Abstract
Several blood biomarkers have been established for the early diagnosis, screening and follow-up of non central nervous system cancers. However, there is lack of knowledge on biochemical blood alterations in brain tumor patients. In this study, we prospectively collected blood plasma samples of 105 adult brain tumor patients with diffuse low-grade glioma (World Health Organization (WHO) II, n = 7), anaplastic glioma (WHO III, n = 10), glioblastoma multiforme (WHO IV, glioblastoma multiforme (GBM)) (n = 34), meningioma (WHO I, n = 8), atypical meningioma (WHO II, n = 5), and intracerebral metastasis (ICM; n = 41). In each case, we measured plasma concentrations of neuropeptide Y, brain-derived neurotrophic factor, glial cell line-derived neurotrophic factor, placental growth factor (PlGF), S100B, secretagogin, interleukin 8, and glial fibrillary acidic protein (GFAP) using enzyme-linked immunosorbent assay. Plasma marker concentrations were correlated to patient parameters including neuropathological diagnosis and neuroradiological features. Most of the markers were detectable in all diagnostic categories in variable concentrations. GFAP plasma detectability was strongly associated with a diagnosis of GBM (p < 0.001). Plasma GFAP and plasma placental growth factor showed promising moderate potential in the differential diagnosis of unifocal GBM versus unifocal supratentorial ICM (area under the curve = 0.73, p < 0.05). To summarize, our data show that none of the investigated markers is suitable to substitute histological diagnosis. However, measurement of circulating GFAP and PlGF may support neuroradiological differential diagnosis of GBM versus ICM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In clinical medicine, biomarkers are defined as objectively measurable factors that provide information about a disease state, thus providing the possibility for early diagnosis, differential diagnosis, and follow-up of disease. In oncology, blood is a feasible medium for routine clinical biomarker investigations, as blood sampling is usually performed repeatedly during the disease course of cancer patients, e.g., for verification of adequate organ function prior to, during, or after diagnostic or therapeutic interventions. Blood drawing is usually easily and quickly performed by puncture of a peripheral arm vein and is normally associated with only minor discomfort for the patient. For most major cancer types, distinct blood biomarkers have been firmly established in the routine clinical patient management. Examples include factors that facilitate screening and early diagnosis (e.g., prostate-specific antigen in prostate cancer), differential diagnosis (e.g., beta-human chorionic gonadotrophin or alpha-fetoprotein in germ cell tumors) and monitoring (e.g., cancer antigen 15-3 (CA 15-3) in breast cancer, carcinoembryonic antigen (CEA) in breast and colorectal cancer) of neoplastic disease [32, 33].
Brain tumors comprise a heterogenous spectrum of neoplasms including approximately 120 entities and variants of primary brain tumors and a variety of secondary (metastatic) neoplasms [31]. At initial presentation, neuroimaging is usually performed. Implementation of advanced imaging modalities has improved the neuroradiological diagnostic accuracy. Still, neuroimaging lacks perfect specificity for differentiation of brain tumors. The definite tumor typing and grading relies on histopathological evaluation of tumor tissue extracted by a neurosurgical intervention (biopsy or resection).
Reliable blood biomarkers could support the management of brain tumors, e.g., by facilitating neuroradiological differential diagnosis at initial presentation, planning of surgical interventions, or monitoring of the disease course. However, except for rare pediatric germ cell tumors [13], no blood biomarkers have been established in the routine clinical management of brain tumor patients, although some previous studies have identified biochemical blood alterations with potential clinical utility in neurooncology [10, 24].
Here, we report the results of a prospective, exploratory study investigating the blood plasma concentrations of several distinct proteins (Table 1) and their association with tumor type and neuroradiological features in adult brain tumor patients.
We included S100B, neuropeptide Y (NPY) and secretagogin (SCGN) in the panel of investigated proteins, because we have observed markedly elevated plasma levels of these proteins in the peripheral blood approximately 1 year before manifestation of malignant glioma [15]. We studied glial fibrillary acidic protein (GFAP), because two previous reports have indicated its potential usability as clinical blood biomarker of glioblastoma [9, 24]. We also included placental growth factor (PlGF), interleukin 8 (IL8), brain-derived neurotrophic factor (BDNF), and glial cell derived neurotrophic factor (GDNF) in our study. These factors were found to be differentially expressed in distinct types of brain tumors at the tissue level and were demonstrated to be important as plasma/serum markers for non-neoplastic central nervous system diseases [7, 14, 34, 40, 44, 47]. Interestingly, a recent study showed that changes in serum levels of PlGF over time associate with overall survival times of patients with recurrent glioblastoma treated with cediranib [3]. To our knowledge, BDNF and GDNF have not been investigated in the blood of neurooncological patients so far.
Materials and methods
Study population
In this study, we prospectively enrolled 105 adult brain tumor patients at the Department of Neurosurgery, Medical University of Vienna. Inclusion criteria comprised: age 18 years or older; neuroradiologically verified brain tumor scheduled for stereotactic biopsy, neurosurgical resection, radiosurgery or radiotherapy; written informed consent to participate in the study.
Patients with a histologically confirmed noncentral nervous system primary tumor, who presented with typical symptoms and neuroradiological appearance of intracerebral metastasis (ICM) and who underwent radiosurgery or radiotherapy of the cerebral lesion were eligible for our study even if ICM was not verified histologically.
Twenty-six healthy volunteers and 25 patients with multiple sclerosis (MS) as nonmalign central nervous system pathology served as control subjects. For each MS patient, an Expanded Disability Status Score (EDSS) was calculated by an experienced neurologist at the time of blood sampling [28]. The study was approved by the ethics committee of the Medical University of Vienna.
Sample collection
In tumor patients, blood samples were collected before the neurosurgical intervention or before the start of radiotherapy. From each patient and each control subject, one blood sample was collected from a forearm vein into a 7 ml vacutainer EDTA tube and immediately cooled on 4 °C. Samples were centrifuged at 3,000 rounds per minute for 10 min at 4 °C within 1 h after collection and the plasma was stored at −80 °C in small aliquots after separation from cells.
Biochemical plasma analyses
SCGN, S100B, and GFAP plasma concentrations were determined using commercially available enzyme-linked immunosorbent assay (ELISA) kits from BioVendor (Brno, Czech Republic). PlGF and IL8 plasma concentrations were analyzed using ELISA kits from Quantikine (R&D Systems, Minneapolis, MN, USA). BDNF and GDNF plasma concentrations were measured using ELISA kits from Promega (Promega Corporation, Madison, WI, USA). NPY plasma concentration was quantified using a commercially available radioimmunoassay kit, purchased from EURIA (Euro Diagnostica, Malmö, Sweden). All assays were performed according to the manufacturer’s instructions. GFAP, SCGN, and IL8 plasma level measurements were conducted in duplicates. Due to the lack of plasma sample volumes, BDNF, GDNF, PlGF, S100B, and NPY assays were performed as single measurements only. In control subjects (healthy individuals and MS patients), only measurements of plasma GFAP concentrations were performed. The limit of detection for each assay was defined as mean of the absorbance of the blanks (dilution buffer) plus 3 SD of the mean of the blanks and was calculated as 6 pmol/L for NPY, 8.19 pg/ml for BDNF, 8.81 pg/ml for GDNF, 0.24 pg/ml for PlGF, 26.39 pg/ml for S100B, 7.93 pg/ml for SCGN, 0.43 pg/ml for IL8, and 0.03 ng/ml for GFAP.
Neurosurgery
In case of stereotactic biopsy, the tumor region with significant contrast enhancement and in tumors with nonsignificant contrast enhancement, the intratumoral area with maximal 11C methionine positron emission tomography (PET) tracer uptake was used as biopsy target. In case of tumor resection, multiple tumor tissue samples were collected from areas of different tumor consistency and appearance including samples from the contrast-enhancing tumor part and/or the area with maximum PET tracer uptake.
Neuropathology
We recorded the neuropathological diagnosis made from the tumor specimen obtained at the neurosurgical intervention (biopsy or resection) after blood sample collection. Neuropathological diagnosis was made by a board-certified neuropathologist from formalin-fixed and paraffin-embedded neurosurgical specimens according to the current edition of the World Health Organization Classification of Tumours of the Central Nervous System [31]. Diagnosis was made on routinely prepared hematoxylin and eosin-stained slides, supplemented by standard immunohistochemical stains as deemed adequate by the responsible neuropathologist. The diagnosis of two glioblastoma multiforme (GBM) patients and one ICM patient was made from autopsy specimens according to the aforementioned criteria.
Neuroradiological analyses
In each patient, we retrieved the most representative MRI investigation performed around the time of blood sample collection and before the neurosurgical intervention or start of radiotherapy. In each case, we analyzed the following neuroradiological features: anatomical tumor localization, contrast enhancement of the tumor (yes/no), perifocal edema (yes/no), necrosis within the tumor (yes/no), contact of the tumor with ependyma (yes/no), infiltration of the hippocampus by the tumor (yes/no), contact of the tumor with meninges (yes/no), number of distinct neoplastic lesions. For meningiomas, we additionally analyzed the following features: brain compression by the tumor (yes/no) and brain invasion by the tumor (yes/no). For all measurable lesions, we calculated the tumor volume using a previously described modified ellipsoid volume equation of (A × B × C)/2, where A, B, and C correspond to the three dimensions of the tumor [27]. In cases with multiple tumors, we calculated the sum of the tumor volumes of all measurable neoplastic lesions. MRI data were extracted from the following sequences obtained at a field strength of 3 T: T1 before and after contrast media, T2, and fluid-attenuated inversion recovery.
Statistical analyses
Quantitative variables were described with median, minimum, and maximum, and boxplots were used for graphic representation. Boxplots were defined to consist of interquartiles range (box), median (horizontal line within box), and maximum and minimum (whiskers). Group comparisons for quantitative variables were performed with Mann–Whitney U and Kruskal–Wallis tests for two and more than two groups, respectively. Chi-squared test (or Fisher’s exact test if appropriate) were used for the evaluation of categorical variables. Agreement between duplicate ELISA measurements was assessed with Bland–Altman plots.
Logistic regression models were used to evaluate the detectability of plasma markers in dependence of tumor diagnosis and tumor localization. Due to the small sample size, Firth correction or exact tests were used if appropriate.
A stepwise logistic regression model was employed to distinguish unifocal supratentorial GBM from unifocal supratentorial intracerebral ICM with plasma markers. The aim of this analysis was to analyze the biomarker utility for supporting the most common and typical neuroradiolocal differential diagnosis of GBM versus ICM in patients with first presentation of a solitary intracranial tumor. For the sake of robustness, seven out of eight plasma markers were used in dichotomous form (detected versus nondetected), only for NPY the quantitative values were used as NPY was always detected. It is quite obvious that in such a small dataset there cannot be a definite answer which plasma marker is most promising [19]; however, the collective diagnostic potential of the plasma markers can be assessed in order to judge the meaningfulness of future large-scale diagnostic studies. Internal validation was used to correct the inevitable over-optimism of the stepwise model results (e.g., area under the receiver operating characteristic curve (AUC)) by employing the so-called bootstrap method [19]. Bootstrap is based on repeatedly resampling (with replacement) from the dataset, so that a series of training and test datasets are formed. After applying the statistical approach in question to a training dataset, it is validated in the corresponding independent test dataset. This is repeated many times and the combined results are summarized.
Overall survival time data were obtained from patient records of the Medical University of Vienna and the Austria Brain Tumour Registry [45]. Survival probabilities were computed with the Kaplan–Meier method, and log-rank tests were used to compare overall survival between groups. Patients with relapsing GBM (n = 4) and multifocal lesions (n = 18) were excluded from stepwise logistic regression model and Kaplan–Meier curve analyses.
All reported p values are results of two-sided tests. A significance level of 5 % was used. No adjustment for multiple testing has been performed as the goals of the study are exploratory rather than confirmatory [5]. Statistical Software packages SPSS version 18 (SPSS Inc, Chicago, IL, USA) and SAS version 9.2 (SAS Institute Inc., Cary, NC, USA) were used for the statistical calculations. Figures were designed with GraphPad Prism (La Jolla, CA, USA).
Results
Patients
Baseline characteristics of all brain tumor patients included in our study are demonstrated in Table 2. Neuropathological diagnoses included diffuse low grade glioma (World Health Organization (WHO) II, n = 7), anaplastic glioma (WHO III, n = 10), GBM (WHO IV, n = 34), meningioma (WHO I, n = 8), atypical meningioma (WHO II, n = 5), and ICM (n = 13). Twenty-eight brain tumor patients with a proven extracerebral primary tumor were treated with either radiosurgery or radiotherapy and diagnosed as ICM.
The primary tumors of patients diagnosed with ICM included 17 non-small cell lung cancer, nine small cell lung cancer, six clear cell renal cell carcinoma, three breast cancer, three melanoma, one thyroid carcinoma, one rectal adenocarcinoma, and one endometrial cancer.
The group of control subjects without evidence for any cerebral neoplasm included 25 MS patients (age, median 40 years; range, 22–60 years; 18 females and seven males) and 26 healthy volunteers (age, 50 median years; range, 31–84 years; 11 females and 15 males).
The time lags between date of blood sample collection and date of neurosurgical intervention (biopsy or subtotal/total resection or radiosurgery) or start of radiotherapy ranged from 1 to 7 days (median, 3 days). The time lags between date of blood sample collection and date of MRI investigation selected for our study ranged from 0 to 33 days (median, 2 days).
Plasma markers
Correlation with diagnosis
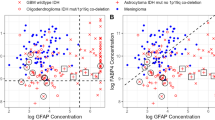
Table 2 details the plasma concentration profiles of the individual plasma markers according to brain tumor type and Fig. 1 demonstrates the results of statistical group comparisons. None of the markers showed exclusive plasma detectability in a given brain tumor type. However, GFAP plasma detectability was strongly associated with a diagnosis of GBM (p < 0.001, chi-square test). GFAP was detectable in the plasma of 13/34 GBM and only 1/41 ICM patient, while it was not detectable in the plasma of any other brain tumor patient. The only plasma GFAP positive ICM patient had a small single parapontine lesion that was treated by radiosurgery without histological confirmation. Based on the strong association of plasma GFAP with a diagnosis of GBM, GFAP was evaluated within a cohort consisting of MS patients and control subjects. Of note, 1/25 MS patients and 1/26 healthy control subjects were positive for plasma GFAP (0.11 and 0.13 ng/ml, respectively). The plasma GFAP positive healthy control subject is a full time working academician, who does not suffer from any signs of neurological disorder. Notably, among the MS patients of our study cohort, the only plasma GFAP positive individual had the highest EDSS score (EDSS = 5).
Boxplots summarizing the plasma concentrations of each marker according to brain tumor diagnosis. The significant differences between patient groups were calculated using Mann–Whitney U test and are depicted with asterisks (*p < 0.05, **p < 0.01, and ***p < 0.001). Demonstrated are the pairwise tests between glioma and ICM groups, among the glioma (WHO II–IV) and meningioma (WHO I–II) groups. BDNF brain-derived neurotrophic factor, GDNF glial cell line-derived neurotrophic factor, GFAP glial fibrillary acidic protein, glioma II glioma WHO II, glioma III glioma WHO III, glioma IV glioma WHO IV, ICM intracerebral metastasis, IL8 interleukin 8, Men I meningioma WHO I, Men II meningioma WHO II, NPY neuropeptide Y, PlGF placental growth factor, SCGN secretagogin
When comparing GBM and ICM patients, we found statistically significant differences in plasma concentrations of BDNF, PlGF, IL8, and GFAP. PlGF and IL8 plasma concentrations were significantly higher in ICM patients than in GBM patients (p = 0.002, p = 0.001, respectively, both with Mann–Whitney U test). In contrast, GFAP and BDNF plasma concentrations were significantly lower in ICM patients than in GBM patients (p < 0.001, p = 0.04, respectively, both with Mann–Whitney U test; Fig. 1). None of the other markers (NPY, GDNF, S100B, or SCGN) showed statistically different plasma concentrations between GBM and ICM patients. All eight plasma parameters analyzed in this study were included in a stepwise logistic regression model in order to explore their discriminatory value in the differential diagnosis of unifocal GBMs versus singular supratentorial ICMs. The area under the curve of the model was 0.84 which was reduced to 0.73 (p < 0.05) after internal validation with bootstrap method. The bootstrap method also allows counting how often a candidate variable enters the final model. GFAP and PlGF were chosen in 79 and 70 % of the bootstrap replications, respectively, indicating rather strong predictability whereas all other parameters failed to show a relevant predictability (ranging from 6 to 37 %).
NPY and IL8 plasma concentrations showed a statistically significant inverse association with tumor grade in glioma (p = 0.02 for both, Mann–Whitney U test; Fig. 1a). NPY concentrations were significantly lower in the blood plasma of high grade meningioma patients than in the plasma of low-grade meningioma patients (p = 0.004, Mann–Whitney U test). PlGF concentrations were significantly higher in the blood plasma of high grade meningioma patients than in the plasma of low grade meningioma patients (p = 0.03, Mann–Whitney U test).
Correlation with neuroradiological findings
Evaluable neuroradiological images were available in 96/105 patients. Electronic supplementary material (ESM) 1 shows the correlation of plasma detectability of each marker with neuroradiological parameters.
In brief, none of the eight investigated plasma markers showed statistically significant association with presence of contrast enhancement, perifocal edema, necrosis, hippocampus infiltration, contact with meninges, brain compression, brain invasion, tumor volume, or number of intracerebral neoplastic lesions (ESM 1). Solely, lack of GDNF plasma detectability was associated with lack of ependymal contact within ICM patient group (p < 0.05, Fisher’s exact test).
Among anaplastic gliomas (WHO III), tumors with ependyma contact were significantly larger than tumors without ependyma contact, respectively (p = 0.04, Mann–Whitney U test). ICM cases with perifocal edema were significantly larger than ICM cases without perifocal edema (p = 0.002, Mann–Whitney U test). Tumor volume or number of intracerebral neoplastic lesions did not show statistically significant associations with plasma detectability of any of the investigated markers.
The correlation of plasma marker concentrations with anatomical tumor localization according to tumor type is summarized in ESM 2. Plasma detectability of any of the eight parameters was not associated with tumor location (all p < 0.05, logistic regression).
Assessing agreement of the duplicate measurements
Agreement of the duplicate measurements of GFAP, SCGN, and IL8 plasma concentrations were assessed using Bland–Altman diagram and showed highly congruent results.
Survival analysis
Clinical follow-up data were available of 27/34 GBM patients. We did not detect a statistically significant association of plasma concentration of any of the eight investigated markers with patient overall survival time. However, there was an interesting difference in median overall survival times between GBM patients with (11.3 months) and GBM patients without (5.2 months) detectable plasma GFAP (Fig. 2).
Discussion
In this study, we characterized the blood plasma concentrations of eight markers in brain tumor patients. Most of the markers were detectable in all diagnostic categories in variable concentrations, which may reflect distinct biological tumor features. We observed some associations of blood marker concentrations with clinical parameters that may be of relevance for patient management.
We show that plasma GFAP detectability is highly associated with the diagnosis of GBM. This finding is in line with two previous investigations that have described circulating GFAP as potentially useful biomarker in malignant glioma patients [9, 24]. However, in contrast to the study by Jung et al., we did not detect circulating GFAP exclusively in GBM patients. We detected GFAP also in the plasma of one patient with ICM, one patient with MS, and even in one healthy control subject. While breakdown of CNS tissue associated with the metastasis in the ICM patient and with inflammation in the MS patient seem plausible explanations for the elevation of circulating GFAP, it is unclear what may have caused plasma GFAP detectability in the healthy control subject. Anyway, our data show that plasma GFAP elevations lack perfect accuracy for GBM. However, also most well established and clinically useful tumor markers like CEA, CA 19-9 or CA125 lack perfect accuracy [2, 6, 13].
In concordance with Jung et al. [24], we show that not all cases of GBM are plasma GFAP positive. We were not able to identify a difference in neuroradiological appearance between GBM patients with and without detectable plasma GFAP. In contrast to the two previous studies by Jung et al. and Brommeland et al. [9, 24], we could not detect a correlation between the concentration of circulating GFAP and tumor volume in GBM patients. One reason for this discrepancy could be that volumetric assessment of GBM is hampered by its infiltrative growth pattern, which limits reliable demarcation of tumor borders on neuro-images.
Differential diagnosis of GBM from ICM is a common neuroradiological problem. Both tumor types may appear as contrast-enhancing ring-like lesions in the brain parenchyma. Characteristic plasma biomarker profiles for these entities could potentially support radiological differential diagnosis and clinical decision making [24]. In our study, we found that four of the investigated markers, namely BDNF, IL-8, PlGF, and GFAP showed statistically significant differences in plasma concentrations between GBM and ICM cases. Using a stepwise logistic regression model with internal bootstrap validation, we found that blood markers have the potential to distinguish unifocal supratentorial GBMs from ICMs in case of a supratentorially located singular contrast-enhancing lesion with an AUC value of 0.73 (p < 0.05), a value that is considered to indicate a good diagnostic potential [20]. In our dataset, plasma GFAP and plasma PlGF showed to be the most promising marker. Our exploratory data demonstrate that presence of GFAP and absence of PlGF in the plasma associates with GBM and thus may support the neuroradiological differential diagnosis of GBM versus ICM, although measurement of these markers does not have the potential to replace histological diagnosis. In addition, as none of the other tumor types investigated showed detectable plasma GFAP levels, this may help to distinguish rare cases with atypical neuroradiological appearance from glioblastoma. Our findings should be further evaluated with larger prospective cohorts. Furthermore, it would be also interesting to study the plasma concentrations of these markers in other lesions with a similar neuroradiological appearance, e.g., abscesses or lymphomas, or to correlate metabolic tumor characteristics (e.g., MR spectroscopy data) to blood biomarker concentrations.
Analyzing the association of plasma markers with tumor grade, we detected (1) inverse associations of plasma–NPY concentrations with tumor grade both in glioma and meningioma cases, (2) an inverse association of IL8 plasma concentration with tumor grade in glioma, and (3) a positive association of plasma–PlGF concentrations with tumor grade in meningioma. We can only speculate on the reasons for these findings. Changes in NPY homeostasis associated with stress response, anxiety or metabolism may be responsible for the observed differences in NPY plasma levels in gliomas and meningiomas of different grades. Interestingly, brain tumor development has been linked to decreases in NPY–mRNA expression in mouse brain [22] and it has been reported that NPY receptors are highly associated with higher grades of gliomas and are also expressed in meningiomas [25]. It seems conceivable that expression of NPY or its receptors may be pathogenetically linked to glioma or meningioma progression and NPY detectability in the blood. The clinical utility of the association of NPY, PlGF, and IL8 with tumor grade in glioma and meningioma, respectively, remains unclear, as the low number of cases prevented meaningful statistical exploration of the diagnostic potential of these markers in our study.
Survival analysis did not reveal a statistically significant association of blood plasma concentration of any of the investigated markers with survival times in GBM patients. However, it must be noted that the statistical power of our survival analyses was limited, as clinical follow-up data were only available in 27 cases. Of note, we observed a trend towards more favorable survival times of GBM patients with detectable plasma GFAP as compared to GBM patients without detectable plasma GFAP. Although this result is not statistically significant, it may reflect the findings of a previous study that showed decreasing GFAP expression with increasing malignancy grade of gliomas [23].
This study was performed in an explorative manner and surely includes some limitations. One important limitation is that we could analyze plasma concentrations of only one marker in control and MS subjects due to the lack of sample volumes. We selected GFAP, as this marker showed the most distinct association with a given diagnosis, namely GBM. A second limitation of the plasma analyses for different parameters is rather a technical issue that commercially available ELISA tests measures only the concentrations which are above the level of detection given for each assay. Therefore, we had to categorize seven out of eight plasma markers according to their detectability as detectable vs. nondetectable which unfortunately associates with loss of information. While we used ELISA kits for detection of selected markers, proteomic-based approaches may enable the measurement of a broader spectrum of proteins. Another arguable limitation of our study may be that in 28 patients there was no histological investigation of the cerebral lesion diagnosed as ICM based on clinical history and neuroradiology. These patients presented with histologically confirmed primary noncentral nervous system tumors and intracerebral lesions with the typical neuroradiological appearance of ICM. According to common practice at our and other centers, histological confirmation of intracerebral metastatic lesions is not mandatory prior to the treatment with radiosurgery or radiotherapy, although a study published in 1990 reported that 11 % of suspected brain metastases were not confirmed by histology [35]. However, we believe that the presentation of our patients as assessed by modern multimodal high-field MRI imaging (3 T) was typical enough to make our findings reliable despite the missing formal verification of ICM by histology. Therefore, we decided to include such patients in our analyses in order to increase the statistical power of our models.
To summarize the most interesting finding of our study, our data indicate that GFAP and PlGF are potentially useful as clinical biomarkers that may support neuroradiological differential diagnosis of GBM versus ICM. However, it should be noted that we can only conclude minor results derived from our study and none of the markers investigated showed the potential to replace histological diagnosis. We have initiated a prospective study investigating the dynamics of blood biomarker levels during the disease course of glioma patients.
References
Attems J, Preusser M, Grosinger-Quass M, Wagner L, Lintner F, Jellinger K (2008) Calcium-binding protein secretagogin-expressing neurones in the human hippocampus are largely resistant to neurodegeneration in Alzheimer's disease. Neuropathol Appl Neurobiol 34:23–32
Azad NS, Annunziata CM, Steinberg SM, Minasian L, Premkumar A, Chow C, Kotz HL, Kohn EC (2008) Lack of reliability of CA125 response criteria with anti-VEGF molecularly targeted therapy. Cancer 112:1726–1732
Batchelor TT, Duda DG, di Tomaso E, Ancukiewicz M, Plotkin SR, Gerstner E, Eichler AF, Drappatz J, Hochberg FH, Benner T, Louis DN, Cohen KS, Chea H, Exarhopoulos A, Loeffler JS, Moses MA, Ivy P, Sorensen AG, Wen PY, Jain RK (2010) Phase II study of cediranib, an oral pan-vascular endothelial growth factor receptor tyrosine kinase inhibitor, in patients with recurrent glioblastoma. J Clin Oncol 28:2817–2823
Benarroch EE (2009) Neuropeptide Y: its multiple effects in the CNS and potential clinical significance. Neurology 72:1016–1020
Bender R, Lange S (2001) Adjusting for multiple testing—when and how? J Clin Epidemiol 54:343–349
Berglund A, Molin D, Larsson A, Einarsson R, Glimelius B (2002) Tumour markers as early predictors of response to chemotherapy in advanced colorectal carcinoma. Ann Oncol 13:1430–1437
Brat DJ, Bellail AC, Van Meir EG (2005) The role of interleukin-8 and its receptors in gliomagenesis and tumoral angiogenesis. Neuro Oncol 7:122–133
Brochez L, Naeyaert JM (2000) Serological markers for melanoma. Br J Dermatol 143:256–268
Brommeland T, Rosengren L, Fridlund S, Hennig R, Isaksen V (2007) Serum levels of glial fibrillary acidic protein correlate to tumour volume of high-grade gliomas. Acta Neurol Scand 116:380–384
Christensen JG, Vincent PW, Klohs WD, Fry DW, Leopold WR, Elliott WL (2005) Plasma vascular endothelial growth factor and interleukin-8 as biomarkers of antitumor efficacy of a prototypical erbB family tyrosine kinase inhibitor. Mol Cancer Ther 4:938–947
Ekblad E, Edvinsson L, Wahlestedt C, Uddman R, Hakanson R, Sundler F (1984) Neuropeptide Y co-exists and co-operates with noradrenaline in perivascular nerve fibers. Regul Pept 8:225–235
Eng LF, Ghirnikar RS, Lee YL (2000) Glial fibrillary acidic protein: GFAP-thirty-one years (1969–2000). Neurochem Res 25:1439–1451
Englund AT, Geffner ME, Nagel RA, Lippe BM, Braunstein GD (1991) Pediatric germ cell and human chorionic gonadotropin-producing tumors. Clinical and laboratory features. Am J Dis Child 145:1294–1297
Frota ER, Rodrigues DH, Donadi EA, Brum DG, Maciel DR, Teixeira AL (2009) Increased plasma levels of brain derived neurotrophic factor (BDNF) after multiple sclerosis relapse. Neurosci Lett 460:130–132
Gartner W, Ilhan A, Neziri D, Base W, Weissel M, Wohrer A, Heinzl H, Waldhor T, Wagner L, Preusser M (2010) Elevated blood markers 1 year before manifestation of malignant glioma. Neuro Oncol 12:1004–1008
Gartner W, Lang W, Leutmetzer F, Domanovits H, Waldhausl W, Wagner L (2001) Cerebral expression and serum detectability of secretagogin, a recently cloned EF-hand Ca(2+)-binding protein. Cereb Cortex 11:1161–1169
Hamaya K, Doi K, Tanaka T, Nishimoto A (1985) The determination of glial fibrillary acidic protein for the diagnosis and histogenetic study of central nervous system tumors: a study of 152 cases. Acta Med Okayama 39:453–462
Harada A, Sekido N, Akahoshi T, Wada T, Mukaida N, Matsushima K (1994) Essential involvement of interleukin-8 (IL-8) in acute inflammation. J Leukoc Biol 56:559–564
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Hosmer DW, Lemeshow S (2000) Applied logistic regression. Wiley, New York
Hu Y, Wang YD, Guo T, Wei WN, Sun CY, Zhang L, Huang J (2007) Identification of brain-derived neurotrophic factor as a novel angiogenic protein in multiple myeloma. Cancer Genet Cytogenet 178:1–10
Ilyin SE, Gayle D, Gonzalez-Gomez I, Miele ME, Plata-Salaman CR (1999) Brain tumor development in rats is associated with changes in central nervous system cytokine and neuropeptide systems. Brain Res Bull 48:363–373
Jacque CM, Vinner C, Kujas M, Raoul M, Racadot J, Baumann NA (1978) Determination of glial fibrillary acidic protein (GFAP) in human brain tumors. J Neurol Sci 35:147–155
Jung CS, Foerch C, Schanzer A, Heck A, Plate KH, Seifert V, Steinmetz H, Raabe A, Sitzer M (2007) Serum GFAP is a diagnostic marker for glioblastoma multiforme. Brain 130:3336–3341
Korner M, Reubi JC (2008) Neuropeptide Y receptors in primary human brain tumors: overexpression in high-grade tumors. J Neuropathol Exp Neurol 67:741–749
Kos K, Harte AL, James S, Snead DR, O'Hare JP, McTernan PG, Kumar S (2007) Secretion of neuropeptide Y in human adipose tissue and its role in maintenance of adipose tissue mass. Am J Physiol Endocrinol Metab 293:E1335–1340
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, Khoury J (1996) The ABCs of measuring intracerebral hemorrhage volumes. Stroke 27:1304–1305
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452
Lee YB, Nagai A, Kim SU (2002) Cytokines, chemokines, and cytokine receptors in human microglia. J Neurosci Res 69:94–103
Lin LF, Doherty DH, Lile JD, Bektesh S, Collins F (1993) GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons. Science 260:1130–1132
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. IARC, Lyon
Mariani L, Miceli R, Michilin S, Gion M (2009) Serial determination of CEA and CA 15.3 in breast cancer follow-up: an assessment of their diagnostic accuracy for the detection of tumour recurrences. Biomarkers 14:130–136
McDavid K, Lee J, Fulton JP, Tonita J, Thompson TD (2004) Prostate cancer incidence and mortality rates and trends in the United States and Canada. Public Health Rep 119:174–186
Nomura M, Yamagishi S, Harada S, Yamashima T, Yamashita J, Yamamoto H (1998) Placenta growth factor (PlGF) mRNA expression in brain tumors. J Neurooncol 40:123–130
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500
Pipp I, Wagner L, Rossler K, Budka H, Preusser M (2007) Secretagogin expression in tumours of the human brain and its coverings. APMIS 115:319–326
Przedborski S, Goldman S, Schiffmann SN, Vierendeels G, Depierreux M, Levivier M, Hildebrand J, Vanderhaeghen JJ (1988) Neuropeptide Y, somatostatin, and cholecystokinin neurone preservation in anaplastic astrocytomas. Acta Neuropathol 76:507–510
Rickmann M, Wolff JR (1995) Modifications of S100-protein immunoreactivity in rat brain induced by tissue preparation. Histochem Cell Biol 103:135–145
Saavedra A, Baltazar G, Duarte EP (2008) Driving GDNF expression: the green and the red traffic lights. Prog Neurobiol 86:186–215
Straten G, Eschweiler GW, Maetzler W, Laske C, Leyhe T (2009) Glial cell-line derived neurotrophic factor (GDNF) concentrations in cerebrospinal fluid and serum of patients with early Alzheimer's disease and normal controls. J Alzheimers Dis 18:331–337
Tjwa M, Luttun A, Autiero M, Carmeliet P (2003) VEGF and PlGF: two pleiotropic growth factors with distinct roles in development and homeostasis. Cell Tissue Res 314:5–14
Vogelbaum MA, Masaryk T, Mazzone P, Mekhail T, Fazio V, McCartney S, Marchi N, Kanner A, Janigro D (2005) S100beta as a predictor of brain metastases: brain versus cerebrovascular damage. Cancer 104:817–824
Wagner L, Oliyarnyk O, Gartner W, Nowotny P, Groeger M, Kaserer K, Waldhausl W, Pasternack MS (2000) Cloning and expression of secretagogin, a novel neuroendocrine- and pancreatic islet of Langerhans-specific Ca2+-binding protein. J Biol Chem 275:24740–24751
Wiesenhofer B, Stockhammer G, Kostron H, Maier H, Hinterhuber H, Humpel C (2000) Glial cell line-derived neurotrophic factor (GDNF) and its receptor (GFR-alpha 1) are strongly expressed in human gliomas. Acta Neuropathol 99:131–137
Wohrer A, Waldhor T, Heinzl H, Hackl M, Feichtinger J, Gruber-Mosenbacher U, Kiefer A, Maier H, Motz R, Reiner-Concin A, Richling B, Idriceanu C, Scarpatetti M, Sedivy R, Bankl HC, Stiglbauer W, Preusser M, Rossler K, Hainfellner JA (2009) The Austrian Brain Tumour Registry: a cooperative way to establish a population-based brain tumour registry. J Neurooncol 95:401–411
Yamamoto H, Gurney ME (1990) Human platelets contain brain-derived neurotrophic factor. J Neurosci 10:3469–3478
Yan Q, Yu HL, Li JT (2009) Study on the expression of BDNF in human gliomas. Sichuan Da Xue Xue Bao Yi Xue Ban 40:415–417
Acknowledgments
This work was supported by the Anniversary Fund (Jubilaeumsfonds) of the Austrian National Bank, project number: 13402.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Benedicto Oscar Colli, Ribeirão Preto, Brasil
I would like to congratulate the authors for this interesting work on tumor biology. Identification of biological markers in the blood associated with tumors probably will be the key for precocious detection of tumors and, we hope, even before the tumor starts to develop and this paper is a practical evidence of the utility of molecular biology. Using imunohistochemistry detection of some biological markers in the blood, the authors intended to associate these markers with primary and secondary tumors of the central nervous system, a topic not so much explored in the literature.
The authors appropriately comment the weak points of the study, emphasizing the small sample number for some tumors (low-grade gliomas and meningiomas) and the lack of histopathological diagnosis for most part (62.3 %) of patients with supposed brain metastasis that precluded stronger conclusions. Besides of this, only one marker was analyzed in the control group and in the group with multiple sclerosis due the small amount volume of the samples. Another problem was a technical limitation due to the fact that commercial kits for plasma analysis measures only the concentrations which are above the level of detection givens for each assay and, therefore, the measures were done according to their detectability (detectable vs. nondetectable), which causes loss of information.
Their results were submitted to very meticulous and sophisticated statistical analysis that allowed confidence on the results.
The main conclusion was that presence of GFAP (glial fibrillary acidi protein) in the plasma was more frequent in patients with glioblastoma multiforme and PlGF (placental growth factor) was more frequent in patients with brain metastasis and this can help in the differentiation of these tumors before histopathological analysis.
Additionally, it was also suggested, without statistical significance, that patients with glioblastoma and with GFAP detected in the plasma has better survival than patients that had not GFAP detected in the plasma. It was also noted inverses association of plasma–NPY concentrations with tumor grade for gliomas and meningiomas, an inverse association of IL8 plasma concentration with tumor grade in gliomas, and a positive association of plasma–PlGF concentrations with tumor grade in meningiomas.
The results of this study are promising and if confirmed and more explored with adequate samples of tumors, they can be a valuable contribution for diagnosis and prognosis of tumors of the central nervous system.
Tamas Doczi, Pecs, Hungary
Conventional structural imaging provides limited information on tumor characterization and prognosis. Advances in neurosurgical techniques, radiotherapy planning and novel drug treatments for malignant brain tumors have generated increasing need for reproducible, noninvasive, quantitative imaging biomarkers such as physiological MRI and PET molecular imaging that help in understanding metabolic processes associated with tumor growth, blood flow and fine structure. Despite their added value, the effect of these imaging biomarkers as an adjunct to structural imaging in clinical research and practice have remained rather limited. Searching for systemic biomarkers of intracerebral pathologies is also of major interest. Blood markers for CNS tumors, if identified, would be of great value for allowing differential diagnosis without obtaining tissue and for diagnosing recurrences of CNS tumors. This latter would be of considerable value especially in the case of malignant gliomas where pseudo-progression is a common clinical problem. The authors investigated at 8 of traditional and some novel candidate plasma markers. Their present results and conclusions are limited by the small number of probands. The study in the present form does not help the reader to get a definite answer to the question, are molecular biomarkers in neuro-oncology ready for clinical practice? The study presents tendencies rather than definite differences, with the exception of the authors’ (non-novel) observation of higher GFAP levels in GBM patients than in metastasis patients.
However, this prospective exploratory study investigating the blood plasma concentrations of several distinct proteins and their association with cerebral tumor type and neuroradiological features in adult brain tumor patients may help neurosurgeons to get acquainted with potential areas for which biomarkers can improve patient care. It may range from early detection and diagnosis, prediction of response or toxicity of therapy and prognosis. Blood markers can also potentially improve the efficiency of the development of novel treatment approaches.
James T Rutka, Toronto, Canada
The authors have examined the role of plasma biomarkers in 105 adult brain tumor patients who had a variety of different tumor types. They chose, a priori, 8 different biomarkers that were selected on the basis of their known involvement in processes that affect the growth of cells within the central nervous system. The concentrations of these biomarkers were correlated with clinicopathological data. In the end, they show that GFAP was a strongly associated biomarker with GBM, and GFAP and PlGF were promising in differentiating between GBM and unifocal supratentorial metastasis.
This is an important study because any attempt at establishing a diagnosis of an intracranial brain tumor by minimally invasive strategies, such as a blood marker, would be extremely valuable. A lot of energy and effort now are being directed at establishing such biomarkers in a host of different cancer types. Ideally, we would like to see the sensitivity and specificity of a biomarker that is wholly diagnostic and prognostic such as is the case with certain intracranial germ cell tumors that express alpha fetoprotein, or human chorionic gonadotropin to give some examples.
As the field of proteomics expands, and as the detection of rare proteins at low concentrations becomes possible, we can look forward to the establishment of unique biomarkers for various brain tumors which have hitherto gone undetected. I congratulate the authors for this interesting body of work.
Walter Stummer, Münster, Germany
This is an analysis of potential blood markers for CNS tumors. Such blood markers, if identified, would be of great value for allowing differential diagnosis without obtaining tissue and for diagnosing recurrences of CNS tumors. The latter would be of considerable value especially in the case of malignant gliomas where phenomena as pseudo-progression or pseudo-response are a common clinical problem. The authors investigate a number of traditional and some novel candidate plasma markers.
However, the results and conclusions are limited by the small number of patients and require careful scrutiny, with the exception of the authors’ (non-novel) observation of higher GFAP levels in GBM patients than in those with metastastic tumors. To be more convincing, this dataset needs to be validated in an independent sample or, in a first step, should be expanded to a larger group of patients. It would be of particular interest to test the markers in recurrent glioblastomas. In my experience these tumors pose much more of a formidable clinical problem than discerning a malignant glioma from a metastasis.
Enver Bogdanov and A. Zabbarova, Kazan, Russia
Ilhan-Mutlu A., Preusser M. and co-authors present the results of the research of eight circulation plasma markers in brain tumor patients. In the panel of investigated proteins authors used six known and 2 new for the neurooncological patients’ substances. Results of this study indicate that 2 proteins (GFAP and PIGF) are potentially useful as clinical biomarkers that may support neuroradiological differential diagnosis of glioblastoma multiforme versus intracerebral metastasis. None of the markers investigated in this study showed the potential to replace histological diagnosis.
This research is based on sufficient clinical material and references and is of big practical interest. At the same time, as noted by the authors themselves, this study requires further. The search for new markers, a comparison of markers in plasma and in CSF, the expansion of the number of patients enrolled in the study and analysis of their neurological status and outcomes is an important for the screening, early diagnosis and prognosis of the patients, as well as to clarify the classification of brain tumors and to identify possible paraneoplastic syndroms.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
ESM 1
Plasma marker detectability according to tumor type and neuroradiological parameters. Statistically significant group differences are highlighted (gray background; p < 0.05, tumor volume was assessed using Mann–Whitney U test, all other variables were analyzed using chi-square test). BDNF brain-derived neurotrophic factor, GDNF glial cell line-derived neurotrophic factor, GFAP glial fibrillary acidic protein, IL8 interleukin 8, M median, NPY neuropeptide Y, R range (calculated at least from two positive values), PlGF placental growth factor, SCGN secretagogin. Tumor volume is demonstrated in median with minimum and maximum (XLS 36 kb)
ESM 2
Plasma marker detectability according to tumor type and anatomical localization. There was no statistically significant association of plasma marker detectability with tumor localization (all p > 0.05, logistic regression). Tumor volume is demonstrated in median with minimum and maximum and was assessed using Kruskal–Wallis test. BDNF brain-derived neurotrophic factor, GDNF glial cell line-derived neurotrophic factor, GFAP glial fibrillary acidic protein, IL8 interleukin 8, NPY neuropeptide Y, PlGF placental growth factor, SCGN secretagogin (XLS 22 kb)
Rights and permissions
About this article
Cite this article
Ilhan-Mutlu, A., Wagner, L., Widhalm, G. et al. Exploratory investigation of eight circulating plasma markers in brain tumor patients. Neurosurg Rev 36, 45–56 (2013). https://doi.org/10.1007/s10143-012-0401-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0401-6