Abstract
Recombinant human bone morphogenetic protein-2 (rhBMP-2) and basic fibroblast growth factor (bFGF) are the focus of research pertaining to the stimulation of bone formation. We ascertained the effects of different concentrations rhBMP-2 on proliferation and differentiation of bone marrow stromal cells (BMSCs) in vitro and on ectopic bone formation in rats. BMSCs were obtained from beagle dogs and cultured in medium containing different concentrations rhBMP-2 and bFGF (0, 25, 50, 100, or 200 ng/mL). In a separate experiment, BMSCs were treated with different ratios (1:1, 2:1, 4:1, or 8:1) of rhBMP to bFGF (in each case the concentration of rhBMP was 100 ng/mL and the bFGF concentrations 100, 50, 25, or 12.5 ng/mL). Proliferation and differentiation of BMSCs were quantified by assessing methyl thiazole tetrazolium (MTT) and alkaline phosphatase (ALP) over 6 consecutive days. Von Kossa staining was performed on day 6. For the in vivo tests, porous calcium phosphate cement (CPC) was seeded with BMSCs (5 × 104) in medium containing 100 ng/mL rhBMP-2, 50 ng/mL bFGF or combined 100 ng/mL rhBMP-2 and 50 ng/mL bFGF. These cells were then subcutaneously implanted in four sites in nude rats. Bone formation was detected by histology at weeks 4 and 12 and quantified using a KS400 computer based image analysis system. It was determined that combined rhBMP-2 and bFGF at a ratio of 2:1 (100:50 ng/mL) promoted significantly increased BMSC proliferation and differentiation of BMSCs compared to rhBMP-2 or bFGF alone (p < 0.05). CPC with combined 100 ng/mL rhBMP-2 and 50 ng/mL bFGF stimulated more bone formation than either 100 ng/mL rhBMP-2 or 100 ng/mL bFGF (p < 0.05). These results show that a combination of rhBMP-2 and bFGF effectively induces early BMSC proliferation and differentiation in vitro. When combined, rhBMP-2 and bFGF synergistically promote new bone formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been reported that bone morphogenetic protein (BMP) and basic fibroblast growth factor (bFGF) can induce bone formation in ectopic and orthotopic sites in vivo. 12–14,31,49 Growth factors are endogenous regulators of cells responsible for mineralized tissue formation that are being explored therapeutically for bone tissue engineering. Growth factors have been used clinically within scaffolding biomaterial carriers for bone repair.18,20 They have also been administered systemically in preclinical models to stimulate bone deposition throughout skeletal tissues.1,18,43
BMPs belong to the transforming growth factor superfamily and play an important role in osteogenesis and bone metabolism.29,30 Among these, BMP-2 has a very strong osteoinductive activity. Since recombinant human BMP-2 (rhBMP-2) became available, many animal studies have been performed examining the induction of bone formation following implantation of rhBMP-2 using various carriers.34,36,38,46,48
Fibroblast growth factor (FGF) was originally identified from extracts of the pituitary gland and brain, and has been demonstrated to stimulate the proliferation of fibroblasts.22 The activity was mainly attributed to two similar proteins, acidic and basic fibroblast growth factor (bFGF, also known as bFGF-2).10,21 The basic form has been extensively studied because of its stronger potency in comparison with the acidic form. To date, it has been established through in vitro studies that bFGF is a potent mitogen not only for fibroblasts, but also for other mesoderm-derived cells including osteoblasts and vascular endothelial cells.3,24,43,48 Most in vitro studies have reported that bFGF can influence differentiation of bone marrow stromal cells (BMSCs), and enhance chondrogenic and osteogenic differentiation of BMSCs. bFGF stimulates BMSCs to deposit new mineralized bone yet allows these cells to retain differentiation potential.41
BMP-2 and bFGF are growth factors that act as prototypical mitogen and morphogen, respectively.11 bFGF administered via the intravenous route has been shown to stimulate endocortical bone deposition. Angiogenic and mitogenic effects of bFGF have been demonstrated to exert beneficial effects at bone sites.17,33,45 Systemic administration of BMP-2 in an osteoporotic mouse model has been reported to increase femur trabecular bone volume.1 The combination of growth factors has been shown to result in synergistic effects that might further stimulate the complex cellular events and interactions that lead to new bone formation.2,9,23,28,32,43,47 However, it is not clear what concentrations and ratios of BMP to bFGF are optimal for improving bone formation both in vivo and in vitro.
The aims of this study were to determine the optimal concentrations and ratios of rhBMP-2 to bFGF and the effects of these combinations on bone formation in rats following ectopic administration of cultured beagle dog marrow stem cells loaded onto porous calcium phosphate cement (CPC). We chose to use CPC as the carrier in this study as it has been demonstrated to offer several advantages over other potential carriers. These include ease of shaping, and excellent bone biocompatibility, osteoconductivity and bioresorbability.16,27,42 CPC also has an amorphus structure which is comparable to the bone mineral phase.4
Materials and Methods
Preparation of rhBMP-2 and bFGF Solutions
Both rhBMP-2 and bFGF were purchased from PeproTech, Inc (London, UK). Freeze-dried rhBMP-2 was dissolved in phosphate buffered saline (PBS) containing BSA (50 μg of BSA per 1 μg of protein) to give a concentration of 2 μg/mL, while freeze-dried bFGF was dissolved in PBS containing 10 mM Tris (pH 8.5) to give a concentration of 2 μg/mL and stored at −20 °C.
Cytokine Carrier Preparation
CPC was purchased from Rebone Biomaterial Ltd Co (Shanghai, China). According to the supplier, CPC was manufactured by mixing the following: hydroxyapatite, tetracalcium phosphate, tricalcium phosphate, dicalcium phosphate dehydrate, and distilled water at room temperature.35 The cement had an average pore size of 400 μm and 70% porosity (see Fig. 1). CPC was used as a carrier (4 mm diameter × 2 mm thickness) for rhBMP-2 and bFGF (Fig. 1). The pieces were submerged in 10 mL of culture medium for 30 min before in vitro use.
Animal Protocol
A total of 12 male Nu/Balb-c nude rats (aged 5 weeks, weighing 100–200 g) were used. These T-lymphocyte deficient, athymic mice were used to avoid any potential cross-species incompatibility response to the beagle cells. Three beagle dogs (aged 1.5–2 years, weighing 15–20 kg) obtained from the animal holding centre of Ninth People’s Hospital, Shanghai Jiaotong University Medical College (Shanghai, China) were also used. All animal experimentation protocols were approved by the Institutional Animal Care and Use Committee of Ninth People’s Hospital, Shanghai Jiaotong University. The animals were handled according to the guidelines established for animal care at the center.
Preparation of BMSCs
The beagles were injected with 10 mg/kg ketamine. After routine sterilization, 2 mL of bone marrow was aspirated from the ilium as described previously.40 BMSCs were plated at a density of 5 × 104 cells per 10 mm diameter culture dish in 10 mL of Dulbecco’s Modified Eagle Medium (DMEM, Gibco) supplemented with 10% fetal calf serum (Hyclone), 2 mM l-glutamine (Sigma), 100 U/mL penicillin, 100 μg/mL streptomycin (complete mixture abbreviated to DMEM) at 37 °C in 95% relative humidity and 5% CO2.40 The medium was changed every 3 days. Cells were passaged when confluent, up to a maximum of two passages. The cells were washed with 10 mL of PBS and then detached by exposing to 0.25% trypsin (Sigma) 1 mM EDTA for 3 min at 37 °C, followed by tapping of the dishes and addition of 5 mL of culture medium. The cells were centrifuged then resuspended in medium and plated at a density of 5 × 105 cells/dish. The cell number per dish was 3 × 106 cells before starting the experiments. Remaining cells were stored at −70 °C until use.
Preparation of Composite for Experimental Groups
Osteogenic medium was basal medium (as already described) supplemented with 10−8 mol/L dexamethasone, 50 μg/mL ascorbic acid, and 2.16 g of ß-glycerolphosphate. Three series of experiments were conducted for the purposes of this study to determine the appropriate concentrations of BMP and FGF and the ratio of BMP to FGF for optimal proliferation and differentiation of BMSCs in vitro and ectopic bone formation.
In the first series of experiments, the effective concentrations of rhBMP-2 and bFGF were investigated. Cells were plated at a density of 5 × 104 cells/well and a volume of 0.1 mL in 96-well plates. The treatment groups were as follows: (1) 10 mL osteogenic medium; (2) 25 ng/mL rhBMP-2; (3) 50 ng/mL rhBMP-2; (4) 100 ng/mL rhBMP-2; (5) 200 ng/mL rhBMP-2; (6) 25 ng/mL bFGF; (7) 50 ng/mL bFGF; (8) 100 ng/mL bFGF; and (9) 200 ng/mL bFGF. Every day for 6 days after treatment, the cells were collected and methyl thiazole tetrazolium (MTT) and alkaline phosphatase (ALP) analysis was performed (details regarding these assays ensues).
In the second series of experiments the synergistic effect of rhBMP-2 and bFGF was investigated. The treatment groups were as follows: (1) 10 mL osteogenic medium; (2) 100 ng/mL rhBMP-2; (3) 100 ng/mL bFGF; (4) rhBMP-2 and bFGF (1:1, both 100 ng/mL); (5) rhBMP-2 and bFGF (2:1, rhBMP-2 = 100 ng/mL); (6) rhBMP-2 and bFGF (4:1, rhBMP-2 = 100 ng/mL); and (7) rhBMP-2 and bFGF (8:1, rhBMP-2 = 100 ng/mL). Treatment exposure was for 6 days, after which the cells were collected and MTT, ALP, and Von Kossa analysis were performed. All experiments were repeated in triplicate with three independent cell seedings.
In the third series of experiments, the effect of rhBMP-2 and bFGF loaded onto porous CPC on ectopic bone formation was assessed. The treatment groups were as follows: (1) CPC loaded BMSCs (6.0 × 105 cells/mL) with serum-free DMEM; (2) CPC loaded BMSCs (6.0 × 105 cells/mL) with 100 ng/mL rhBMP-2; (3) CPC loaded BMSCs (6.0 × 105 cells/mL) with 50 ng/mL bFGF; and (4) CPC loaded BMSCs (6.0 × 105 cells/mL) with 100 ng/mL rhBMP-2 and 50 ng/mL bFGF.
The initial dose ranges and ratios were chosen with reference to previous studies.18,48
Animal Surgical and Treatment Protocols
Rats were anesthetized with a 40 mg/kg body weight intraperitoneal injection of pentobarbital sodium. After routine sterilization, four 4 mm longitudinal skin incisions were made to expose the muscle. Four blocks of porous CPC (as already described) were placed subcutaneously into the right and left back (one in each site) of each rat (n = 6), and the skin was closed with 5-0 nylon suture. The rats were sacrificed at 4 and 12 weeks postoperatively. The specimens were excised, fixed in 10% buffered formalin and processed for hematoxylin/eosin histology.
BMSC Proliferation
BMSCs were plated at a density of 5 × 104 cells/well and a volume of 0.1 mL in 96-well plates. The cells were grown in basal medium (composition previously described) and were allowed to adhere for 24 h. Thereafter, serum-free DMEM culture medium, containing the various growth factors as described per the first series of experiments was added in 6 wells and the plates were incubated at 37 °C, 95% relative humidity and 5% CO2. The rates of proliferation were estimated by performing MTT analysis every day for 6 days. The MTT assay has been previously described and is based on the reduction of MTT by mitochondrial dehydrogenases of viable cells.33 The MTT reaction product, a blue formazan derivative, was measured photometrically at 490 nm. Ten microliters of MTT stock solution (5 g/L) were added to each well and incubated at 37 °C for 4 h. Dimethylsulphoxide was added to each well to solubilize the formazan crystals. Thereafter, microtiter plates were shaken for 5 min and the absorbance at 490 nm determine using a microtiter plate reader.
BMSCs Differentiation
The extent of cell differentiation was determined by semi-quantitatively assessing the increase in ALP enzymatic activity as previously described.1 In multiple 96-well culture plates, BMSCs were cultured as already described and ALP examined every day for 6 days. After washing the cells three times with PBS, a lysis buffer solution containing 0.1% Triton-100, 1 mmol/L MgCl2, 0.1 mmol/L ZnCl2, and 20 mmol/L Tris (pH 10) was added and the cells were frozen at −80 °C. For each assay, 100 μL of cell lysate was incubated with 1 mL of P-nitrophenol phosphate solution (10 mmol/L).1 All measurements were performed in triplicate and the activity of ALP was determined using a spectrophotometer.
ALP and Von Kossa Staining
ALP analysis and Von Kossa staining were used to verify the phenotype of cells. Staining for ALP was performed as previously described.21 The formation of osteoblast bone nodules in cells cultured in 6-well plates at an initial density of 105/well were determined. Experiments were terminated by fixing cell layers in 2% glutaraldehyde for 5 min. Cells were then stained with an alizarin red (1% solution in water) for 5 min, and rinsed with 50% ethanol to remove excess stain. Cells were then air dried and the bone nodules visualized.
Histological Examination
Following euthanasia, the specimens from the rats were fixed in 10% buffered formalin, decalcified, embedded in paraffin, cut into 5 μm-thick sections, stained with hematoxylin/eosin, and examined for bone tissue formation. Light microscopic analysis consisted of morphological assessment of the tissue response to the different implants. For histomorphometry, the following elements were identified: mineralized bone-like tissue, non-mineralized bone-like tissue (osteoid), fibrous tissue, scaffold material, and osteoblast-like cells. The percentage of tissue formed was calculated by dividing the surface area of each tissue type by the whole surface area assessed per field of vision. Five fields of vision were evaluated per section. The assessment of tissue types was performed at a magnification of 10×. The amount of newly formed bone was assessed using a Zeiss Axioplan 2 microscope (Oberkochen, Germany) and quantified using computer based KS400 image analysis (Wetzlar, Germany). The perimeter around the newly formed bone was traced, and the enclosed area was determined in mm2 using image analysis software. The percentages of newly formed bone within each specimen outline were then calculated.40
Statistical Analysis
The results pertaining to MTT and ALP are expressed as means ± standard deviation. Analysis of variance was performed to determine within and between group differences. Statistical analysis was performed using SPSS statistical software (version 15.0, SPSS Inc., Chicago, IL). Differences were considered to be statistically significant when p < 0.05.
Results
BMSCs Proliferation
Figure 2 shows that the proliferation of BMSCs was significantly different in the rhBMP-2 100 ng/mL, bFGF 100 ng/mL, rhBMP-2 and bFGF (1:1), rhBMP-2 and bFGF (4:1) and rhBMP-2 and bFGF (8:1) groups compared to the rhBMP-2 and bFGF (2:1) group. Moreover, compared to both the 100 ng/mL rhBMP-2 and 100 ng/mL bFGF alone groups at day 6, proliferation of BMSCs treated with both rhBMP-2 and bFGF (2:1) was significantly enhanced (p < 0.001 for both comparisons).
BMSCs Differentiation
Among the groups, ALP immunostaining was most pronounced in BMSCs treated with both rhBMP-2 and bFGF (Fig. 3). Compared to control group, the number of ALP-positive cells was significantly increased in the rhBMP-2 and bFGF (1:1), rhBMP-2 and bFGF (2:1), rhBMP-2 and bFGF (4:1) and rhBMP-2 and bFGF (8:1) groups (all p < 0.001). The number of ALP-positive cells was significantly different between both the rhBMP-2 and bFGF (1:1) and rhBMP-2 and bFGF (2:1) groups compared to the rhBMP-2 100 ng/mL group (p < 0.001 for both). Moreover, compared to the rhBMP-2 and bFGF (2:1) group, the number of ALP-positive cells was significantly decreased in the rhBMP-2 and bFGF (4:1) and rhBMP-2 and bFGF (8:1) groups (p < 0.05). In contrast, there was no difference between the rhBMP-2 and bFGF (1:1) and rhBMP-2 and bFGF (2:1) groups.
ALP and Von Kossa Staining
Strongly stained ALP-positive cells with prominent nodular formations were observed on day 6 in BMSCs treated with both rhBMP-2 and bFGF. BMSCs treated with rhBMP-2, and other combinations of rhBMP-2 and bFGF showed similar nodular formations; however those treated with bFGF alone did not exhibit mineralization in vitro (see Figs. 4 and 5).
Histological Examination
A histological examination of the specimens revealed that they were encapsulated in a fibrous capsule, and that there was trabecular bone as well as an amorphous calcified matrix in all the samples. The trabeculae included many osteocytes regularly lined with numerous osteoblasts. At the periphery of specimens, the bone had a laminar pattern similar to normal bone. There was no evidence of inflammation or foreign-body reaction in the host tissue adjacent to the new bone. There was bone formation in all treatment groups at 4 weeks. The CPC with BMSC group exhibited mainly immature cells, with the bone marrow beginning to appear at 4 weeks. There was basophilic mineralization throughout in all the BMSCs groups at 4 weeks. The BMSCs treated with both rhBMP-2 and bFGF exhibited the most advanced bone formation (both peripheral and central: Fig. 6), with some osteoblastic linings observed. At 12 weeks basophilic mineralization was apparent, along with immature endogenous mesenchymal cells, bone marrow, lamellar structure and a bone ridge pattern in the BMSC group, while there were osteocytes surrounded by osteoblasts or osteoclasts in the groups of cells treated with both rhBMP-2 and bFGF.
Histological comparison of the four groups at 12 weeks after implantation. New bone (arrow shows NB) formation was observed. In group CPC/BMSCs/rhBMP-2(H), more mature bone existed than in other groups. Hematoxylin and eosin staining was performed. (a, b) = CPC/BMSCs; (c, d) = CPC/BMSCs/rhBMP-2; (e, f) = CPC + BMSCs + bFGF; (g, h) = CPC + BMSCs + rhBMP-2 + bFGF. (a, c, e, g) = ×2 magnification; (b, d, f, h) = ×10 magnification
New bone formation was significantly higher in rats implanted with carrier containing BMSCs + rhBMP + bFGF at 12 weeks as compared to bone formation in all other groups (p < 0.001, Fig. 7).
Discussion
A variety of bone growth factors participate in the regulation of cell proliferation, differentiation and bone metabolism. New bone formation involves the recruitment of osteoprogenitor cells, with the rate of mature bone-formation being dependent on the commitment and replication of these cells, their differentiation into functional osteoblasts, and the lifespan of mature osteoblasts. Osteoblast differentiation and matrix mineralization are regulated by the actions of systemic and local signaling factors, such as BMP-2 and bFGF.15 Growth factors are differentially expressed during the temporal acquisition of bone-specific markers as osteoprogenitor cell maturation proceeds in vitro. BMP-2 and FGF-2 are late-response growth factors.14 This study investigated the responsiveness of BMSCs to rhBMP-2 and bFGF, two regulatory mediators of osteoinduction and osteogenesis.
BMP-2 is a member of the transforming growth factor-ß superfamily, and is a powerful inducer of osteoblast differentiation in vitro and bone formation in vivo.12,31,44 Dexamethasone/ascorbic acid/glycerolphosphate (DAG) and BMP-2 are potent agents of cell proliferation and differentiation. BMP-2 enhances DAG-induced osteogenic differentiation in mesenchymal bone marrow cells, and both agents have been demonstrated to interact and modify osteoblastic bone formation.15 bFGF has a strong proliferative effect on various cells involved in angiogenesis, which is a vital process for early bone formation and remodeling.5,25 A number of studies have shown that cells exposed to bFGF appear dystrophic and have low ALP activity or are incapable of osteoblast differentiation in vitro.6,21 In the present study we found that rhBMP-2 was a more potent stimulator of BMSC differentiation than bFGF, while the reverse was true for BMSC proliferation. These conclusions were drawn on the basis of ALP activity, which is a well-accepted marker of osteogenesis in BMSCs.7 bFGF is only an initiation factor for osteogenesis and cannot further promote the proliferation of differentiated osteoblasts, osteocytes and chondrocytes,43,44 while rhBMP-2 irreversibly induces undifferentiated BMSCs to form cartilage and bone forming cells.32,50,51
Disruption of the FGF-2 gene results in reduced bone mass in mice and impairs the expression of BMP-2, an important mediator of osteoblast and osteoclast differentiation.26 Endogenous FGF-2 is an important mediator of the BMP-2 response in bone; this may be dependent on the p42/44 MAPK signaling pathway and downstream modulation of Runx2.26 BMP-2 can compensate for any defect in the biological action of bFGF and vice versa. Co-administration of osteogenic rhBMP-2 and bFGF may result in enhanced proliferation and differentiation of BMSCs in vitro and heightened bone formation in vivo as cytokines presumably affect BMSCs via an independent signal transduction pathway in the bone development process.33 Co-treatment with BMP-2 and bFGF on dexamethasone-dependent osteogenic differentiation has been investigated using rat and rabbit BMSCs in vitro.17,25,32 Maegawa et al.22 reported that the differentiation of rat BMSCs was further enhanced by early supplementation of culture medium with FGF-2, followed by BMP-2. The supplementation resulted in prompt and extensive osteoblastic activity, together with abundant bone matrix formation. In the present study, rhBMP-2 and bFGF were added at the same time and were found to enhance proliferation and differentiation of BMSCs. We found that there were increased nodular formations associated with this combined treatment, particularly when the ratio of rhBMP-2 to bFGF was 2:1. BMP-2 may provide bFGF with numerous target cells after initiating osteogenesis, hence accelerating osteoinduction and osteogenesis. The reason for this may be as described by Singhatadgit et al.,37 namely that BMP receptor (BMPR) expression is differentially modulated by TGF-b1, FGF-2, and PDGF-AB. All three growth factors were found to enhance certain BMP-2-induced functional activities in human bone cells, for example, ALP activity, which was found to be mediated at least partly via the BMPR-IB.37
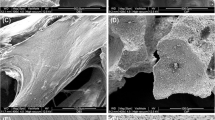
The delivery system releases and localizes the BMP/FGF, ensuring interaction with mesenchymal cells that can differentiate into osteoblasts. CPC has been found to have the capacity to induce rapid deposition of new bone at the cement surface interface in vivo, and is hence considered to be a good scaffold material candidate for bone engineering.4,8,27,39 Scanning electron microscopy of CPC with BMSCs demonstrated that cells were attached to the CPC surface 4 h after seeding. In this study we found that the rhBMP-2/bFGF implantation in rat subcutaneous tissue induced bone formation. The ectopic bone formed in the CPC containing BMP-2, bFGF, and BMP-2/bFGF groups was similar to normal bone. CPC with 100 ng/mL rhBMP-2 and 50 ng/mL bFGF stimulated more bone formation than did CPC with 100 ng/mL rhBMP-2 or 50 ng/mL bFGF both centrally and peripherally at weeks 4 and 12. FGF has been purported to play an important role during rhBMP-2-induced bone formation.19 In the present study, treatment with bFGF at an early stage increased the amount of rhBMP-2-induced mineralization. Generally, FGF family members stimulate cellular proliferation rather than cellular differentiation and exert an anabolic effect on bone formation when systemically or locally administered.21 Our results suggest that rhBMP-2 and bFGF are indispensable in regulating bone induction and formation. Furthermore, CPC can act as an effective delivery system for both BMSCs and BMP-2/bFGF.
In conclusion, we have found that rhBMP-2 and bFGF are effective inducer of BMSC proliferation and differentiation at an early stage in vitro and in vivo. Our findings emphasize the importance of bFGF in BMP-2-induced ectopic bone formation. The concentration ratio of 2:1 rhBMP-2/bFGF was found to be most effective in stimulating new bone formation. The combination of rhBMP-2 and bFGF was synergistic with regards to bone formation. Further studies should establish the suitability of combined rhBMP-2 and bFGF for treating bone defects.
References
Akita, S., M. Fukui, H. Nakagawa, T. Fujii, and K. Akino. Cranial bone defect healing is accelerated by mesenchymal stem cells induced by coadministration of bone morphogenetic protein-2 and basic fibroblast growth factor. Wound. Repair Regen. 12:252–259, 2004.
Alam, S., K. Ueki, K. Marukawa, T. Ohara, T. Hase, D. Takazakura, and K. Nakagawa. Expression of bone morphogenetic protein 2 and fibroblast growth factor 2 during bone regeneration using different implant materials as an onlay bone graft in rabbit mandibles. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 103:16–26, 2007.
Asplin, I. R., S. M. Wu, S. Mathew, G. Bhattacharjee, and S. V. Pizzo. Differential regulation of the fibroblast growth factor (FGF) family by alpha(2)-macroglobulin: evidence for selective modulation of FGF-2-induced angiogenesis. Blood 97:3450–3457, 2001.
Calafiori, A. R., M. G. Di, G. Martino, and M. Marotta. Preparation and characterization of calcium phosphate biomaterials. J. Mater. Sci. Mater. Med. 18:2331–2338, 2007.
Carmeliet, P., and R. K. Jain. Angiogenesis in cancer and other diseases. Nature 407:249–257, 2000.
Chaudhary, L. R., A. M. Hofmeister, and K. A. Hruska. Differential growth factor control of bone formation through osteoprogenitor differentiation. Bone 34:402–411, 2004.
Collin, P., J. R. Nefussi, A. Wetterwald, V. Nicolas, M. L. Boy-Lefevre, H. Fleisch, and N. Forest. Expression of collagen, osteocalcin, and bone alkaline phosphatase in a mineralizing rat osteoblastic cell culture. Calcif. Tissue Int. 50:175–183, 1992.
Fei, Z., Y. Hu, D. Wu, H. Wu, R. Lu, J. Bai, and H. Song. Preparation and property of a novel bone graft composite consisting of rhBMP-2 loaded PLGA microspheres and calcium phosphate cement. J. Mater. Sci. Mater. Med. 19:1109–1116, 2008.
Franke, S. V., C. B. Johansson, T. Sawase, Y. Yamasaki, and S. Oida. FGF-4 and titanium implants: a pilot study in rabbit bone. Clin. Oral. Implants Res. 14:363–368, 2003.
Gospodarowicz, D., N. Ferrara, L. Schweigerer, and G. Neufeld. Structural characterization and biological functions of fibroblast growth factor. Endocr. Rev. 8:95–114, 1987.
Hanada, K., J. E. Dennis, and A. I. Caplan. Stimulatory effects of basic fibroblast growth factor and bone morphogenetic protein-2 on osteogenic differentiation of rat bone marrow-derived mesenchymal stem cells. J. Bone Miner. Res. 12:1606–1614, 1997.
Hay, E., M. Hott, A. M. Graulet, A. Lomri, and P. J. Marie. Effects of bone morphogenetic protein-2 on human neonatal calvaria cell differentiation. J. Cell. Biochem. 72:81–93, 1999.
Hosokawa, R., K. Kikuzaki, T. Kimoto, T. Matsuura, D. Chiba, M. Wadamoto, Y. Sato, M. Maeda, A. Sano, and Y. Akagawa. Controlled local application of basic fibroblast growth factor (FGF-2) accelerates the healing of GBR. An experimental study in beagle dogs. Clin. Oral Implants Res. 11:345–353, 2000.
Huang, Z., E. R. Nelson, R. L. Smith, and S. B. Goodman. The sequential expression profiles of growth factors from osteoprogenitors [correction of osteroprogenitors] to osteoblasts in vitro. Tissue Eng. 13:2311–2320, 2007.
Jager, M., J. Fischer, W. Dohrn, X. Li, D. C. Ayers, A. Czibere, W. C. Prall, S. Lensing-Hohn, and R. Krauspe. Dexamethasone modulates BMP-2 effects on mesenchymal stem cells in vitro. J. Orthop. Res. 26:1440–1448, 2008.
Khairoun, I., D. Magne, O. Gauthier, J. M. Bouler, E. Aguado, G. Daculsi, and P. Weiss. In vitro characterization and in vivo properties of a carbonated apatite bone cement. J. Biomed. Mater. Res. 60:633–642, 2002.
Kotev-Emeth, S., S. Pitaru, S. Pri-Chen, and N. Savion. Establishment of a rat long-term culture expressing the osteogenic phenotype: dependence on dexamethasone and FGF-2. Connect. Tissue Res. 43:606–612, 2002.
Lan, J., Z. Wang, Y. Wang, J. Wang, and X. Cheng. The effect of combination of recombinant human bone morphogenetic protein-2 and basic fibroblast growth factor or insulin-like growth factor-I on dental implant osseointegration by confocal laser scanning microscopy. J. Periodontol. 77:357–363, 2006.
Lane, N. E., J. Kumer, W. Yao, T. Breunig, T. Wronski, G. Modin, and J. H. Kinney. Basic fibroblast growth factor forms new trabeculae that physically connect with pre-existing trabeculae, and this new bone is maintained with an anti-resorptive agent and enhanced with an anabolic agent in an osteopenic rat model. Osteoporos. Int. 14:374–382, 2003.
Lecanda, F., L. V. Avioli, and S. L. Cheng. Regulation of bone matrix protein expression and induction of differentiation of human osteoblasts and human bone marrow stromal cells by bone morphogenetic protein-2. J. Cell. Biochem. 67:386–396, 1997.
Lieberman, J. R., A. Daluiski, and T. A. Einhorn. The role of growth factors in the repair of bone. Biology and clinical applications. J. Bone Joint Surg. Am. 84-A:1032–1044, 2002.
Maegawa, N., K. Kawamura, M. Hirose, H. Yajima, Y. Takakura, and H. Ohgushi. Enhancement of osteoblastic differentiation of mesenchymal stromal cells cultured by selective combination of bone morphogenetic protein-2 (BMP-2) and fibroblast growth factor-2 (FGF-2). J. Tissue Eng. Regen. Med. 1:306–313, 2007.
Manolagas, S. C., D. W. Burton, and L. J. Deftos. 1,25-Dihydroxyvitamin D3 stimulates the alkaline phosphatase activity of osteoblast-like cells. J. Biol. Chem. 256:7115–7117, 1981.
Mathew, S., S. Arandjelovic, W. F. Beyer, S. L. Gonias, and S. V. Pizzo. Characterization of the interaction between alpha2-macroglobulin and fibroblast growth factor-2: the role of hydrophobic interactions. Biochem. J. 374:123–129, 2003.
Morley, P., J. F. Whitfield, and G. E. Willick. Parathyroid hormone: an anabolic treatment for osteoporosis. Curr. Pharm. Des. 7:671–687, 2001.
Naganawa, T., L. Xiao, J. D. Coffin, T. Doetschman, M. G. Sabbieti, D. Agas, and M. M. Hurley. Reduced expression and function of bone morphogenetic protein-2 in bones of Fgf2 null mice. J. Cell. Biochem. 103:1975–1988, 2008.
Pan, Z., and P. Jiang. Assessment of the suitability of a new composite as a bone defect filler in a rabbit model. J. Tissue Eng. Regen. Med. 2:347–353, 2008.
Presta, M., P. Dell’Era, S. Mitola, E. Moroni, R. Ronca, and M. Rusnati. Fibroblast growth factor/fibroblast growth factor receptor system in angiogenesis. Cytokine Growth Factor Rev. 16:159–178, 2005.
Reddi, A. H. Bone morphogenetic proteins: an unconventional approach to isolation of first mammalian morphogens. Cytokine Growth Factor Rev. 8:11–20, 1997.
Reddi, A. H., and N. S. Cunningham. Initiation and promotion of bone differentiation by bone morphogenetic proteins. J. Bone Miner. Res. 8(Suppl 2):S499–S502, 1993.
Rice, D. P., T. Aberg, Y. Chan, Z. Tang, P. J. Kettunen, L. Pakarinen, R. E. Maxson, and I. Thesleff. Integration of FGF and TWIST in calvarial bone and suture development. Development 127:1845–1855, 2000.
Rifkin, D. B., and D. Moscatelli. Recent developments in the cell biology of basic fibroblast growth factor. J. Cell Biol. 109:1–6, 1989.
Rubin, M. R., and J. P. Bilezikian. New anabolic therapies in osteoporosis. Curr. Opin. Rheumatol. 14:433–440, 2002.
Ruhe, P. Q., H. C. Kroese-Deutman, J. G. Wolke, P. H. Spauwen, and J. A. Jansen. Bone inductive properties of rhBMP-2 loaded porous calcium phosphate cement implants in cranial defects in rabbits. Biomaterials 25:2123–2132, 2004.
Shen, Q. G., C. H. Lin, and X. Zhen. Practical Biomedical Materials. Shanghai: Shanghai Science and Technology Press, 2005.
Sieron, A. L., N. Louneva, and A. Fertala. Site-specific interaction of bone morphogenetic protein 2 with procollagen II. Cytokine 18:214–221, 2002.
Singhatanadgit, W., V. Salih, and I. Olsen. Up-regulation of bone morphogenetic protein receptor IB by growth factors enhances BMP-2-induced human bone cell functions. J. Cell. Physiol. 209:912–922, 2006.
Sorensen, R. G., U. M. Wikesjo, A. Kinoshita, and J. M. Wozney. Periodontal repair in dogs: evaluation of a bioresorbable calcium phosphate cement (Ceredex) as a carrier for rhBMP-2. J. Clin. Periodontol. 31:796–804, 2004.
Strauss, E. J., B. Pahk, F. J. Kummer, and K. Egol. Calcium phosphate cement augmentation of the femoral neck defect created after dynamic hip screw removal. J. Orthop. Trauma 21:295–300, 2007.
Sun, X. J., Z. Y. Zhang, S. Y. Wang, S. A. Gittens, X. Q. Jiang, and L. L. Chou. Maxillary sinus floor elevation using a tissue-engineered bone complex with OsteoBone and bMSCs in rabbits. Clin. Oral Implants Res. 19:804–813, 2008.
Tabata, Y. Tissue regeneration based on growth factor release. Tissue Eng. 9(Suppl 1):S5–S15, 2003.
Tadic, D., F. Beckmann, K. Schwarz, and M. Epple. A novel method to produce hydroxyapatite objects with interconnecting porosity that avoids sintering. Biomaterials 25:3335–3340, 2004.
Tanaka, E., Y. Ishino, A. Sasaki, T. Hasegawa, M. Watanabe, D. A. la-Bona, E. Yamano, T. M. van Eijden, and K. Tanne. Fibroblast growth factor-2 augments recombinant human bone morphogenetic protein-2-induced osteoinductive activity. Ann. Biomed. Eng. 34:717–725, 2006.
Tanaka, H., A. Wakisaka, H. Ogasa, S. Kawai, and C. T. Liang. Effects of basic fibroblast growth factor on osteoblast-related gene expression in the process of medullary bone formation induced in rat femur. J. Bone Miner. Metab. 21:74–79, 2003.
Tsutsumi, S., A. Shimazu, K. Miyazaki, H. Pan, C. Koike, E. Yoshida, K. Takagishi, and Y. Kato. Retention of multilineage differentiation potential of mesenchymal cells during proliferation in response to FGF. Biochem. Biophys. Res. Commun. 288:413–419, 2001.
Turgeman, G., Y. Zilberman, S. Zhou, P. Kelly, I. K. Moutsatsos, Y. P. Kharode, L. E. Borella, F. J. Bex, B. S. Komm, P. V. Bodine, and D. Gazit. Systemically administered rhBMP-2 promotes MSC activity and reverses bone and cartilage loss in osteopenic mice. J. Cell. Biochem. 86:461–474, 2002.
Ueda, H., L. Hong, M. Yamamoto, K. Shigeno, M. Inoue, T. Toba, M. Yoshitani, T. Nakamura, Y. Tabata, and Y. Shimizu. Use of collagen sponge incorporating transforming growth factor-beta1 to promote bone repair in skull defects in rabbits. Biomaterials 23:1003–1010, 2002.
Varkey, M., C. Kucharski, T. Haque, W. Sebald, and H. Uludag. In vitro osteogenic response of rat bone marrow cells to bFGF and BMP-2 treatments. Clin. Orthop. Relat. Res. 443:113–123, 2006.
Yamagiwa, H., N. Endo, K. Tokunaga, T. Hayami, H. Hatano, and H. E. Takahashi. In vivo bone-forming capacity of human bone marrow-derived stromal cells is stimulated by recombinant human bone morphogenetic protein-2. J. Bone Miner. Metab. 19:20–28, 2001.
Zellin, G., and A. Linde. Effects of recombinant human fibroblast growth factor-2 on osteogenic cell populations during orthopic osteogenesis in vivo. Bone 26:161–168, 2000.
Zhang, Y., B. Shi, C. Li, Y. Wang, Y. Chen, W. Zhang, T. Luo, and X. Cheng. The synergetic bone-forming effects of combinations of growth factors expressed by adenovirus vectors on chitosan/collagen scaffolds. J. Control. Release 136:172–178, 2009.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, L., Huang, Y., Pan, K. et al. Osteogenic Responses to Different Concentrations/Ratios of BMP-2 and bFGF in Bone Formation. Ann Biomed Eng 38, 77–87 (2010). https://doi.org/10.1007/s10439-009-9841-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9841-8