistical analyses were conducted using SPSS 21 for Mac (SPSS, Inc., Chicago, IL, USA).
Results
Pre-operative serum GFAP
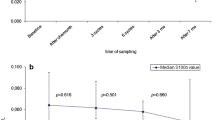
12 patients (86 %) with glioblastoma and three patients (23 %) with anaplastic glioma had pre-operatively detectable serum GFAP levels (≥0.014 ng/ml). All control subjects but one showed zero serum GFAP (detection limit 0.014 ng/ml). Serum GFAP was significantly higher in glioblastoma patients (0.079 ± 0.100) compared to anaplastic glioma patients (0.012 ± 0.028; P = 0.003) or controls (P = 0.001) (Fig. 1a). No difference was observed between anaplastic glioma patients and control subjects (P = 1.000). Serum GFAP levels for primary and recurrent HGGs were 0.055 ± 0.098 and 0.032 ± 0.038, respectively (P = 0.979).
Box plot of serum GFAP (a) and serum EGFR (b) values in healthy control subjects (n = 13) and patients with primary or recurrent anaplastic glioma (n = 13) or glioblastoma (n = 14) before surgery. GFAP values were significantly elevated in glioblastoma patients when compared with anaplastic glioma (P = 0.003) or control subjects (P = 0.001)
Pre-operative serum GFAP values significantly correlated to enhancing tumor volume and necrotic tumor volume in MRI-T1-Gad both in primary (r = 0.64; P = 0.005 and r = 0.73; P = 0.001, respectively) and in recurrent HGGs (r = 0.76; P = 0.011 and r = 0.64; P = 0.047, respectively) (Fig. 2). Additionally, enhancing tumor volume correlated to necrotic tumor volume (r = 0.73; P < 0.001).
Patients with HGGs carrying IDH1 gene mutation showed significantly lower serum GFAP levels (0.012 ± 0.033 ng/ml) compared to patients with IDH1 mutation-negative HGGs (0.061 ± 0.091 ng/ml; P = 0.016). In relation to 1p19q co-deletion or MGMT promoter methylation status, however, no variation in serum GFAP level was observed (P = 0.775 and P = 0.864, respectively). In contrast, serum GFAP values correlated to Ki67 proliferation index (r = 0.78; P < 0.001). All HGGs expressed GFAP detected by immunohistochemistry (GFAP positive cells 87 ± 20 %), the extent of which, however, did not correlate to serum GFAP levels (P = 0.761).
ROC analysis for the differentiation of glioblastoma from anaplastic glioma or control patients produced a serum GFAP cut-off value of 0.014 ng/ml with a sensitivity of 86 % and a specificity of 85 % (AUC 0.86; P < 0.001; CI 0.72–0.99). Univariate Cox regression analysis revealed serum GFAP value of ≥0.014 ng/ml to be a significant predictor of PFS in primary HGGs (Hazard ratio 5.9; P = 0.032; CI 1.2–29.9). The Kaplan–Meier curve (Fig. 3) illustrates that serum GFAP ≥ 0.014 ng/ml was related to poor PFS in patients with primary HGG compared to HGG patients with serum GFAP < 0.014 ng/ml (P = 0.008; Log rank).
Pre-operative serum EGFR
No statistical difference was observed in pre-operative serum EGFR values between glioblastoma patients (52.6 ± 11.0 ng/ml), anaplastic glioma patients (50.6 ± 9.2 ng/ml), and control subjects (55.8 ± 7.8 ng/ml P = 0.391) (Fig. 1b). Accordingly, ROC analysis of serum EGFR values resulted in poor discrimination between glioblastoma and anaplastic glioma patients (AUC 0.57; P = 0.528; CI 0.35–0.79). Serum EGFR values did not correlate to enhancing or necrotic tumor volume in MRI-T1-Gad (P = 0.985 and P = 0.261, respectively), nor to Ki67 proliferation index (P = 0.235). Furthermore, the status of IDH1 mutation, 1p19q co-deletion, or MGMT promoter methylation were not associated to different levels of serum EGFR (P = 0.392, P = 0.762, and P = 0.197, respectively).
Serum EGFR concentration was not related to tumor EGFR gene amplification or immunohistochemistry. Similar serum EGFR values were observed in HGG patients with EGFR amplification (54.5 ± 12.0 ng/ml) and without EGFR amplification (50.5 ± 9.2 ng/ml; P = 0.351). All HGGs studied showed positive staining in EGFR immunohistochemistry. Highest staining intensity was three in most specimens, whereas the most common staining intensity varied from 0 to 3. Location of EGFR IHC staining most commonly was both cytoplasmic and membranous. However, the intensity or the location of the staining was not associated to serum EGFR concentration (P = 0.418 and P = 0.206, respectively) nor to EGFR amplification (P = 0.091 and P = 0.943, respectively). Elevated (>71.3 ng/ml) or diminished serum EGFR values (<40.2 ng/ml; healthy controls serum EGFR mean ± 2SD) were not associated to PFS in patients with primary HGG (HR 1.5; P = 0.707; CI 0.2–12.2 and HR 0.9; P = 0.958; CI 0.1–7.6, respectively). For repeated EGFR ELISA measurements, ICC(3,1) was 0.764 (CI 0.532–0.890) and CR 14.5 ng/ml indicating moderate agreement between measurements.
Post-operative serum GFAP and EGFR levels
Post-operative serum GFAP levels were elevated from pre-operative levels in 65 % of the HGG patients with available post-operative serum samples (n = 20). The average increase in post-operative serum GFAP levels was 0.39 ± 0.63 ng/ml, which was statistically significant (P = 0.003; Fig. 4a). This increase in serum GFAP or the separate post-operative values, however, showed no correlation to either enhancing residual tumor volume in post-surgical MRI or to the EOR% (P = 0.583; P = 0.719; P = 0.372; P = 0.508, respectively). Post-operative serum EGFR levels did not differ from those observed pre-operatively (P = 0.354; Fig. 4b), nor did they correlate to enhancing residual tumor volume or EOR%. The range of EOR% in those patients with available post-operative serum samples was 63–100 % (mean 89 ± 13 %).
Post-operative serum samples were obtained on day 2 (n = 5), day 3 (n = 11), day 4 (n = 3), or day 5 (n = 1). No significant difference in mean serum GFAP or EGFR values was observed between these post-operative days (P = 0.280 and P = 0.260, respectively).
Discussion
In this study we found that serum GFAP is a potential biomarker for diagnosis of recurrence since GFAP levels significantly correlated with tumor burden in recurrent HGGs. Serum GFAP may thus be helpful in the follow-up of patients with HGG who often present controversial findings on MRI after oncologic therapy. Additionally, serum GFAP may confer prognostic value since it seems to be associated with IDH1 mutation-negative tumors and short PFS. In contrast, serum EGFR provides little value in patients with HGG since it showed no difference compared to healthy control subjects and no association with tumor burden, EGFR amplification or protein expression.
Serum GFAP provides diagnostic and prognostic value in primary and recurrent HGGs
We found that serum GFAP was detectable in most glioblastoma patients but only 3 out of 13 anaplastic glioma patients. Accordingly, serum GFAP level above 0.014 ng/ml provided a sensitivity of 86 % and specificity of 85 % for the diagnosis of GBM. Our results correspond to previous studies confirming the diagnostic value of serum GFAP in differentiating GBM from gliomas of lower grade [8, 9, 22]. High serum GFAP value in one control subject remains unclarified as there was no history of brain trauma, brain MRI was normal, and after 10 months of follow-up this subject remained neurologically symptom-free.
The correlation of serum GFAP to tumor burden in recurrent HGGs is of interest and suggests a possible value of serum GFAP as a biomarker for tumor recurrence. Previously the association between serum GFAP and tumor volume has been evaluated only in primary HGGs [8, 10]. Clearly, difficulties in determining true recurrence in the era of pseudoprogression and pseudoregression resulting from novel oncologic therapies underlines the potential importance of our finding. However, a longitudinal follow-up with a larger patient population is warranted to study in more detail the ability of serum GFAP to detect recurrent HGGs at the earliest possible stage.
Serum GFAP was related to both enhancing and necrotic tumor volume in MRI-T1-Gad. Tumor necrosis might therefore partially explain the elevated serum GFAP levels associated with bulky tumors. In a previous study, Jung et al. found a correlation between serum GFAP levels and the histologic measure of necrotic GFAP positive tumor cells in patients with GBM, further emphasizing that the size of the tumor and the amount of GFAP positive cells, necrosis and the disruption of BBB, may all be factors involved in the elevation of serum GFAP levels in patients with HGG [8].
To our knowledge, this study demonstrates for the first time that serum GFAP level is related to IDH1 mutation status in HGGs. IDH1 mutation in gliomas is regarded as the most powerful prognostic marker for a favourable outcome compared to their IDH1 mutation-negative counterparts [23]. Relation of high serum GFAP to IDH1 mutation-negative HGGs, and also correlation to high Ki67 proliferation index implicate the highly aggressive characteristics of HGGs associated with high serum GFAP. Furthermore, using 0.014 ng/ml as a cutoff value we found high serum GFAP to be a significant prognostic marker for a poor PFS in patients with primary HGG. On the contrary, a previous study reported a non-significant trend for a more favourable overall survival in GBM patients with higher serum GFAP levels [22]. The authors speculated that this is due to decreasing GFAP expression with increasing malignancy grade. However, we found no such difference in tumor GFAP expression between anaplastic gliomas and glioblastomas (P = 0.435).
The increase in serum GFAP levels after surgical tumor resection is consistent to a previous study where plasma GFAP values were elevated 24–48 h after surgery in 83 % of patients including both low-grade and high-grade gliomas [9]. Furthermore, post-operative serum GFAP values in our cohort showed no correlation to either enhancing residual tumor volume or to EOR%. These results indicate that post-operative blood levels of GFAP represent brain injury induced by the surgery rather than being a measure of residual tumor burden.
Serum EGFR is not related to EGFR status in the tumor tissue
In contrast to a previous study [18], we were unable to detect any difference in serum EGFR levels between patients with GBM, anaplastic glioma, and healthy controls. We used the same ELISA assay as Quaranta et al., but included also anaplastic oligodendrogliomas, oligoastrocytomas, and GBMs with oligodendroglioma component. However, this is not likely to explain the discrepancy since HGGs with or without oligodendroglioma component presented with similar pre-operative serum EGFR values (P = 1.0).
Circulating EGFR concentrations are altered in various cancers. Compared to controls, lower serum EGFR levels have been detected in patients with ovarian and breast cancer, whereas elevated concentrations have been associated with cervical and gastric carcinomas, and pleural mesotheliomas [14–17, 24]. We found no such alteration in serum EGFR concentrations in HGG patients compared to healthy controls. Furthermore, EGFR gene amplification or protein overexpression in tumor tissue was not related to circulating EGFR levels. These results suggest that tumor cells are not likely to be the major source of circulating EGFR in patients with HGG, which is supported by the fact, that serum EGFR levels did not correlate to tumor burden in MRI. According to our findings, BBB disruption does not affect the release of ECD of EGFR into circulation. Our results indicate that serum EGFR has no diagnostic or prognostic value in patients with HGG and we further believe that serum EGFR is not applicable as a predictive marker for efficacy or treatments targeting EGFR.
Our study confronts limitations. First, ELISA tests for GFAP or EGFR have not yet been standardized. Second, the number of patients was limited and, therefore, our preliminary results require confirmation in larger cohorts.
Conclusion
This is the first study to show the potential of serum GFAP as a biomarker for tumor recurrence in patients with HGG since it correlated with recurrent tumor burden. Serum GFAP may thus offer a valuable tool in the follow-up of HGG patients. However, larger prospective trial to confirm this relationship is warranted. Furthermore, our results suggest a prognostic value for serum GFAP since it associated with IDH1 mutation status and PFS. In contrast, we conclude that circulating EGFR is not related to tumor EGFR expression and thus provides little value in planning and follow-up of EGFR-targeted therapies.
References
Ohgaki H (2009) Epidemiology of brain tumors. Methods Mol Biol 472:323–342
Gerlinger M, Rowan AJ, Horswell S et al (2012) Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 366:883–892
Hygino da Cruz LC, Jr Rodriguez I, Domingues RC, Gasparetto EL, Sorensen AG (2011) Pseudoprogression and pseudoresponse: imaging challenges in the assessment of posttreatment glioma. AJNR Am J Neuroradiol 32:1978–1985
Holdhoff M, Yovino SG, Boadu O, Grossman SA (2013) Blood-based biomarkers for malignant gliomas. J Neurooncol 113:345–352
Eng LF, Ghirnikar RS, Lee YL (2000) Glial fibrillary acidic protein: GFAP-thirty-one years (1969–2000). Neurochem Res 25:1439–1451
Herrmann M, Vos P, Wunderlich MT, de Bruijn CH, Lamers KJ (2000) Release of glial tissue-specific proteins after acute stroke: a comparative analysis of serum concentrations of protein S-100B and glial fibrillary acidic protein. Stroke 31:2670–2677
Vos PE, Jacobs B, Andriessen TM, Lamers KJ, Borm GF, Beems T, Edwards M, Rosmalen CF, Vissers JL (2010) GFAP and S100B are biomarkers of traumatic brain injury: an observational cohort study. Neurology 75:1786–1793
Jung CS, Foerch C, Schanzer A, Heck A, Plate KH, Seifert V, Steinmetz H, Raabe A, Sitzer M (2007) Serum GFAP is a diagnostic marker for glioblastoma multiforme. Brain 130:3336–3341
Husain H, Savage W, Grossman SA et al (2012) Pre- and post-operative plasma glial fibrillary acidic protein levels in patients with newly diagnosed gliomas. J Neurooncol 109:123–127
Brommeland T, Rosengren L, Fridlund S, Hennig R, Isaksen V (2007) Serum levels of glial fibrillary acidic protein correlate to tumour volume of high-grade gliomas. Acta Neurol Scand 116:380–384
Ohgaki H, Kleihues P (2007) Genetic pathways to primary and secondary glioblastoma. Am J Pathol 170:1445–1453
Hegi ME, Rajakannu P, Weller M (2012) Epidermal growth factor receptor: a re-emerging target in glioblastoma. Curr Opin Neurol 25:774–779
Shinojima N, Tada K, Shiraishi S et al (2003) Prognostic value of epidermal growth factor receptor in patients with glioblastoma multiforme. Cancer Res 63:6962–6970
Oh MJ, Choi JH, Kim IH et al (2000) Detection of epidermal growth factor receptor in the serum of patients with cervical carcinoma. Clin Cancer Res 6:4760–4763
Lafky JM, Wilken JA, Baron AT, Maihle NJ (2008) Clinical implications of the ErbB/epidermal growth factor (EGF) receptor family and its ligands in ovarian cancer. Biochim Biophys Acta 1785:232–265
Gaafar R, Bahnassy A, Abdelsalam I, Kamel MM, Helal A, Abdel-Hamid A, Eldin NA, Mokhtar N (2010) Tissue and serum EGFR as prognostic factors in malignant pleural mesothelioma. Lung Cancer 70:43–50
Asgeirsson KS, Agrawal A, Allen C, Hitch A, Ellis IO, Chapman C, Cheung KL, Robertson JF (2007) Serum epidermal growth factor receptor and HER2 expression in primary and metastatic breast cancer patients. Breast Cancer Res 9:R75
Quaranta M, Divella R, Daniele A, Di Tardo S, Venneri MT, Lolli I, Troccoli G (2007) Epidermal growth factor receptor serum levels and prognostic value in malignant gliomas. Tumori 93:275–280
Capper D, Zentgraf H, Balss J, Hartmann C, von Deimling A (2009) Monoclonal antibody specific for IDH1 R132H mutation. Acta Neuropathol 118:599–601
Ålgars A, Lintunen M, Carpen O, Ristamäki R, Sundström J (2011) EGFR gene copy number assessment from areas with highest EGFR expression predicts response to anti-EGFR therapy in colorectal cancer. Br J Cancer 105:255–262
Tuononen K, Tynninen O, Sarhadi VK et al (2012) The hypermethylation of the O6-methylguanine-DNA methyltransferase gene promoter in gliomas—correlation with array comparative genome hybridization results and IDH1 mutation. Genes Chromosomes Cancer 51:20–29
Ilhan-Mutlu A, Wagner L, Widhalm G et al (2013) Exploratory investigation of eight circulating plasma markers in brain tumor patients. Neurosurg Rev 36:45–56
Horbinski C (2013) What do we know about IDH1/2 mutations so far, and how do we use it? Acta Neuropathol 125:621–636
Choi JH, Oh JY, Ryu SK, Kim SJ, Lee NY, Kim YS, Yi SY, Shim KS, Han WS (1997) Detection of epidermal growth factor receptor in the serum of gastric carcinoma patients. Cancer 79:1879–1883
Acknowledgments
We thank Taina Kirjonen (Department of Physiology, University of Turku), Sinikka Kollanus and Minnamaija Lintunen (Department of Pathology, Turku University Hospital) for excellent technical assistance.
Funding
This study was funded by Cancer Society of Finland and Southwest Finland Hospital District (EVO research funding). A.K. is a Ph.D. student supported by the National Graduate School of Clinical Investigation.
Conflict of interest
The authors declare that they have no conflict of interest.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiviniemi, A., Gardberg, M., Frantzén, J. et al. Serum levels of GFAP and EGFR in primary and recurrent high-grade gliomas: correlation to tumor volume, molecular markers, and progression-free survival. J Neurooncol 124, 237–245 (2015). https://doi.org/10.1007/s11060-015-1829-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1829-7