Type I collagen was obtained in gel-like form by enzymatic-acidic extraction from cattle tail tendons and was polymerized at room temperature in ammonia vapor to form a transparent film 60.47–64.9 μm thick with good adhesive properties of 11.6–12.4 kPa and tensile strength 559.5–600.5 kPa. The dependence of the film adhesive properties on its ability to stimulate regenerative processes in tissues was found. The collagen was characterized by X-ray photoelectron spectroscopy. The C 1s spectrum showed peaks for C–C/C–H, C–O–C/C–OH, O=C–N, and O=C–OH groups; the N 1s spectrum for C–NH2, O=C–N, and C–NH3+ groups.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The development of bandages and structures for replacement and regenerative medicine with therapeutic effects, self-restoration, adhesion, and the required medical properties is one of the most challenging and actively emerging fields [1]. However, the creation of systems with the required adhesion under wet conditions and adequate bioavailability of drugs is still an unsolved problem [2]. Type I collagen is the most common protein of the extracellular matrix in the human body. It is broadly used as a base or biochemical ligand for maintaining cellular adhesion in tissue-engineering structures and hybrid materials for therapy of organ defects [3]. Collagen is nontoxic, nonpyrogenic, and biocompatible with all types of tissues and cells within a species and between species because of the absence of histocompatibility proteins. Collagen stimulates cell migration, growth, and proliferation and can interact with biologically active organic and inorganic components, which allows the construction of polyfunctional hybrid materials based on it [4]. Collagen is used in model systems and in therapy of neurodegenerative diseases [5]; spinal cord injuries [6]; bone [7] and skin [8] regeneration; eye [9], tendon [10], and cartilage pathologies [11]; and spine defects [12].
The best substrates for producing collagen are mammal skin, ligaments, and tendons, including waste of the meat industry [13]. Currently, efforts are aimed at improving collagen isolation methods and stages [14]. For example, a method for alkaline-salt extraction of collagen led to deamination of asparagine and glutamine residues, resulting in disruption of the charge distribution along the collagen molecule and the inability to form fibrils and gels [14]. A method of acidic extraction allowed the separation of collagen that retained the ability for gelation and polymerization to form films [15]. Research is examining the choice of suitable substrates for isolating collagen produced from mammal skins and tendons, fish industry waste, and marine mollusks [16] with the use of gene-engineering methods [17] and human placentas [18].
The present article demonstrated the effectiveness of using enzymatic acidic extraction of type I collagen from cattle tendons to create new film materials based on it. A conclusion about the direct dependence of the adhesive properties of wound dressings and their ability to stimulate tissue regeneration could be drawn from an analysis of the structure, morphology, and composition of surface film and gel forms of collagen and a comparison of data on the regenerative activity of the obtained coatings with previous research results [15, 19].
The research was directed at producing type I collagen. The work removed tendons (58.27 g) from cattle tails (1250 g). Collagen gel (3377 mL) was prepared by the isolation and purification of the collagen and afforded 28.8 g of powdered product after lyophilization. The collagen yield from the tendons was 49.6 and 2.24% of the tendon and tail mass, respectively. Repeated hydrolysis of tendon fragments remaining after the primary hydrolysis produced an additional 675.4 mL of collagen gel or 5.7 g of lyophilized protein. The total collagen yields from the tails and tendons were 2.76 and 69.6%, respectively. The use of cattle skin, bone, and cartilage besides tendons as substrate could significantly increase the product yields. For example, the collagen yields previously ranged from 12.5 to 18.0% of the total byproduct mass [13]. However, the obtained product was not monotypic because the used substrates contained other types of collagen (II–VI, IX, and XI) besides type I collagen, which prevented the product from being used for several biomedical purposes. Such collagen was undesirable for use in replacement therapy of bone and skin, where the protein base is type I collagen [20].
Collagen gel was dialyzed, after which it was used to produce films and lyophilized products. The resulting collagen forms were studied by literature methods [21].
Thermogravimetric analysis (TGA) of lyophilized collagen showed that mass loss by collagen in air occurred in several stages. Moisture adsorbed from air was removed in the heating interval up to 100°C. The most rapid collagen destruction process occurred in the range 250–400°C. Increasing the temperature further continued mass loss at a much slower rate up to 700°C. The thermal destruction parameters of the collagen were comparable to those reported previously [22].
Figure 1 shows X-ray phase analysis (XPA) data of lyophilized collagen. The diffraction pattern had a small peak near 2θ ≈ 8° and a broad peak with a maximum at 2θ ≈ 20°. The lack of strong reflections in the diffraction pattern of the collagen characterized its X-ray amorphous nature [23].
Small angle X-ray scattering (SAXS) found that the intensity of the small angle scattering I(s) at the smallest angles increased insignificantly for dialyzed collagen. This indicated that it had a more homogeneous structure. The intensity I(s) in this range increased considerably for collagen before dialysis and characterized it as a polydisperse polymer. The results allowed the size distribution of the heterogeneities in these samples to be determined, despite the very weak scattering from the collagen gels before and after dialysis.
An analysis of the volume distribution functions (Fig. 2) showed that dialyzed gel became significantly more homogeneous. It lacked heterogeneities with sizes of the order of 20–50 nm, which were observed in the collagen before dialysis. The nature of these heterogeneities could be due to compactions and voids or air bubbles in the gels.
Surface analysis of the collagen was very important for understanding the composition and structure of this promising medical material. Lyophilized collagen was studied by X-ray photoelectron spectroscopy. The elemental composition of the collagen surface was determined from a survey spectrum as 52% C, 15% O, and 32% N (in at. %).
The C 1s spectrum (Fig. 3a) of the collagen could be described by four states at 285.0, 286.3, 288.0, and 289.1 eV with equivalent Gaussian widths of 1.65 that were assigned to C–C/C–H, C–O−C/C–OH, O=C–N, and O=C–OH groups and relative intensities of 0.58, 0.24, 0.14, and 0.04, respectively. The N 1s spectrum (Fig. 3b) represented three states at 399.3, 400.1, and 401.3 eV with equivalent Gaussian widths of 1.46 that could be assigned to C–NH2, O=C–N, and C–NH3+ groups with relative peak intensities of 0.21, 0.69, and 0.10, respectively. The O 1s spectrum (Fig. 3c) could be described by three states with binding energies of 531.6, 532.7, and 533.8 eV and equivalent Gaussian widths of 1.99. The states were assigned to O=C–N, O=C–O, and C–O–C with relative peak intensities of 0.68, 0.22, and 0.10, respectively [24].
Table 1 presents characteristics of photoelectron spectra of the collagen.
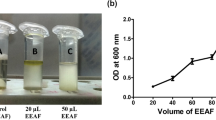
Film wound dressings are most convenient for therapy of skin defects. Gelatinous collagen was treated with medical glycerin (1%) and poured (40 mL) into sterile Petri dishes of diameter 90 mm to produce films with good organoleptic properties. Open Petri dishes with collagen were stored in ammonia vapor for 20–25 min to polymerize the gel. The adhesion force, thickness, and tensile strength of the resulting films were measured. The studies were performed in comparison with a commercial preparation based on NeuSkin-F collagen [Eucare Pharmaceuticals (P) Ltd., India]. Table 2 lists the thicknesses, adhesion forces, and tensile strengths of the collagen films.
Table 2 shows the commercial preparation NeuSkin-F was almost twice the thickness (P ≤ 0.001) and stronger than the produced films. However, the adhesion force was 1.85 times less (P ≤ 0.002). This was the most important parameter for wound dressings. The adhesion forces for the obtained films were 11.6–12.4 kPa, which significantly exceeded the parameters for similar commercial materials such as GelMA60-DA nanofiber hydrogels containing dopamine (DA) and methacryloyl gelatin (GelMA), which showed an adhesion force of ~9.1 kPa [25]. An adhesion force of 7.86 ± 1.22 kPa was recorded for PNIPAM hydrogel bandage based on N-isopropylacrylamide/alginate sodium/graphene oxide with double cross linking by chitosan solution [26]. The adhesive properties of the wound dressing were apparently due to the presence of chitosan. This was demonstrated before [27], where a hemostatic biohydrogel based on chitosan possessed high self-adhesion (68.5 kPa) under wet conditions and a simultaneously high degree of hemostasis. Collagen is the most biomimetic material for human and mammal bodies, despite the good adhesive properties of chitosan and the physicochemical properties of other polymers. This stimulates research on collagen and development of medical materials based on it. A direct dependence of the adhesion force on the amount of collagen in tissue engineering structures [28] and an increase in the adhesive properties of collagen upon introducing catechin groups into the composition [29] were found.
Apparently, the low adhesive properties were responsible for the negative result of using the NeuSkin-F commercial product as the reference preparation in in vivo experiments on purulent [30] and full-thickness skin wounds [31]. The preparation was shown to stimulate weakly regenerative processes in tissues. It was rather difficultly attached to experimental defects [15, 19].
The present study showed that enzymatic acidic extraction was effective for isolating type I collagen. New film materials with good adhesive properties were prepared from it. Results of thermogravimetric and XPA found that this product had thermal stability comparable to that of analogous materials and had an X-ray amorphous structure. SAXS allowed the homogeneity of the components forming the gelatinous systems to be studied. The collagen gel had a more homogeneous structure after dialysis than before it, which may have helped to form more homogeneous films. Surface analysis of the obtained material by XPS showed that production of the collagen did not lead to its destruction products or contaminants. Polymerization of the obtained collagen at room temperature in ammonia vapor gave a thin transparent film with good adhesive properties. Film wound dressings with strong adhesion were complementary to the wound shape and tightly adhered to it, adopting its configuration, which had a positive effect on tissue regeneration. Because of these qualities, the obtained collagen films showed a better regenerative effect than NeuSkin-F in in vivo experiments [15, 19].
The results demonstrated that the obtained material based on collagen was promising for use in biomedical purposes.
Experimental
General Comments. The following equipment and consumables were used to isolate the collagen and evaluate its properties: A Prodion 10BC-MA water purification system (China), a TDZ4-4WS tabletop centrifuge (Hunan Xiangyi Laboratory Instrument Development Co., Ltd. Huna, China), a laboratory sublimation dryer (Biobase BK-FD12PT –60/–80), a laminar box and cabinet (BBS8V1708247D, China), a MOM apparatus (Hungary), a D8 Advance diffractometer (Bruker AXS), a Thermo Fisher Scientific Theta Probe device, an AMUR-K diffractometer (developed at A. V. Shubnikov Inst. Crystallogr., RAS, Moscow), crystalline trypsin (Samson-Med, Russia), glycerin (Radiks, NPP, Uzbekistan), and chemical reagents produced in CIS countries.
Isolation and Purification of Collagen from Cattle Tendons. Tendons from cattle tails were purified of muscle, ligaments, and skin; ground to particle size 1–2 mm; treated with trypsin solution (0.25%) at 37°C for 72 h; rinsed in distilled H2O to remove proteins other than collagen; and hydrolyzed for 72 h in AcOH solution (0.1 N) in a 1:100 ratio. The mixture was centrifuged for 10 min at 3,000 rpm. The precipitate of collagens was filtered through a laboratory sieve with pore size 2 mm to separate large pieces that were sent for repeated hydrolysis. The collagen solution was dialyzed in dialysis bags with pore sizes 12–14 kDa (Spectrum Labs, USA) against distilled H2O at 5°C for 12 h with four exchanges of H2O. Films were prepared by treating gelatinous collagen with glycerin (1%) and pouring (40 mL) into sterile Petri dishes of diameter 90 mm. Open Petri dishes with collagen were stored in ammonia vapor for 20–25 min for complete polymerization.
Physicochemical Studies of Collagen Film Form. The collagen polymerization conditions, adhesion force, and thickness and strength of the obtained films were studied. The film thickness was determined using a micrometer at various places on the films (n = 6). Film tensile strength was determined by cutting a strip 5 mm wide and 50 mm long from the film. The ends of the film were clamped and stretched until breaking using a dynamometer (Fizpribor Plant, Kirov, Russia). The adhesion strength of the film was determined by cutting a sample 1 cm2 in area, gluing one side of the film using cyanoacrylic glue to tissues of equal area with an attached silk thread, moistening the films with water, and gluing to wet glass. The force necessary to cleave the film from the glass surface was determined using a dynamometer.
References
S. Guo, Y. Ren, R. Chang, Y. He, D. Zhang, F. Guan, and M. Yao, ACS Appl. Mater. Interfaces, 14, 34455 (2022).
S. Hu, X. Pei, L. Duan, Z. Zhu, Y. Liu, J. Chen, T. Chen, P. Ji, Q. Wan, and J. Wang, Nat. Commun., 12, 1689 (2021).
A. E. Stanton, X. Tong, and F. Yang, APL Bioeng., 3, 036108 (2019).
N. Tseomashko, M. Rai, and A. Vasil′kov, in: Biopolymer-Based Nano Films. Applications in Food Packaging and Wound Healing, M. Rai and C. Alves dos Santos (eds.), Elsevier, Cambridge, UK, 2021, pp. 203–246.
B. M. Saleh, A. Pourmostafa, N. Y. Patrawalla, and V. Kishore, J. Funct. Biomater., 14, 256 (2023).
S. Zhang, Q. Li, and S. Zhang, Regen. Ther., 24, 85 (2023).
M. E. Doyle, K. Dalgarno, E. Masoero, and A. M. Ferreira, Biopolymers, 114, e23527 (2023).
M. McGrath, K. Zimkowska, K. J. Genoud, J. Maughan, J. G. Gonzalez, Sh. Browne, and F. J. O′Brien, ACS Appl. Mater. Interfaces, 15, 17444 (2023).
Zh. Chen, X. Liu, J. You, E. Tomaskovic-Crook, Zh. Yue, A. Talaei, G. Sutton, J. Crook, and G. Wallace, J. Biomed. Mater. Res. Part A, 111, 1151 (2023).
M. Sun, H. Li, Y. Hou, N. Huang, X. Xia, H. Zhu, Q. Xu, Y. Lin, and L. Xu, Sci. Adv., 9, eade6973 (2023).
A. Baawad, D. Jacho, T. Hamil, E. Yildirim-Ayan, and D.-S. Kim, Tissue Eng., Part B, 29, 123 (2023).
M. Sharabi, Sh. Wertheimer, K. R. Wade, F. Galbusera, D. Benayahu, H.-J. Wilke, and R. Haj-Ali, J. Mech. Behav. Biomed. Mater., 94, 298 (2019).
A. R. Vidal, L. P. Duarte, M. M. Schmidt, R. L. Cansian, I. A. Fernandes, M. R. de Oliveira, I. M. Demiate, and R. C. P. Dornelles, Waste Manage., 102, 838 (2020).
L. V. Kukhareva, I. I. Shamolina, and E. V. Polevaya, J. Cytol., 52, 597 (2010).
N. E. Tseomashko, A. D. Abidova, D. A. Kadyrova, S. D. Makhmudov, S. F. Aripova, Kh. T. Zairova, and Kh. M. Kamilov, RUz Pat. No. IAP 06668, 2018, pp. 1–13.
S. Lukomski and D. H. McNitt, Methods Mol. Biol., 2136, 163 (2020).
T. Kalic, S. D. Kamath, T. Ruethers, A. C. Taki, R. Nugraha, T. T. K. Le, P. Humeniuk, N. A. Williamson, D. Hira, J. M. Rolland, R. E. O′Hehir, D. Dai, D. E. Campbell, H. Breiteneder, and A. L. Lopata, J. Allergy Clin. Immunol.: Pract., 8, 3084 (2020).
A. P. N. N. Alves, E. M. Lima Junior, N. S. Piccolo, M. J. Borges de Miranda, M. E. Q. L. Verde, A. E. C. Ferreira Junior, P. G. de Barros Silva, V. P. Feitosa, T. J. P. G. de Bandeira, M. B. Mathor, and M. O. de Moraes, Cell Tissue Bank., 19, 373 (2018).
S. D. Makhmudov, N. N. Abrekova, A. D. Abidova, N. E. Tseomashko, Sh. M. Turaboev, N. S. Beknazarova, F. N. Atamuratov, O. R. Akhmedov, A. A. Mamadrakhimov, A. S. Turaev, and B. T. Sagdullaev, RUz Pat. No. IAP 06575, 2020, pp. 1–15.
S. Yao, Y. Xu, C. Shao, F. Nudelman, N. A. J. M. Sommerdijk, and R. Tang, Methods Mol. Biol., 1944, 39 (2019).
A. Vasil′kov, I. Butenko, A. Naumkin, A. Voronova, A. Golub, M. Buzin, E. Shtykova, V. Volkov, and V. Sadykova, Int. J. Mol. Sci., 24, 7667 (2023).
A. Cucos and P. Budrugeac, J. Therm. Anal. Calorim., 115, 2079 (2014).
T.-W. Sun, Y.-J. Zhu, and F. Chen, RSC Adv., 8, 26218 (2018).
G. Beamson, High Resolution XPS of Organic Polymers, The Scienta ESCA 300 Database, 1992.
Y. Liu, Q. Wang, X. Liu, P. Nakielski, F. Pierini, X. Li, J. Yu, and B. Ding, ACS Appl. Bio Mater., 5, 1047 (2022).
Y. Cao, L. Wang, X. Zhang, Y. Lu, Y. Wei, Z. Liang, Y. Hu, and D. Huang, Regener. Biomater., 10, rbad081 (2023).
F. Song, Y. Kong, C. Shao, Y. Cheng, J. Lu, Y. Tao, J. Du, and H. Wang, Acta Biomater., 136, 170 (2021).
C. Wang, X. Xie, X. Huang, Z. Liang, and C. Zhou, Colloids Surf., B, 132, 1 (2015).
Z. Yang, R. Huang, B. Zheng, W. Guo, C. Li, W. He, Y. Wei, Y. Du, H. Wang, D. Wu, and H. Wang, Adv. Sci., 8, 2003627 (2021).
A. K. Kar, A. Singh, N. Dhiman, M. P. Purohit, P. Jagdale, M. Kamthan, D. Singh, M. Kumar, D. Ghosh, and S. Patnaik, Int. J. Nanomed., 14, 9837 (2019).
S. G. Priya, A. Gupta, E. Jain, J. Sarkar, A. Damania, P. R. Jagdale, B. P. Chaudhari, K. C. Gupta, and A. Kumar, ACS Appl. Mater. Interfaces, 8, 15145 (2016).
Acknowledgment
The work was supported by the Ministry of Science and Higher Education of the Russian Federation in the framework of State Task No. 075-00277-24-00 using scientific equipment at the Center for Molecular Structure Studies, NIOEC, RAS.
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Khimiya Prirodnykh Soedinenii, No. 4, July–August, 2024, pp. 596–600.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tseomashko, N.E., Tretyakova, A.N. & Vasil′kov, A.Y. Preparation and Physicochemical Properties of Collagen for Wound Dressings. Chem Nat Compd 60, 688–692 (2024). https://doi.org/10.1007/s10600-024-04412-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10600-024-04412-5