Abstract
Our objective was to study the impact of vaccinations on COVID-19 pandemic indicators across different regions of Malaysia. We collected population-level pandemic data from government open sources from 1 January 2021 until 30 June 2022. The aggregated data was then analysed by rates for vaccinations, infections, hospital admissions, intensive care unit (ICU) admissions, and case fatalities according to five regions in Malaysia. From the cumulative data, a total of 4,456,066 COVID-19 cases that contributed to 489,210 hospital admissions, 292,897 ICU admissions, and 35,378 deaths were operationalized to regional-levels, coherently stratified by pandemic-control measures. Vaccination rates were computed based on the proportion of people within each region who completed their primary doses (27,275,616 people) and booster shots (16,230,989 people). Geographic visualizations, ecological correlations, and ordinary least squares (OLS) regressions for statistically significant effect quantification were synthesized. Region-specific geo-visualization using choropleth maps confirmed that the indicators of the pandemic were effectively controlled with vaccinations. It was observed that a percent increase in vaccination rates resulted in a significant decrease in the rates of infections, hospital admissions, ICU admissions, and case fatalities. This reduction in pandemic indicators was greater in populations with higher booster vaccination rates across the country. However, the magnitude effect of those suppression coefficients as explained by the populations’ vaccination showed different gradients and varying consistencies, indicating the influence of geographical variations and pandemic control measures in different regions. Vaccinations were largely effective in reducing pandemic indicators but were not powered to halt or zero them. Trend reductions varied by regions and by pandemic control measures in place, suggesting that interventions for pandemic control are highly influenced by geographical contexts, coexistent with a certain degree of sustained mitigation strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic had a profound impact on health systems, the governance, and economies of countries worldwide at an unexpected rate. In response, global public health systems had to configure immediate suppression measures to contain the transmission of the SARS-CoV-2 virus. With public health containment measures rapidly implemented across different settings, biomedical scientists, major pharmaceuticals, and regulatory agencies expedited the development and emergency use authorisation of COVID-19 vaccines for active immunization of eligible populations to prevent the coronavirus disease. These COVID-19 vaccines utilised a range of platforms, including traditional (inactivated, live-attenuated, recombinant vaccines) as well as innovative technologies (mRNA, DNA, adenoviral vector vaccines) (Sikora & Rzymski, 2022).
In the real-world, COVID-19 vaccines administered to populations showed different levels of effectiveness, suggesting that epidemiological targets of the pandemic may vary across specific settings and geographical locations (Ganasegeran et al., 2021a). Although assessments of individual-level data demonstrated the ability of vaccines to decrease severe complications and clinical endpoints (Polack et al., 2020), these evaluations were not powered to offer epidemiological insights. Therefore, the aggregation of regression-based prediction trends from a population-level to local public health systems is essential for the development of effective pandemic suppression strategies and the attainment of herd immunity in response to outbreaks. Clinical-evidence at the individual-level on infection suppression, transmissibility, and associated comorbidities or complications are mainly influenced by biological factors. On the other hand, the control of an outbreak and indicators at an area-level are influenced by the environmental or external exposomes, mediated by population’s demography, compactness of cities, network contacts, mobility, health literacy, and people’s behaviour (Ganasegeran et al., 2021a, 2022; Mollalo et al., 2021). Complementing individual-level evidence and sparse spatial-vaccination uptake evidence from previous works (Chen et al., 2023; Ganasegeran et al., 2021a, 2022; Mollalo et al., 2021), here, we describe the potential strategies for controlling the pandemic at the area-level (regions) in Malaysia within the conjugate effect of vaccinations, mitigation or containment measures, and the COVID-19 pandemic indicators over time.
Territorial interventions during outbreaks play a critical role in the governance of health systems. It involves exercising of political, economic, and executive authority and obligations over public affairs and safety through strategic management, direction-setting, and rule-making of healthcare decisions. These interventions are vital in achieving national targets for pandemic containment while sustaining a functional healthcare system. The COVID-19 geometric spread was highly heterogeneous causing unforeseen challenges to crisis management and policy responses. The territorial impacts of the pandemic were observed through four critical dimensions, namely health, economic, social, and fiscal systems. In order to effectively sustain these dimensions, it is essential for national (i.e., federal) and subnational (i.e., state, local) governments to promptly implement response measures to control the spread and swiftly conduct vaccination campaigns across all levels of the population to mitigate the territorial effects of the crisis (OECD, 2021). The external capacity is where subnational governments secure vaccines from the federal crisis response centre during periods of high vaccine demand, whereas the internal capacity refers to the speed at which these subnational governments can vaccinate the local population to meet targets aimed at reducing critical pandemic indicators such as cases, hospitalisations, ICU admissions, and deaths (Tevdovski et al., 2022). Our current research is based on this workflow, examining the evolution of pandemic indicators over time with vaccinations at different containment phases of the country’s pandemic response strategy. The purpose of this study is to understand how vaccination efforts can be optimized at a regional level to effectively control the transmission of COVID-19 and reduce the burden on healthcare systems.
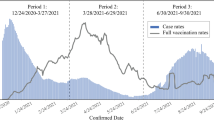
Pandemic control phases
All pandemic indicators were aggregated from state level to the regional levels and stratified by different epidemiological phases of the country’s outbreak response. From January 2021 to June 2022, the country transitioned into six core phases of the pandemic control. These phases included the implementation of the Movement Control Order (MCO) between January 2021 and May 2021. During the MCO phase, each state had to achieve targeted indicators before being relaxed from strict containment measures. Depending on the severity of the situation, the states switched between MCO, Conditional Movement Control Order (CMCO), Recovery Movement Control Order (RMCO), and Enhanced Movement Control Order (EMCO).
In June 2021, the country once again transitioned to a nationwide total lockdown (Phase 1 of the containment measure). Subsequently, in July 2021, the country introduced the National Recovery Plan (NRP) over a period of 9 months, allowing the transition to an endemic phase. The status of containment measures varied across different states, with Phases 2, 3, and 4 allowing for different degrees of relaxation subjected to the state's targeted pandemic indicators being achieved. To ease statistical interpretation, the nine months of NRP phases 2, 3, and 4 were classified as the three-monthly duration of NRP 1, NRP 2, and NRP 3 respectively. Between April 2022 and June 2022, the country began transitioning to an endemic phase, with plans to reopen social, economic, and international borders (Fig. 1) (National Security Council, 2022). Our rationale for analysing the linkage on the effectiveness of vaccine coverage at different pandemic control phases lies within the community structured compartmental model synthesis proposed by Aruffo and colleagues (2022). While extensive vaccine coverage could significantly decrease the number of cases and fatalities, it was observed that relaxation of mitigation and containment strategies in specific regions during certain phases could lead to a resurgence of infections, even when vaccine coverage was high. Conversely, tighter mitigation and containment measures were found to reduce local transmissions. Under these circumstances, it was recommended that a minimum of 60% vaccine coverage in areas or phases with tighter containment measures would be sufficient to prevent new infections (Aruffo et al., 2022). Our interest in understanding the distribution patterns of infectiousness serves as a catalyst to public health advocates to strategize optimal vaccine distribution, with a focus on prioritizing vulnerable populations in local areas, considering the time-lag for governments to acquire vaccine doses for mass vaccination. Furthermore, with this phase-wise geographical distribution for optimal vaccine coverage, it would be essential to identify the threshold for the next epidemiological transition – determining when it is safe to relax or completely lift mitigation and containment measures. Following these justifications and needs-gaps, our current work proposes the following approach: (1) recognising regional differences in vaccine coverage and uptake rates among populations; (2) acknowledging that the saturation of vaccine coverage and its impact on critical pandemic indicators may exhibit geographical variations; (3) understanding that these variations are influenced by the different phases of mitigation and containment measures in Malaysia; and (4) highlighting that the findings of this study can help guide national and subnational governments in planning vaccine distribution in areas of high vulnerability, as well as to identify factors of “risk–benefit assessments” and “risk–benefit considerations,” and evaluate the subsequent actions required for pandemic control measures, such as easing or tightening mitigation and containment measures, while understanding local geographies and communities response patterns towards vaccine uptake. The overall statistics data used to yield the parameter of pandemic indices are summarized in Table 1 (Ministry of Health Malaysia, 2022a, 2022b).
Different phases of the pandemic control measures according to states in Malaysia [Note: Phase-wise chart developed by the authors based on summary information from the National Security Council, 2022]
Current situational analysis
During the period spanning from July 2022 to February 2024, we have observed intermittent surges in the number of COVID-19 cases from the end of the vaccination campaigns (Appendix 1 see Fig. 9). However, the critical pandemic indicators have displayed a relatively low and plateaued trending over time since the post-vaccination period (Appendix 1 see Fig. 9). These trends suggest that while the population remains susceptible to contracting COVID-19, the severity of the infections has decreased from a population perspective as a result of the vaccination campaigns. However, with diverse population attributes and different geographical circumstances and demographic shifts, densification, and urbanizations, we believe that this study would contribute additional insights to existing literature. In addition to understanding the population risk-reduction of COVID-19 and their complications with vaccinations at the individual level, the study aims to investigate whether the impact of vaccinations differ within communities based on their geographic locations. This aspect is relatively sparse in the current vaccine epidemiology literature.
Methods and materials
Study design and setting
This countrywide geo-ecological study was conducted using real-time nationally representative pandemic data captured between 1st January 2021 until 30th June 2022 across thirteen states and three federal territories, nested in five major regions of Malaysia. The epidemiological analysis was conducted using regional aggregated data from state-level counts as depicted in the baseline map (Fig. 2).
Data sources
Data on daily COVID-19 cases, hospital admissions, intensive care unit (ICU) admissions, fatalities, primary vaccinations, and booster vaccinations were analysed between 1 January 2021 until 30 June 2022 (data retrieved from a single time point on 7 July 2022) sourced from the COVID-19 Malaysia GitHub Open Data portal (Ministry of Health Malaysia, 2022b). The data can be accessed freely on GitHub via Jupyter Notebook programming from the following link: https://github.com/MoH-Malaysia/covid19-public. The Malaysian government has granted a free use license for this data (Appendix B of the Circular on Implementation of Open Data Bil.1/2015). Administrative shapefiles were obtained from the 2019 Malaysia-Subnational Administrative Districts and States Data (United Nations Office for Coordination of Humanitarian Affairs, 2023).
Computations of the COVID-19 pandemic indicators
COVID-19 crude rates were computed as the total number of cases per 100,000 population for each region in Malaysia. Hospital admission rates were computed as the proportion of the total admissions amongst cases for each region. ICU admission rates were computed as the proportion of total ICU admissions amongst cases for each region. Case fatality rates were computed as the proportion of total deaths amongst cases for each region. Vaccination rates were calculated as the proportion of cumulative vaccinations amongst the total population in each region. Booster vaccination rates were calculated as the proportion of cumulative booster administrations amongst the total population in each region.
Cartography development
To visualize how vaccinations changed with population’s pandemic indicators by geography, we first determined a classification scheme that was deemed suitable to yield a sufficient proportion of the population to be vaccinated, countrywide, stratified by regions in Malaysia. Assuming a vaccine efficacy of 95% within a series of lag time during Malaysia’s pandemic times while interventions were still in place, we determined our critical vaccination threshold as 78%, based on our previous work, through a mathematical epidemiological synthesis developed for Malaysia, as published here (Ganasegeran et al., 2021a). Given that the threshold of herd immunity is influenced by the proportional vaccine efficacy value (ε), and we postulate that a desirable efficacy for vaccines administered to the Malaysian population as 95%; hence in our previous work an extended formula to calculate the threshold of herd immunity or impacts to reversal for pandemic indicators utilised the formula Pcrit = 1 − (1/Rt)/ε, where Pcrit (critical level) is defined as the minimum number of the population that needs to be vaccinated, based on time-varying reproduction number (Rt) estimator. The parameter synthesized was based on assumptions that the whole population was susceptible to COVID-19 at the time of calculation and that the Rt was a valid parameter yielded prior to any interventions being in place or at the beginning of the outbreak (Anderson and May, 1992; Kwok et al., 2020; Ganasegeran et al., 2021a).
Next, we developed a second classification scheme to disaggregate the effect of vaccinations on population’s COVID-19 infections, hospital admissions, ICU admissions, and case-fatality rates, based on three categorical percentile classifications: 0 to less than 33%, 33% to less than 66%, and 66% to 100%, representing low, moderate, or high level of pandemic indicators, respectively. We then developed a series of pre- and post-critical thresholds of choropleth maps to visualize the effect of vaccinations on the geographical differences of the population’s pandemic indicators by regions in Malaysia. ESRI’s administrative data shapefiles were layered by different administrative borders (states and regions) and were subsequently joined to attribute data. Choropleths were synthesized through “Symbology” using Quantum GIS (QGIS), version 3.22 Bialowieza software.
Statistical analyses
Correlation analysis was conducted between vaccination and booster vaccination rates with pandemic indicators across the five regions in Malaysia. Pearson correlation coefficient (r) values that ranged between − 1 and + 1 were synthesized (Gogtay & Thatte, 2017; Schober et al., 2018). Coefficient values nearing − 1 were interpreted as two attributes being more negative-linearly correlated (i.e., as vaccination rate increases, the impact burden of the pandemic indicator reduces), while coefficient values approximating 0 indicate that the two attributes have no linear correlations, and coefficient values nearing + 1 indicate that the two attributes are more positive-linearly correlated (i.e., as vaccination rate increases, the impact burden of the pandemic indicator increases). The size of the effect (r) could be interpreted as follows: (1) 0.10 to 0.29 (or − 0.10 to − 0.29) as a small positive (or negative) correlation; (2) 0.30 to 0.49 (or − 0.30 to − 0.49) as moderate positive (or negative) correlation; (3) 0.50 to 1.00 (or − 0.50 to − 1.00) as large positive (or negative) correlation (Cohen, 1988).
We computed region-based ordinary least squares (OLS) regression models to predict the association of a percentage increase in populations’ vaccination rates on pandemic indicators. Multicollinearity was assessed between covariates. Statistical significance was set at p < 0.05. Our justification of choosing an OLS regression method lies within the requirement to choose a statistical method that is methodological correct to yield place-based summary magnitudes interlinked within our aims and objectives of public health importance. Since pandemic control measures and public health policies are not made at an individual level, but instead at an aggregate level, our statistical approach was primarily ecological-regression based, but assured to be of minimal bias, confounding, and overfitting. As we were dealing with rates at an aggregate areal-level (i.e., regions) with the outcome variable being continuous in nature, our modelling lies within the base execution of a linear regression. With different variants of linear regressions available, we chose the algorithm of an Ordinary Least Square (OLS) estimator that is regarded as the Best Linear Unbiased Estimator (BUSE), capable to work precisely to predict covariates influencing the outcome variable (i.e., vaccination rates) within locations, and when linkage to spatial weights are executed, the OLS model is capable to direct us if the outcome variable is subjected to the influence of neighbouring locations via diagnostic features of spatial dependence. These capabilities are executed within OLS regression under Gaussian-Markov assumption, and works considerably well in predicting covariates influencing the spread of disease geographically during epidemics (Milton et al., 2019). The mathematical equation of the OLS regression is expressed as follows:
whereby y is a vector of the outcome variable (vaccination rates), X is a matrix of observations of the covariates, \(\beta\) is a vector coefficient for the covariates, and \(\varepsilon\) is the vector of independent and identically distributed random error terms (Chi & Zhu, 2020; Gebreab, 2018).
Subsequently, the univariate and multivariate OLS models are capable of yielding collinearity statistics, a parameter value subjected to detect the extremes of confounding – the Variation Inflation Factor (VIF). We executed a univariate OLS model prior to variable selection into the multivariate OLS regression, indicating that minimal VIF values (less than 5) were not subjected to the presence of confounders. To strengthen our statistical justification, we planned to apply “Queen’s Contiguity” weights within the OLS model, however, by default, the training algorithm would be rejected in view of the number of covariates exceeded the number of observations (i.e., the spatial units of five regions in Malaysia) by one variable. But statistical interpretations need to be supported with public health significance; while overfitting of spatial based regression models were avoided due to the above circumstances, our main outcome of vaccination rates had direct causal interpretations with key pandemic indicators (i.e., COVID-19 cases, hospital admissions, ICU admissions, mortalities), a finding which would be substantially important for “risk–benefit assessment” during emergency pandemic times.
Results
Trends of pandemic indicators by regions in Malaysia
Table (2) shows region-based trends of pandemic indicators stratified by phases of pandemic control measures. The overall incidence of COVID-19 cases reported per day ranged between 17.25 cases per 100,000 population (95% confidence interval [CI] 17.24 – 17.27) in the East Malaysia region to 36.97 cases per 100,000 population (95% CI 36.95 – 37.00) in the Central region. Hospital admissions per day ranged from 9.17% (95% CI 9.17 – 9.18) in the Central region to 28.72% (95% CI 28.70 – 28.74) in the East Malaysia region. ICU admission rates per day ranged from 7.36% (95% CI 7.35 – 7.36) in the Central region to 14.51% (95% CI 14.48 – 14.53) in the East Malaysia region. Case-fatality rates ranged from 0.53% (95% CI 0.53 – 0.53) in the Northern region to 0.72% (95% CI 0.72 – 0.72) in the East Malaysia region (note: in view of small parameter values, see Table 2 for complete reporting up to four decimals).
Regional-based geo-visualization of vaccination rates
Vaccination rates (both primary and booster doses) were moderate-to-highly prevalent across the urbanized and densely populated areas within the Central, Southern, and Northern regions of Malaysia. Vaccine uptakes were relatively low within the rural areas of the East Coast and East Malaysia regions (Figs. 3 & 4).
Regional-based geo-visualization of COVID-19 pandemic indicators with vaccination
We found that COVID-19 incidence cases per 100,000 population were significantly reduced across all regions in Malaysia when population’s vaccination rates reached the critical threshold for vaccine effectiveness (Figs. 5A & 5B). Except for the Northern and East Coast regions of Malaysia, hospital admission rates were reduced when the population's vaccination rates reached the critical threshold for vaccine effectiveness (Figs. 6A & 6B). Similarly, except for the East Coast region, ICU admission rates were reduced when the population's vaccination rates reached the critical threshold for vaccine effectiveness (Figs. 7A & 7B). Case-fatality rates showed similar geographic trends with incidence cases, with low-to-moderate fatalities observed across all regions when the critical threshold for vaccine effectiveness were achieved (Figs. 8A and 8B).
Case fatality rates by regions in Malaysia. COVID-19 case fatality rates (%) by regions in Malaysia based on (A) proportion of population vaccinated below critical threshold for anticipated vaccine effectiveness; (B) proportion of population vaccinated at critical threshold for anticipated vaccine effectiveness
Correlation between vaccination rates and pandemic indicators
For those who received complete primary dose vaccination, we found an overall statistically significant negative correlation with hospital admission in the Northern (r = -0.55, p < 0.01), Central (r = -0.72, p < 0.01), Southern (r = -0.73, p < 0.01), East Coast (r = -0.59, p < 0.01), and East Malaysia (r = -0.83, p < 0.01) regions. For critical pandemic indicators, we found statistically significant large negative correlations between primary dose of vaccination and ICU admissions across all regions in Malaysia (r values ranged from -0.75 for Southern region to -0.59 for East Malaysia; p < 0.01). Except for the Northern region, statistically significant negative correlations between vaccinations and case fatalities were observed for the Central (r = -0.40, p < 0.01), Southern (r = -0.22, p < 0.01), East Coast (r = -0.12, p < 0.01) and East Malaysia (r = -0.04, p < 0.01) regions. We found that vaccinations and incidence of COVID-19 cases showed statistically significant positive correlations across all regions (p < 0.01). However, when stratified by phases of pandemic control, we observed that vaccination rates and pandemic indicators showed fluctuant correlation effects, depending on the level of control measures executed in each phase across the regions (Table 3). Strict control phases showed negative correlations and phases with relaxed measures showed positive correlations. Similar trends were observed for correlations between booster vaccinations and pandemic indicators, but here, most indicators across regions showed greater suppression effects as evidenced by stronger correlation coefficients (Table 4).
Associations between vaccinations and pandemic indicators by Ordinary Least Squares (OLS) regression
We first fitted a univariate Ordinary Least Squares (OLS) regression model (see Appendix 2 Table 6) and observed that the VIF values were relatively small (less than 5). We subsequently fitted all covariates into the multivariate OLS model. Table 5 exhibits results of the multivariate Ordinary Least Squares (OLS) regression on the impact of pandemic indicators from vaccinations across the five regions of Malaysia. The OLS model predicted that for every one percentage increase in primary vaccination rates, the associated daily incidence of COVID-19 cases reduced by 0.18 cases per 100,000 population in the Northern region (p < 0.05), 0.12 cases per 100,000 population in the Central and East Coast regions (p < 0.01, p < 0.05 respectively), 0.26 cases per 100,000 population in the Southern region (p < 0.01), and 0.25 cases per 100,000 population in the East Malaysia region (p < 0.01). Similar trends were observed for booster vaccination rates across all regions, except for the Central region that was not statistically significant. A percentage increase in primary vaccination rates was associated with a decrease in daily hospital admissions by 0.63% (p < 0.05), 5.03% (p < 0.01), 1.41% (p < 0.01), 0.55% (p < 0.01), and 0.93% (p < 0.01) in the Northern, Central, Southern, East Coast, and East Malaysia regions respectively. Except for the Northern region, further reductions of hospital admissions were observed for the rest of the regions with a percentage increase in booster vaccinations, and these associations were statistically significant.
For critical pandemic indicators, a percentage increase in primary vaccinations was associated with reduction in daily ICU admissions by 3.03% (p < 0.05), 1.40% (p < 0.05), 2.84% (p < 0.01), 2.50%, (p < 0.01) and 0.51% (p < 0.01) in the Northern, Central, Southern, East Coast, and East Malaysia regions respectively. Similar associations were observed for all regions with a percentage increase in booster vaccinations (p < 0.01). Except for the Northern and East Malaysia regions, a percentage increase in primary vaccinations resulted in a decrease of case fatality rates by 3.34%, 13.73%, and 3.07% in the Central, Southern, and East Coast regions of Malaysia, and these associations were statistically significant (p < 0.05). All regions showed a statistically significant reduction of case fatality rates with a percent rise of booster vaccinations (Table 5). The regression models explained that percent of variation in primary vaccination rates and booster vaccinations as elucidated by the pandemic indicators varied by regions in Malaysia. The indicators were lowest for the East Coast and the highest for East Malaysia (Table 5). There was no multicollinearity between covariates as VIF values were less than 5.
Discussion
Core summary findings
This ecological analysis examined the associations between COVID-19 vaccinations and pandemic indicators in Malaysia. Geo-visually, we observed a reduction in daily rates of infections, hospital admissions, ICU admissions, and case fatalities with vaccinations by regions in Malaysia. Correlation wise, these indicators showed similar trends, and further suppressions were observed in boosted individuals across all regions in Malaysia. The region-based models explained that the effect of vaccinations (adjusted R-squared values) on pandemic indicators was the lowest for the East Coast region and the highest for the East Malaysia region. We found that vaccinations inversed all pandemic indicators, however, the magnitude effect (betas) varied between regions and likely influenced by the level of pandemic control measures.
Comparisons with existing literature
The impact reduction of the pandemic indicators found in this study was consistent with previous findings (Rahman et al., 2022; Valeanu et al., 2023; van Diepen et al., 2023; Whittaker et al., 2022). However, the connection between vaccination and suppression of the pandemic indicators in these studies were only illustrated at the individual-level which are plausibly linked to biological and physiological processes in humans. Although these arguments are useful clinically to identify therapeutic targets, they are not powered to sustain epidemiological plausibility for population-level pandemic control interventions that are highly interconnected within the attributes of socio-spatial-ecological framework (e.g., population’s demography, compactness of living conditions or population density, poverty, rural–urban gaps, circumstances of human living settlements, and proximity to health services or built-environment landscapes).
The mobility of people in highly densely populated regions could facilitate the introduction, spread, or persistence of infections. Densification could be a proxy attribute for high contact rate because of mobility rather than individual’s physical proximity (Ganasegeran et al., 2021b). The Northern, Central, and Southern regions of Malaysia may illustrate this scenario as the states nested within these regions comprise of urban metropolitans, industrial, and economic areas that cultivate high gross domestic product (GDP) growth and employment opportunities, catalysing internal migrations alongside with high human mobility, which are likely to observe greater risk of infections and fatalities. Similar argument was made in a previous study (Fonseca-Rodriguez et al., 2021). This interpretation is supported in our results, as the trends of cases and fatalities, although reduced, remained fluctuant across regions, mediated by area-level public health containment phases between regions. Next, these inconsistencies could also be attributable to indoor ventilation during pandemic measures. Regions with higher population densities or urban areas tend to have greater number of household family members or inhabitants, coupled with the built-engineering of homes, and crowded spaces tend to increase the risk of transmissions and respiratory complications in vulnerable groups (Baker et al., 2023; Li et al., 2021; Ng et al., 2022; Shen et al., 2021).
We could not deny the possibilities that the impact of vaccinations on key pandemic indicators explored in our analyses at the population-level could be influenced by spatial demography and social-vulnerabilities of the population's living circumstances. The three densely populated regions as discussed above could have displaced persons based on economic inequalities, ethnic minorities, employment opportunities, poverty, aging population, neighbourhood social environments, or gentrification, all of which require targeted interventions to address high health needs for outbreak control.
We note from our regional-regression analysis that the models explained the variance of effect on vaccinations for pandemic indicators was the lowest for the East Coast region and the highest for the East Malaysia region, both populated by rural areas. The wide differences could plausibly be influenced by rural–urban gaps, vaccine acceptance, socio-cultural acceptance or beliefs in vaccines and health literacy amongst the population in these areas. The relatively lower magnitude coefficients of the pandemic indicators could be influenced by the geography of the regions, in which human settlements are more dispersed to the outskirts with lesser populated inhabitants, and infrastructure barriers to sustain interconnection between communities, which has high tendency to limit infection transmissions and complications caused by COVID-19. We could not deny the possibility that the regional distribution of different vaccines with different levels of effectiveness would influence the fluctuant trends of key pandemic indicators (Suah et al., 2021). However, we note that the distribution of vaccines should consider the highly vulnerable groups and the identification of areal-level structural and contextual barriers for easy administration and acceptability to communities within the public health contingency plan.
Methodological implications
We note that the functional nature of any spatial data is intrinsically geographic, being capable to reference point-level locations via coordinates (latitude or longitude) or area-level projections via shapefiles to intuitively display patterns, distributions, or trends of data within geographical boundaries that are complemented with descriptive place-based summary geo-statistics (Adrian et al., 2020). Such capabilities are projected through maps which visualize real-life stories of a studied problem. Under these circumstances, our study offered a clear visualization through maps, stratified by regions on the effects of vaccinations on pandemic indicators, in which conventional reporting through tabular data is not powered to do so. We acknowledge that although tabular data is powered to describe the magnitude of values of one group to another, it is incapable to describe patterns or trends in datasets in which place-based spatial data could do via map visualizations, which is consistent with a previous argument that geo-visualization techniques offer better comprehension of risk magnitudes during pandemic times or infectious disease outbreaks (Zhang et al., 2022). We applied this dictum to our study. As the triad of epidemiological investigations include “place” in addition to “time” and “person,” geo-visualization techniques through the building of basic choropleth maps provide clear descriptions on the variations of pandemic indicators that are met prior to and after critical thresholds of vaccinations for pandemic suppression. These maps are yielded through colour gradients through area-estimates (Shaito et al., 2022), hence provide clear descriptions on the variations of COVID-19 disease rates and other outcome indicators on the effectiveness of vaccinations through the visualization of geographical patterns and trends.
Implications for pandemic control and policy
Our results suggest that critical pandemic indicators such as ICU admissions and case fatalities could be significantly reduced with vaccinations, however, the spread of the disease could not be completely suppressed with immunisation alone; in other words, it would be difficult to achieve herd immunity for COVID-19. The primary goal for pandemic control through population vaccination targets could leverage a high extent to minimizing deaths and serious complications (Liu et al., 2021). Nonetheless, the geometric spread and transmissibility within communities that are highly possible to recur or being persistent could be mediated by the compactness of cities, people’s acceptability to periodical immunisation, social and cultural acceptance, vaccine effectiveness, and emergence of new variants, hence, configuration of an acceptable level of continued public health mitigation and containment measures should be in place.
Despite the Malaysian government’s effort to provide equitable access to a diverse range of vaccines (Suah et al., 2021), the rural areas of the East Coast and East Malaysia regions have experienced low vaccine uptake. Despite the decrease in hospital admissions and ICU admissions at post critical thresholds of population vaccinations, these regions somewhat showed moderate incidences of hospital and ICU admission rates. It could be argued that these regions could have regional characteristics that could pose challenges for population’s access to vaccine centres due to geographic barriers to health facilities, as well as factors such as people’s perception towards vaccinations, cultural sensitivities, and health literacy on the importance of vaccine uptake. Populations within these regions should be more cautious on the complications of COVID-19, their mitigation protocols, and the significance of vaccine uptake during pandemic exigencies. Efforts to intensify awareness, health literacy, and assurance within culturally sensitive populations needs to be executed to inculcate the importance of vaccinations programs in reducing critical health complications. These could be done through programs via community engagements or media campaigns as suggested in a recent study (Odunsi et al., 2023).
Future direction
We recommend future works to incorporate spatio-temporal analysis of place-based determinants, either at a finer scale for more accurate local comparisons of predictors or at a regional scale to pool higher level comparisons within or between countries to set global public health priorities in pandemic control. We note that there is a need to differentiate the goals for geographical-based studies within anticipated public health targets during pandemic times. In emergency response situation, the goal of territorial or geographical visualizations on the impact of key pandemic interventions are specifically intended to be a “risk–benefit assessment” requirement within public health governance; that is how would the critical pandemic indicators change overtime or be controlled with vaccinations across regions or territories that offer sustainability and survivability to overwhelmed healthcare systems. To successfully visualize the trends and patterns of these targets, it would be best to assess the risk–benefit interventions by public health advocates at higher area-level boundaries or spatial units for optimization of decision-making at the national level. But to achieve the intended targets of the national “risk–benefit assessment,” it is indeed required to understand the patterns of “risk–benefit considerations” of vaccine uptake by the populations, collectively executed by subnational government agencies to local communities within smaller areal-level or spatial units (e.g., districts or subdistricts), as vaccine uptake by local communities could be hindered by multiple factors such as misinformation, cultural, health literacy, or socio-economic factors (Klee et al., 2023). While our work contributed to the former, we recommend future work to understand the latter, that is to visualize the patterns of “risk–benefit considerations” of vaccine uptake by local communities within small area estimations, as these would direct subnational governments to identify barriers to vaccinations via more granular insights within finer-scales of geographical units to execute appropriate local campaigns or boosts confidence on the benefits of vaccinations. Addressing these local level factors would be a catalyst to ensure the success of national level pandemic control in the country. Our call for these approaches is in line with the latest expert consensus on setting research priorities for global pandemic preparedness (Song et al., 2024).
Study strengths and limitations
This study had certain strengths and limitations. The ecological study design could be subjected to ecological fallacy. Although possible correlations between vaccination rates and pandemic indicators could be appreciated at the population aggregated level, caution should be placed on the interpretation of the findings as the results cannot be interpolated to an individual level, or neither causal links could be established. However, our findings were yielded based on the parameters of the whole (true) population and not a sampled population, complemented with inferential statistics with ecological region-based regression, strengthening that the interpretation would be generalisable to a countrywide level. In terms of data dependability, our analysis relied on official government data that was made publicly available with transparency. The accuracy of the data was established as it was reported based on official diagnosis by health workers and clinical notifications from all health facilities across Malaysia during the pandemic period. While the current study was unable to progress further to spatial simultaneous autoregressive (SAR) models in view of covariates exceeding the number of observations (i.e., five regions of spatial units), our recommendations to explore more covariates or potential confounding factors within smaller areas of estimation through spatial–temporal analysis in future work as recommended above would provide greater exploration and granular insights into “risk–benefit considerations” by the local communities of vaccine uptake speed and success rates. The lack of data availability and varying accessibility across different spatial scales (e.g., districts, or sub-districts) has limited the ability to conduct thorough analysis to understand the patterns of vaccinations and their critical pandemic indicators at a more local level. This limitation has resulted in the absence of certain attribute data (e.g., demographics, health, and census profiles) that could be utilized to explore potential mediators or interactions within our analytical strategies.
Conclusion
Critical population-level pandemic indicators showed substantial reductions in ICU admissions and case fatalities with increased vaccinations over time. However, infectiousness remained fluctuant with different correlation patterns, possibly influenced by the emergence of new variants, as well as factors such as the type of vaccines and their effectiveness, and the different levels of protective measures implemented across phases and environments. Our research illustrates that vaccinations have helped to suppress critical pandemic indicators. The extent to which these indicators were reduced varied depending on the specific phase of pandemic control. Therefore, it is crucial to balance vaccinations with ongoing mitigation strategies (e.g., masking, maintaining personal and environmental hygiene practices like hand washing) in areas of greater susceptibility among local communities, in a harmonized manner.
References
Adrian, D., Reischman, D., Anderson, K., Richardson, M., & Stephenson, P. (2020). Helping introductory statistics students find their way using maps. Journal of Statistics Education, 28(1), 56–74. https://doi.org/10.1080/10691898.2020.1721035
Anderson, R. M., & May, R. M. (1992). Infectious Diseases of Humans: Dynamics and Control (p. 768). Oxford, UK: Oxford Science Publications.
Aruffo, E., Yuan, P., Tan, Y., Gatov, E., Gournis, E., Collier, S., Ogden, N., Belair, J., & Zhu, H. (2022). Community structured model for vaccine strategies to control COVID19 spread: A mathematical study. PLoS ONE, 17(10), e0258648. https://doi.org/10.1371/journal.pone.0258648
Baker, M.G., Kvalsvig, A., Plank, M.J., Geoghegan, J.L., Wall, T., Tukuitonga, C., Summers, J., Bennett, J., Kerr, J., Turner, N., Roberts, S., Ward, K., Betty, B., Huang, Q.S., French, N., & Wilson, N. (2023). Continued mitigation needed to minimise the high health burden from COVID-19 in Aotearoa New Zealand. New Zealand Medical Journal, 136(1583), 67–91. https://journal.nzma.org.nz/journal-articles/continued-mitigation-needed-to-minimise-the-high-health-burden-from-covid-19-in-aotearoa-new-zealand
Chen, H., Cao, Y., Feng, L., Zhao, Q., & Torres, J. R. V. (2023). Understanding the spatial heterogeneity of COVID-19 vaccination uptake in England. BMC Public Health, 23(1), 895. https://doi.org/10.1186/s12889-023-15801-w
Chi, G., & Zhu, J. (2020). Models dealing with both spatial dependence and spatial heterogeneity. In Spatial Regression Models for the Social Sciences 2020; pp. 139–154. SAGE Publications, Inc., https://doi.org/10.4135/9781544302096
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, New York: Erlbaum.
Fonseca-Rodriguez, O., Gustafsson, P. E., San Sebastian, M., & Connolly, A. F. (2021). Spatial clustering and contextual factors associated with hospitalisation and deaths due to COVID-19 in Sweden: A geospatial nationwide ecological study. BMJ Global Health, 6(7), e006247. https://doi.org/10.1136/bmjgh-2021-006247
Ganasegeran, K., & Ch’ngLooi, A. S. H. I. (2021a). What is the estimated COVID-19 reproduction number and the proportion of the population that needs to be immunized to achieve herd immunity in Malaysia? A Mathematical Epidemiology Synthesis. COVID, 1(1), 13–19. https://doi.org/10.3390/covid1010003
Ganasegeran, K., Jamil, M. F. A., Ch’ngLooi, A. S. H. I., & Peariasamy, K. M. (2021b). Influence of population density for COVID-19 spread in Malaysia: An ecological study. International Journal of Environmental Research and Public Health, 18(18), 9866. https://doi.org/10.3390/ijerph18189866
Ganasegeran, K., Jamil, M. F. A., Appannan, M. R., Ch’ngLooi, A. S. H. I., & Peariasamy, K. M. (2022). Spatial dynamics and multiscale regression modelling of population level indicators for COVID-19 spread in Malaysia. International Journal of Environmental Research and Public Health, 19(4), 2082. https://doi.org/10.3390/ijerph19042082
Gebreab, S. Y. (2018). Statistical methods in spatial epidemiology. In I. Kawachi (Ed.), Neighborhoods and Health. New York: Oxford University Press.
Gogtay, N. J., & Thatte, U. M. (2017). Principles of correlation analysis. Journal of the Association of Physicians of India, 65, 78–81.
Klee, B., Diexer, S., Sarajan, M. H., Glaser, N., Binder, M., Frese, T., Girndt, M., Sedding, D., Hoell, J. I., Moor, I., Gekle, M., Mikolajczyk, R., & Gottschick, C. (2023). Regional differences in uptake of vaccination against COVID-19 and influenza in Germany: Results from the DigiHero Cohort. Vaccines (basel), 11(11), 1640. https://doi.org/10.3390/vaccines11111640
Kwok, K. O., Lai, F., Wei, W. I., Wong, S. Y. S., & Tang, J. W. T. (2020). Herd immunity - estimating the level required to halt the COVID-19 epidemics in affected countries. Journal of Infection, 80(6), e32–e33. https://doi.org/10.1016/j.jinf.2020.03.027
Li, Y., Nazaroff, W. W., Bahnfleth, W., Wargocki, P., & Zhang, Y. (2021). The COVID-19 pandemic is a global indoor air crisis that should lead to change: A message commemorating 30 years of Indoor Air. Indoor Air, 31(6), 1683–1686. https://doi.org/10.1111/ina.12928
Liu, Q., Qin, C., Liu, M., & Liu, J. (2021). Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: A systematic review and meta-analysis. Infectious Diseases of Poverty, 10, 132. https://doi.org/10.1186/s40249-021-00915-3
Milton, P., Coupland, H., Giorgi, E., & Bhatt, S. (2019). Spatial analysis made easy with linear regression and kernels. Epidemics, 29, 100362. https://doi.org/10.1016/j.epidem.2019.100362
Ministry of Health Malaysia. (2022a). COVIDNOW. https://data.moh.gov.my/covidnow-data. Accessed 30 December 2022
Ministry of Health Malaysia. (2022b). Open data on COVID-19 in Malaysia. https://github.com/MoH-Malaysia/covid19-public. Accessed 30 December 2022
Mollalo, A., Mohammadi, A., Mavaddati, S., & Kiani, B. (2021). Spatial analysis of COVID-19 vaccination: A scoping review. International Journal of Environmental Research and Public Health, 18(22), 12024. https://doi.org/10.3390/ijerph182212024
National Security Council. (2022). Standard Operating Procedures National Recovery Plan. https://www.mkn.gov.my Accessed 30 December 2022.
Ng, D. C., Tan, K. K., Chin, L., Cheng, X. L., Vijayakulasingam, T., Liew, D. W. X., Abidin, N. Z. Z., Lee, M. L., Ganasegeran, K., & Khoo, E. J. (2022). Risk factors associated with household transmission of SARS-CoV-2 in Negeri Sembilan, Malaysia. Journal of Paediatrics and Child Health, 58(5), 769–773. https://doi.org/10.1111/jpc.15821
Odunsi, O. M., Salisu, U. O., Taiwo, A. O., Odufuwa, B. O., Badiora, A. I., Onanuga, M. Y., Fasina, S. O., Dada, O. T., Ogunseye, N. O., Momodu, S. O., Adebara, T. M., Adeleke, O. R., & Oresanwo, G. A. (2023). Geo-visualisation of COVID-19 pandemic and vaccination in Nigeria: A regional approach. Journal of Geovisualization and Spatial Analysis, 7, 29. https://doi.org/10.1007/s41651-023-00159-9
OECD (2021). The territorial impact of COVID-19: Managing the crisis and recovery across levels of government, OECD Publishing. https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-and-recovery-across-levels-of-government-a2c6abaf/. Accessed 5 Mar 2024.
Polack, F. P., Thomas, S. J., Kitchin, N., Absalon, J., Gurtman, A., Lockhart, S., Perez, J. L., Marc, G. P., Moreira, E. D., Zerbini, C., Bailey, R., Swanson, K. A., Roychoudhury, S., Koury, K., Li, P., Kalina, W. V., Cooper, D., Frenck, R. W., Jr., Hammitt, L. L., et al. (2020). Safety and efficacy of the BNT162b2 MRNA Covid-19 vaccine. New England Journal of Medicine, 383, 2603–2615. https://doi.org/10.1056/NEJMoa2034577
Rahman, M. S., Harun, M. G. D., Sumon, S. A., Mohona, T. M., Abdullah, S. A. H. M., Khan, M. N. H., Gazi, M. I., Islam, M. S., & Anwar, M. M. U. (2022). Hospitalization and mortality by vaccination status among COVID-19 patients aged ≥ 25 years in Bangladesh: Results from a multi-center cross-sectional study. Vaccines, 10(12), 1987. https://doi.org/10.3390/vaccines10121987
Schober, P., Boer, C., & Schwarte, L. A. (2018). Correlation coefficients: appropriate use and interpretation. Anesthesia & Analgesia, 126, 1763–1768. https://doi.org/10.1213/ANE.0000000000002864
Shaito, M., Elmasri, R., & Levine, D. (2022). Comparison of map visualization techniques used for spatial and spatio-temporal data: an analytical survey applied to COVID-19 data. Medical Research Archives, 10(9). https://doi.org/10.18103/mra.v10i9.3072
Shen, J., Kong, M., Dong, B., Birnkrant, M. J., & Zhang, J. (2021). Airborne transmission of SARS-CoV-2 in indoor environments: A comprehensive review. Science and Technology for the Built Environment, 27(10), 1331–1367. https://doi.org/10.1080/23744731.2021.1977693
Sikora, D., & Rzymski, P. (2022). COVID-19 vaccination and rates of infections, hospitalizations, ICU admissions, and deaths in the European economic area during Autumn 2021 wave of SARS-CoV-2. Vaccines, 10(3), 437. https://doi.org/10.3390/vaccines10030437
Song, P., Adeloye, D., Acharya, Y., Bojude, D. A., Ali, S., Alibudbud, R., Bastien, S., Becerra-Posada, F., Berecki, M., Bodomo, A., Borrescio-Higa, F., Buchtova, M., Campbell, H., Chan, K. Y., Cheema, S., Chopra, M., Cipta, D. A., Castro, L. D., Ganasegeran, K., … International Society of Global Health (ISoGH). (2024). Setting research priorities for global pandemic preparedness: An international consensus and comparison with ChatGPT’s output. Journal of Global Health, 14, 04054. https://doi.org/10.7189/jogh.14.04054
Suah, J. L., Tok, P. S. K., Ong, S. M., Husin, M., Tng, B. H., Sivasampu, S., Thevananthan, T., Appannan, M. R., Zin, F. M., Zin, S. M., Yahaya, H., Rusli, N., Ujang, M. F., Ibrahim, H. M., Abdullah, N. A., & Peariasamy, K. M. (2021). PICK-ing Malaysia’s epidemic apart: Effectiveness of a diverse COVID-19 vaccine portfolio. Vaccines, 9(12), 1381. https://doi.org/10.3390/vaccines9121381
Tevdovski, D., Jolakoski, P., & Stojkoski, V. (2022). The impact of state capacity on the cross-country variations in COVID-19 vaccination rates. International Journal of Health Economics and Management, 22(3), 237–255. https://doi.org/10.1007/s10754-021-09319-0
United Nations Office for Coordination of Humanitarian Affairs. Administrative shapefiles Malaysia. (2023). https://www.un.org/en/our-work/deliver-humanitarian-aid Accessed 30 June 2023.
Valeanu, L., Andrei, S., Morosanu, B., Longrois, D., Bubenek-Turconi, S. I., C-R Collaborative. (2023). The COVID-19 vaccination coverage in ICU patients with severe COVID-19 infection in a country with low vaccination coverage - a national retrospective analysis. Journal of Clinical Medicine, 12(5), 1749. https://doi.org/10.3390/jcm12051749
van Diepen, S., McAlister, F. A., Chu, L. M., Youngson, E., Kaul, P., & Kadri, S. S. (2023). Association between vaccination status and outcomes in patients admitted to the ICU with COVID-19. Critical Care Medicine, 51(9), 1201–1209. https://doi.org/10.1097/CCM.0000000000005928
Whittaker, R., Brathen Kristofferson, A., Valcarcel Salamanca, B., Seppala, E., Golestani, K., Kvale, R., Wattle, S. V., & Buanes, E. A. (2022). Length of hospital stay and risk of intensive care admission and in-hospital death among COVID-19 patients in Norway: A register-based cohort study comparing patients fully vaccinated with an mRNA vaccine to unvaccinated patients. Clinical Microbiology and Infection, 28(6), 871–878. https://doi.org/10.1016/j.cmi.2022.01.033
Zhang, J., Wang, Y., Wanta, W., Zheng, Q., & Wang, X. (2022). Reactions to geographic data visualization of infectious disease outbreaks: An experiment on the effectiveness of data presentation format and past occurrence information. Public Health, 202, 106–112. https://doi.org/10.1016/j.puhe.2021.11.011
Acknowledgements
We would like to thank the Director General of Health Malaysia for the permission to publish this article.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: KG, KMP; Data curation: KG, ASHC, IL, MFAJ, NR; Visualization: MFAJ, ASHC, IL, NR; Formal Analysis: KG, MFAJ; Investigation: KG, MFAJ, IL, KMP; Methodology: KG, MFAJ, ASHC, KMP; Resources: NR; Validation: NR, KMP; Writing original draft: KG; Writing-review and editing: ASHC, IL, KMP. All authors have read and agreed on the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Medical Research Ethics Committee (MREC), Ministry of Health Malaysia (NMRR ID-22–01915-SMB; 14 September 2022).
Competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Informed consent
Not applicable.
Conference presentation
Findings from this study were presented at the 16th National Conference for Clinical Research (NCCR) between 20–22 September 2023 at The Waterfront Hotel, Kuching, Sarawak, Malaysia.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ganasegeran, K., Jamil, M.F.A., Ch’ng, A.S.H. et al. COVID-19 pandemic indicators and variation with vaccinations in Malaysia: a regional-based geo-visualization and geo-ecological regression study. GeoJournal 89, 114 (2024). https://doi.org/10.1007/s10708-024-11111-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10708-024-11111-9