Abstract
Objective
Postoperative atrial fibrillation (POAF) complicating coronary artery bypass grafting surgery (CABG) increases morbidity and stroke risk. Total atrial conduction time (PA-TDI duration) has been identified as an independent predictor of new-onset atrial fibrillation (AF). We aimed to assess whether PA-TDI duration is a predictor of AF after CABG.
Methods
In 128 patients who had undergone CABG, preoperative clinical and echocardiographic data were compared between patients with and without POAF. The PA-TDI duration was assessed by measuring the time interval between the beginning of the P wave on the surface ECG and point of the peak A wave on TDI from left atrium (LA) lateral wall just over the mitral annulus.
Results
Patients with POAF (38/128, 29.6 %) were older (68.1 ± 11.1 vs. 59.3 ± 10.2 years; p < 0.001), had higher LA maximum volume, had prolonged PA-TDI duration, and had lower ejection fraction compared with patients without POAF. PA-TDI duration was found to be significantly increased in POAF group (134.3 ± 19.7 vs. 112.5 ± 17.7 ms; p = 0.01). On multivariate analysis, age (95 % CI = 1.03–1.09; p = 0.003), LA maximum volume (95 % CI = 1.01–1.06; p = 0.03), and prolonged PA-TDI duration (95 % CI, 1.02–1.05; p = 0.001) were found to be the independent risk factors of POAF.
Conclusions
In this study, LA maximum volume and PA-TDI duration were found to be the independent predictors of the development of POAF after CABG. Echocardiographic predictors of left atrial electromechanical dysfunction may be useful in risk stratifying of patients in terms of POAF development after CABG.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Atrial fibrillation (AF) is a frequent complication following coronary artery bypass grafting (CABG) with an occurrence rate of from 10 to 40 % [1]. AF was firstly thought to be harmless; however, it is now accepted as a hazardous postoperative condition and it may lead to increased duration of hospitalization, postoperative morbidity, and mortality [2–4]. The risk factor assessment of postoperative AF (POAF) development has generated incoherent results, with the exception of increased age [3–5]. Several studies have been performed to determine the factors associated with the development of AF after CABG. Also, clinical risk stratification to define patients who are at high risk for AF after CABG has been studied extensively [6–8].
Currently, the most commonly used method to estimate the extent of atrial remodeling is the measurement of the left atrial size. Left atrial size and volume are independent predictors of new-onset AF in general population. Additionally, a new noninvasive echocardiographic method has been identified that predicts new-onset AF. This technique measures the total atrial conduction time (PA-TDI duration) using tissue Doppler imaging of the atria and P wave on surface electrocardiogram [9, 10]. The total atrial conduction time provides more exact evaluation of the atrial remodeling than conventional echocardiography parameters [9, 10]. Also, total atrial conduction time has important value for the prediction of new-onset AF or paroxysmal AF [9]. The aim of the present study is to investigate the predictive value of total atrial conduction time for the development of AF after CABG.
2 Methods
2.1 Study population
The study population consisted of consecutive patients whom CABG was recommended after coronary angiography. These patients underwent coronary angiography because of typical or atypical angina pectoris and suspicion of coronary artery disease. We have also evaluated the standard preoperative 12-lead ECG recorded at a paper speed of 25 mm/s obtained for each patient using the MAC 5500 electrocardiograph (GE Healthcare, Milan, Italy) before surgery. One hundred twenty-eight patients with preoperative sinus rhythm who had undergone CABG were included in the study population. Study patients had no previous cardiac surgery and underwent standard CABG requiring cardiopulmonary bypass without concurrent valvular surgery. Exclusion criteria were as follows: emergency surgery patients, repeat CABG, acute coronary syndrome, prior myocardial infarction, congestive heart failure, left ventricular (LV) hypertrophy, significant valvular heart disease, permanent pacemaker implantation, atrial flutter or fibrillation, frequent ventricular preexcitation and atrioventricular conduction abnormalities, pulmonary or neurological disease, pericarditis, congenital heart disease, alcohol abuse, and renal, hepatic, or thyroid disease. Also, all patients with any kind of past AF detected by scanning the hospital records such as holter monitoring and prior ECGs were excluded. All patients were evaluated clinically with electrocardiography, echocardiography, and routine biochemical tests. Written informed consent was obtained from all participants, and the study protocol was approved by the local ethics committee.
2.2 Standard echocardiography
All patients were assessed by transthoracic M mode, two-dimensional (2-D), pulsed-wave, continuous wave, color flow, and tissue Doppler imaging (TDI). All examinations were performed with the GE-Vivid-3 system (GE Vingmed, Horten, Norway) with a 2- to 4-MHz transducer at a depth of 16 cm. During echocardiography, continuous three-lead ECG recording was obtained. All patients were imaged in the left lateral decubitus position. 2-D and conventional Doppler examinations were obtained in the parasternal and apical views according to the guidelines of the American Society of Echocardiography [11]. LV diameters and wall thickness were measured by M mode echocardiography. LV ejection fraction was calculated using the apical two- and four-chamber views by Simpson’s method, according to American Society of Echocardiography guidelines [11]. The mitral valve inflow pattern (E wave, A wave, E wave deceleration time, E/A ratio, and isovolumic relaxation time) were measured using pulsed wave Doppler. Left atrium (LA) volumes were obtained by apical four-chamber and apical two-chamber views by disc’s method [11, 12]. LA maximum volume (V max) at the end-systolic phase, LA minimum volume (V min) at the end-diastolic phase, and LA volume before atrial systole (V p) were measured and indexed to body surface area. The LA function parameters were calculated as follows [13];
2.3 Tissue Doppler echocardiography
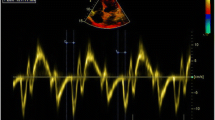
TDI was performed by transducer frequencies of 3.5 to 4.0 MHz, adjusting the spectral pulsed Doppler signal filters to acquire the Nyquist limit of 15 to 20 cm/s and using the minimal optimal gain. Myocardial TDI velocities (peak systolic (S m), early diastolic (E m), and late diastolic velocities (A m)) were measured via spectral pulsed Doppler as of the LV-free wall from the apical four chamber view. The ultrasound beam was positioned as parallel as possible with the myocardial segment to acquire the optimal angle of imaging. A novel echocardiographic consideration based on TDI has been introduced to assess the total atrial conduction time: PA-TDI duration [10]. The PA-TDI duration was assessed by measuring the time interval between the beginning of the P wave on the surface ECG and point of the peak A wave on TDI from LA lateral wall just over the mitral annulus (Fig. 1) [10, 14]. All measurements were repeated three times, and average values were received for each of parameters. All measurements were performed by two experienced investigators before CABG. Twenty-five patients were randomly selected to test the intra- and interobserver variability for the PA-TDI duration measurements by Bland–Altman analysis. The inter- and intraobserver reproducibility of PA-TDI duration measurements showed minimal biases and tight limits of agreement (2.0 ± 12 and 1.9 ± 10 ms, respectively).
2.4 Peroperative assessment
All surgeries were performed through standard procedures: median sternotomy, aortic cannulation, single right atrial cannula, with membrane oxygenator (Dideco Avant 903), single cross clamp, initially anterograde via the aorta than retrograde blood cardioplegia every 15 min via the coronary sinus, a roller pump, and mild systemic hypothermia (32–34 °C). After CPB, heparin sodium was antagonized at the rate of 1 mg heparin/1 mg protamine sulphate. The preferred inotropic agents were dopamine and adrenaline, and if necessary noradrenalin and intra-aortic balloon pump were used. The preferred vasodilator was nitroglycerin, and sodium nitroprusside was the second choice.
All patients were monitored continuously by five-lead telemetry during the intensive care unit (ICU) admission and followed up hourly with monitoring of blood gas samples. If electrolyte imbalance was detected in any patient, immediate treatment was initiated. To avoid withdrawal, beta blockers were continued postoperatively in patients who use them preoperatively. Presence of POAF lasting more than 5 min during hospitalization was detected by using continuous telemetry or 12-lead electrocardiography. After ICU discharge, the patients were monitored once daily by 12-lead electrocardiograms every morning. Additional electrocardiographic recordings were obtained in necessary cases such as reporting of palpitations by a patient or an abnormal rhythm is noticed by a nurse.
2.5 Statistical analysis
All analysis of normality of the continuous variables was performed with the Kolmogorov–Smirnov test. Continuous variables were expressed as mean ± SD and were compared with the Student’s t test. Categorical variables were expressed as number (percentage) and were compared by Chi-square tests. Pearson’s correlation exponents were used to assess the relation between continuous variables. Univariate and multivariate regression analyses were performed to relate clinical characteristics and echocardiographic parameters to the development of postoperative AF. Variables with a p value of <0.05 in the univariate analysis were included into the multivariate analysis. Multivariate analysis was performed using a backward stepwise conditional approach. Variables with a p > 0.05 were excluded from the model. The receiver operator characteristics (ROC) curve was calculated to assess the performance of the strongest independent predictors of postoperative AF. All analyses were performed using the SPSS (SPSS for Windows 15.0) software package.
3 Results
3.1 Patient characteristics
The present study population was prospectively included before CABG. A total of 155 patients were included. Twenty-seven patients were excluded because of previous AF. So, the final study population included 128 patients. Postoperative AF was observed in 38 (29.6 %) patients (mean age = 68.1 ± 11.1); of these, 65.7 % (n = 25) were men, 57.8 % (n = 22) had hypertension, 36.8 % (n = 14) had diabetes, 52.6 % (n = 20) was smoking, and 34.2 % (n = 13) had a history of myocardial infarction. Postoperative AF was not observed in 90 patients (mean age, 59.3 ± 10.2 years); of these, 72.2 % (n = 65) were men, 55.5 % (n = 50) had hypertension, 33.3 % (n = 30) had diabetes, 50.0 % (n = 45) was smoking, and 33.3 % (n = 30) had a history of myocardial infarction. Patients’ demographic and laboratory characteristics and surgical data were presented in Table 1. The average age was significantly higher in POAF patients and also, beta blocker usage was slightly higher in patients without POAF but it did not reach statistical significance.
Patients with POAF had significantly larger LA volumes compared with patients who without POAF (LA maximum volume = 30.6 ± 11.8 vs. 26.1 ± 10.1 ml/m2 (p = 0.011); LA minimum volume = 12.6 ± 4.8 vs. 10.1 ± 4.1 ml/m2 (p = 0.021); LA volume before P wave = 19.9 ± 6.1 vs. 16.9 ± 5.8 ml/m2 (p = 0.012)). The LV ejection fraction was significantly lower in patients with POAF than those without POAF (51.1 ± 12.1 vs. 57.4 ± 10.2 (p = 0.009)). Also, the E m/A m ratio was significantly lower in patients with POAF (Table 2).
3.2 Total atrial conduction time
The mean PA-TDI duration was significantly longer in patients with POAF than those without POAF (134.3 ± 19.7 vs. 112.5 ± 17.7 ms (p = <0.001) (Fig. 2). There was a positive correlation between age and PA-TDI duration (r = 0.250; p = 0.006), and there was a mildly negative correlation between E m/A m ratio and PA-TDI duration (r = −0.180, p = 0.048). There was no relation between the use of beta blocker and PA-TDI duration. Also, LA V max and LA V min were found to be correlated with PA-TDI (r = 0.564, p = 0.001 and r = 0,763, p < 0.001, respectively).
3.3 Predictors of postoperative AF
Univariate and multivariate regression analyses were performed to identify clinical and echocardiographic predictors of POAF after CABG (Tables 3 and 4). Age (HR = 1.060, p = 0.003), LA maximum volume (HR = 1.030, p = 0.030), and PA-TDI duration (HR = 1.03, p = 0.001) were identified as independent predictors of POAF.
To study the discriminative performance of PA-TDI duration to predict POAF after CABG, ROC curve analyses were performed (Fig. 3). The area under the ROC curve (index of discrimination) for PA-TDI duration was 0.863 (p < 0.001), indicating a high discriminative power. Also, PA-TDI duration to be longer than 125.5 ms was found to be predictive for POAF with 87.2 % sensitivity and 92.1 % specificity in the ROC curve analyses.
4 Discussion
The present study investigated the value of pre-procedural echocardiographic evaluation of the total atrial conduction time measured by TDI to predict POAF after CABG. The main finding was that PA-TDI duration was an independent predictor of POAF after CABG. Furthermore, PA-TDI duration was a stronger predictor of POAF than LA maximum volume and established a higher degree of discrimination to identify patients who will have POAF after CABG.
In general, POAF after CABG which is occurring in approximately 30 % of patients, increases the risk of stroke and total cost of operation, and prolongs the duration of hospitalization [4]. Also, in a previous study, it was reported that in the USA only, $ 1 billion is spent each year for this problem [15]. In order to identify patients who are at high risk for developing POAF after CABG, practical, useful, and easily evaluated new methods are required. Identification of patients at high risk for developing POAF can facilitate the detection of a population which is more likely to benefit from anti-arrhythmic drugs or other preventive modalities [16, 17].
A large number of parameters have been related to a high risk of AF recurrence after CABG, such as age, LA size, LV systolic and diastolic functions, and also LV ejection fraction [6, 18, 19]. Interestingly, these parameters all seem to either cause or affect the occurrence and extent of atrial remodeling. A high extent of atrial remodeling is thought to increase POAF. In the present study, we demonstrated that age, E m/A m ratio, LV ejection fraction and a large LA maximum volume were associated with a higher risk for POAF after CABG. In a study of 1,851 patients, Amar et al. [1] have found that age appeared to be the single most important predictor of POAF. Together with ageing, cardiac enlargement, myocardial atrophy, reduction of myocardial tissue conduction, and fibrosis in atria occurs [20]. Additionally, Nardi et al. [21] demonstrated that LA volume measurements were independently correlated to the occurrence of POAF in patients with isolated CABG. Similarly, in our study multivariate analysis demonstrated that age and LA maximum volume were independent predictors of POAF after CABG.
Although LA maximum volume index was independently associated with POAF after CABG, additional parameters are needed to improve patient selection. Because, in addition to atrial dilatation, prolonged atrial conduction time may be another consequence of atrial remodeling [22]. Atrial dilatation and prolonged atrial conduction time could result in a larger number of re-entrant wavelets inside the atria. So, these changes may increase the development of POAF [23]. The total atrial conduction time is associated with atrial size and conduction speed. In our study, LA volumes were found to be correlated with the PA-TDI duration. This make us to think a longer distance for activation to traverse rather than slower conduction velocity have a role on the prolongation of the PA-TDI duration. However, changes in the permeability of ion channels as electrical atrial remodeling may also reduce the transmission speed. Necessarily, compared with LA size, the assessment of the total atrial conduction time can present a more comprehensive evaluation of atrial remodeling since this parameter integrates mechanical and electrical properties of the LA wall [23, 24].
There are several ways to measure total atrial conduction time; one of those is the gold standard technique, Signal Averaged ECG, but it necessitates special hardware and it is a long technique. Because of this, total atrial conduction time measurement by signal-averaged ECG has not found its way into clinical practice. PA-TDI was shown to be an easy, fast, and reliable method to measure the total atrial electrical activation time [10]. The PA-TDI duration is a readily available echocardiographic tool to estimate the total atrial conduction time and it can be measured easily by every cardiologist. This novel echocardiographic tool has been validated by the P wave duration on signal-averaged electrocardiography [10]. Recently, Antoni et al. [14] demonstrated that PA-TDI duration is a simple measurement that provides important value for the prediction of new-onset AF in patients after acute myocardial infarction. In our study, we demonstrated that PA-TDI duration was an independent predictor of POAF after CABG. Additionally, PA-TDI duration was a stronger predictor of POAF after CABG than LA size and demonstrated a higher degree of discrimination (area under the ROC curve of 0.863 (p < 0.001)).
4.1 Limitations
The major limitation of this study is the relatively low number of patients. Secondly, our results and conclusions are limited to the new-onset, in-hospital AF and do not address episodes of AF that occur after discharge. Nevertheless, AF episodes after discharge may have been missed. Additionally, there are many factors related with occurrence of AF, we were able to include only the probable parameters with a major effect in the statistical evaluation of our study.
5 Conclusions
LA maximum volume and PA-TDI duration were independent predictors of the development of POAF after CABG. Also, the PA-TDI duration provided incremental value for the prediction of POAF to known clinical and echocardiographic risk factors. Echocardiographic evaluation of the PA-TDI duration is a simple, fast, and reliable method to obtain total atrial activation time that can be used in risk stratification for POAF after CABG.
References
Amar, D., Shi, W., Hogue, C. W., Jr., et al. (2004). Clinical prediction rule for atrial fibrillation after coronary artery bypass grafting. Journal of the American College of Cardiology, 44, 1248–1253.
Hogue, C. W., & Hyder, M. L. (2000). Atrial fibrillation after cardiac operation: risks, mechanisms, and treatment. The Annals of Thoracic Surgery, 69, 300–306.
Mathew, J. P., Fontes, M. L., Tudor, I. C., et al. (2004). A multicenter risk index for atrial fibrillation after cardiac surgery. Journal of the American Medical Association, 291, 1720–1729.
Villareal, R. P., Hariharan, R., Liu, B. C., et al. (2004). Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. Journal of the American College of Cardiology, 43, 742–748.
Mahoney, E. M., Thompson, T. D., Veledar, E., Williams, J., & Weintraub, W. S. (2002). Cost-effectiveness of targeting patients undergoing cardiac surgery for therapy with intravenous amiodarone to prevent atrial fibrillation. Journal of the American College of Cardiology, 40, 737–742.
Sezai, A., Hata, M., Niino, T., et al. (2009). Study of the factors related to atrial fibrillation after coronary artery bypass grafting: a search for a marker to predict the occurrence of atrial fibrillation before surgical intervention. The Journal of Thoracic and Cardiovascular Surgery, 137, 895–900.
El-Chami, M. F., Kilgo, P., Thourani, V., et al. (2010). New-onset atrial fibrillation predicts long-term mortality after coronary artery bypass graft. Journal of the American College of Cardiology, 55, 1370–1376.
Shen, J., Lall, S., Zheng, V., Buckley, P., Damiano, R. J., & Schuessler, R. B. (2011). The persistent problem of new-onset postoperative atrial fibrillation: a single institution experience over two decades. The Journal of Thoracic and Cardiovascular Surgery, 141, 559–570.
Den Uijl, D. W., Gawrysiak, M., Tops, L. F., Trines, S. A., Zeppenfeld, K., Schalij, M. J., et al. (2011). Prognostic value of total atrial conduction time estimated with tissue Doppler imaging to predict the recurrence of atrial fibrillation after radiofrequency catheter ablation. Europace, 13, 1533–1540.
Merckx, K. L., De Vos, C. B., Palmans, A., Habets, J., Cheriex, E. C., Crijns, H. J., et al. (2005). Atrial activation time determined by transthoracic Doppler tissue imaging can be used as an estimate of the total duration of atrial electrical activation. Journal of the American Society of Echocardiography, 18(9), 940–944.
Lang, R. M., Bierig, M., Devereux, R. B., Flachskampf, F. A., Foster, E., Pellikka, P. A., et al. (2005). Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. Journal of the American Society of Echocardiography, 18, 1440–1463.
Quinones, M. A., Otto, C. M., Stoddard, M., Waggoner, A., & Zoghbi, W. A. (2002). Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. Journal of the American Society of Echocardiography, 15, 167–184.
Acar, G., Akcay, A., Sökmen, A., Özkaya, M., Güler, E., Sökmen, G., et al. (2009). Assessment of atrial electromechanical delay, diastolic functions, and left atrial mechanical functions in patients with type 1 diabetes mellitus. Journal of the American Society of Echocardiography, 22, 732–738.
Antoni, M. L., Bertini, M., Atary, J. Z., Delgado, V., ten Brinke, E. A., Boersma, E., et al. (2010). Predictive value of total atrial conduction time estimated with tissue Doppler imaging for the development of new-onset atrial fibrillation after acute myocardial infarction. The American Journal of Cardiology, 106(2), 198–203.
Steinberg, J. S. (2004). Postoperative atrial fibrillation: a billion-dollar problem. Journal of the American College of Cardiology, 43, 1001–1003.
Blommaert, D., Gonzalez, M., Mucumbitsi, J., et al. (2000). Effective prevention of atrial fibrillation by continuous atrial overdrive pacing after coronary artery bypass surgery. Journal of the American College of Cardiology, 35, 1411–1415.
Budeus, M., Hennersdorf, M., Perings, S., et al. (2006). Amiodarone prophylaxis for atrial fibrillation of high risk patients after coronary bypass grafting: a prospective, double blinded, placebo controlled, randomized study. European Heart Journal, 27, 1584–1591.
Açil, T., Cölkesen, Y., Türköz, R., et al. (2007). Value of preoperative echocardiography in the prediction of postoperative atrial fibrillation following isolated coronary artery bypass grafting. The American Journal of Cardiology, 100(9), 1383–1386.
Osranek, M., Fatema, K., Qaddoura, F., et al. (2006). Left atrial volume predicts the risk of atrial fibrillation after cardiac surgery: a prospective study. Journal of the American College of Cardiology, 48, 779–786.
Davies, M., & Pomerance, A. (1972). Pathology of atrial fibrillation in man. British Heart Journal, 34, 520–525.
Nardi, F., Diena, M., Caimmi, P. P., Iraghi, G., Lazzero, M., Cerin, G., et al. (2012). Relationship between left atrial volume and atrial fibrillation following coronary artery bypass grafting. Journal of Cardiac Surgery, 27(1), 128–135.
Gaspo, R., Bosch, R. F., Talajic, M., & Nattel, S. (1997). Functional mechanisms underlying tachycardia-induced sustained atrial fibrillation in a chronic dog model. Circulation, 96, 4027–4035.
Choi, J. I., Ryu, K., Park, E., Benser, M. E., Jang, J. K., Lee, H. S., et al. (2010). Atrial activation time and pattern of linear triple-site vs. single-site atrial pacing after cardioversion in patients with atrial fibrillation. Europace, 12, 508–516.
De Vos, C. B., Weijs, B., Crijns, H. J., Cheriex, E. C., Palmans, A., Habets, J., et al. (2009). Atrial tissue Doppler imaging for prediction of new-onset atrial fibrillation. Heart, 95, 835–840.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özlü, M.F., Erdem, K., Kırış, G. et al. Predictive value of total atrial conduction time measured with tissue Doppler imaging for postoperative atrial fibrillation after coronary artery bypass surgery. J Interv Card Electrophysiol 37, 27–33 (2013). https://doi.org/10.1007/s10840-012-9756-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-012-9756-4