Abstract
Introduction
There is an increasingly controversial debate about the best possible incisional hernia repair technique. Despite the good outcomes of laparoscopic IPOM, concerns about the intraperitoneal mesh placement and its potential intraabdominal complications have risen. Against that background, this paper now analyzes changes and trends in incisional hernia repair techniques in the recent decade.
Methods
Between 2010 and 2019 a total of 61,627 patients with primary elective incisional hernia repair were enrolled in the Herniamed Registry. The outcome results were assigned to the year of repair and summarized as curves to visualize trends. The explorative Fisher’s exact test was used for statistical calculation of significant differences. Since the number of cases entered into the Herniamed Registry for the years 2010–2012 was still relatively small, the years 2013 and 2019 were compared for statistical analysis.
Results
In the analyzed time period, the proportion of incisional hernias repaired in open suture technique remained unchanged at about 10%. The proportion of laparoscopic IPOM repairs decreased significantly from 33.8% in 2013 to 21.0% (p < 0.001) in 2019. Conversely, the proportion of open sublay repairs increased significantly from 32.1% in 2013 to 41.4% (p < 0.001) in 2019. Starting in 2015, there has also been the introduction and increasing use (4.5% in 2013 vs. 10.0% in 2019; p < 0.001) of new minimally-invasive techniques with placement of a mesh into the sublay/retromuscular/preperitoneal abdominal wall layer (E/MILOS, eTEP, preperitoneal mesh technique).
Conclusion
Analysis of data from the Herniamed Registry shows a significant trend to the disadvantage of the laparoscopic IPOM and to the advantage of the open sublay operation and the new minimally-invasive techniques (E/MILOS, eTEP, preperitoneal mesh technique). Despite all the recommendations in the guidelines, 10% of incisional hernias continue to be treated by means of a suture technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of incisional hernias three years after abdominal surgery is as high as 22.4% [1,2,3], with equal distribution between men and women [4]. In Germany around 50,000 [5] and in the USA 100,000 [6] incisional hernia repairs are carried out each year. In the USA the costs incurred in 2011 for hospital treatment of an incisional hernia were $60,968, amounting to annual costs of $7.3 billion for the healthcare system [6].
Several guidelines for ventral hernia repair have been published in recent years [8,9,10,11,12,13,14,15], indicating that the laparoscopic intraperitoneal onlay mesh (IPOM) and open sublay mesh repair techniques are currently the most widely used procedures for the treatment of abdominal wall hernias [16]. It has also been shown that there is a significant difference in the outcome of primary ventral hernia repair (umbilical, epigastric) compared to incisional hernia repair, underlining that merging of both patient populations in studies should be omitted [17,18,19,20,21,22]. Especially for incisional hernia repair, surgical site occurrences are the ‘Achilles heel’ [7] with a strong economic burden. Therefore, strict adherence to standardized guidelines is of utmost importance to keep the postoperative complication rate to a minimum [7]. With respect to wound complications, lower rates have been shown for the laparoscopic intraperitoneal onlay mesh (IPOM) technique compared to open mesh repair [23,24,25,26,27]. As regards recurrence rates following primary elective incisional hernia repair, a Danish Ventral Hernia Database study was unable to demonstrate any difference on comparing laparoscopic IPOM and open mesh procedures (10.6% vs. 12.3%) with a mean follow-up of 59 months. However, in the same population mesh-related complications requiring reoperation occurred less frequently in laparoscopic IPOM repairs than in open mesh repair (2.4% vs. 5.2%) [28].
Interestingly, over the last decade laparoscopic IPOM was deemed to cause more intraperitoneal complications since it has been shown to carry an increased risk of intraoperative bowel injuries [16]. Concerns have been raised about potential visceral adhesions, bowel obstruction, fistulation, mesh migration and impaired durability of bridging repairs, thus challenging the role of laparoscopic IPOM repair as the gold standard in ventral hernia repair [29]. At the same time this discussion has propelled the development of alternative techniques with mesh placement outside the abdominal cavity under perpetuation of the minimally-invasive approach [29]. Accordingly, these new minimally-invasive extraperitoneal techniques, such as E/MILOS (Mini Less Open Sublay repair) or eTEP (Extended totally extraperitoneal repair), have been introduced [15], showing promising results compared to the laparoscopic IPOM and conventional open techniques [16].
Since laparoscopic IPOM is now being challenged by the new minimally-invasive extraperitoneal techniques as the gold standard in ventral hernia repair, it remains unclear to what extent everyday surgical techniques have changed over the last decade. Therefore, this study aims to analyze incisional hernia repair techniques and their outcomes over the past 10 years based on data from the Herniamed registry [30, 31].
Methods
Herniamed is an internet-based hernia registry with voluntary participating hospitals and surgeons from Germany, Austria and Switzerland [4, 27, 30, 31]. In Herniamed the participating institutions can enter prospective data on all routine hernia repairs performed. The number of participating institutions by December 31, 2019 was 737. All patients have signed a consent form agreeing to their data being processed by Herniamed. As part of the informed consent declaration regarding participation in the Herniamed Registry, patients are informed that the hospital or surgeon providing treatment would like to be informed about any problem occurring after the hernia operation and that the patient may at any time contact the treating institution or surgeon to arrange for clinical examination.
Initially, the postoperative complications are registered for up to postoperative day 30 [31]. For the postoperative surgical complications a distinction is made between bleeding, wound healing disorder, deep infection, seroma and hematoma [31]. Complication-related reoperations are also recorded [31]. Here seroma is defined as serous fluid collection in the wound area, wound healing disorder as superficial wound dehiscence and deep infection as deep wound infection with mesh involvement.
After 1, 5 and 10 years patients and their general practitioner are sent a questionnaire by the treating institution, enquiring once again about any subsequent postoperative complications [31].
The questionnaire also asks patients and the general practitioner about any pain at rest, pain on exertion or pain requiring treatment. Patients are also asked whether they have experienced any protrusion suggestive of hernia recurrence. If the patient or general practitioner reports such a finding, the patient is contacted by the treating institution and requested to attend clinical examination [27, 30, 31].
In the current analysis, prospective data of patients who underwent primary elective incisional hernia repair with the laparoscopic intraperitoneal onlay mesh (IPOM) technique or open suture, sublay, onlay, IPOM or other procedures were evaluated to determine the perioperative and one-year follow-up outcomes. All infrequently used alternative techniques and new procedures can only be documented in the Herniamed registry in the group of “other techniques”. Under “other techniques” the surgical technique can be entered as free text and later evaluated.
The explorative Fisher’s exact test was used for statistical calculation of significant differences with an alpha = 5%. For post-hoc tests of single categories, a Bonferroni adjustment for multiple testing was implemented. Since the annual number of cases in the Herniamed Registry for the years 2010–2012 was still relatively low and there was thus considerable fluctuation in the analysis result, the years 2013 and 2019 exhibiting a more stable trend were compared. That applies for comparison of the surgical techniques used and of the postoperative complications. Since only the results for the years 2010–2018 were available for one-year follow-up, testing for significant differences in the recurrence and pain rates is based on comparison of the results obtained for the years 2013 and 2018.
Results
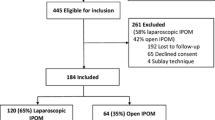
Between 2010 and 2019 a total of 61,627 patients with primary elective incisional hernia repair were enrolled in the Herniamed Registry (Fig. 1). The increase in the number of cases each year is due to the growing number of hospitals participating in the Herniamed Registry (Table 1). Follow-up is available for 40,169 of 51,517 (78%) of patients for the years 2010–2018.
Surgical procedures
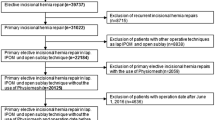
Open sublay and laparoscopic IPOM techniques were the most frequently used surgical procedures (Table 2) in the study population. Statistical analysis of the use of the various surgical techniques for 2013 versus 2019 reveals a significant decline in the use of the laparoscopic IPOM technique from 33.8% to 21.0% (p < 0.001) (Fig. 2). During the same period, the rate of open sublay repairs rose significantly from 32.1% in 2013 to 41.4% (p < 0.001) in 2019. The proportion of incisional hernias repaired in open suture technique remained unchanged at about 10%.
The use of open IPOM and open onlay remained relatively constant at a low level during the investigated time period. Component separation technique was used significantly more often (1.9% in 2013 vs. 3.1% in 2019; p < 0.001) but with a low frequency. The continuing use of the suture technique to treat around 10% of incisional hernias is surprising.
Noteworthy is then the significant rise (4.5% in 2013 vs. 10.0% in 2019; p < 0.001) in the “other techniques” starting in 2015. Further analysis of this subgroup revealed that this group contained 955 E/MILOS, 878 laparo-endoscopic procedures with mesh placement in the sublay/retromuscular space (eTEP) and 681 open preperitoneal mesh techniques.
Hence, a significant trend is seen in favor of the new techniques as well as in favor of the open sublay over the laparoscopic IPOM technique.
Hernia size
The European Hernia Society (EHS) width classification was used to assess whether the patient collective operated on over the observation period had changed [32,33,34]. Analysis of EHS width classification showed a marked rise in smaller defects (EHS W1: < 4 cm) from 34.3% in 2013 to 39.7% in 2019 (p < 0.001) and a decline in the medium defect sizes (EHS W2: ≥ 4–10 cm) from 47.1% in 2013 to 43.7% in 2019 (p < 0.001). The proportion of large defects (EHS W3: > 10 cm) decreased from 18.6% in 2013 to 16.6% in 2019 (p = 0.0063).
The proportion of patients with incisional hernia and previous laparoscopic gallbladder removal, appendectomy and inguinal hernia repair increased significantly over the 7-year period (Fig. 3). The proportion of medial localizations in primary elective incisional hernia repairs also increased significantly (71.6% in 2013 vs. 77.4% in 2019; p < 0.0001) and the lateral and combined defect localizations decreased.
Complications, recurrence and pain
Comparison of the postoperative surgical complication rates and rates of complication-related reoperations (Fig. 4) showed that in the case of sublay repair these declined significantly from 11.8% in 2013 to 9.0% in 2019 (p = 0.0013). The complication-related reoperation rate dropped slightly, but not significantly, from 5.3% in 2013 to 4.5% in 2019. That was also true for the laparoscopic IPOM, where the postoperative surgical complication rate decreased significantly from 5.3% in 2013 to 3.0% in 2019 (p = 0.0004). Similarly, the complication-related reoperation rate dropped significantly from 2.2% to 1.3% (p = 0.0449). Of importance for the decline in the postoperative complication rate was the significantly decreased seroma rate from 4.2% in 2013 to 2.5% in 2019 (p < 0.0001) (Fig. 5).
Based on one-year follow-up of the n = 40,169/51,517 (78.0%) patients for the years 2010–2018, it was also possible to identify the pain rates and hernia recurrence rates. The recurrence rate significantly decreased from 5.6% in 2013 to 4.7% in 2018 (p = 0.0385). Whereas the rate of chronic pain requiring treatment at about 8% did not change between 2013 and 2018, the rate of pain on exertion declined significantly from 19.5% in 2013 to 16.7% in 2018 (p = 0.0006) (Fig. 6).
Discussion
This is the first prospective study investigating the trends in the application of different surgical techniques for incisional hernia repair over a full decade (2010–2019) based on the validated large-scale database Herniamed. Several important trends have been identified, such as the significant decline in the application of laparoscopic IPOM repair, challenging its perceived role as the gold standard in incisional hernia repair. By contrast, new minimally invasive and open techniques with extraperitoneal mesh placement, such as E/MILOS, eTEP and laparo-endoscopic preperitoneal mesh placement, have been used more frequently with every year. This is also true for open sublay repair, although its disadvantages regarding wound complications are undisputed. The quality of hernia repair has significantly increased, as indicated by the decreasing rates of postoperative complications for open sublay and laparoscopic IPOM, complication-related reoperations for laparoscopic IPOM and seroma formation, recurrence rate and rate of pain on exertion for the total collective. However, it has also been demonstrated that some outcomes such as wound healing disorder, deep infection and rates of pain at rest and chronic pain requiring treatment have not changed over the last decade, underlining the need for further optimization of the quality of incisional hernia repair.
One of the most important findings of our study is the significant decline in the use of the laparoscopic IPOM technique in incisional hernia repair. After reaching its peak in 2013 with a proportion of 33.8%, it continued to drop to 21.0% in 2019. These numbers are reflected by data from French [21] and USA [35] databases, where laparoscopic IPOM techniques were used for incisional hernia repair in 26% and 31%, respectively. However, the central issue is not the proportion alone but the dramatic decline over time. This steeply sloping trend may be explained by the increasing apprehensions associated with potential intraoperative complications and the intraperitoneal mesh position [15, 16, 29]. Our data suggest that surgeons have therefore either switched back to standard open sublay repair or applied new techniques, such as E/MILOS, eTEP or laparo-endoscopic preperitoneal mesh placement, while striving to assure a low risk of surgical site occurrences and infections using minimally-invasive approaches for incisional hernia repair. Another explanation may be that as per the current guideline recommendations the laparoscopic IPOM approach is suitable only for defects of less than 8–10 cm [8,9,10,11,12,13,14,15]. But considering that in our study the proportion of defects > 10 cm remained unchanged and defects of 4–10 cm even decreased over the 10-year time period, the incremental growth in open sublay repair seems worrisome in view of the associated risks of wound complications. The current proportion of open sublay repairs of 41.4% by 2019 in our study population exceeds, for example, that in the French registry (30% in the period of 2011–2016) [21, 33]. The trend towards applying new minimally-invasive techniques, as recorded in our registry, may be the solution to this problem. This development seems a logical step driven by the dilemma presented by the laparoscopic IPOM, while moving the mesh out of the abdominal cavity into the retromuscular space, without abdicating the minimally-invasive approach. Although the initial study results comparing these techniques with laparoscopic IPOM and open sublay provided excellent outcomes [15, 16], more long-term data are needed to underscore their claim to being the new standard for minimally-invasive incisional hernia repair. Furthermore, there is an urgent need to clearly name each new minimally-invasive extraperitoneal technique in the registry to be able to differentiate between such new techniques and effectively link them with their respective outcomes.
There are also changing trends in surgical techniques apart from laparoscopic IPOM and open sublay repair. The proportion of open intraperitoneal onlay mesh (IPOM) repair slightly declined from 12.0% to 10.8% in the last 7 years in our study, which contradicts the unchanged high proportion of 31.1% in the French registry [21]. Open onlay repairs, although indicated in certain circumstances and experiencing a revival especially in the USA, decreased from 5.1% to 3.8% (p = 0.0042) during our 7-year study period, reflecting proportions in the French registry (3%) [21]. The proportion of surgical procedures using component separation techniques increased significantly from 1.9% in 2013 to 3.1% in 2019 (p < 0.001),but in general remained low, reflecting their main indication to facilitate tension-free closure of complex incisional hernias.
Another interesting finding of our study was that 10% of patients are still undergoing simple suture repair, despite all guidelines recommending the use of meshes for incisional hernia repair [8,9,10,11,12,13,14,15]. This trend has not changed over the last decade, indicating that there seem to be legitimate reasons justifying the violation of the guidelines. This is reflected by Danish, British and French database analyses, where the portion of primary suture repairs was similar or even higher ranging from 10 to 18% [21, 36, 37]. One explanation for this discrepancy may be the fear of mesh-related complications or mesh refusal by the patient, although the use of mesh repair even in smaller incisional trocar hernias has been proven to be advantageous.
Obviously, the practicability of mesh implantation in small hernias seems to be questioned by some surgeons, tending towards simple suture repair in cases of smaller incisional hernias, such as trocar hernias. In our study population the proportion of small incisional hernias (EHS defect width W I, < 4 cm) increased from 30 to 40% in the last 10 years, with a simultaneous decline in larger incisional hernias (EHS defect width II and III). The overall rate of trocar hernias was reported in a systematic review [38] to have increased from 5.2% to 26% in a three-year follow-up after laparoscopic cholecystectomy [39]. Most trocar hernias occur around the umbilicus [38], which may be explained by the fact that this trocar site is frequently used for the larger camera port or for specimen extraction. Considering the constant rise in laparoscopic procedures, in general, and in visceral surgery since its implementation in the 1990s, it is not surprising that the proportion of incisional hernias following such procedures (e.g., laparoscopic cholecystectomy, appendectomy or inguinal hernia repair) increased in our study period. The increase was especially noticeable in the patient subgroup with EHS defect width W I (< 4 cm) and predominantly medial defect localizations, serving as a surrogate marker for trocar hernias. This underlines the importance of keeping the trocar diameter to the smallest possible size, using 5 mm optics when applicable and extracting specimens through lateral port sites.
As a result of the promotion of quality-guided hernia surgery, the postoperative complication rates and complication-related reoperation rates for both the open sublay and laparoscopic IPOM techniques improved over the last decade in our study population. In the case of the laparoscopic IPOM, this is thought to be due to the continuously updated guideline restricting this technique to defects measuring at most 8–10 cm [9,10,11,12,13,14,15]. With strict compliance with these guidelines, the positive impact of these evidence-based recommendations on the outcome quality of surgical procedures is clearly visible in our study population. Since postoperative surgical site occurrences are considered to be the “Achilles heel” [7] in open sublay repair, the improvement in these events in our study population was essentially due to reduction of the seroma rate. In a systematic review the adjuncts to reduce seroma in open incisional hernia repair were identified [40]. However, the clear role of drains, abdominal binders, fibrin glue and other agents must be investigated further. Another explanation for this trend may be that surgeons are increasingly avoiding the use of wide tissue dissection with creation of large flaps [41]. Also, the increasing proportion of smaller incisional hernias < 4 cm has helped to improve the rates of wound complications for both the laparoscopic IPOM and open sublay repair techniques in our study population, underlining the strong correlation between the defect width and risk of postoperative complication [33, 34]. The rate of recurrences and pain on exertion showed only a slight improvement over the 7-year period. Since the outcome parameters are of multifactorial genesis, these minor changes are thought to be linked to the composition of the patient collectives and to the strong adherence to the available evidence-based guidelines, for example avoidance of the laparoscopic IPOM approach for hernias > 10 cm.
Registry studies have certain limitations. Since participation in the Herniamed Registry is voluntary, thus making it attractive to hernia-interested surgeons, bias cannot be ruled out here. To achieve as far as possible complete and correct data entry, all surgeons participating in the Herniamed Registry sign a contract committing to complete and correct data entry. Missing data are highlighted by the software. Data entry can be verified at the time of auditing certification or recertification of hernia centers. Since follow-up in the Herniamed Registry is based on questionnaires with patient and general practitioner reported outcomes, which has been proven to be effective by Baucom et al. [42], follow-up is not available for a relevant proportion of patients. In other analyses of data from the Herniamed Registry it has been possible to reliably detect only negligible selection bias by calculating the standardized differences for all patient- and operation-related variables as well as the post- and perioperative outcome variables [34]. Furthermore, concordance between these findings and those in the literature is always verified.
In summary, we have shown that over the last decade there has been a significant change in the operation techniques used, with a growth in open sublay repair and new minimally-invasive extraperitoneal techniques to the previous level of the laparoscopic IPOM, which now decreased dramatically. Some trends remained unchanged, such as the number of suture repairs. An increase in smaller incisional hernia repairs, mostly composed of trocar hernias, has been detected. Last but not least, the quality of incisional hernia repair has improved, as measured by a decline in postoperative surgical complications and complication-related reoperations in open sublay and laparoscopic IPOM repair, complication-related reoperation rate in laparoscopic IPOM as well as a slightly improved rate of recurrence and pain on exertion. This real-world study therefore contributes to the important outcome research in the field of incisional hernia surgery.
References
Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A et al (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14.618 patients. PLoS ONE 10:e0138745. https://doi.org/10.1371/journal.pone.0138745
Fink C, Baumann P, Wente MN, Knebel P, Bruckner T, Ulrich A et al (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg 101:51–54. https://doi.org/10.1002/bjs.9364
Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y et al (2014) Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg 101:1439–1447. https://doi.org/10.1002/bjs.9600
Köckerling F, Hoffmann H, Adolf D, Weyhe D, Reinpold W, Koch A, Kirchhoff P (2019) Female gender as independent risk factor for chronic pain following elective incisional hernia repair: a registry-based, propensity score-matched comparison of 22.895 patients. Hernia. https://doi.org/10.1007/s10029-019-02089-2 ((epub ahead of print))
Statistisches Bundesamt (Destatis), 2019 Artikelnummer: 5231402187005
Shubinets V, Fox JP, Lanni MA, Ticce MG, Pauli EM, Hope WW et al (2018) Incisional Hernia in the United States: trends in hospital encounters and corresponding healthcare charges. Am Surg 84:118–125
Tubre DJ, Schroeder AD, Estes J, Eisenga J, Fitzgibbons RJ Jr (2018) Surgical site infection: the “Achilles Heel” of all types of abdominal wall hernia reconstruction. Hernia 22:1003–1013. https://doi.org/10.1007/s10029-018-1826-9
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F et al (2014a) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part 1. Surg Endosc 28:2–29. https://doi.org/10.1007/s00464-013-3170-6
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F et al (2014b) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part 2. Surg Endosc 28:353–379. https://doi.org/10.1007/s00464-013-3171-5
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F et al (2014c) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part 3. Surg Endosc 28:380–404. https://doi.org/10.1007/s00464-013-3172-4
Earle D, Roth JS, Saber A, Haggerty S, Bradley JF, Fanelli R et al (2016) SAGES guidelines for laparoscopic ventral hernia repair. Sur Endosc 30:3163–3183. https://doi.org/10.1007/s00464-016-5072-x
Silecchia G, Campanile FC, Sanchez L, Ceccarelli G, Antinori A, Ansaloni L et al (2015) Laparoscopic ventral/incisional hernia repair: updated guidelines from the EAES and EHS endorsed Consensus Development Conference. Surg Endosc 29:2463–2584. https://doi.org/10.1007/s00464-015-4293-8
Liang MK, Holihan JL, Itani K, Alawadi ZM, Flores Gonzales JR, Askenasi EP et al (2017) Ventral Hernia management—expert consensus guided by systematic review. Ann Surg 265:80–89. https://doi.org/10.1097/SLA.0000000000001701
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D et al (2019a) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—part A. Surg Endosc 33:3069–3139. https://doi.org/10.1007/s00464-019-06907-7
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D et al (2019b) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—part B. Surg Endosc 33:3511–3549. https://doi.org/10.1007/s00464-019-06908-6
Reinpold W, Schröder M, Berger C, Nehls J, Schroeder A, Hukauf M, Köckerling F, Bittner R (2019) Mini- or less-open sublay operation (milos): a new minimally invasive technique for the extraperitoneal mesh repair of incisional hernias. Ann Surg 269:748–755. https://doi.org/10.1097/SLA.0000000000002661
Kurian A, Gallagher S, Cheeyandira A, Josloff R (2010) Laparoscopic repair of primary versus incisional ventral hernias: time to recognize the differences? Hernia 14:383–387. https://doi.org/10.1007/s10029-010-0649-0
Stirler VMA, Schoenmaeckers EJP, de Haas RJ, Raymakers JTFJ, Rakic S (2014) Laparoscopic repair of primary and incisional ventral hernias: the differences must be acknowledged. Surg Endosc 28:891–895. https://doi.org/10.1007/s00464-013-3243-6
Köckerling F, Schug-Paß C, Adolf D, Reinpold W, Stechemesser B (2015) Is pooled data analysis of ventral and incisional hernia repair acceptable? Front Surg 2:15. https://doi.org/10.3389/fsurg.2015.00015
Subramanian A, Clapp ML, Hicks SC, Awad SS (2013) Liang MK (2013) Laparoscopic ventral hernia repair: primary versus secondary hernias. J Surg Res 181(1):e1-5. https://doi.org/10.1016/j.jss.2012.06.028
Kroese LF, Gillion JF, Jeekel J, Kleinrensink GJ, Lange JF (2018) The Hernia Club Members Primary and incisional ventral hernias are different in terms of patient characteristics and postoperative complications—a prospective cohort study of 4,565 patients. Int J Surg 51:114–119. https://doi.org/10.1016/j.ijsu.2018.01.010
Stabilini C, Cavallaro G, Dolce P, Giovannini SC, Corcione F, Frascio M, Sodo M, Merola G, Bracale U (2019) Pooled data analysis of primary ventral (PVH) and incisional hernia (IH) repair is no more acceptable: results of a systematic review and meta-analysis of current literature. Hernia 23:831–845. https://doi.org/10.1007/s10029-019-02033-4
Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74. https://doi.org/10.1016/j.ijsu.2015.05.050
Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, Memon MA (2015a) Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia 19:449–463. https://doi.org/10.1007/s10029-015-1351-z
Jensen KK, Jorgensen LN (2015) Comment to: Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Awaiz A et al. Hernia 2015;19:449–463. Hernia 19:1025–1026. https://doi.org/10.1007/s10029-015-1412-3
Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, Memon MA (2015b) Reply to comment to Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Jensen K, Jorgensen LN. Hernia 19:1027–1029. https://doi.org/10.1007/s10029-015-1432-z
Köckerling F, Simon T, Adolf D, Köckerling D, Mayer F, Reinpold W, Weyhe D (2019) Laparoscopic IPOM versus open sublay technique for elective incisional hernia repair: a registry-based, propensity score-matched comparison of 9.907 patients. Surg Endosc 33:3361–3369. https://doi.org/10.1007/s00464-018-06629-2
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 316(15):1575–1582. https://doi.org/10.1001/jama.2016.15217
Sharma A, Berger D (2018) The current role of laparoscopic IPOM repair in abdominal wall reconstruction. Hernia 22:739–741. https://doi.org/10.1007/s10029-018-1820-2
Stechemesser B, Jacob DA, Schug-Pass C (2012) Köckerling Herniamed: an internet-based registry for outcome research in hernia surgery. Hernia 16:269–276. https://doi.org/10.1007/s10029-012-0908.3
Kyle-Leinhase I, Köckerling F, Jorgensen LN, Montgomery A, Gillion JF, Rodriguez JAP, Hope W, Muysoms F (2018) Comparison of hernia registries: the CORE project. Hernia 22:561–575. https://doi.org/10.1007/s10029-017-1724-6
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RKF, Simons MP, Smietanski M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
Kroese LF, Kleinrensink GJ, Lange JF, Gillion JF, and the Hernia Club Members (2017) External validation of the European hernia society classification for postoperative complications after incisional hernia repair: a cohort study of 2,191 patients. Am College Surg. https://doi.org/10.1016/j.jamcollsurg.2017.11.018
Köckerling F, Hoffmann H, Adolf D, Reinpold W, Kirchhoff P, Mayer F, Weyhe D, Lammers B, Emmanuel K (2020) Potential influencing factors on the outcome in incisional hernia repair: a registry-based multivariable analysis of 22,895 patients. Hernia. https://doi.org/10.1007/s10029-020-02184-9
Savitch SL, Shah P (2016) Closing the gap between the laparoscopic and open approaches to abdominal wall hernia repair: a trend and outcomes analysis of the ACS-NSQIP database. Surg Endosc 30:3267–3278. https://doi.org/10.1007/s00464-015-4650-7
Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Bisgaard T (2013) Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll Surg 216:217–228. https://doi.org/10.1016/j.jamcollsurg.2012.10.013
Pawlak M, Tulloh B, de Beaux A (2020) Current trends in hernia surgery in NHS England. Am R Coll Surg Engl 102:25–27. https://doi.org/10.1308/rcsann.2019.0118
Helgstrand F, Rosenberg J, Bisgaard T (2011) Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia 15:113–121. https://doi.org/10.1007/s10029-010-0757-x
Comajuncosas J, Hermosos J, Gris P, Jimeno J, Orbeal R, Vallveru H et al (2014) Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: a prospective 3-year follow-up study. Am J Surg 207:1–6. https://doi.org/10.1016/j.amjsurg.2013.05.010
Massey LH, Pathak S, Bhargava A, Smart NJ, Daniels IR (2018) The use of adjuncts to reduce seroma in open incisional hernia repair: a systematic review. Hernia. https://doi.org/10.1007/s10029-017-1690-z
Chawla S commentary: changing trends in the management of incisional hernias. Medical Journal of Dr. D.Y. Patil University (2013) 6:1
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair—establishing the ventral hernia recurrence inventory. Am J Surg 212:81–88. https://doi.org/10.1016/j.amjsurg.2015.06.007
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Köckerling reports grants from Johnson & Johnson, Norderstedt, grants from Karl Storz, Tuttlingen, grants from pfm medical, Cologne, grants from Dahlhausen, Cologne, grants from B Braun, Tuttlingen, grants from MenkeMed, Munich, grants from Bard, Karlsruhe, during the conduct of the study; personal fees from Bard, Karlsruhe, outside the submitted work. All other authors have nothing to disclose.
Ethical approval
As only cases of routine hernia surgery are documented in the Herniamed Registry, an ethical approval was not neccessary.
Human and animal rights
This article does not contain any study with animals performed by any of the authors.
Informed consent
All patients with routine hernia surgery documented in the Herniamed Registry have signed an informed consent declaration agreeing to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Köckerling, F., Hoffmann, H., Mayer, F. et al. What are the trends in incisional hernia repair? Real-world data over 10 years from the Herniamed registry. Hernia 25, 255–265 (2021). https://doi.org/10.1007/s10029-020-02319-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02319-y