Abstract
Numerous pandemics have ravaged the world since prehistoric times. Some of the prevalent pandemics include the flu pandemic (1889–1890), Spanish flu (1918–1920), AIDS (1981–present) and the H1N1 swine flu pandemic (2009–2010). As pandemics occur, their incidence and prevalence rates are spatially heterogeneous, and the spatial distributions change over time. Understanding the national spatial distribution, temporal epidemic trends and transmission patterns of COVID-19 contributes to providing timely information for the national response to the pandemic. This chapter examines the Zimbabwean COVID-19 pandemic spatial patterns and temporal trends to enable decision-makers to prioritise vulnerable regions and plan appropriately as informed by the temporal patterns. A quantitative research design was adopted, which involved statistical computations and mapping of COVID-19 variable data obtained from web-based repositories. Results indicate spatial variability in the proliferation of COVID-19, with the most populated areas experiencing higher infection rates. There is a significant increase in the monthly new infections and new deaths, while the cumulative infection rates show some phases of steep increase. The case fatality rate has flattened. Policymakers and stakeholders must design strategies that respond to the spatial and temporal trends for optimal containment of the pandemic.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Since late 2019, the world has been grappling with the coronavirus disease of 2019 (COVID-19), which was first observed in Wuhan, China (Mohammed et al., 2021). Scientific inquiry has established that COVID-19 originates from a virus known as severe acute respiratory syndrome coronavirus 2 (SARs-CoV-2) (Forman et al., 2021). The symptoms of infection include fatigue, fever, dry cough, loss of smell, breathing difficulties, lung infection and diarrhoea (Huang et al., 2020; WMHC, 2020). The widespread transmission of COVID-19 led the World Health Organization (WHO) to recognise the disease as a pandemic on 11 March 2020, when it was reported in every continent worldwide (Guner et al., 2020; WHO, 2020). By the time of finalising this write-up, the pandemic had hit almost all countries worldwide with numerous negative impacts on the health system, economy and society. Zimbabwe has not been spared from the devastating impacts of the pandemic and reported its first case of COVID-19 on 20 March 2020.
As pandemics occur, their incidences and prevalence rates are spatially heterogeneous, and the spatial distributions change over time. Understanding the national spatial distribution, temporal epidemic trends and transmission patterns of COVID-19 contributes to providing timely information for the national response to the pandemic. There are considerable geographic dissimilarities in the occurrence and predominance of COVID-19 in Zimbabwe. As in many other countries, the spatial variation in the distribution of the disease has been attributed to a plethora of driving forces, including the physical environmental conditions, the nature of public health interventions, the area’s preparedness, the individuals’ underlying health conditions and the general access to health facilities. Fedele and Francesco (2021) argue that concerning the health conditions of individuals, the risk of contracting a respiratory disease increases if the individual has conditions such as chronic diseases, vitamin deficiency and obesity. The main transmission routes of the COVID-19 virus in humans are direct contact, aerosol and droplets (Yan et al., 2020; Lu & Shi, 2020; Aziz et al., 2020). Numerous scholars (Lu et al., 2020; Benvenuto et al., 2020; Chen, 2019) have, however, confirmed that COVID-19 infection is zoonotic, transmitted from animals to humans.
The movement of people plays a significant role in the spread of infectious diseases (Gayawan et al., 2020a). This applies to COVID-19 since SARS-CoV-2 spreads quickly between people. The factors that influenced SARS-CoV-2’s late transmission in Africa remain veiled in obscurity, but it may be relatively due to the limited mobility of the population across the international boundaries (Martinez-Alvarez et al., 2020). Most African countries reported the influence of international travel from Europe in their first COVID-19 cases (Adegboye et al., 2021). To confirm the influence of mobility on the spread of COVID-19, the first cases in Africa were observed in countries with highly internationally mobile populations, Egypt and Nigeria (Gayawan et al., 2020a, b). The disease’s initial spatial and temporal trends on the African continent indicated a slow spread until the cases increased abruptly in the last week of March 2020 (Gilbert et al., 2020).
In the early phases of the pandemic, there was concern among health experts about its proliferation in Africa due to its preparedness to deal with a pandemic of that magnitude (Gayawan et al., 2020a, b). The health systems in most African countries are underfunded, and consequently, their capacity to effectively deal with a vicious pandemic like COVID-19 is compromised. Early detection and control of diseases are shrouded in inefficiency due to poor infection surveillance and inadequate data transmission, among other factors (El-Sadr & Justman, 2020; Adekunle et al., 2020). Thus, the need for up-to-date spatial and temporal trend data and information about an infectious disease cannot be overemphasised, given its importance in enabling efficient combating of the spread of diseases.
Several statistical models have been applied to predict infection rates of COVID-19 (Gayawan et al., 2020a; Wang et al., 2020a). However, Adegboye et al. (2018) observed that mapping disease incidence, fatality rate and related deaths to identify geographic concentration and patterns is the sine qua non for comprehending the epidemiology of the disease and is a necessity for effective planning, containment and preventive action (Gayawan et al., 2020b). Spatial mapping of COVID-19 has been done by some studies (Gayawan et al., 2020a; Kang et al., 2020; Arab-Mazar et al., 2020). However, most of them focused on the spatial dimension without a focus on the temporal distribution. More so, in Zimbabwe, the spatial and temporal trends of COVID-19 have not been keenly taken into account to assess space-time dynamics to enhance the containment capacity. In view of this gap, this study explores the temporospatial trends of the disease between March 2020 and March 2022.
2 Materials and Methods
The study focuses on Zimbabwe, a developing country in Southern Africa which shares borders with South Africa (to the south), Zambia (to the northwest), Mozambique (to the northeast) and Botswana and the Caprivi Strip of Namibia (to the southwest) (Fig. 2.1). According to Worldometer (2022), Zimbabwe’s population is estimated at 15.2 million people, with a density of about 38 people per km2. As of 20 March 2022, there were 224,452 confirmed cumulative cases of COVID-19 and 5429 COVID-19-related deaths (Hannah et al., 2022). The country has 10 provinces and 61 administrative districts. The ten provinces (Fig. 2.1) are used as spatial units of analysis in this chapter. This is because the data on COVID-19 is unavailable on lower spatial scales of analysis, such as districts in the country.
This study examines the spatial and temporal trends of COVID-19 in Zimbabwe. It employs a quantitative research design coupled with document analysis to understand the factors behind the trends. The period considered in this study stretches from March 2020 to February 2022. Data on monthly infections, cumulative cases and deaths were obtained from interactive COVID-19 dashboards, including the Our World in Data platform managed by the University of Oxford, ZimStats dashboard and Zimbabwe’s Ministry of Health and Child Care website.
Both exploratory and confirmatory analysis approaches were used to determine statistical temporal trends of COVID-19 between March 2020 and February 2022. For spatial trends, statistical thematic maps were used, employing colour intensity to correspond with the aggregate summary of COVID-19 proliferation in the country’s provinces, which were used as the spatial enumeration units. The COVID-19 statistical data were first subjected to a Kolmogorov-Smirnov normality test before it was analysed to determine the significance of the trends using the Mann-Kendal (M-K) test in XLSTAT 2020. The M-K test detects monotonic trends in a data series (Chapungu & Nhamo, 2021) and has the dexterity to deal with values which are omitted and values under the detection boundary (Kocsis et al., 2020). Equations 2.1–2.3 show the procedure for computing the M-K test:
Where S is the Kendall score. Sgn (x) = {1 if x > 0, 0 if x = 0, −1 if x < 0} (Mann, 1945)
The variance of S is calculated from Eq. (2.2)” (Chapungu & Nhamo, 2021):
Where ɡ is the number of tied groups and tp is the number of observations in the pth group. After computing the variance, the Z value (ZMK) is computed in Eq. (2.3)” (Chapungu & Nhamo, 2021):
Tehran et al. (2021) propounded that a positive M-K statistic ZMK shows an affirmative change in the pattern of the variable, whereas a negative ZMK signposts a declining inclination. The values less than 0.05 show significant changes at 95% confidence level, while the values greater than 0.05 indicate no significant change.
As a data validation strategy, Zimbabwe’s national testing capacity was determined and compared with the WHO recommended standard. From the official report (as of 12 January 2022), the testing capacity in Zimbabwe was approximately 19,914 tests per week. If this is compared to the WHO standard, which recommends performing 1 test per 1000 populations per week, the test capacity in Zimbabwe is above the WHO standard.
3 Presentation of Results
3.1 Spatial Distribution of COVID-19 Cases
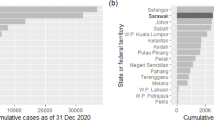
Results show that the burden of COVID-19 varies geographically across provinces. Figure 2.2 shows the spatial distribution of the cumulative cases of COVID-19 in the provinces of Zimbabwe.
As shown in Fig. 2.2, Harare has extremely high cases of COVID-19. As of 18 March 2022, the cumulative cases of COVID-19 in the province had gone above 95,000. This was followed by Manicaland Province, with a cumulative total between 55,000 and 60,000. Mashonaland East and Mashonaland West had cumulative cases between 45,000 and 55,000 by the time this study was conducted. Bulawayo had a moderate number of cumulative cases of COVID-19, around 42,000. Finally, there is a group of provinces with the lowest cumulative cases of COVID-19. The remaining provinces had below 40,000 cumulative cases, with Mashonaland Central being the least affected with less than 25,000 cases. Masvingo and Midlands provinces had cumulative cases slightly higher than that of Matabeleland South and Matabeleland North.
The high number of cumulative cases across the provinces was influenced by periodic waves of COVID-19 upsurge, which occurred four times between March 2020 and February 2022. Figure 2.3 shows the cases across provinces during the periodic upsurges commonly referred to as waves.
As shown in Fig. 2.3, the fourth wave contributed most of the confirmed cumulative cases across the provinces. During the fourth wave, Harare had more than 45,000, comprising nearly 50% of the total number of cases in the province as of 18 March 2022. This was followed by Mashonaland East and Mashonaland West, with close to 29,000 cases each during the December 2021–January 2022 fourth wave. These were closely followed by Manicaland Province, with above 25,000 cases during the same period. The other provinces experienced less than 20,000 cases during this period, with Mashonaland Central experiencing the least number of cases.
This study observes a pattern showing an increase in wave intensity with time. The first wave contributed about 11,000 cases in the most affected province. During the second wave, the number increased to around 13,000 in the most affected province. This was followed by another increase in the third wave to above 27,000 and, lastly, in the fourth wave, about 29,000.
3.2 Temporal Trend of COVID-19 in Zimbabwe
Dynamic change is an inherent feature of infections as they affect countries or parts of countries. COVID-19 in Zimbabwe has not been spared from such a general global trend. As alluded to earlier, there have been four waves during the occurrence of COVID-19 in Zimbabwe. Figure 2.4 shows the changes that have taken place in the spatial pattern of the cumulative cases of COVID-19 over time from the first wave to the fourth wave.
Changes in the magnitude of periodic upsurges in COVID-19 cases. (Source: Authors, data from ZimStats (2022))
Figure 2.4 shows that Harare province dominated the four waves concerning the number of COVID-19 cases. It is observed, however, that the epicentres of the hotspots of the disease have shifted during the four waves. During the first wave, cumulative cases were high in the provinces with the biggest cities in the country, namely, Harare, Bulawayo, Mutare and Gweru. During the second wave of the disease, the diffusion of the disease was significant in the expansion diffusion type, i.e. the spreading of the disease through a population in an area in such a way that the number of those influenced grows progressively larger (Walter, 2000). The southwestern and eastern parts of the country had higher cases of COVID-19 during the second wave, as shown in Fig. 2.4.
During the third and fourth waves, there was generally a shift in the centre of gravity of the pandemic towards the provinces of the country in the northern and eastern parts of the country except for Mashonaland Central Province, which remained with comparatively low numbers of cumulative cases of COVID-19 during all the four waves. On the other hand, Harare and Manicaland provinces had comparatively high numbers of COVID-19 cumulative cases throughout all four waves. Apart from the changes in the spatial patterns that occurred in the provinces during the different waves, Zimbabwe experienced a considerable increase in cumulative cases of COVID-19 since the beginning of the pandemic in the country, as shown in Fig. 2.5.
As indicated in Fig. 2.5, the gradient of the cumulative cases changes with time, with periods of waves having very steep gradients. The four waves can easily be identified, showing upsurges depicted by steep gradients. Periods of steep gradients (June–July 2020, December 2020–January 2021, July–August 2021 and December 2021–January 2022) were followed by phases of relative stability. As shown earlier, the steep gradients were mainly enhanced by highly populated areas characterised by highly mobile populations. While it is expected that the cumulative cases show a continuous increase in numbers, monthly cases have fluctuated throughout the pandemic, with some months having as low as 8 cases, while others had more than 7000. Figure 2.6 shows the monthly cases over the pandemic period.
Figure 2.6 shows a statistically significant (p = 0.000; α = 0.05) increase in the number of monthly COVID-19 new infections. A statistically significant increase implies that action must be taken to control the proliferation of the pandemic as more new people are conducting the virus every month. However, the fluctuations are mainly a function of periods of a huge upsurge of cases. As observed earlier, the wave or periods of case upsurge are becoming more intense with time, with some phases exceeding 45,000 cases in one geographic location only.
The statistically significant temporal trend of new infections is associated with an increasing trend in monthly new deaths. The Mann-Kendall trend tests reveal that the trend for monthly new deaths in Zimbabwe is increasing (p = 0.001; α = 0.05), as shown in Fig. 2.7.
The COVID-19-driven monthly death rate has been on the increase since the outbreak of the pandemic. As shown in Fig. 2.7, there is a significant increase in the number of people who die from COVID-19 per month with time. The increasing cases of infection mean more people are exposed, and the probability of fatalities increases. It appears that Zimbabwe’s health management system has managed to withstand the onslaught of COVID-19 with regard to the case fatality rate. Figure 2.8 shows the case fatality rate over the 2-year period.
The case fatality rate is considered a weak indicator in determining whether a health system is well managed or not, but it gives a general indication of whether the chances are high that an infected person will die from COVID-19. As shown in Fig. 2.8, at the beginning of the pandemic, the case fatality rate was very high but decreased with time until it reached a point where it was almost stable over time. This can be attributed to a cocktail of pharmaceutical and non-pharmaceutical interventions introduced due to increased knowledge about the pandemic.
4 Discussion
4.1 Spatial Pattern
The study has observed spatial variability in the prevalence of COVID-19 in Zimbabwe. The spatial variations evolve at the instigation of a plethora of factors. This confirms Gayawan et al. (2020a, b)’s observations that the proliferation of COVID-19 is spatially variable as determined by several variables. The provinces with high numbers of cumulative cases in the country are Harare, Bulawayo, Manicaland, Mashonaland West and Mashonaland East. One of the reasons to explain the comparatively higher cumulative cases of COVID-19 in those provinces is that they are located in areas harbouring large cities with high populations, making the transmission of SARS-CoV-2 easier than in areas that are sparsely populated. The virus is transmitted from infected persons through airborne transmission. Hence, the higher the population density, the more likely it is to efficiently transmit the virus (Wang et al., 2021). Besides population density, the characteristics of the population also determine the level of exposure to and transmissibility of the virus. Cities have a highly mobile and agile group of people who have greater chances of travelling to other countries where infections are high.
On the other hand, lower cumulative cases of COVID-19 in Masvingo, Matabeleland South and Matabeleland North can also be attributed to comparatively lower population numbers in the smaller urban areas in the provinces and lower population densities in the surrounding rural areas. The Midlands Province is an exception because cumulative cases are comparatively low despite the big city (Gweru) in that province. Previous studies by numerous scholars (Bhadra et al., 2021; Kadi & Khelfaoui, 2020; Alam, 2021; Wong & Li, 2020) support the positive relationship between high population density and high cumulative cases of COVID-19. The potential spreading risk of communicable disease is high when the population size and population density are large. Higher population density leads to more significant reports of COVID-19 diffusion.
In line with the distance decay law, the diffusion process of disease is associated with geographic interaction (Chen, 2019; Banks, 2014). Distance decay propounds that the further a place is from a source, the less it is affected by a disease, and the inverse is true. Mashonaland West Province is near Harare Province and has a more significant linkage with that province. The province (Mashonaland West) had high cumulative cases of COVID-19, which can be attributed to the strong linkage and proximity of the province with Harare Province. Mashonaland West Province also has a suitably developed transport network linking it with Harare Province and has a highway linking Zimbabwe with Zambia. Coelho et al. (2020) and Zhong et al. (2020) noted that various ways of transference provide an indispensable way for the diffusion of the virus. Transport routes in Mashonaland West, thus, serve as diffusion channels of COVID-19.
Meteorological factors also affect the spatial pattern of the cumulative cases of COVID-19 in Zimbabwe. Some provinces such as Harare, Bulawayo, Manicaland and parts of Mashonaland West and Mashonaland East experience lower temperatures and higher precipitation in the country. On the other hand, lower cumulative cases of COVID-19 in Masvingo, Matabeleland South and Matabeleland North can also be attributed to a comparatively higher temperature and lower precipitation. Evidence of the impact of meteorological factors such as precipitation and lower temperatures leading to higher incidence and prevalence rates of COVID-19 has been given by previous scholars (Oliveiros et al., 2020; Shahzad et al., 2021; Wang et al., 2020a, b; Sajadi et al., 2020). Climate conditions are thus significant predictors of coronavirus as they are critical in transmitting infectious diseases. Low temperatures, high humidity and high precipitation tend to increase the diffusion of COVID-19. Therefore, this chapter argues that warmer and drier parts of Zimbabwe are expected to have lower cumulative cases of COVID-19. As Gramsone aptly stated, “Some scientists think that the high temperatures make life harder for the virus that causes COVID-19” (Gramsone, 2020: 17).
4.2 Temporal Trends of COVID-19
This study employed the Mann-Kendall trend test to ascertain the temporal trends in monthly COVID-19 cases, monthly COVID-19-induced deaths and case fatality rate. It has established a significant trend in the temporal trends of monthly new infections and the number of deaths. The likelihood of coming into contact with an uninfected individual is less than the possibility of coming into contact with an infected person, resulting in a decrease in the number of new cases. Initially, from 21 March 2020 to 01 August 2020, there were few cases of the disease. This can be described as the lag phase of the disease diffusion. This is possibly because the pathogens (coronavirus) are still familiarising with the new conditions (human body), or the stage might have overlapped with the incubation phase of the disease. There are also chances that due to a few people infected at the initial stages, the prospect of coming into contact with an exposed individual is shallow, resulting in a low number of new cases.
After 05 August 2020, there is the acceleration phase of the disease. There is an increase in the number of infected people interacting within specific spatial contexts, and disease diffusion occurs. There has been an explosion of COVID-19 cases. That exponential phase marks the period of a swift upsurge in COVID-19-infected people in Zimbabwe. Such an exponential trend is inevitable. Epidemics typically obey the law of exponential growth in their initial stages, particularly for infectious diseases (Zhu et al., 2021). Under such conditions, R0 > 1.0, where each existing infection causes more than one new infection, more people contract the disease and the interaction between infected and uninfected people increases. During the period, the prospect of coming into contact with an uninfected person increases, and the number of new cases increases. The curve is souring upwards as the disease diffusion wave has broken out of the source region and is spreading out rapidly across the spatial landscape of Zimbabwe.
5 Conclusion
This study has examined the spatial and temporal patterns of COVID-19 in Zimbabwe. COVID-19 has become a significant challenge to the health systems of countries worldwide. It is imperative that the spatial and temporal patterns of the disease be understood in Zimbabwe. Based on the analysis of the cumulative cases in the spatial and temporal patterns of COVID-19 in Zimbabwe, it emerged that the disease rapidly spread to all provinces of Zimbabwe. The highest cumulative cases were found in Harare Province of the country. Other provinces with high numbers of COVID-19 cases were Manicaland, Mashonaland West, Bulawayo and Mashonaland East provinces. The provinces are characterised by comparatively low temperatures, high rainfall and high population densities. All such conditions are conducive to the fast spreading of the pandemic. Meteorological factors, population sizes and density had a significant impact on the spatial pattern of COVID-19 in Zimbabwe. The spatial distribution of the disease was characterised by expansion diffusion outwards from the initial hotspot centres in the country.
On the other hand, comparatively low cumulative cases of COVID-19 were identified in the provinces in the southern and western parts of the country (Masvingo, Matabeleland South and Matabeleland), as well as Mashonaland Central in the northern part of the country had low cumulative cases of COVID-19. The provinces are generally hot and dry, which creates conditions which limit the spreading of COVID-19. The country has experienced four waves of COVID-19. During the four waves, the spatial patterns of the cumulative cases of COVID-19 were generally shifting northwards. During the waves, some provinces experienced increases in the COVID-19 cases, while others experienced some decline. Apart from such a trend, it also emerged from the study that the total cumulative cases of COVID-19 increased sharply from March 2020 to March 2022. Analyses of spatial and temporal distribution characteristics of COVID-19 indicated that Zimbabwe was changing with time and was unevenly geographically distributed.
References
Adegboye, O. A., Leung, D. H., & Wang, Y. G. (2018). Analysis of spatial data with a nested correlation structure. Journal of the Royal Statistical Society: Series C (Applied Statistics), 67(2), 329–354.
Adegboye, O. A., Adekunle, A. I., Pak, A., Gayawan, E., Leung, D. H., Rojas, D. P., Elfaki, F., McBryde, E. S., & Eisen, D. P. (2021). Change in outbreak epicentre and its impact on the importation risks of COVID-19 progression: A modelling study. Travel Medicine and Infectious Disease, 40, 101988.
Adekunle, A. I., Adegboye, O. A., Gayawan, E., & McBryde, E. S. (2020). Is Nigeria really on top of COVID-19? (Vol. 148, pp. 1–7). Message from effective reproduction number.
Alam, M. Z. (2021). Is population density a risk factor for communicable diseases like COVID-19? A case of Bangladesh. Asia Pacific Journal of Public Health, 1, 11–22.
Arab-Mazar, Z., Sah, R., Rabaan, A. A., Dhama, K., & Rodriguez-Morales, A. J. (2020). Mapping the incidence of the COVID-19 hotspot in Iran–Implications for Travellers. Travel Medicine and Infectious Disease, 34, 101630.
Aziz, P. Y., Hadi, J. M., Aram, M. S., Aziz, S. B., Rahman, H. S., & Ahmed, H. A. (2020). The strategy for controlling COVID-19 in Kurdistan Regional Government (KRG)/ Iraq: Identification, epidemiology, transmission, treatment, and recovery. International Journal Surgery, 25, 41–46.
Banks, R. B. (2014). Growth and diffusion phenomena: Mathematical frameworks and applications. Springer-Verlag.
Benvenuto, D., Giovanetti, M., Ciccozzi, A., Spoto, S., Angeletti, S., & Ciccozzi, M. (2020). The 2019-new coronavirus epidemic: Evidence for virus evolution. Journal of Medical Virology, 92(4), 455–459.
Bhadra, A., Mukherjee, A., & Sarkar, K. (2021). Impact of population density on COVID-19 infected and mortality rate in India. Modeling Earth Systems and Environment, 7, 623–629.
Chapungu, L., & Nhamo, G. (2021). Interfacing vector-borne disease dynamics with climate change: Implications for the attainment of SDGs in Masvingo City, Zimbabwe. Jàmbá: Journal of Disaster Risk Studies, 13(1), a1175. https://doi.org/10.4102/Jamba.v13i1.1175
Chen, Y. G. (2019). Fractal dimension analysis of urban morphology based on spatial correlation functions. In L. D’Acci (Ed.), Mathematics of urban morphology (pp. 21–53). Springer Nature Switzerland AG.
Coelho, M. T. P., Rodrigues, J. F. M., Medina, A. M., Scalco, P., Terribile, L. C., Vilela, B., Diniz-Filho, J. A. F., & Dobrovolski, R. (2020). Global expansion of COVID-19 pandemic is driven by population size and airport connections. PeerJ. Available on https://doi.org/10.7717/peerj.9708. Accessed on 12-01-2022.
El-Sadr, W. M., & Justman, J. (2020). Africa in the path of Covid-19. New England Journal of Medicine, 383(3), e11.
Fedele, D., & Francesco, A. (2021). Obesity, malnutrition, and trace element deficiency in the coronavirus disease (COVID-19) pandemic. Nutrition, 81, 111–116.
Forman, R., Atun, R., McKee, M., & Mossialos, E. (2021). ‘12 Lessons learned from the management of the coronavirus pandemic’. Health Policy, 124, 577–580. https://doi.org/10.1016/j.healthpol.2021.05.008. Accessed 27 December 2021.
Gayawan, E., Awe, O. O., Oseni, B. M., Uzochukwu, I. C., Adekunle, A., Samuel, G., Eisen, D. P., & Adegboye, O. A. (2020a). The spatio-temporal epidemic dynamics of COVID-19 outbreak in Africa. Epidemiology and Infection, 148, e212. https://doi.org/10.1017/S0950268820001983
Gayawan, E., Fasusi, O. D., & Bandyopadhyay, D. (2020b). Structured additive distributional zero augmented beta regression modeling of mortality in Nigeria. Spatial statistics, 35, 100415.
Gilbert, M., Pullano, G., Pinotti, F., Valdano, E., Poletto, C., Boëlle, P. Y., d’Ortenzio, E., Yazdanpanah, Y., Eholie, S. P., Altmann, M., & Gutierrez, B. (2020). Preparedness and vulnerability of African countries against importations of COVID-19: A modelling study. The Lancet, 395(10227), 871–877.
Gramsone, K. (2020). Meteorological and climatic factors and COVID-19. International Journal of Epidemiology, 10(2), 400–417.
Guner, R., Hasanoglu, I., & Aktas, F. (2020). COVID-19: Prevention and control measures in community. Turk Journal Medical Science, 50(3), 571–577.
Hannah R., Edouard M., Lucas R., Cameron A., Charlie G., Esteban O., Joe H., Bobbie M., Diana B. and Max R. (2022). Coronavirus Pandemic (COVID-19). Available at https://ourworldindata.org/coronavirus, Accessed on 10-01-2022
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., & Hu, Y. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 395, 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Kadi, N., & Khelfaoui, M. (2020). Population density, a factor in the spread of COVID-19 in Algeria: Statistic study. Bulletin of the National Research Centre, 44, 138.
Kang, D., Choi, H., Kim, J. H., & Choi, J. (2020). Spatial epidemic dynamics of the COVID-19 outbreak in China. International Journal of Infectious Diseases, 94, 96–102.
Kocsis, L., Usman, A., Jourdan, A.-L., Hassan, S. H., Jumat, N., Daud, D., Briguglio, A., Slik, F., Rinyu, L., Futo, I., (2020). The Bruneian record of “Borneo Amber”: A regional review of fossil tree resins in the Indo-Australian Archipelago. Earth-Science Reviews, 201(103005), 1–21. Available at https://doi.org/10.1016/j.earscirev.2019.103005. Accessed 30 December 2021
Lu, Q., & Shi, Y. (2020). Coronavirus disease (COVID-19) and neonate: What neonatologist need to know. Journal of Medical Virology, 92(6), 564–567.
Lu, H., Stratton, C. W., & Tang, Y. W. (2020). Outbreak of pneumonia of unknown etiology in Wuhan China: The mystery and the miracle. Journal of Medical Virology, 92(4), 401–420.
Martinez-Alvarez, M., Jarde, A., Usuf, E., Brotherton, H., Bittaye, M., Samateh, A. L., Antonio, M., Vives-Tomas, J., D’Alessandro, U., & Roca, A. (2020). COVID-19 pandemic in West Africa. The Lancet Global Health, 8(5), e631–e632.
Mann, H. B. (1945). Non-Parametric Test against Trend. Econometrica, 13, 245–259. Available at https://dx.doi.org/10.2307/1907187. Accessed 28 December 2021.
Mohammed, A., Sha’aban, A. I., Jatau, I., Yunusa, A. M., Isa, A. S., Wada, K., Obamiro, H., & Zainal, B. (2021). Assessment of COVID-19 information overload among the general public. Journal of Racial and Ethnic Health Disparities, 1–9, https://doi.org/10.1007/s40615-020-00942-0
Oliveiros, B., Caramelo, L., Ferreira, N. C., & Caramelo, F. (2020). Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. MedRxiv.
Sajadi, P., Habibzadeh, A., Vintzileos, S., Shokouhi, F., & Miralles-Wilhelm, A. (2020). Amoroso temperature and latitude analysis to predict potential spread and seasonality for COVID-19. Available at SSRN 3550308, Accessed 10 Jan 2022.
Shahzad, K., Farooq, T. H., Doğan, B., Zhong, H. L., & Shahzad, U. (2021). Does environmental quality and weather induce COVID-19: Case study of Istanbul Turkey. Environmental Forensics, 1–12.
Tehran, S., Khabiri, N., Moradi, H., Mosavat, M. S., & Khabiri, S. (2021). Evaluation of vitamin D levels in COVID-19 patients referred to Labafinejad hospital in Tehran and its relationship with disease severity and morality. Clin Nutr ESPEN, 42, 313.
Walter, S. D. (2000). Disease mapping: A historical perspective: Spatial epidemiology methods and applications. Oxford University Press.
Wang, H., Zhang, Y., Lu, S., & Wang, S. (2020a). Tracking and forecasting milepost moments of the epidemic in the early-outbreak: Framework and applications to the COVID-19. F1000Research, 9.
Wang, J., Tang, K., Feng, K., & Lv, W. (2020b). High temperature and high humidity reduce the transmission of COVID-19. Available at SSRN 3551767. Accessed 09 Jan 2022.
Wang, Y., Liu, Y., Struthers, J., & Lian, M. (2021). Spatiotemporal characteristics of the COVID-19 epidemic in the United States. Clinical Infectious Diseases, 72(4), 643–651. https://doi.org/10.1093/cid/ciaa934
Wong, D. W. S., & Li, Y. (2020). Spreading of COVID-19: Density matters. Public Library of Science ONE, 15, 200–212.
World Health Organisation (WHO). (2020). Coronavirus disease (COVID-19) Pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 27 December 2021.
Wuhan Municipal Health and Health Commission. (2020). Wuhan Municipal Health and Health Commission’ Briefing on current pneumonia epidemic situation in our city. Available on http://www.wuhan.gov.cn/front/web/showDetail/2019123108989. Accessed 02 Jan 2022.
Yan, Y., Chen, H., Chen, L., Cheng, B., Diao, P., & Dong, L. (2020). Consensus of Chinese experts on protection of skin and mucous membrane barrier for health-care workers fighting against coronavirus disease 2019. Dermatology Therapy Journal, 33(4), 133–140.
Zhong, P., Guo, S., & Chen, T. (2020). Correlation between travellers departing from Wuhan before the spring festival and subsequent spread of COVID-19 to all provinces in China. Journal of Travel Medicine, 27(3), 260–373.
Zhu, M., Kleepbua, J., Guan, Z., Chew, S. P., Tan, J. W., Shen, J., Latthitham, N., Hu, J., Law, J. X., & Li, L. (2021). Early spatiotemporal patterns and population characteristics of the COVID-19 pandemic in Southeast Asia. Healthcare, Available at https://doi.org/10.3390/healthcare9091220. Accessed 05 Jan 2022.
ZimStats. (2022). Monitoring COVID-19 impact on households. Zimbabwe Data Portal. https://zimbabwe.opendataforafrica.org/wadppcg/monitoring-covid-19-impact-on-households. Accessed 23 Feb 2022.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chazireni, E., Chapungu, L., Nhamo, G. (2023). The COVID-19 Pandemic in Zimbabwe: A Spatial and Temporal Perspective. In: Chapungu, L., Chikodzi, D., Dube, K. (eds) The COVID-19 - Health Systems Nexus. Global Perspectives on Health Geography. Springer, Cham. https://doi.org/10.1007/978-3-031-21602-2_2
Download citation
DOI: https://doi.org/10.1007/978-3-031-21602-2_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-21601-5
Online ISBN: 978-3-031-21602-2
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)