Abstract
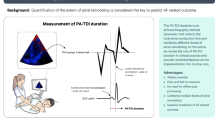
Prolonged total atrial conduction time is caused by atrial remodeling. Left atrial remodeling is associated with poor outcome in patients with heart failure (HF). This study aimed to investigate whether prolonged total atrial conduction time predicts poor prognosis in patients with HF. We performed transthoracic echocardiography in 100 patients (65 men; mean age 68 ± 13 years) who were hospitalized for HF. Total atrial conduction time was defined as the duration from P wave onset on electrocardiography to peak A′ wave on tissue Doppler imaging (TDI) echocardiography (PA-TDI duration). There were 37 cardiac events (37%) during a median follow-up period of 414 days. The PATDI duration was significantly longer in patients with cardiac events than in those without (150 ± 18 ms vs 133 ± 19 ms; P < 0.05). There were no significant differences in left ventricular end-diastolic dimensions and ejection fractions between patients with and without cardiac events. Patients with HF were divided into 3 groups according to tertiles of the PA-TDI duration. Kaplan–Meier analysis showed that the highest tertile of PA-TDI duration was associated with the greatest risk among patients with HF. Multivariate Cox proportional hazard analysis showed that the PA-TDI duration was an independent predictor of cardiac events, leading to the conclusion that prolonged PA-TDI duration was a feasible predictor of cardiac prognosis in patients with HF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a major and growing health problem in developed countries. Despite advances in medical treatment, the annual mortality and morbidity rates for HF are still high [1,2,3]. Several studies have shown that increased left atrial (LA) remodeling predicts a poor prognosis in patients with HF [4]. Since the LA is directly exposed to left ventricular (LV) filling pressure during the diastolic phase, an increase in LA filling pressure leads to dilatation of the chamber in patients with HF. Therefore, LA pressure and size can be a marker of the burden of LV diastolic dysfunction [5].
Atrial size is most commonly used as a marker of structural atrial remodeling [6]. By contrast, prolonged total atrial conduction time is a sign of electrical and structural remodeling of the atria [7]. Several studies have suggested that atrial conduction time evaluated through signal-averaged electrocardiography (ECG) was associated with poor cardiac prognosis in patients with HF [8]. However, it takes a long time to evaluate atrial conduction time with signal-averaged ECG. Recently, an easy method for evaluating atrial conduction time by means of tissue Doppler imaging (TDI) echocardiography was reported [7]. The present study aimed to examine whether the total atrial conduction time as evaluated by TDI echocardiography can risk-stratify patients with HF and predict cardiac prognosis.
Methods
Patients
One hundred patients (65 men and 35 women; mean age 68 ± 13 years) who were admitted to Yamagata University Hospital for the treatment of worsening HF or therapeutic evaluation of HF were enrolled in the study. The diagnosis of HF was made by two senior cardiologists using the generally accepted Framingham criteria and other relevant information, including a history of dyspnea and symptomatic exercise intolerance with signs of pulmonary congestion or peripheral edema, the presence of moist rales on auscultation, or the documentation of LV enlargement or dysfunction by chest radiography or echocardiography [9, 10]. The functional severity of HF at admission was assessed by the New York Heart Association (NYHA) functional class. Diagnoses of hypertension, diabetes, and hyperlipidemia were obtained from medical records or patient histories of current or previous medical therapy.
All patients were evaluated clinically through ECG, echocardiography, and routine biochemical tests. Echocardiography recordings were obtained when patients had a normal sinus rhythm with a heart rate of 50–100 beats/min. The exclusion criteria were as follows: advanced malignant tumors, renal insufficiency characterized by a serum creatinine concentration > 2.0 mg/dL, severe valvular heart disease, atrial flutter, chronic atrial fibrillation (AF), and permanent pacemaker implantation. Informed consent was given by each patient before participation in the study, and the protocol was approved by the institution’s Human Investigations Committee.
Blood samples were obtained for the measurement of plasma B-type natriuretic peptide (BNP) upon admission and discharge and for the measurement of estimated glomerular filtration rate (eGFR) upon discharge. Plasma BNP levels were measured using a commercially available specific radio-immunoassay (SHIONORIA BNP assay kit; Shionogi & Co. Ltd., Osaka, Japan) [10]. Clinical data, including age, sex, and NYHA functional class upon admission, were obtained from hospital medical records and patient interviews. The time of discharge was decided by two senior cardiologists.
Echocardiography
Transthoracic echocardiography (TTE) was performed on a Vivid E9 ultrasound instrument (GE Healthcare, Chicago, IL USA), equipped with a sector transducer (carrier frequency of 2.5 or 3.75 MHz). During echocardiography, single-lead ECG was simultaneously recorded. TTE was performed while the patient was in a stable condition with HF before discharge. The following parameters were assessed using standard views and techniques: left atrial dimension (LAD) was measured at end-systole in the 2-dimensional parasternal long-axis view. LA volume was assessed at LV end-systole using the biplanar area-length method from the 4- and 2-chamber views [11]. Measurements of LA volume were indexed by body surface area (LA volume index, LAVI). LV internal diameter was measured at end-diastole and end-systole in the 2-dimensional parasternal long-axis view. LV ejection fraction (LVEF) was calculated using the biplanar method of disks (modified Simpson’s rule) [12]. All patients underwent pulsed-wave Doppler examination of mitral inflow. Peak transmitral flow E wave and A wave velocities, E wave deceleration time (DCT), and ratio of E wave to A wave were measured from the apical 4-chamber view. The apical 4-chamber view was used to obtain the TDI of the mitral annulus. A sample volume of pulsed-wave Doppler was positioned at the septal and lateral side of the mitral annulus, and the spectral signal of the mitral annular velocity was recorded. The peak early (E′) mitral annular velocity was measured, and the ratio of the E wave to E′ (E/E′) was calculated. Total atrial conduction time was assessed by measuring the time interval between the onset of the P wave on the surface ECG and the point of the peak A wave on TDI echocardiography from the LA lateral wall just over the mitral annulus (PA-TDI duration) [7]. All valves were evaluated using continuous Doppler color flow and Doppler imaging for stenosis and regurgitation. Patients with severe stenosis and regurgitation were excluded, and those with less than moderate stenosis and regurgitation were included in the present study. All echocardiographic measurements were calculated as mean values from three consecutive cardiac cycles and evaluated by two independent experienced echocardiologists who were blinded to the clinical status of patients.
The reproducibility of the PA-TDI duration measurement was assessed in 20 randomly selected subjects. Interobserver variability presented by interclass correlation coefficient (ICC) was calculated using images independently recorded on two different occasions by two different observers. Interobserver ICC of the PA-TDI duration was 0.85, indicating that the reproducibility was good.
Endpoints and follow-up of patients
Patients were prospectively followed until the occurrence of cardiac events, and no patients were lost to follow-up after discharge (median follow-up period of 414 days, interquartile range 192–730 days). The endpoints were the following: (1) cardiac death, defined as death due to worsening HF or sudden cardiac death, and (2) worsening HF requiring rehospitalization. Sudden cardiac death was defined as death without definite preceding symptoms or signs and was confirmed by the attending physician.
Statistical analysis
Results are expressed as means ± standard deviation (SD) for continuous variables and as percentages of the total number of patients for categorical variables. Data for skewed variables are presented as medians with interquartile ranges. Independent t-tests and chi-squared tests were used for comparison of continuous and categorical variables, respectively. If data were not normally distributed, the Mann–Whitney U test was used. Cox proportional hazard analysis was performed to determine independent predictors of cardiac events for the entire population. Variables that were significant in the univariate analysis were entered into the multivariate model. The cardiac event-free curve was analyzed using the Kaplan–Meier method and compared using the log-rank test. Statistical significance was defined as P values < 0.05. Statistical analyses were performed using a standard statistical program (JMP software, version 11.2, SAS Institute Inc., Cary, NC USA).
Results
Clinical characteristics of the study subjects
There were 13 patients (13%) in NYHA functional class II, 47 patients (47%) in class III, and 40 patients (40%) in class IV. The etiology of HF was dilated cardiomyopathy in 24 patients (24%), ischemic heart disease in 31 (31%), valvular heart disease in 10 (10%), hypertensive heart disease in 19 (19%), and other causes in 16 (16%). During the median follow-up of 414 days, there were 37 cardiac events (37%) including 6 cardiac deaths and 31 rehospitalizations due to worsening HF. The clinical characteristics of patients with or without cardiac events are shown in Table 1. Patients with cardiac events were significantly older than those without. There were no significant differences identified in sex; NYHA functional class; prevalence of hypertension, diabetes mellitus, dyslipidemia, and paroxysmal AF; and the etiology of HF between patients with and without cardiac events.
Echocardiographic parameters
Patients with cardiac events had a significantly greater LAVI, E wave, E/E′ ratios, and a longer PA-TDI duration than did those without (Table 1). There were no significant differences in LVDd, LVEF, and E/A ratios between patients with and without cardiac events. There was a weak correlation between the PA-TDI duration and the LAVI (r = 0.232; P = 0.023) (Fig. 1a). However, simple linear regression analysis showed no correlation between the PA-TDI duration and age (P = 0.599) (Fig. 1b), E/E′ (P = 0.709) (Fig. 1c), and BNP (P = 0.565) (Fig. 1d).
The relationship between the PA-TDI duration and LAVI. The PA-TDI duration has a weak correlation with LAVI (r = 0.232; P = 0.023) (a). The relationship between the PA-TDI duration and age. The PA-TDI duration has no correlation with age (P = 0.599) (b). Relationship between the PA-TDI duration and E/E′. The PA-TDI duration has no correlation with E/E′ (P = 0.709) (c). The relationship between the PA-TDI duration and BNP. The PA-TDI duration has no correlation with BNP (P = 0.565) (d). LAVI left atrial volume index, PA-TDI prolonged total atrial conduction time on tissue Doppler imaging echocardiography, E/E′ the peak early (E′) mitral annular velocity was measured, and the ratio of the E wave to E′ (E/E′) was calculated, BNP plasma B-type natriuretic peptide
Blood markers and medication use
Although there was no significant difference in plasma BNP levels at admission between patients with and without cardiac events, plasma BNP levels at discharge were significantly higher in patients with cardiac events than in those without. eGFR was significantly lower in patients with cardiac events than in those without. There were no significant differences in medication use between patients with and without cardiac events.
Risk stratification by PA-TDI duration and clinical outcome
The univariate Cox proportional hazard analysis revealed that the PA-TDI duration was associated with cardiac events (Table 2). LAVI, E wave, E/E′, BNP, and eGFR were related to cardiac events. In a multivariable Cox analysis adjusted for age, LAVI, and E/E′, the PA-TDI duration was independently associated with cardiac events [hazard ratio (HR) 2.498; 95% confidence interval (CI) 1.684–3.714; P < 0.001; Table 3, model 1]. The PA-TDI duration remained independently associated with cardiac events with the adjustment for BNP instead of E/E′ (HR 2.542; 95% CI 1.727–3.745; P < 0.001; Table 3, model 2). The results were similar after the adjustment for eGFR instead of E/E′ (HR 2.476; 95% CI 1.726–3.582; P < 0.001; Table 3, model 3).
Supplemental Figure 1 is the scatter plot of the PA-TDI duration in patients with HF with and without cardiac events. There was a slight overlap in the distribution between the 2 groups. All patients were divided into tertiles according to the PA-TDI duration: first tertile ( < 131 ms, n = 33), second tertile (131–147 ms, n = 34), and third tertile ( > 147 ms, n = 33). Kaplan–Meier analysis demonstrated that the risk of cardiac events was significantly higher in patients in the third tertile than in the other groups (Fig. 2). We then categorized patients into four groups according to the median LAVI (51.3 mL/m2) and median PA-TDI duration (140 ms): low LAVI and short PA-TDI duration, low LAVI and long PA-TDI duration, high LAVI and short PA-TDI duration, and high LAVI and long PA-TDI duration. Figure 3 shows hazard ratios for cardiac events in patients stratified by LAVI and PA-TDI duration categories compared to those with low LAVI and short PA-TDI duration. Patients with high LAVI and long PA-TDI duration had the highest risk for cardiac events among patients with HF (HR 5.270; 95% CI 1.979–18.187; P = 0.005).
Discussion
The new findings from this study are as follows: (1) PA-TDI duration was associated with poor cardiac prognosis in patients with HF. (2) PA-TDI duration showed weak or no correlation to conventional echocardiographic parameters and BNP, suggesting that these parameters may have different prognostic significance. (3) The combined assessment of the PA-TDI duration and LAVI appeared to be clinically relevant to the risk stratification of adverse outcome in patients with HF.
Van Beeumen et al. [13] reported that atrial conduction delay is independent of the atrial tissue mass or the surface area in patients with HF. Atrial conduction disturbance results from the structural remodeling of the atria, characterized by the occurrence of fragmented atrial activity, regions of low voltage, and interstitial atrial fibrosis [14]. These findings demonstrate that this functional physiological parameter, atrial conduction time, is a surrogate marker of atrial remodeling. Ozer et al. [15] showed that the total atrial conduction time was longer in patients with mitral stenosis than in control subjects and that atrial conduction delay was related with LA size. Similarly, Caglar et al. [16] showed that the right atrial conduction time is longer in patients with chronic obstructive pulmonary disease than in control subjects, and they observed a positive correlation between the right atrial area and atrial conduction time. These indicate atrial size as being an important factor for determining the atrial conduction time.
Signal-averaged ECG is a noninvasive method for measuring the cardiac conduction time and has been used as the gold standard for determining the atrial conduction time. Atrial conduction time has been evaluated for atrial remodeling in some cardiac disorders such as paroxysmal AF, acute myocardial infarction, and congestive HF [8, 17, 18]. However, signal-averaged ECG is not routinely used in every hospital because of the requirement for special hardware and the time-consuming nature of the technique. On the contrary, atrial conduction time evaluated by TDI echocardiography is easy to assess in clinical practice. Merckx et al. [7] demonstrated that the PA-TDI duration showed a significant correlation with the signal-averaged P wave duration. Furthermore, Deniz et al. [19] demonstrated that the PA-TDI duration showed a fair correlation with the atrial conduction time as evaluated by an electrophysiological study. These findings support the finding that the PA-TDI duration is a feasible marker for total atrial conduction time.
Several studies have identified the PA-TDI duration as an independent predictor of new-onset AF, postoperative AF after cardiac surgery, and recurrent AF after catheter ablation and electrical cardioversion [20, 21]. These suggested that a prolonged PA-TDI duration is considered to be a predictor of the development of AF and a useful parameter of atrial remodeling. Waggoner et al. showed that the atrial conduction time is increased in patients with severe left ventricular systolic dysfunction and wide QRS interval [22].
However, the prognostic value of the PA-TDI duration in patients with HF has not been fully determined. For the first time, we demonstrated that the PA-TDI duration was an independent predictor of adverse cardiac events in patients with HF. Similarly, Bilgin et al. showed that atrial conduction delay is frequently observed in patients with systolic HF and is associated with mortality [23]. In their study, patients with systolic HF had prolonged PA-TDI duration (139 ms) compared with patients without HF (109 ms). PA-TDI duration in patients with systolic HF [ejection fraction (EF) < 50%] was 138 ± 20 ms in the present study which was equal to the results from the previous report.
In the present study, the PA-TDI duration did not correlate with E/E′ and plasma BNP levels at discharge. E/E′ and the plasma BNP level are established markers associated with LV end-diastolic pressure (LVEDP) [24, 25]. However, Doppler variables and plasma BNP levels are affected by hemodynamic changes and are easily altered. We suggest that the PA-TDI duration is less influenced by acute hemodynamic changes and reflects the atrial structural and the electrical remodeling more than other markers.
Our results are consistent with those in these earlier reports. In the present study, since there were 35 patients with a preserved EF, LVEF was not a significant predictor of cardiac events. By contrast, Hosseinsabet [26] showed that there was no significant difference in the atrial conduction time between patients with mild LV diastolic dysfunction and normal LA volume who showed normal LV filling pressure and healthy subjects. Kishima et al. [27] reported that atrial conduction delay was significantly associated with high LA pressure in patients with AF who have normal LA size. These findings suggested that the atrial conduction time can better reflect atrial pressure than atrial size. Atrial conduction time correlates to the severity of atrial remodeling rather than the atrial size itself in HF. Further, combined assessment of LAVI and the PA-TDI duration stratified patients with HF well.
Many previous studies have reported that AF is an independent risk factor for a deteriorating clinical prognosis in patients with HF. Finding a feasible prognostic predictor is still important even for patients without AF. The PA-TDI duration provides new insight into the evaluation of atrial remodeling.
The present study has several limitations. First, this study population was relatively small and from a single institution. The present findings should be validated in a larger prospective study. Second, the PA-TDI duration can be measured only in patients with sinus rhythm. Third, because echocardiography was not performed during follow-up, it remains unclear whether the long-term prognosis was affected by improvement in the PA-TDI duration. Fourth, since we included patients admitted for HF into this study, the characteristics of patients were heterogenous, including patients with different etiologies and varied EFs. Therefore, the study patients included both those with a preserved EF and a reduced EF. We could not perform a subanalysis to clarify the predictive value of the PA-TDI duration for HF patients with a preserved EF and a reduced EF because of the small number of patients in each subgroup. Further study with a large study population is needed for an adequate subanalysis.
Conclusion
The PA-TDI duration may be a feasible noninvasive parameter for predicting poor cardiac prognosis in patients with HF. It is important to evaluate not only structural LA remodeling but also functional LA remodeling.
References
Funk M, Krumholz HM (1996) Epidemiologic and economic impact of advanced heart failure. J Cardiovasc Nurs 10:1–10
CONSENSUS Trial Study Group (1987) Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 316:1429–1435
SOLVD Investigators (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 325:293–302
Tamura H, Watanabe T, Nishiyama S, Sasaki S, Arimoto T, Takahashi H, Shishido T, Miyashita T, Miyamoto T, Nitobe J, Hirono O, Kubota I (2011) Increased left atrial volume index predicts a poor prognosis in patients with heart failure. J Card Fail 17:210–216
Faggiano P, D’Aloia A, Zanelli E, Gualeni A, Musatti P, Giordano A (1997) Contribution of left atrial pressure and dimension to signal-averaged P-wave duration in patients with chronic congestive heart failure. Am J Cardiol 79:219–222
Hof I, Chilukuri K, Arbab-Zadeh A, Scherr D, Dalal D, Nazarian S, Henrikson C, Spragg D, Berger R, Marine J, Calkins H (2009) Does left atrial volume and pulmonary venous anatomy predict the outcome of catheter ablation of atrial fibrillation? J Cardiovasc Electrophysiol 20:1005–1010
Merckx KL, De Vos CB, Palmans A, Habets J, Cheriex EC, Crijns HJ, Tieleman RG (2005) Atrial activation time determined by transthoracic Doppler tissue imaging can be used as an estimate of the total duration of atrial electrical activation. J Am Soc Echocardiogr 18:940–944
Dixen U, Wallevik L, Hansen MS, Haghfelt A, Aqraou KF, Abildstrom SZ, Frandsen E, Jensen GB (2003) Prolonged signal-averaged P wave duration as a prognostic marker for morbidity and mortality in patients with congestive heart failure. Scand Cardiovasc J 37:193–198
McKee P, Castelli W, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285:1441–1446
Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TS (2006) Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol 47:2357–2363
Basnight MA, Gonzalez MS, Kershenovich SC, Appleton CP (1991) Pulmonary venous flow velocity: relation to hemodynamics, mitral flow velocity and left atrial volume, and ejection fraction. J Am Soc Echocardiogr 4:547–558
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ (2005) American Society of Echocardiography’s Guidelines and Standards Committee, European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Van Beeumen K, Duytschaever M, Tavernier R, Van de Veire N, De Sutter (2007) Intra- and interatrial asynchrony in patients with heart failure. Am J Cardiol 99:79–83
Khan A, Moe GW, Nili N, Rezaei E, Eskanadarian M, Botany J, Strauss BH (2004) The cardiac atria are chambers of active remodeling and dynamic collagen turnover during evolving heart failure. J Am Coll Cardiol 43:68–76
Ozer N, Yavuz B, Can I, Atalar E, Aksöyek S, Ovünç K, Ozmen F, Kes S (2005) Doppler tissue evaluation of intra-atrial and interatrial electromechanical delay and comparison with P-wave dispersion in patients with mitral stenosis. J Am Soc Echocardiogr 18:945–948
Caglar IM, Dasli T, Turhan Caglar FN, Teber MK, Ugurlucan M, Ozmen G (2012) Evaluation of atrial conduction features with tissue Doppler imaging in patients with chronic obstructive pulmonary disease. Clin Res Cardiol 101:599–606
Budeus M, Wieneke H, Sack S, Erbel R, Perings C (2006) Long-term outcome after cardioversion of atrial fibrillation: prediction of recurrence with P wave signal averaged ECG and chemoreflex-sensitivity. Int J Cardiol 112:308–315
Ciçek D, Camsari A, Pekdemir H, Kiykim A, Akkuş N, Sezer K, Diker E (2003) Predictive value of P wave signal-averaged electrocardiogram for atrial fibrillation in acute myocardial infarction. Ann Noninvasive Electrocardiol 8:233–237
Deniz A, Sahiner L, Aytemir K, Kaya B, Kabakci G, Tokgozoglu L, Oto A (2012) Tissue Doppler echocardiography can be a useful technique to evaluate atrial conduction time. Cardiol J 19:487–493
De Vos CB, Weijs B, Crijns HJ, Cheriex EC, Palmans A, Habets J, Prins MH, Pisters R, Nieuwlaat R, Tieleman RG (2009) Atrial tissue Doppler imaging for prediction of new-onset atrial fibrillation. Heart 95:835–840
Muller P, Schiedat F, Bialek A, Bösche L, Ewers A, Kara K, Dietrich JW, Mügge A, Deneke T (2014) Total atrial conduction time assessed by tissue Doppler imaging (PA-TDI interval) to predict early recurrence of persistent atrial fibrillation after successful electrical cardioversion. J Cardiovasc Electrophysiol 25:161–167
Waggoner AD, Kalathiveetil S, Spence KE, Dávila-Román VG, de las Fuentes L (2009) Interatrial conduction time and left atrial function in patients with left ventricular systolic dysfunction: effects of cardiac resynchronization therapy. J Am Soc Echocardiogr 22:472–477
Bilgin M, Yıldız BS, Tülüce K, Gül İ, Alkan MB, Sayın A, İslamlı A, Efe TH, Alihanoğlu Yİ, Zoghi M, Akın M (2016) Evaluating functional capacity, and mortality effects in the presence of atrial electromechanical conduction delay in patients with systolic heart failure. Anatol J Cardiol 16:579–586
Okura H, Kubo T, Asawa K, Toda I, Yoshiyama M, Yoshikawa J, Yoshida K (2009) Elevated E/E′ predicts prognosis in congestive heart failure patients with preserved systolic function. Circ J 73:86–91
Kazanegra R, Cheng V, Garcia A, Krishnaswamy P, Gardetto N, Clopton P, Maisel A (2001) A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail 7:21–29
Hosseinsabet A (2015) Assessment of atrial conduction times in patients with mild diastolic dysfunction and normal atrial size. Anatol J Cardiol 15:925–931
Kishima H, Mine T, Takahashi S, Ashida K, Ishihara M, Masuyama T (2016) The impact of left atrial pressure on filtered P-wave duration in patients with atrial fibrillation. Heart Vessels 31:1848–1854
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamaura, G., Watanabe, T., Tamura, H. et al. Prolonged total atrial conduction time evaluated with tissue Doppler imaging predicts poor cardiac prognosis in patients with heart failure. Heart Vessels 34, 1769–1776 (2019). https://doi.org/10.1007/s00380-019-01416-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01416-y