Abstract
The exact etiology and pathogenesis of chronic prostatitis (CP/CPPS) remain unclear. However, autoimmunity is a widely known theory. Precise treatment of CP/CPPS is not available. Here, we developed a new effective treatment method to prevent the occurrence of CP/CPPS. A total of 40 male C57BL/6 mice were randomly divided into four groups (n = 10): i.e., naive, model, high-dose (500 μg/ml), and low-dose (50 μg/ml) groups. High-dose and low-dose groups were orally given 0.4 ml of T2-containing soybean trypsin inhibitor (STI) at once after every 2 days for a total of 10 days. On day 10 and day 24 all the groups except naïve group were subcutaneously injected with 0.2 ml of T2 peptide along with CFA to make valid CP/CPPS models. Hematoxylin and eosin staining were used to evaluate the variation in CP/CPPS manifestation. Voiding behavior was recorded for the evaluation of urine frequencies. ELISA was used to measure the serum level of TNF-α in each group. The high- and low-dose groups of T2-containing STI displayed a reduction in urine frequencies, and inflammation, and there was a slight inflammatory infiltration as compared to the model group. In contrast, there was no difference observed in the TNF-α concentration of model as well as high- and low-dose groups compared to the naïve group. Our study demonstrates that oral T2-containing STI prevents CP/CPPS and provides an effective approach for the treatment of CP/CPPS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Chronic prostatitis is one of the common diseases in men, with an incidence of 2.5% to 16.0% and mostly occurs in male between the ages of 35 and 45 and impairing severely quality of life [18] in similar degree as Crohn’s, CHF (congestive heart failure), and Angina and DM (diabetes mellitus) diseases [25]. Among the American CP/CPPS is very common and occupying about 8% of visits to urologists, which mainly influence in the age group 36–50 years [7]. Patients of CP/CPPS manifest mostly a pain in the pelvic region, which can observe in the perineum, penis, perianal, urethra, pubic, or lumbosacral area. Abnormal urination can manifest as urgency, frequent urination, dysuria, and nocturia [29]. Currently, the pathogenesis and the etiology of CP/CPPS is unclear and very complicated. Therefore, effective treatment for CP/CPPS is not available.
Several theories explain the development of CP/CPPS including microbial infection, autoimmune theory, neurogenic inflammatory theory, local hormonal abnormality theory, and urine reflux theory [33]. In recent years, with the advancement in CP/CPPS animal models and data from clinical patients, there is increasing evidence that autoimmunity plays a significant role in the pathogenesis of CP/CPPS [23]. Domestic and foreign scholars have successfully established CP/CPPS animal models by using different methods for preparing autoimmune diseases. Rivero et al. [24] successfully created experimental autoimmune prostatitis (EAP) animal model in Wistar rats using adenoid extract combined with complete Freund’s adjuvant for the first time. Similarly, Zhou Xiaohui et al. [32] successfully prepared the Wistar rat experimental autoimmune prostatitis (EAP) model using prostate homogenate protein combined with complete Freund’s adjuvant.
Our laboratory has previously established CP/CPPS mice model by using the combination of T2 peptide and complete Freund adjuvant. In this model, there were increased T cells, and macrophage infiltration into the prostate stroma and glandular epithelium and significantly increased levels of TNF-α and IL-β along with the high amount of CRP. The T2 peptide is a promiscuous epitope of transient receptor melastatin 8 (TRMP8) protein that is CP/CPPS relevant and induces the syndrome in animal models [10, 12].
Oral soluble protein antigen induces antigen-specific immune tolerance in the body. Oral tolerance has excellent potential for clinical application due to its ease of use and non-toxic side effects and has applied to the clinical treatment of autoimmune diseases. In 1990, Nussenblatt et al. observed that the use of oral S antigens could alleviate the antigen-induced autoimmune uveoretinitis [22]. Autoimmune tolerance consists of central immune tolerance, and peripheral immune tolerance, which is a complex network of immune regulation that refers to the inability of T and B lymphocytes to produce an immune response to autoantigens in the body [15]. Symptoms of many animal models of autoimmune disease were alleviated by oral immunization. It had reported that oral administration of myelin could suppress autoimmune meningitis in Louise rats [3]. It has also been described that oral CII (type II collagen) delays and inhibits the incidence of CIA (collagen-induced arthritis) in WA/KIR rats and DBA/1 mice before modeling [21, 27]. At present, the existing treatment programs cannot satisfy patients and doctors. Therefore, there is a need to develop a new treatment method [6]. Here, in this study, we evaluated for the first time that oral T2-containing STI induces immune tolerance and improves the urinary symptoms in CP/CPPS mice model.
METHODS AND MATERIALS
Reagents
T2 peptide (an amino acid sequence of CSEEM RHRFR QLDTK LNDLKG) having molecular weight 2.57695 kDa is an antigenic epitope inducing autoimmune prostatitis; it was further synthesized and purified by Wuhan Buyers Biotechnology Co. Ltd. in China.
Complete Freund’s adjuvant (CFA) and STI (soybean trypsin inhibitor) were purchased from the Sigma Aldrich Chemical Co. (St. Louis, MO, USA). Mouse TNF-α (tumor necrosis factor-alpha) ELISA kit was purchased from Elabscience Biotechnology Co., Ltd. and was used according to manufacturer instructions.
Animals
Forty male C57BL/6 mice an average weight 18–22 g (6–8 weeks old) were purchased from the Qinglong shan mountain animal breeding farm (Nanjing, China). They all were housed and fed in an animal room with a 12-h light/dark cycle under standard temperature and relative humidity. The protocol for this study was approved by the animal committee of China Pharmaceutical University and confirmed with the guidelines for care and use of laboratory animals published by US national institute of health (NIH, 1996). Forty mice were randomly divided into four groups (n = 10): naive group, model group, high dose group, and low dose group. The naïve group was used as a control group.
Immunization
In the high dose group, 1000 μg/ml of T2 was mixed with 1000 μg/ml of STI in equal volumes. In low dose group, 100 μg/ml T2 was mixed with 100 μg/ml STI in the same volume. Except for the naïve and model groups, the high dose group (T2 was 500 μg/ml) and the low dose group (T2 was 50 μg/ml) were orally administered with 0.4 ml of T2-containing STI antigen once every 2 days for a total of 10 days.
Induction of CPPS Model
T2 was dissolved to 1 mg/ml of reserves for a combination of an equal volume of CFA. On day 10 and day 24, all the groups except naïve group were subcutaneously injected with 0.2 ml of T2 peptide with CFA to make valid CP/CPPS models. The final concentration of T2 was 225 μg/ml.
Voiding Behavior Analysis
On day 38th, voiding spot assay (VSA) test was used to analyze the voiding behaviors of mice [4] as described previously. In brief, immunized mice were individually kept on filter paper in a metabolic chamber for 1 h. Then, filter papers were collected, and images of urine spots were taken by using ultraviolet light. Finally, urine spots were evaluated by using the Fiji version of ImageJ software. Urine frequencies of mice were calculated by considering the number of urine spots (spots with size ≥ 6.6mm2 were considered). Blinded observers collected data.
Histopathology
The tissues of anterior lobe and the ventral lobe of the prostate were removed and fixed in 10% formaldehyde solution for 24–48 h. The tissues were dehydrated in ethanol, inserted in paraffin wax by a paraffin embedding machine, and cut into slices of 5-μm by a microtome for hematoxylin-eosin staining and observed under a microscope. A double-blind manner pathologically evaluated all prostatic pathology slices. The severity of the pathology and inflammation were assessed by 4-point scale. Point 0: no inflammatory cell infiltration or any signs of inflammation observed under the microscope. Point 1: small amount of epithelial acinar atrophy or a small amount of inflammatory cell infiltration observed under the microscope. Point 2: some epithelial acinar atrophy and some inflammatory cells infiltration observed under the microscope. Point 3: epithelial acinar atrophy, a large number of inflammatory cells infiltration and severe glandular congestion found under the microscope.
Enzyme-Linked Immunosorbent Assay
Enzyme-linked immunosorbent assay (ELISA) was used to determine the serum concentration of tumor necrosis factor-alpha (TNF-α). The blood taken from the heart of each mice was put on room temperature for 1 h. It was then centrifuged at 1000 rpm/min for 20 min, and the supernatant was collected and stored at − 20 °C. TNF-α was measured by a mouse TNF-α ELISA kit (Elabscuence Biotechnology Co., Ltd., China). All operations were performed in accordance following the manufacturer’s instructions.
Statistical Analysis
The statistical differences between naïve, model, high dose, and low dose groups were analyzed by one-way ANOVA test. Data were expressed as the mean ± standard error of the mean (SEM). The P value < 0.05 was considered a significant difference. The P < 0.01 was deemed to be an extremely significant difference.
RESULTS
Voiding Behavior
Voiding behavior was analyzed by VSA test. Urine spots were collected on filter paper. As shown in Fig. 1a, a significant number of urine spots, frequent urination, and largest area of urine spots were observed in the model group as compared to the naïve group indicating the successful induction of CPPS model. The high dose and the low dose groups showed a smaller number of plaques, lower urination, and a smaller area of plaques compared to the model group indicating successful induction of oral tolerance. In accordance with this result, the model group showed a significant difference with a high number of urine spots as compared to the naïve group (#P < 0.05) (Fig. 1b). Similarly, the high dose and the low dose groups showed a significant difference from the model group (*P < 0.05) with less number of urine spots. Compared to the naïve group, the high and low dose groups showed no significant difference. Also, there was no significant difference between the high dose group and low dose group. Thus, minimum micturition frequency and urine spots were observed in the groups treated with a high and low dose of T2-containing STI as compared with the model group (Fig. 1).
Voiding behavior analysis. a The number of collected urine spots processed by ImageJ software. b The number of urine spots. #P < 0.05 indicates the comparison of the model group with the naïve group.*P < 0.05 means the comparison of the naïve group, high dose group, and the low dose group with the model group.
Histopathology
H&E staining was used to score the severity of inflammation as described in the “MATERIALS AND METHODS” section. As shown in Fig. 2a, severe inflammatory cells infiltration, hyperemia in the glands, and atrophy of prostate epithelial acinar were observed in the model group as compared to the naïve group. There was no difference between the histopathology of the high dose group and the low dose group compared with the naïve group. Among the high dose group and the low dose group, no significant difference was observed. As expected, the inflammation score was more significant in the model group as compared to the naive group (#P < 0.05) (Fig. 2b). The high dose group and the low dose group showed minimal inflammation as compared to the model group (*P < 0.05). Compared to the naïve group, the high and low dose group exhibited no significant difference. Thus, high dose group and low dose group successfully reduced the sign of inflammation and inflammatory cell infiltration (Fig. 2).
a Histopathological observations of the prostate tissue from C57BL/6 mice (magnification × 400). b The inflammation score of each group. #P < 0.05 means there was a significant difference in the inflammatory score of the model group in comparison to the naïve group. *P < 0.05 means the inflammation scores of the naïve group, the high dose group, and the low dose group were significantly different from the model group.
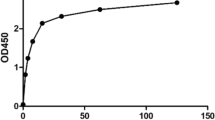
Serum Levels of TNF-α
ELISA was used to measure the serum expression level of TNF-α in C57BL/6 mice. As shown in Fig. 3, the model group was compared to the naïve group, but there was no significant difference observed. The high dose group and low dose group also did not show a significant difference as compared to the model group, and there was no significant difference between the high dose group and low dose group. When high dose group and low dose group were compared to the naïve group, also no significant difference was observed.
DISCUSSION
CP/CPPS is a complicated condition that results from chronic autoimmune reactions encouraging T cell-mediated impairment of prostate-tissues. Autoimmunity develops due to the failure of peripheral tolerance, which regulates self-reactive T and B cells. There are many methods for immune tolerance, including subcutaneous injection, intradermal injection, intravenous injection, oral administration, nasal mucosal administration, and portal vein administration [17]. The method of oral immune tolerance is relatively simple and convenient. Oral tolerance is defined as that after oral administration of a protein antigen, the body is induced to have no immune response or low response to the protein antigen while maintaining normal immune response to other antigens [31]. Oral tolerance appears after multiple small doses of exposure (100 ng–1 mg) or a single high dose of antigen (> 20 mg). These two forms of oral tolerance have different tolerance mechanisms [17]. Currently, mechanisms for oral tolerance are considered to include clonal deletion, clonal anergy, active suppression, and bystander inhibition [31]. Oral low-dose antigens can induce a low immune response through active suppression. Low-dose-tolerant effector cells are T cells. It has been shown that T cells produced by oral tolerance release cytokine-transforming growth factor-beta (TGF-β) mediators for internal and external inhibition [20]. Activated B cells, T cells, and macrophages secrete TGF-β [2]. According to a study [13], overexpression of transforming growth factor may play an essential role in the pathogenesis of ATL-related (adult T cell Leukemia) immunosuppression and hypercalcemia. Oral high doses of antigen can induce colony clearance. The apoptotic mechanism achieves clonal clearance. Oral administration of high doses of antigen to mice resulted in the inability of antigen-specific T cells in Peyer’s patch (PP), mesenteric lymph nodes (MLNs), spleen, and peripheral lymph nodes (LNs). Moreover, it also induces apoptosis of antigen-specific T cells in PP [26].
The induction of systemic immune tolerance by orally administered antigen is affected by various factors such as the time, dose, frequency, form of the oral antigen, and the genetic background of the immune host [30]. Currently, oral antigen immune tolerance has been used to prevent or treat autoimmune diseases in animals. According to reports, Lewis rats with experimental autoimmune encephalomyelitis (EAE) were clinically and histopathologically inhibited by oral myelin basic protein (MBP) [9]. In experiments with EAE tolerance to oral antigens, both CD4 and CD8 cells have been shown to mediate active suppression and anergy/deletion [8]. Research had shown that when insulin-derived B-peptide administered to NOD mice, diabetes effectively inhibited [19]. It has been previously reported that orally administered acetylcholine receptor (AchR) produced oral tolerance against myasthenia gravis induced by immunization with acetylcholine receptors plus CFA in Lewis rats. The results showed that it could prevent the clinical onset of autoimmune myasthenia gravis and significantly inhibit serum AhcRLgG antibody response and reduced muscle AchR loss [28].
The pathogenesis of CP/CPPS is currently unclear. Studies have shown that the pathogenesis of CP/CPPS is related to microbial infection, autoimmune abnormalities, neurogenic inflammation, oxidative stress, local hormonal abnormalities, and urinary reflux. At present, the abnormal autoimmune mechanism is a hot issue in the pathogenesis of CP/CPPS. Many studies had confirmed that the immune response causes CP/CPPS is due to autoimmunity. An autoimmune reaction is the cause of 35% CP/CPPS [16]. Studies have shown that there are T cells in the acinar of the prostate in CP/CPPS patients, and the presence of CD3, CD4, and CD8 cells is associated with serum and ejaculation interleukin concentrations and serum complement components [11, 34]. There also have macrophage, granulocyte, and B lymphocytes infiltrating the prostate interstitial in a CP/CPPS model [14, 34].
Immune factors act locally and initiate and regulate immune responses [1]. At present, CP/CPPS is treating symptomatically, and the successful treatment for CP/CPPS is still unsufficient. According to the 2014 edition of the Chinese urological disease diagnosis recommendation, patients are recommended oral antibiotics for 2–4 weeks and then decide whether to use antibiotics according to the efficacy [29]. For the improvement of urinary symptoms and pain, the recommended drugs are α-blockers, non-steroidal anti-inflammatory drugs, and M-receptor blockers [29]. Based on the principle of immune tolerance, our laboratory has developed a new idea for the treatment of CP/CPPS, by oral administration of T2 to achieve therapeutic outcomes and induce oral tolerance. The structure and possible mechanism of oral tolerance produced by T2 is shown in Fig. 4. T2 is a segment of a peptide isolated from transient receptor potential M8(TRPM8) protein. TRPM8 is expressed in the prostate, bladder, lung, dorsal root nerve. In previous studies in our laboratory, we have demonstrated that T2 can cause CP/CPPS as an autoantigen [5].
In this study, we administered high dose and low dose mixtures of T2 antigen and STI to the experimental groups 5 times for 10 days. After that, we induce CP/CPPS model with T2 and CFA emulsions, to observe whether oral antigens could prevent/alleviate CP/CPPS. From the histogram of urine spots, it shows that the urine spots in the model group are significantly different from the urine spots in the naïve group, representing the successful induction of CPPS model. The oral administration of T2 antigen in the high and low doses can improve the frequent urination and can reduce the inflammation in the mice model of CP/CPPS. In the serum concentration of TNF-α, no statistical difference was observed among the naïve, model, and high and low dose group, which might be due to the limited sample size.
Our results indicated that T2-containing STI was effective in improving CP/CPPS symptoms in mice models. The therapeutic efficacy of T2-containing STI was supported by a reduction in urination output and decreasing inflammation.
CONCLUSION
The results of this study demonstrated that oral tolerance induced by a mixture of oral T2 antigen and STI could alleviate CP/CPPS symptoms. The preliminary results of our study are promising and will provide a new way of thinking for the treatment of CP/CPPS. However, there is a need to further validate the therapeutic efficacy of this new approach.
References
Alexander, R.B., S. Ponniah, J. Hasday, and J.R. Hebel. 1998. Elevated levels of proinflammatory cytokines in the semen of patients with chronic prostatitis/chronic pelvic pain syndrome. Urology 52 (5): 744–749.
Assoian, R.K., B.E. Fleurdelys, H.C. Stevenson, P.J. Miller, D.K. Madtes, E.W. Raines, R. Ross, and M.B. Sporn. 1987. Expression and secretion of type beta transforming growth factor by activated human macrophages. Proceedings of the National Academy of Sciences of the United States of America 84 (17): 6020–6024.
Bitar, D.M., and C.C. Whitacre. 1988. Suppression of experimental autoimmune encephalomyelitis by the oral administration of myelin basic protein. Cellular Immunology 112 (2): 364–370.
Chen, H., L. Zhang, W.G. Hill, and W. Yu. 2017. Evaluating the Voiding Spot Assay in Mice: A Simple Method With Complex Environmental Interactions. American Journal of Physiology. Renal Physiology 313 (6): ajprenal.00318.02017.
Cheng, Y., Y. Cao, A.U. Ihsan, F.U. Khan, X. Li, D. Xie, X. Cui, W. Wang, Z. Liu, C. Li, K.A. Ahmad, K.R. Sembatya, R. Mikrani, and X. Zhou. 2019. Novel Treatment of Experimental Autoimmune Prostatitis by Nanoparticle-Conjugated Autoantigen Peptide T2. Inflammation 42 (3): 1071–1081. https://doi.org/10.1007/s10753-019-00968-5.
Cohen, J.M., A.P. Fagin, E. Hariton, J.R. Niska, M.W. Pierce, A. Kuriyama, J.S. Whelan, J.L. Jackson, and J.D. Dimitrakoff. 2012. Therapeutic intervention for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): a systematic review and meta-analysis. PLoS One 7 (8): e41941. https://doi.org/10.1371/journal.pone.0041941.
Collins, M.M., R.S. Stafford, M.P. O'Leary, and M.J. Barry. 1998. How common is prostatitis? A national survey of physician visits. Journal of Urology 159 (4): 1224–1228.
Faria, A.M., and H.L. Weiner. 2006. Oral tolerance: therapeutic implications for autoimmune diseases. Clinical & Developmental Immunology 13 (2–4): 143–157.
Higgins, P.J., and H.L. Weiner. 1988. Suppression of experimental autoimmune encephalomyelitis by oral administration of myelin basic protein and its fragments. Journal of Immunology 140 (2): 440–445.
Ihsan, A.U., F.U. Khan, W. Nawaz, M.Z. Khan, M. Yang, and X. Zhou. 2017. Establishment of a rat model of chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) induced by immunization with a novel peptide T2. Biomedicine & Pharmacotherapy 91: 687–692. https://doi.org/10.1016/j.biopha.2017.05.004.
John, H., A. Barghorn, G. Funke, T. Sulser, S. Hailemariam, D. Hauri, and H. Joller-Jemelka. 2001. Noninflammatory chronic pelvic pain syndrome: immunological study in blood, ejaculate and prostate tissue. European Urology 39 (1): 72–78.
Khan, Farhan Ullah, Awais Ullah Ihsan, Waqas Nawaz, Muhammad Zahid Khan, Mengqi Yang, Gang Wang, Xiaoqian Liao, Lei Han, and Xiaohui Zhou. 2017. A novel mouse model of chronic prostatitis/chronic pelvic pain syndrome induced by immunization of special peptide fragment with aluminum hydroxide adjuvant. Immunology Letters 187: S0165247817301669.
Kim, S.J., J.H. Kehrl, J. Burton, C.L. Tendler, K.T. Jeang, D. Danielpour, C. Thevenin, K.Y. Kim, M.B. Sporn, and A.B. Roberts. 1990. Transactivation of the transforming growth factor beta 1 (TGF-beta 1) gene by human T lymphotropic virus type 1 tax: a potential mechanism for the increased production of TGF-beta 1 in adult T cell leukemia. Journal of Experimental Medicine 172 (1): 121–129.
Krieger, J.N., L. Nyberg, and J.C. Nickel. 1999. NIH consensus definition and classification of prostatitis. JAMA 282 (3): 236–237.
Li, Lequn, and Vassiliki A. Boussiotis. 2006. Physiologic regulation of central and peripheral T cell tolerance: lessons for therapeutic applications. Journal of Molecular Medicine 84 (11): 887–899.
Li, Meng, Jinhu Wu, and Yonggang Chen. 2012. Advances in animal models of prostatitis. Medical Review 18 (4): 567–570.
Lloyd, Mayer, and Ling Shao. 2004. Therapeutic potential of oral tolerance. Nature Reviews Immunology 4 (6): 407–419.
Mahal, Brandon A., Jeffrey M. Cohen, Stephen A. Allsop, John B. Moore, Salman F. Bhai, Gino Inverso, and Jordan D. Dimitrakoff. 2011. The role of phenotyping in chronic prostatitis/chronic pelvic pain syndrome. Current Urology Reports 12 (4): 297–303.
Maron, R., M. Guerau-de-Arellano, X. Zhang, and H.L. Weiner. 2001. Oral administration of insulin to neonates suppresses spontaneous and cyclophosphamide induced diabetes in the NOD mouse. Journal of Autoimmunity 16 (1): 21–28. https://doi.org/10.1006/jaut.2000.0471.
Miller, A., O. Lider, A.B. Roberts, M.B. Sporn, and H.L. Weiner. 1992. Suppressor T cells generated by oral tolerization to myelin basic protein suppress both in vitro and in vivo immune responses by the release of transforming growth factor beta after antigen-specific triggering. Proceedings of the National Academy of Sciences of the United States of America 89 (1): 421–425.
Nagler-Anderson, C., L.A. Bober, M.E. Robinson, G.W. Siskind, and G.J. Thorbecke. 1986. Suppression of type II collagen-induced arthritis by intragastric administration of soluble type II collagen. Proceedings of the National Academy of Sciences of the United States of America 83 (19): 7443–7446. https://doi.org/10.1073/pnas.83.19.7443.
Nussenblatt, R.B., R.R. Caspi, R. Mahdi, C.C. Chan, F. Roberge, O. Lider, and H.L. Weiner. 1990. Inhibition of S-antigen induced experimental autoimmune uveoretinitis by oral induction of tolerance with S-antigen. Journal of Immunology 144 (5): 1689–1695.
Pontari, Michel A., and Michael R. Ruggieri. 2008. Mechanisms in Prostatitis/Chronic Pelvic Pain Syndrome. Journal of Urology 179 (5): S61–S67.
Rivero, Virginia E., Pablo Iribarren, and Clelia M. Riera. 1995. Mast Cells in Accessory Glands of Experimentally Induced Prostatitis in Male Wistar Rats. Clinical Immunology and Immunopathology 74 (3): 236–242.
Schaeffer, Anthony J. 2008. Epidemiology and evaluation of chronic pelvic pain syndrome in men. J International journal of antimicrobial agents 31: 108–111.
Sricharunrat, T., P. Pumirat, and P. Leaungwutiwong. 2018. Oral tolerance:Recent advances on mechanisms and potential applications. Asian Pacific Journal of Allergy and Immunology 36 (4): 207–216. https://doi.org/10.12932/ap0848.
Thompson, S.J., H.S. Thompson, N. Harper, M.J. Day, A.J. Coad, C.J. Elson, and N.A. Staines. 1993. Prevention of pristane-induced arthritis by the oral administration of type II collagen. Immunology 79 (1): 152–157.
Wang, Z.Y., J. Qiao, and H. Link. 1993. Suppression of experimental autoimmune myasthenia gravis by oral administration of acetylcholine receptor. Journal of Neuroimmunology 44 (2): 209–214.
Wu, Zaide, and Wu Yuhan. 2004. Surgery [M]. 6th ed, 683–684. Beijing: People’s Medical Publishing House.
Weiner, Howard L, Andre Pires da Cunha, Francisco Quintana, and Henry Wu. 2011. Oral tolerance. Immunological reviews 241 (1):241-259.
Xiaofeng, Han. 2001. Progress in the mechanism and application of oral tolerance. International Journal of Immunology 24 (5): 265–268.
Xiaohui, Zhou, Han Lei, Zhou Zhiheng, Liu Zhongde, Yang Jixiang, Lu Yanwei, and You Chunlai. 2005. Morphological and molecular biological characteristics of a rat model of immune chronic nonbacterial prostatitis. Chinese Journal of Andrology: 290–295.
Yanqun, A., Ye Zhangqun, and Sun Yinghao. 2014. Guidelines for the diagnosis and treatment of urological diseases in China. Beijing: People’s Health Publishing House.
Zhang, L., A.U. Ihsan, Y. Cao, Y. Cheng, and X. Zhou. 2017. Establishment of experimental autoimmune prostatitis model by T2 peptide in aluminium hydroxide adjuvant. Andrologia 50: 5.
Funding
This work was supported by the National Natural Science Foundation of China [Grant Nos. 30973003 & 30901993] and Administration of TCM of Jiangsu province [Grant No. LZ11093].
Author information
Authors and Affiliations
Contributions
Meng Tang, Rahat Ullah, and Junaid Wazir designed the study; Meng Tang and Rahat Ullah performed the experiments and wrote the manuscript; Xinxing Cui and Wenlu Wang contributed to the establishment of mice model. Min Hu and Yuqian Liu helped analyze the data; Farhan Ullah Khan and Awais Ullah Ihsan revised the manuscript; Xiaohui Zhou supervised the whole study.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tang, M., Ullah, R., Wazir, J. et al. Effect of Oral T2 Antigen on Chronic Prostatitis/Chronic Pelvic Pain Syndrome in Mice Model. Inflammation 42, 2086–2094 (2019). https://doi.org/10.1007/s10753-019-01072-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-019-01072-4