Abstract
Malignant gliomas are highly lethal tumors resistant to current therapies. The standard treatment modality for these tumors, surgical resection followed by radiation therapy and concurrent temozolomide, has demonstrated activity, but development of resistance and disease progression is common. Although oncogenic Ras mutations are uncommon in gliomas, Ras has been found to be constitutively activated through the action of upstream signaling pathways, suggesting that farnesyltransferase inhibitors may show activity against these tumors. We now report the in vitro and orthotopic in vivo results of combination therapy using radiation, temozolomide and lonafarnib (SCH66336), an oral farnesyl transferase inhibitor, in a murine model of glioblastoma. We examined the viability, proliferation, farnesylation of H-Ras, and activation of downstream signaling of combination-treated U87 cells in vitro. Lonafarnib alone or in combination with radiation and temozolomide had limited tumor cell cytotoxicity in vitro although it did demonstrate significant inhibition in tumor cell proliferation. In vivo, lonafarnib alone had a modest ability to inhibit orthotopic U87 tumors, radiation and temozolomide demonstrated better inhibition, while significant anti-tumor activity was found with concurrent lonafarnib, radiation, and temozolomide, with the majority of animals demonstrating a decrease in tumor volume. The use of tumor neurospheres derived from freshly resected adult human glioblastoma tissue was relatively resistant to both temozolomide and radiation therapy. Lonafarnib had a significant inhibitory activity against these neurospheres and could potentate the activity of temozolomide and radiation. These data support the continued research of high grade glioma treatment combinations of farnesyl transferase inhibitors, temozolomide, and radiation therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioma is the most common type of primary brain tumor diagnosed in the United States. The standard of care for this disease includes a multi-modal approach usually involving surgical resection, radiation therapy, and chemotherapy [1] with temozolomide [2]. Despite this aggressive treatment regimen, glioblastoma (GBM) remains highly lethal, with a median survival time of approximately 1 year [3]. With its extensive infiltrative and aggressive nature, GBM is highly refractory to the current available therapies.
At the molecular and genetic levels, epidermal growth factor receptor (EGFR) activation, loss of or mutation in p53, aberrant telomerase activity, and loss of phosphatase and tensin homolog (PTEN) are commonly observed in glioma [4–8]. Receptor tyrosine kinases (RTKs) such as the EGFR can function, in part, through activation of the Ras/Raf/Mitogen-Activated protein kinase (MAPK) signaling cascade. Thus, it is not surprising that EGFR upregulation of Ras signaling is one of the major intracellular pathways implicated in glioma growth and development [9–12].
Although activating Ras mutations are quite common in many types of cancer, such mutations are very rare in gliomas. Thus, the elevation of Ras activity characteristic of this disease is predominantly wild type. This aspect of biology suggests gliomas may be sensitive to the effects of a farnesyltransferase inhibitor (FTI). FTIs block the farnesylation of Ras, and render it unable to associate with the plasma membrane. Unfarnesylated Ras remains cytosolic and can not participate in intracellular signaling. Tipifarnib (R115777) has completed phase I testing both alone [13] and in combination with radiation therapy [14] and has been well tolerated. Lonafarnib (SCH66336, Sarasar®, Schering-Plough) is another potent orally active tricyclic FTI with less myelosuppressive side effects, now in clinical trials [15, 16]. Lonafarnib, which competes with the CAAX peptide substrate motif, blocks farnesyltransferase activity in vitro with an IC50 value of 1–2 nM.
Recent evidence indicates FTIs may be capable of exploiting some of the molecular characteristics of glioma. For example, it has been reported that tumors with endogenous Ras activation are more resistant to radiation therapy (XRT) than those in which Ras activity has been blocked [17–20], and the use of FTIs to inhibit activated Ras in human tumor cells resulted in XRT sensitization in vitro [21]. Moreover, cells with amplification of EGFR, which is common in GBM, have been shown to be more sensitive to lonafarnib in vitro [22].
Given this evidence, we tested whether the addition of an FTI given concurrently with the standard of care would potentiate the anti-tumor effects in an orthotopic model of glioma. In this study, we looked for preclinical evidence of synergy or additive effects of combination therapy including XRT, temozolomide (Tem), and lonafarnib. We found the addition of the FTI lonafarnib to a regimen of concomitant XRT and Tem enhanced growth inhibition in vitro and in vivo. Our data suggest the addition of a FTI to the current standard of care for gliomas should be evaluated for its ability to improve the outcome of glioma patients.
Materials and methods
Cell culture and luciferase expression
U87 human glioma cells (American Type Culture Collection, Manassas, VA) expressing MGMT as determined by immunohistochemistry were cultured in DMEM with 10% FCS (Invitrogen/GIBCO, Carlsbad, CA). The coding sequences for luciferase and neomycin phosphotransferase were fused and introduced into a pMMP retrovirus (Richard Mulligan, Children’s Hospital, Boston), generating pMMP-LucNeo. pMMP-LucNeo was packaged in 293T cells by cotransfection with plasmids encoding helper functions (from pMD murine leukemia virus) and vesicular stomatitis virus (VSV)-G envelope protein (pMD-G; Richard Mulligan). Pseudotyped VSV-G was applied to cells with 8 μg/ml polybrene (Sigma, St. Louis, MO). LucNeo-expressing U87 cells were selected in growth media supplemented with 1 mg/ml G418 (Invitrogen/GIBCO, Carlsbad, CA).
In vivo drug prep, dosing, and XRT
lonafarnib (SCH66336, Sarasar®) and Temozolomide (Temodar®, Tem) were kindly provided by Schering-Plough (Kenilworth, NJ). Drugs were reconstituted in 4% DMSO in 20% (2-hydroxypropyl)-β-cyclodextrin in PBS. Lonafarnib was given once daily at 80 mg/kg with twice weekly weightings to ensure accurate dosing. Tem was given by gavage at 5 mg/kg 90 min prior to XRT. For irradiation, anesthetized mice were placed in a lead shielding apparatus which limited radiation exposure to the head only. Treatment (2.5 Gy/day for 2 days) was delivered using a Gammacell 40 (MDS Nordion, Ottawa, Canada) irradiator delivering 100 rads/min. For in vivo combination experiments, suboptimal doses of XRT/Tem were selected to permit identification of synergistic effects of lonafarnib.
In vitro drug stocks, treatments, and XRT
Drugs were reconstituted in DMSO and stock solutions (10 mM Lonafarnib, 25 mM Tem) were stored at −20°C. Drugs were diluted in culture media and fresh media was prepared and applied to cells every 24 h. For XRT, culture plates were irradiated using a GammaCell 1000 (MDS Nordion, Ottawa, Canada) at a rate of 80 rads/min.
Non-radioactive MTS cytotoxicity assay
CellTiter96 Aqueous Assay kit was purchased from Promega (Madison, WI). Assays were performed under manufacturer’s instructions with 5000 cells/well in a 96-well tissue culture plate. Plates were irradiated 24 h after drug exposure and assayed 96 h after XRT, with fresh drug treatments applied each day. For quantification, dye was added directly to each well, plates were washed as per the manufactures recommendation and cell viability determined by optical density. Significance was analyzed using the Student’s t-test.
Proliferation assay
12-well plates were seeded with 100,000 cells/well. Drug treatments were initiated 24 h after plating, and media was replaced every 24 h for a total of 96 h of drug exposure. Plates were irradiated after 24 h of drug exposure. Cells from triplicate sets of treatments were trypsonized and counted 48 h after irradation using a Z1 series coulter counter (Beckman Coulter, Fullerton, CA), and compared to cell numbers from wells counted on Day 1 (the day drug treatment was initiated). Proliferation after drug treatments were normalized to the control wells and expressed as % of the control treatment. Significance was analyzed using the Student’s t-test.
Downstream pathway analysis
2.5 × 106 cells per 100 mm3 dish were seeded, and drug treatments initiated 24 h after plating. Plates were irradiated after 24 h of drug exposure, and cells were lysed after 48 h of drug exposure (24 h after XRT). Total protein was extracted with ice-cold T-Per (Pierce, Rockford, IL) supplemented with protease and phosphatase inhibitors, and quantitated using the BCA protein assay kit (Pierce, Rockford, IL). 500 μg of total protein was used to probe different Human Phospho-RTK Human Phospho-MAPK Arrays (R&D Systems, Minneapolis, MN). Arrays were washed and developed according to manufacturer’s instructions, and exposed to film. Films were scanned using a flatbed scanner, and dots were quantitated using ImageJ (NIH, Bethesda, MD). Relative changes between treatment groups were expressed as percentage of control, with significance assessed by Student’s t-test.
Western blotting of H-Ras
2.5 × 106 cells per 100 mm3 dish were seeded, and drug treatments initiated 24 h after plating. Plates were irradiated after 24 h of drug exposure, and cells were lysed after 48 h of drug exposure (24 h after XRT). Total protein was extracted with ice-cold T-Per (Pierce, Rockford, IL) supplemented with protease and phosphatase inhibitors, and quantitated using the BCA protein assay kit (Pierce, Rockford, IL). Samples (20 μg total protein) were run on 4–15% Tris HCl SDS-PAGE Criterion gels (Biorad, Hercules, CA) and probed for
H-Ras (1:500 Santa Cruz Biotech, Santa Cruz, CA) and α-tubulin (1:5000, Sigma, St. Louis, MO) as an internal loading control. Blots were exposed to film, and films were scanned using a flat bed scanner. Bands were quantitated using ImageJ (NIH, Bethesda, MD), and graphed using Excel (Microsoft, Redmond, WA). H-Ras was normalized to the loading control and expressed as a % of the control treatment. Significance was assessed using the Student’s t-test.
Tumor cell line xenografts
Tumor cell lines were harvested in mid-logarithmic growth phase and resuspended in PBS. Homozygous NCR nude mice (Taconic Farms, Hudson, NY) were anesthetized with Ketamine/Xylazine before exposure of the cranium and removal of the periosteum with a size 34 inverted cone burr (Roboz, Gaithersburg, MD). Mice were fixed in a stereotactic frame (Stoelting, Wood Dale, IL), and 5 × 104 cells in 10 μl of PBS were injected through a 27-gauge needle over 5 min at 2 mm lateral and posterior to the bregma and 3 mm below the dura. The incision was closed with staples. Animals were observed daily for signs of distress or development of neurologic symptoms at which time the mice were sacrificed.
In vivo imaging
Mice were anesthetized with Ketamine/Xylazine, injected with d-luciferin at 50 mg/kg i.p. (Promega, Madison, WI), and imaged with the Xenogen IVIS 100 Imaging System for 10–120 s, bin size 2 as previously published [23, 24]. To quantify bioluminescence, identical circular regions of interest were drawn to encircle the entire head of each animal, and the integrated flux of photons (photons per second) within each region of interest was determined by using the Xenogen LIVING IMAGES software package. Data were normalized to bioluminescence at the initiation of treatment for each animal. Statistical significance was assessed using the Student’s t-test.
Glioma neurosphere assay
Collection and use of fresh and discarded human tumor tissue was approved by the Brigham and Women’s Hospital Institutional Review Board. After frozen section diagnosis of malignant glioma by the attending neuropathologist, tumor material was grossly dissected from the tissue sample. Portions of the tumors were collected in chilled media for the studies described here and other portions were allocated for paraffin embedding for histological diagnosis and for genotyping. Expansion of tumor material and propagation was accomplished by subcutaneous implantation in Icr SCID mice (cells were never grown on plastic). When tumors reached ~1 cm, tumors were disaggregated, cells were counted and then grown in serum-free media with EGF, FGF and LIF as described previously to form tumorspheres [25, 26]. Drugs (SCH 5uM, TMZ 100uM) were added immediately after plating cells into 24 well plates and radiation given at 24 h after plating and tumor neurospheres were counted in triplicate 10 days after plating.
Results
Enhanced cytotoxic and anti-proliferative effects of lonafarnib (SCH66336)/XRT/Tem combination in U87 glioma cells in vitro
The effect of lonafarnib, and different combinations of lonafarnib, XRT, and Tem on U87 cytotoxicity in vitro were examined over a wide range of doses using the standard MTS assay (Promega, Madison, WI). Doses of XRT and Tem were designed to provide a small but significant decrease in proliferation alone (91 and 76%, respectively) and a moderate effect in combination (71%) to allow easy identification of synergistic action with lonafarnib (Fig. 1a). Lonafarnib alone or SCH/Tem did not induce dramatic U87 cell cytotoxicity in vitro at physiologically achievable doses (<10 μM, Fig. 1a). Lonafarnib/XRT/Tem was significantly more effective than lonafarnib alone (65 vs. 85%, respectively, P < 0.001), but cell viability still remained high (Fig. 1a). Although we did find an increase in U87 cytotoxicity, it was difficult to determine the added benefit of the combination treatment with this method. To further analyze the effects of the combination we employed a traditional proliferation assay. Lonafarnib alone, at the lowest dose (5 μM) was significantly more effective in blocking U87 proliferation than XRT/Tem (54% proliferation vs. 83%, respectively, P < 0.01, Fig. 1b) although increasing doses of lonafarnib did not further increase the effect. Combination of lonafarnib/XRT/Tem enhanced inhibition of proliferation and was more effective than either lonafarnib alone or XRT/Tem (24% proliferation with lonafarnib/XRT/Tem vs. 54% with 5 μM lonafarnib, and 83% with XRT/Tem, P < 0.001). This assay clearly showed the impact of adding lonafarnib to the standard of XRT/Tem. In vitro dosages of 10 μM lonafarnib and 100 μM Tem, which are physiologically achievable in vivo, were chosen for subsequent experiments based on cytotoxicity and proliferation data.
Combination treatment has an effect on U87 cell cytotoxicty and proliferation in vitro (a) Lonafarnib alone or SCH/Tem (10 μM/100 μM) induced some U87 cell cytotoxicity compared to vehicle treated control while SCH/XRT/Tem was notably more effective than lonafarnib alone, but cell viability still remained high. b Combination treatment has a strong synergistic effect on U87 cell proliferation. The combination of SCH/XRT/Tem displayed significantly more inhibition than lonafarnib alone (5 μM 0 versus 6 Gy P < 0.001, 10 μM 0 versus 6 Gy P < 0.001, 15 μM 0 versus 6 Gy P < 0.001). The number of cells per well of quadruplicate treatments was normalized to control and plotted as the mean ± s.e.m. Statistical significance was determined by Student’s t-test (**P < 0.01, ***P < 0.001). Results are representative of three independent experiments
Farnesylation of H-Ras is inhibited by lonafarnib (SCH66336) alone and in combination with XRT and Tem, but not XRT, Tem, or XRT/Tem in vitro
In order to assess the immediate downstream effects of lonafarnib and ascertain whether the in vitro levels were sufficient to inhibit farnesylation of H-Ras, we examined the level of farnesylation of H-Ras in response to combinations of lonafarnib (10 μM), XRT (6 Gy), and Tem (100 μM). Cells were treated for 24 h and then given a single pulse of XRT and a media change (drug containing). Cells were harvested for Western blot 24 h after the pulse of XRT. Two species of H-Ras were found, the upper band, unprocessed inactive Ras, and the faster migrating lower band which is farnesylated and active [27] (Fig. 2a). Treatment of U87 cells with XRT, Tem, or XRT/Tem were identical to control treated samples. Treatment with any combination including lonafarnib had a dramatic, near complete suppression of H-Ras farnesylation (lower band). When normalized for loading with α-tubulin, levels of H-Ras were found to be very consistent in all groups not exposed to lonafarnib (90–100% relative density, Fig. 2b). Interestingly, all treatment groups containing lonafarnib showed a significantly higher level of unfarnesylated H-Ras (116–137%) compared to control treatment (Fig. 2b).
Lonafarnib (SCH66336) blocks farnesylation and increases overall levels of H-Ras in vitro. a Lonafarnib alone strongly blocked the farnesylation of H-Ras protein, with the farneslylated form barely visible by immunoblot (lower band, active H-Ras). b Overall levels of H-Ras protein were also altered in any treatment containing lonafarnib. Levels of H-Ras were normalized to α-tubulin and plotted as the mean of three replicates ± s.e.m. Statistical significance of increased unfarnesylated H-Ras was determined by Student’s t-test (*P < 0.05, **P < 0.01). Results representative of three independent experiments
Effect of lonafarnib (SCH66336)/XRT/Tem combination treatment on signaling molecules in vitro
Next we characterized the activation state of some of the common signaling pathways after in vitro treatment of U87 cells with lonafarnib alone, lonafarnib/XRT, and lonafarnib/XRT/Tem. We examined both serine/threonine molecules associated with the MAPK pathways and RTK signaling components. Activation of the EGFR (phosphoEGFR, or pEGFR) was reduced by 44% with lonafarnib alone (P < 0.01), but this attenuation was lost with lonafarnib/XRT. Interestingly, the combination of lonafarnib/XRT/Tem resulted in a significant increase (126%, P < 0.01) of EGFR activation (Fig. 3a, b).
Combination treatment influences activation of MAPK and RTK pathways (a) representative Proteome Profiler (R&D Systems, Minneapolis MN) dot blot is shown for EGF receptor (EGFR). b Phosphorylation of EGFR was significantly attenuated by lonafarnib alone but reversed with the addition of XRT and Tem. Activation of pEphA7 was also highly suppressed with lonafarnib alone while ERK1 activation was slightly reduced by lonafarnib. Levels of p38δ were induced by SCH alone but not by SCH/XRT or SCH/XRT/Tem. The optical density of duplicate dots were normalized to control and plotted as the mean ± s.e.m. Statistical significance was determined by Student’s t-test (*P < 0.05, **P < 0.01, ***P < 0.001)
An effect of combination treatment was found on the hepatocyte growth factor receptor (HGFR, c-Met) phosphorylation. Lonafarnib alone caused a modest decrease of ~9% in HGFR activation (P < 0.05, Fig. 3b), while significant inhibition of HGFR activation was found with lonafarnib/XRT (51%, P < 0.001), and with the combination of lonafarnib/XRT/Tem (53%, P < 0.01). Another interesting finding was the effect of lonafarnib on the activation of the RTK EphA7 (Fig. 3b). Phosphorylation of this receptor, which is activated by a GPI-linked ephrin ligand, was significantly decreased by 63% in lonafarnib alone and lonafarnib/XRT (P < 0.05) and 58% by lonafarnib/XRT/Tem (P < 0.05).
Downstream elements commonly associated with Ras, ERK and p38δ showed changes in response to treatment (Fig. 3b). Activation of ERK1 was decreased to 82% with lonafarnib alone, although was not found to be statistically significant (P = 0.08), while the combination of lonafarnib/XRT caused a significant increase of phosphorylation (120%, P < 0.05). Treatment of U87 cells with lonafarnib/XRT/Tem resulted in significant reduction of ERK1 activation (81%, P < 0.05, Fig. 3b). p38δ showed a modest, but significant increase (113%, P < 0.05) in response to lonafarnib alone, and this increase was attenuated to control levels by the combination of lonafarnib/XRT/Tem (Fig. 3b and Supplemental Fig. 1).
Signaling through the PI3K/AKT pathway functions independently of Ras, and we found no significant effect on AKT with lonafarnib alone or in combination with XRT and Tem on U87 glioma cells in vitro (data not shown). We found little change in the activation of RSK, JNK1, or GSK-3α/β with lonafarnib alone, or with combination treatment (data not shown).
Addition of lonafarnib (SCH66336) potentiates the anti-tumor affect of XRT/Tem on orthotopic U87 glioma in vivo
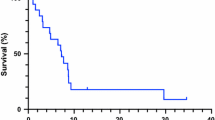
Given the encouraging in vitro data generated with the combination of lonafarnib/XRT/Tem, we next tested this drug regimen in vivo. Using an orthotopic murine model of U87 glioma we assessed the ability of lonafarnib alone and lonafarnib/XRT/Tem to block the growth of intracranial tumors. Lonafarnib alone (80 mg/kg by oral gavage, once daily) had limited ability to inhibit orthotopic U87 tumors compared to vehicle treated control animals (T/C of 0.67, Fig. 4a, b). The combination of XRT/Tem (2.5 Gy/day for 2 days; 5 mg/kg by oral gavage 90 min prior to XRT) was designed to produce modest tumor growth inhibition in vivo (T/C of 0.42). Concurrent lonafarnib/XRT/Tem (lonafarnib 80 mg/kg by oral gavage, once daily, XRT 2.5 Gy/day for 2 days, and Tem 5 mg/kg by oral gavage 90 min prior to XRT) provided the strongest growth reduction (T/C of 0.02) and was significantly more effective than XRT/Tem (P < 0.04), with the majority of animals demonstrating a decrease in tumor volume (P < 0.05, Fig. 4a, b) after 2 weeks and persisting after 4 weeks (P < 0.05, Fig. 4b).
Combination of SCH/XRT/Tem displays additional anti-tumor activity over XRT/Tem in in vivo orthotopic U87 gliomas (a) Lonafarnib alone was not effective in blocking intracranial tumor growth (n = 6) compared to vehicle treated control animals (n = 5). XRT/Tem treatment was designed to produce modest tumor growth inhibition so the effect of combination treatment could be assessed. b Combination of SCH/XRT/Tem displays additional anti-tumor activity over XRT/Tem in in vivo orthotopic U87 gliomas. Combination of SCH/XRT/Tem inhibited intracranial tumor growth. Relative tumor burden is plotted on the Y axis as the tumor volume relative to the day treatment is initiated. Statistical significance was determined by Student’s t-test (*P < 0.05) and are the average of the means of four different experiments
Addition of lonafarnib (SCH66336) potentiates the anti-tumor affect of XRT/Tem on human glioblastoma neurospheres in vitro
The utility of established tumor cell lines grown in serum to predict treatment response in vitro or in vivo remains controversial. To assess the activity of the combination of lonafarnib/XRT/Tem in a more clinically relevant model [28], we treated glioblastoma neurospheres derived from surgical specimens of adult glioblastoma. Lonafarnib alone demonstrated significant inhibition of neurosphere proliferation (lane 2) compared to temozolomide (lane 3), radiation (600 rad) (lane 5) and radiation + temozolomide (lane 7). The addition of lonafarnib to either temozolomide (lane 4), radiation (lane 6) or to radiation and temozolomide (lane 8) demonstrate almost complete inhibition of proliferation (Fig. 5). Thus, while radiation and/or temozolomide had only limited proliferation inhibition on this population, lonafarnib demonstrated significant activity alone compared to controls (lanes 1 versus 2, P < 0.0001, Fig. 5), and significantly improved the results when combined with radiation and temozolomide (lanes 7 versus 8, P < 0.001, Fig. 5).
Discussion
Glioma is the most common primary brain tumor diagnosed in the United States. The standard of care for a newly diagnosed adult high-grade glioma, GBM, is XRT and Temozolomide treatment. While active, this therapy is not curative in the vast majority of patients. Current clinical strategies are to augment the effectiveness of the current standard therapy by adding in novel chemotherapeutic and biological agents.
Excessive growth factor stimulation of glioma cells results in aberrant constitutive activity of Ras. The overabundance of Ras activity promotes glioma cell growth and proliferation, and is a target of novel anti-cancer drug design. FTIs block the activation of Ras by inhibiting its farnesylation, rendering it unable to associate with the plasma membrane which is required for its activity (Fig. 6). FTIs have been shown to block in vitro anchorage-dependent and anchorage-independent growth and proliferation of a variety of cancer cell lines [29–31]. In addition to blocking the activation of Ras, treatment of cancer cells in vitro with FTI has been shown to reverse radiation resistance and increase the sensitivity of the cells to XRT [17–21]. FTIs have little to no effect on normal cells in vitro and in vivo [32] and show little systemic toxicity in animal models [33, 34], supporting FTIs as promising agents for the treatment of cancer.
Schematic representation of the ras signaling pathway. Lonafarnib (SCH66336) blocks the farnesylation of Ras-GDP forcing it to remain in the cytoplasm where it cannot activate the Ras signal transduction pathway. Synergistic inhibition of tumor growth by lonafarnib after treatment with radiation and temozolomide suggests that resistance to DNA damage is mediated by Ras-GTP or other farnesylation dependent pathways. FT Farnesyl Group, FT Farnesyltransferase, SCH Lonafarnib (SCH66336), RTK receptor tyrosine kinase, XRT radiation therapy, TMZ temozolomide
Lonafarnib has been tested pre-radiation for adults with glioblastoma without significant activity [35] while it has shown promise in combination with the cytotoxic drug Paclitaxel in Non Small Cell Lung Cancer (NSCLC) [36]. This reinforces the development of combination therapies, which may provide additional efficacy. Our goal was to assess, in vitro and in vivo, if lonafarnib/XRT/Tem showed evidence of additive or synergistic activity in a preclinical model of GBM. We tested the effectiveness of the FTI lonafarnib in combination with XRT and Tem in vitro and an in vivo animal model of orthotopic U87 GBM as well as in adult glioblastoma derived tumorspheres. As predicted by previously published studies, lonafarnib alone had limited single agent activity in vitro and in vivo. We found lonafarnib did not induce dramatic cell death as measured by MTS cytotoxicity assay. In contrast, lonafarnib inhibited glioma cell proliferation, and showed marked increase in activity when combined with XRT and Tem. In vivo activity of lonafarnib may be related to a combination of the cytotoxic and antiproliferative effects.
Doses of lonafarnib used in our in vitro studies were sufficient to block activation of H-Ras in the U87 glioma cells, and are physiologically achievable in vivo. In addition to preventing the prenylation of H-Ras, overall levels of H-Ras protein were elevated in treatments including lonafarnib. This suggests accumulation of unprocessed H-Ras seen in other cell lines after treatment with an FTI [27, 37], is also found in the U87 cells.
To identify compensatory mechanisms a cell may upregulate after treatment with lonafarnib/XRT/Tem, we examined several RTK and MAPK signaling molecules after combination treatment. We found activation of EGFR was strongly inhibited in U87 cells in vitro by lonafarnib alone, but this effect was lost with lonafarnib/XRT, and activation was induced by lonafarnib/XRT/Tem. The response of the cell to damage by XRT/Tem resulting in increased activation of EGFR, perhaps as a survival mechanism as the cell tries to overcome the effects of XRT/Tem are of interest. We are investigating the possible significance of adding an EGFR inhibitor to the lonafarnib/XRT/Tem combination.
Ras is a major signaling mediator of EGFR and it has been reported that inhibition of Ras can feedback and block EGFR activation. We found EGFR activation was reduced after treatment with lonafarnib and dramatic synergy was found with lonafarnib/XRT/Tem combination treatment. Previous studies have reported near complete inhibition of EGFR expression and activation of EGFR in U-373 and T98G glioma cell lines after in vitro treatment with a FTI [38]. Our data support this bidirectional signaling in U87 glioma cells in vitro.
Although the Ras pathway is mostly known for its role in growth and transformation, it also has been shown to affect axon guidance and cell adhesion. The ephrin-Ras relationship has been shown to function in these processes. Eph receptors (EphR) are among the few RTKs that negatively regulate H-Ras and the downstream MAPK pathway in a wide range of cell lines in vitro. EphR negatively regulates the Ras/MAPK/ERK pathway through p120RasGAP, which inhibits the positive signals of Grb2/Sos [39–41]. We found that activation of EphA7 was dramatically inhibited by lonafarnib, alone and in combination with XRT/Tem. This unexpected finding was quite striking, and indicates the EphR may play a more significant role in cellular proliferation than previously thought. EphR activation can block the activation of the Ras/MAPK/ERK pathway by platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), and angiopoietin-1 (Ang-1), suggesting cross-talk between downstream signals of Eph receptors and other RTKs [41–44]. Separation of the direct anti-tumor and anti-angiogenic effects of FTIs [45] is difficult due to the significant overlap of signaling via the Ras pathway in both tumor and endothelial cells. Similarly, radiation therapy and temozolomide target dividing endothelial cells in the same way that they target dividing tumor cells. The ability to potentially target both populations simultaneously however may be of therapeutic benefit in vivo and account for the significant inhibition of tumor growth in the orthotopic models. Our data suggests that in glioma cells, the EphR-Ras relationship is bidirectional, and that inhibition of H-Ras by a FTI potently blocks the activation of EphA7.
Our data show that glioma cells counterbalance the inhibition of H-Ras by lonafarnib with compensatory pathway activation in vitro. Activation of p38δ was increased after treatment with lonafarnib alone, but the increase was abrogated when XRT and Tem were added. Although Ras is a main signaling input for the MAPK/ERK signaling cascade, we found little downregulation of ERK1 activation with lonafarnib alone. Alternative prenylation of K-Ras and N-Ras by geranylgeranyl transferase-I still occurs in the presence of an FTI [46, 47], which may account for the continued activity of MAPK/ERK signaling and thus possible resistance to FTIs. This also could suggest other signaling mechanisms that function through the MAPK/ERK cascade are sufficient to fully activate the pathway in vitro. Activation of ERK1 was significantly upregulated with lonafarnib/XRT and significantly less in lonafarnib/XRT/Tem treated cells. Our data suggests XRT causes a rise in MAPK/ERK signaling, as others have reported [48], which is blocked by the addition of Tem.
Our results indicate that there is added in vitro efficacy with the combination of lonafarnib/XRT/Tem. Although we did not find lonafarnib alone or in combination with XRT/Tem to be highly cytotoxic, it was found to be potently cytostatic. Because XRT/Tem can induce significant inhibition of glioma growth in vivo, we reduced the amount of XRT/Tem given to animals in our preclinical model of GBM in order to be able to evaluate the potential effects of lonafarnib. Given that we are using only two doses of XRT/Tem, the in vivo response to lonafarnib/XRT/Tem in humans in the clinic may be amplified with the extended course of XRT/Tem typically prescribed for GBM. The combination of lonafarnib/XRT/Tem in vivo not only prevented progression of tumor growth, but also caused a significant decrease in tumor size. This indicates the combination of lonafarnib/XRT/Tem may manifest differently in vivo from what is found in vitro and highlights the role tumor microenvironment plays in a tumor’s response to biologic agents. Our goal is to improve response of GBM to standard modalities, and the addition of a drug that potently inhibits cell proliferation could maximize the effects of standard therapy.
Current strategies for the treatment of malignant gliomas have resulted in prolongation of survival but most patients eventually succumb to disease. This is thought in part to be related to the presence of a rare population of glioma stem cells that are highly radiation and chemotherapy resistant [49, 50]. Developing new strategies that specifically inhibit these cells may be critic in improving the outcome of this disease [51]. Our results demonstrating a significant inhibitory action of lonafarnib on glioma stem cell derived neurospheres and the complete suppression of proliferation when combined with radiation and temozolomide provide additional rational for further testing of this combination.
We hope to now translate the combination of lonafarnib/XRT/Tem to the clinical setting. To test this combination, we suggest a clinical trial in both adult and pediatric patients with newly diagnosed gliomas where lonafarnib is added concurrently to the standard of care XRT/Tem schedule. Our results support the continued investigation of combining novel molecular therapeutic agents with XRT/Tem with the goal of offering progress in the treatment of highly aggressive brain tumors.
References
Scott CB, Scarantino C, Urtasun R, Movsas B, Jones CU, Simpson JR, Fischbach AJ, Curran WJ Jr (1998) Validation and predictive power of Radiation Therapy Oncology Group (RTOG) recursive partitioning analysis classes for malignant glioma patients: a report using RTOG 90–06. Int J Radiat Oncol Biol Phys 40:51–55
Stupp R, Dietrich PY, Ostermann Kraljevic S, Pica A, Maillard I, Maeder P, Meuli R, Janzer R, Pizzolato G, Miralbell R, Porchet F, Regli L, de Tribolet N, Mirimanoff RO, Leyvraz S (2002) Promising survival for patients with newly diagnosed glioblastoma multiforme treated with concomitant radiation plus temozolomide followed by adjuvant temozolomide. J Clin Oncol 20:1375–1382
Nicholas MK (2007) Glioblastoma multiforme: evidence-based approach to therapy. Expert Rev Anticancer Ther 7:S23–S27
Falchetti ML, Mongiardi MP, Fiorenzo P, Petrucci G, Pierconti F, D’Agnano I, D’Alessandris G, Alessandri G, Gelati M, Ricci-Vitiani L, Maira G, Larocca LM, Levi A, Pallini R (2008) Inhibition of telomerase in the endothelial cells disrupts tumor angiogenesis in glioblastoma xenografts. Int J Cancer 122:1236–1242
Falchetti ML, Fiorenzo P, Mongiardi MP, Petrucci G, Montano N, Maira G, Pierconti F, Larocca LM, Levi A, Pallini R (2006) Telomerase inhibition impairs tumor growth in glioblastoma xenografts. Neurol Res 28:532–537
Belda-Iniesta C, de Castro Carpeno J, Sereno M, Gonzalez-Baron M, Perona R (2008) Epidermal growth factor receptor and glioblastoma multiforme: molecular basis for a new approach. Clin Transl Oncol 10:73–77
Ohgaki H, Kleihues P (2007) Genetic pathways to primary and secondary glioblastoma. Am J Pathol 170:1445–1453
Sarkar C, Karak AK, Nath N, Sharma MC, Mahapatra AK, Chattopadhyay P, Sinha S (2005) Apoptosis and proliferation: correlation with p53 in astrocytic tumours. J Neurooncol 73:93–100
Voelzke WR, Petty WJ, Lesser GJ (2008) Targeting the epidermal growth factor receptor in high-grade astrocytomas. Curr Treat Options Oncol 9:23–31
Failly M, Korur S, Egler V, Boulay JL, Lino MM, Imber R, Merlo A (2007) Combination of sublethal concentrations of epidermal growth factor receptor inhibitor and microtubule stabilizer induces apoptosis of glioblastoma cells. Mol Cancer Ther 6:773–781
Knobbe CB, Reifenberger J, Reifenberger G (2004) Mutation analysis of the Ras pathway genes NRAS, HRAS, KRAS and BRAF in glioblastomas. Acta Neuropathol 108:467–470
Feldkamp MM, Lala P, Lau N, Roncari L, Guha A (1999) Expression of activated epidermal growth factor receptors, Ras-guanosine triphosphate, and mitogen-activated protein kinase in human glioblastoma multiforme specimens. Neurosurgery 45:1442–1453
Widemann BC, Salzer WL, Arceci RJ, Blaney SM, Fox E, End D, Gillespie A, Whitcomb P, Palumbo JS, Pitney A, Jayaprakash N, Zannikos P, Balis FM (2006) Phase I trial and pharmacokinetic study of the farnesyltransferase inhibitor tipifarnib in children with refractory solid tumors or neurofibromatosis type I and plexiform neurofibromas. J Clin Oncol 24:507–516
Haas-Kogan DA, Banerjee A, Kocak M, Prados MD, Geyer JR, Fouladi M, McKnight T, Poussaint TY, Broniscer A, Blaney SM, Boyett JM, Kun LE (2008) Phase I trial of tipifarnib in children with newly diagnosed intrinsic diffuse brainstem glioma. Neuro Oncol 10:341–347
Kieran MW, Packer RJ, Onar A, Blaney SM, Phillips P, Pollack IF, Geyer JR, Gururangan S, Banerjee A, Goldman S, Turner CD, Belasco JB, Broniscer A, Zhu Y, Frank E, Kirschmeier P, Statkevich P, Yver A, Boyett JM, Kun LE (2007) Phase I and pharmacokinetic study of the oral farnesyltransferase inhibitor lonafarnib administered twice daily to pediatric patients with advanced central nervous system tumors using a modified continuous reassessment method: a Pediatric Brain Tumor Consortium Study. J Clin Oncol 25:3137–3143
Morgillo F, Lee HY (2006) Lonafarnib in cancer therapy. Expert Opin Invest Drugs 15:709–719
Bernhard EJ, McKenna WG, Hamilton AD, Sebti SM, Qian Y, Wu JM, Muschel RJ (1998) Inhibiting Ras prenylation increases the radiosensitivity of human tumor cell lines with activating mutations of Ras oncogenes. Cancer Res 58:1754–1761
Ling CC, Endlich B (1989) Radioresistance induced by oncogenic transformation. Radiat Res 120:267–279
McKenna WG, Weiss MC, Bakanauskas VJ, Sandler H, Kelsten ML, Biaglow J, Tuttle SW, Endlich B, Ling CC, Muschel RJ (1990) The role of the H-Ras oncogene in radiation resistance and metastasis. Int J Radiat Oncol Biol Phys 18:849–859
Miller AC, Gafner J, Clark EP, Samid D (1993) Differences in radiation-induced micronuclei yields of human cells: influence of Ras gene expression and protein localization. Int J Radiat Biol 64:547–554
Gupta AK, Bakanauskas VJ, McKenna WG, Bernhard EJ, Muschel RJ (2001) Ras regulation of radioresistance in cell culture. Methods Enzymol 333:284–290
Glass TL, Liu TJ, Yung WK (2000) Inhibition of cell growth in human glioblastoma cell lines by farnesyltransferase inhibitor SCH66336. Neuro-Oncol 2:151–158
Szentirmai O, Baker CH, Lin N, Szucs S, Takahashi M, Kiryu S, Kung AL, Mulligan RC, Carter BS (2006) Noninvasive bioluminescence imaging of luciferase expressing intracranial U87 xenografts: correlation with magnetic resonance imaging determined tumor volume and longitudinal use in assessing tumor growth and antiangiogenic treatment effect. Neurosurgery 58:365–372 (discussion 365–372)
Rubin JB, Kung AL, Klein RS, Chan JA, Sun Y, Schmidt K, Kieran MW, Luster AD, Segal RA (2003) A small-molecule antagonist of CXCR4 inhibits intracranial growth of primary brain tumors. Proc Natl Acad Sci USA 100:13513–13518
Ligon KL, Huillard E, Mehta S, Kesari S, Liu H, Alberta JA, Bachoo RM, Kane M, Louis DN, Depinho RA, Anderson DJ, Stiles CD, Rowitch DH (2007) Olig2-regulated lineage-restricted pathway controls replication competence in neural stem cells and malignant glioma. Neuron 53:503–517
Singh SK, Clarke ID, Terasaki M, Bonn VE, Hawkins C, Squire J, Dirks PB (2003) Identification of a cancer stem cell in human brain tumors. Cancer Res 63:5821–5828
Desrosiers RR, Cusson MH, Turcotte S, Beliveau R (2005) Farnesyltransferase inhibitor SCH-66336 downregulates secretion of matrix proteinases and inhibits carcinoma cell migration. Int J Cancer 114:702–712
Laks DR, Masterman-Smith M, Visnyei K, Angenieux B, Orozco NM, Foran I, Yong WH, Vinters HV, Liau LM, Lazareff JA, Mischel PS, Cloughesy TF, Horvath S, Kornblum HI (2009) Neurosphere formation is an independent predictor of clinical outcome in malignant glioma. Stem Cells 27:980–987
Dowlati A, Kluge A, Nethery D, Halmos B, Kern JA (2008) SCH66336, inhibitor of protein farnesylation, blocks signal transducer and activators of transcription 3 signaling in lung cancer and interacts with a small molecule inhibitor of epidermal growth factor receptor/human epidermal growth factor receptor 2. Anticancer Drugs 19:9–16
Feldkamp MM, Lau N, Guha A (1999) Growth inhibition of astrocytoma cells by farnesyl transferase inhibitors is mediated by a combination of anti-proliferative, pro-apoptotic and anti-angiogenic effects. Oncogene 18:7514–7526
Sepp-Lorenzino L, Ma Z, Rands E, Kohl NE, Gibbs JB, Oliff A, Rosen N (1995) A peptidomimetic inhibitor of farnesyl:protein transferase blocks the anchorage-dependent and -independent growth of human tumor cell lines. Cancer Res 55:5302–5309
Pollack IF, Bredel M, Erff M, Hamilton AD, Sebti SM (1999) Inhibition of Ras and related guanosine triphosphate-dependent proteins as a therapeutic strategy for blocking malignant glioma growth: II–preclinical studies in a nude mouse model. Neurosurgery 45:1208–1214 (discussion 1214–1205)
Liu M, Bishop WR, Nielsen LL, Bryant MS, Kirschmeier P (2001) Orally bioavailable farnesyltransferase inhibitors as anticancer agents in transgenic and xenograft models. Methods Enzymol 333:306–318
Shi Y, Wu J, Mick R, Cerniglia GJ, Cohen-Jonathan E, Rhim JS, Koch CJ, Bernhard EJ (2005) Farnesyltransferase inhibitor effects on prostate tumor micro-environment and radiation survival. Prostate 62:69–82
Lustig R, Mikkelsen T, Lesser G, Grossman S, Ye X, Desideri S, Fisher J, Wright J (2008) Phase II preradiation R115777 (tipifarnib) in newly diagnosed GBM with residual enhancing disease. Neuro Oncol 10:1004–1009
Loprevite M, Favoni RE, De Cupis A, Scolaro T, Semino C, Mazzanti P, Ardizzoni A (2004) In vitro study of farnesyltransferase inhibitor SCH 66336, in combination with chemotherapy and radiation, in non-small cell lung cancer cell lines. Oncol Rep 11:407–414
Lerner EC, Qian Y, Blaskovich MA, Fossum RD, Vogt A, Sun J, Cox AD, Der CJ, Hamilton AD, Sebti SM (1995) Ras CAAX peptidomimetic FTI-277 selectively blocks oncogenic Ras signaling by inducing cytoplasmic accumulation of inactive Ras–Raf complexes. J Biol Chem 270:26802–26806
Chakravarti A, Chakladar A, Delaney MA, Latham DE, Loeffler JS (2002) The epidermal growth factor receptor pathway mediates resistance to sequential administration of radiation and chemotherapy in primary human glioblastoma cells in a RAS-dependent manner. Cancer Res 62:4307–4315
Abounader R, Ranganathan S, Kim BY, Nichols C, Laterra J (2001) Signaling pathways in the induction of c-met receptor expression by its ligand scatter factor/hepatocyte growth factor in human glioblastoma. J Neurochem 76:1497–1508
Elowe S, Holland SJ, Kulkarni S, Pawson T (2001) Downregulation of the Ras-mitogen-activated protein kinase pathway by the EphB2 receptor tyrosine kinase is required for ephrin-induced neurite retraction. Mol Cell Biol 21:7429–7441
Holland SJ, Gale NW, Gish GD, Roth RA, Songyang Z, Cantley LC, Henkemeyer M, Yancopoulos GD, Pawson T (1997) Juxtamembrane tyrosine residues couple the Eph family receptor EphB2/Nuk to specific SH2 domain proteins in neuronal cells. EMBO J 16:3877–3888
Tong J, Elowe S, Nash P, Pawson T (2003) Manipulation of EphB2 regulatory motifs and SH2 binding sites switches MAPK signaling and biological activity. J Biol Chem 278:6111–6119
Kim I, Ryu YS, Kwak HJ, Ahn SY, Oh JL, Yancopoulos GD, Gale NW, Koh GY (2002) EphB ligand, ephrinB2, suppresses the VEGF- and angiopoietin 1-induced Ras/mitogen-activated protein kinase pathway in venous endothelial cells. FASEB J 16:1126–1128
Klemke RL, Cai S, Giannini AL, Gallagher PJ, de Lanerolle P, Cheresh DA (1997) Regulation of cell motility by mitogen-activated protein kinase. J Cell Biol 137:481–492
Scott AN, Hetheridge C, Reynolds AR, Nayak V, Hodivala-Dilke K, Mellor H (2008) Farnesyltransferase inhibitors target multiple endothelial cell functions in angiogenesis. Angiogenesis 11:337–346
Basso AD, Mirza A, Liu G, Long BJ, Bishop WR, Kirschmeier P (2005) The farnesyl transferase inhibitor (FTI) SCH66336 (lonafarnib) inhibits Rheb farnesylation and mTOR signaling Role in FTI enhancement of taxane and tamoxifen anti-tumor activity. J Biol Chem 280:31101–31108
Sebti SM, Hamilton AD (2000) Farnesyltransferase and geranylgeranyltransferase I inhibitors and cancer therapy: lessons from mechanism and bench-to-bedside translational studies. Oncogene 19:6584–6593
Whyte DB, Kirschmeier P, Hockenberry TN, Nunez-Oliva I, James L, Catino JJ, Bishop WR, Pai JK (1997) K- and N-Ras are geranylgeranylated in cells treated with farnesyl protein transferase inhibitors. J Biol Chem 272:14459–14464
Lu C, Shervington A (2008) Chemoresistance in gliomas. Mol Cell Biochem 312:71–80
Rich JN (2007) Cancer stem cells in radiation resistance. Cancer Res 67:8980–8984
Sauvageot CM, Kesari S, Stiles CD (2007) Molecular pathogenesis of adult brain tumors and the role of stem cells. Neurol Clin 25:891–924 (vii)
Acknowledgments
Funding was provided by the Stop & Shop Family Pediatric Brain Tumor Fund, the C.J. Buckley Fund (J.W.B., D.C., D.P., E.R.G., M.W.K.), the Kyle Johnson Fund (J.W.B., M.W.K.), the Pediatric Low-Grade Astrocytoma Foundation (C.S., M.W.K.), the Solomon and Marlene Finvarb Brain Tumor Research Fund (P.Y.W., C.S.), the Brudnick Foundation (N.R.), by NIH K08 (SK: K08CA124804) and by Sontag Foundation Distinguished Scientist Award (SK).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2010_502_MOESM1_ESM.ppt
Supplemental Figure 1 Combination treatment influences activation of MAPK and RTK pathways. (A) Representative Proteome Profiler (R&D Systems, Minneapolis MN) dot blot is shown for pEGF receptor (pEGFR), pHGFR, pEphA7, pP38 and ERK1. The optical density of duplicate dots were normalized to control and plotted as the mean ± s.e.m. Statistical significance was determined by Student’s t-test (*P < 0.05, **P < 0.01, ***P < 0.001). (PPT 443 kb)
Rights and permissions
About this article
Cite this article
Chaponis, D., Barnes, J.W., Dellagatta, J.L. et al. Lonafarnib (SCH66336) improves the activity of temozolomide and radiation for orthotopic malignant gliomas. J Neurooncol 104, 179–189 (2011). https://doi.org/10.1007/s11060-010-0502-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0502-4