Abstract
Purpose
There is a risk of developing a trocar site hernia (TSH) after laparoscopic surgery, but data is sparse and based mostly on retrospective studies with a short and poorly defined follow-up period. Surgical approaches and patient-related co-morbidity have also been suggested as risk factors for development of TSH. The aim of the present review was to perform a qualitative systematic analysis to estimate the incidence of TSH and to discuss the surgical and patient-related risk factors for development of TSH.
Methods
The literature search was until 19 May 2010. Studies with TSH, defined as either operation for TSH or a hernia found during clinical follow-up, were included. We included randomised controlled trials, prospective non-controlled studies including >200 patients, and retrospective studies including >200 patients. The review was completed according to the PRISMA guidelines.
Results
We included 19 studies in adults and 3 studies in paediatric patients (<18 years), and a total of 30,568 adults and 1,098 children were analysed. The overall incidence of TSH was 0–5.2%. TSH occurred most often (96%) in trocar sites of a minimum of 10 mm, located mostly in the umbilicus region (82%). Data supported a higher incidence of TSH when the trocar site fascia was not sutured, and in pre-school children undergoing a laparoscopic procedure.
Conclusions
Current data suggests a relatively low incidence of TSH but that all trocar incisions of a minimum of 10 mm should be closed. In pre-school children undergoing laparoscopic surgery, all port sites should be closed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Compared with open abdominal surgery, the laparoscopic approach has gained widespread acceptance because of the perceived better postoperative outcomes in terms of less pain, faster recovery, and lower risk of incisional hernias [1, 2]. However, the risk of incisional hernia following laparoscopic surgery—trocar site hernia (TSH)—has been known since 1967 [3]. Nevertheless, data is sparse and based mostly on retrospective studies with a short and poorly defined follow-up [4–6]. Surgical approaches and patient-related co-morbidity have also been suggested as risk factors for development of TSH [5, 7], and controversies exist regarding both prevention and repair of TSH [6, 8].
The aim of this qualitative systematic review was to estimate the incidence of TSH, as well as to describe surgical- and patient-related risk factors for development of TSH.
Methods
We searched the literature from 1960 to 19 May 2010. Databases used were Pubmed and Embase, using “trocar site” or “port site” and “hernia” as search strings limited by “English” and “human”. In addition, manual searches in reference lists were performed. We defined adults as patients >18 years.
Studies were included only if TSH was clearly defined as either a clinical manifestation that made the patient contact the healthcare system or was found during follow-up. TSH was included if discovered at a clinical examination, ultrasound, computed tomography (CT)-scan or if the patient underwent surgery for TSH after a specific laparoscopic procedure. We included only randomised controlled trials (RCTs), prospective non-controlled studies including >200 patients, and retrospective studies including >200 patients. Duplicates, reviews and studies not concerning TSH and special new technologies in laparoscopic surgery (e.g. robotic and single port laparoscopy) were excluded.
The study was completed using the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [9].
Results
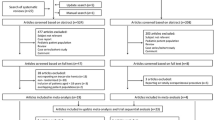
We identified 346 studies, including two studies from reference lists [10, 11] and 105 duplicates. In total, 219 studies were excluded. A total of 19 studies in adult patients and three studies in paediatric patients were included (Fig. 1). Thus, we included data from 30,568 adults and 1,098 children in the present analysis. This included three RCTs in adults (TSH were secondary end-points) [12–14], six prospective trials in adults [15–20], nine retrospective reports in adults [7, 10, 11, 21–26], and three retrospective studies in paediatric patients [27–29]. Results from studies in adult patients are outlined in Table 1.
Flowchart of study selection [9]. RCT Randomised controlled trial
Overall, the studies varied with respect to design, surgical procedures and follow-up (Table 1). The mean follow-up was described in seven studies and ranged from 1 to 31 months [7, 13, 15, 23–25]. One study [17] comparing two different trocars, presented a median follow-up for each group, which was 27 months and 54 months, respectively. Two studies [14, 22] had a median follow-up period of 13 and 16 months, respectively. Taylor et al. [30] registered retrospectively the incidence of TSH at admission within 3 years after primary surgery. In ten studies the follow-up periods were not mentioned [10–12, 18–21, 26–28].
In the randomised and prospective studies [12, 14–19], TSH was defined as a clinical palpable fascia defect in a previous trocar site found during follow-up. In two studies, TSH was found by either CT-scan or sonography [20, 22]. In 12 retrospective studies, TSH was found by clinical examination or following TSH repair, and in all cases the TSH were repaired [7, 10, 21, 23–30].
Trocar site hernia incidence in adults
The incidence of TSH in adults in the published studies was between 0 and 5.2% (Table 1), with an overall incidence of 0.5% when summarising data from the different studies. In total, 160 TSH were reported: 56 TSH occurred within 30 days (between 2 and 25 days) after the first laparoscopic procedure, 57 TSH were reported between 30 days and 2 years after laparoscopy, and in 47 patients the timing for reoperation was not provided. Except for one patient all patients had only a single TSH, meaning the incidence of hernia per trocar is 3–5 times lower, depending on the number of trocars used in the specific laparoscopic procedure. The incidence of acute operation for TSH was not reported in the available studies.
Surgical related risk factors for developing trocar site hernia in adults
Entry techniques
One randomised trial (n = 244) comparing blunt trocars with cutting trocars in abdominal surgery (not defined) found no TSH during a 6–18 months follow-up period [12]. On the other hand, Leibl et al. [17] found that cutting trocars (n = 600) were associated with a significantly higher TSH rate than blunt trocars (n = 600) (1.8% vs 0.2%, P < 0.01). However, the cutting trocar group had twice as long a follow-up period compared with the blunt trocar group (median 54 months vs 27 months). A prospective non-randomised study [18] (n = 403) comparing trocar entry using either Veress needle and a cutting trocar or open entry by Hasson technique, showed six TSH in the Veress needle group (3.0%) and no TSH in the open entry group (P = 0.01). One of the six TSH was in a patient who did not have the fascia closed, whereas all fascias in the group with open entry were closed using absorbable suture. In the group using Veress needle, the fascia at the umbilical port site was sutured when the defect was widened to remove specimens. The follow-up period ranged between 3 and 51 months.
Closure of the fascia
Adding together the data from Table 1, the incidence of TSH after suturing the fascia (regardless of the suture material) may be 0.6% (42 of 8,719), compared to 1.5% (53 of 3,585) when not suturing the fascia [4, 7, 10, 12, 16, 21]. Slow absorbable sutures were used to close the trocar site in three studies, with an incidence of TSH of up to 2.2% [13, 14, 23]. When using fast absorbable sutures, the TSH incidence was up to 2.8% [7, 16]. No study directly compared slow absorbable and non-absorbable with fast absorbable sutures to reduce the incidence of TSH.
Trocar size
In the included studies (Table 1) the size of trocar was described in 13 studies (129 TSH) [7, 10, 11, 13, 14, 16, 18, 19, 21, 22, 24–26]. Only five of 129 (4%) TSH were from 5 mm trocars, whereas 118 (96%) originated from 10–12 mm trocars.
Trocar location
Summarising from the included studies (Table 1), a total of 82% of TSH were located at the umbilical port site, and 18% at other locations. The high frequency of TSH at the umbilical port site is supported by case reports from the early 1990s [31, 32] and is congruent with a survey from the American Association of Gynecologic Laparoscopists [33].
Procedure-specific incidence of trocar site hernias in adults
Laparoscopic cholecystectomy
In three studies, the incidence of TSH after laparoscopic cholecystectomy [11, 19, 21] was 0.2–5.2%. All studies were retrospective and included 765–9,542 patients. In only one study, that by Uslu et al. [19], were patients routinely examined for TSH after 1 month, revealing that 40 of 765 patients (5.2%) had a TSH, which is the highest reported incidence in this review. In a study from Romania [11] 18 of 9,542 (0.2%) patients had a TSH; however, there was no description of how the hernias were found. After 1,300 laparoscopic cholecystectomies in Pennsylvania, only ten patients (0.8%) were referred with a TSH. The studies did not describe how often the fascia was expanded to remove the gallbladder. Due to study heterogeneity, the data cannot be pooled.
Laparoscopic gastric bypass
Data from retrospective and prospective studies [16, 25, 26] comprised a total of 1,596 patients. The incidence of TSH in these studies ranged between 0.2 and 1.3%.
Other procedures
Five other specific laparoscopic procedures (ventral hernia repair, gastric banding, colectomy, fundoplication, and laparoscopic inguinal hernia repair) [7, 13–15, 17, 20, 26, 30], and six studies concerning more general procedures (general digestive, bariatric, gynaecologic and urologic oncology) [10, 12, 18, 22–24] are described in Table 1. Overall, the incidence of TSH was low, at levels ranging from 0 to 3.9% with follow-up periods of 1–65 months. Though some studies showed a high TSH incidence after specific procedures, other authors have reported the opposite [11, 12, 16, 17].
Patient-related risk factors
Gender and age
Female gender and high age may predispose to TSH after laparoscopic cholecystectomy [19, 34]. However, large prospective studies are needed to confirm these findings.
Children
In a study from Austria, all laparoscopic procedures in a single paediatric surgical unit during a 4-year period were analysed retrospectively [28]. Of the 293 patients included in the study, 53 were pre-school children with a mean age of 1.7 years (7 days–4.5 years). Of the 53 pre-school children (≤5 years), 3 (5.3%) had omental prolapse through a lateral port site without sutured fascias (trocar size 2–5 mm) 3–4 days after the primary laparoscopic operation (P = 0.006 compared with children >5 years). No long-term follow-up data were given in the paper. In another large retrospective study only 2 of 574 (0.3%) children (mean 6.7 years) had a TSH reported, both with an omental herniation through the umbilical port site [27]. The results from this study are difficult to interpret because the data, based on patient records, included large variations in laparoscopic procedures and patient co-morbidity. The follow-up was defined as the time between the laparoscopic procedure and the last clinical examination (range 1 week–45 months). No details of the patients who had a TSH were described.
Rescorla et al. [29] showed the incidence of TSH after 227 laparoscopic splenectomies to be 0.4% (1/227) in children with a mean age of 7.7 years. No further details were given regarding the TSH.
Obesity
As shown in Table 1, two large retrospective and one prospective study [16, 25, 26] (n = 459–849) found a incidence of TSH after bariatric surgery ranging from 0.3 to 1.25% with a mean follow-up of 1.5 years.
Diabetes mellitus and smoking
The literature does not suggest a relation between diabetes and incidence of TSH [4, 18, 21]. However, diabetes is correlated to an increased risk of wound infection [35], and wound infection in open surgery predisposes to the development of incisional hernia [36].
Smoking is a significant risk factor for incisional hernia after open abdominal surgery [37]. A retrospective study including 320 laparoscopic fundoplications [7] showed that four of the nine patients who developed TSH were smokers (>25 pack years), but smoking habits in patients not developing TSH were not reported.
Special trocars and protective mesh plugs
Johnson et al. [16] found a low incidence of TSH after using bladeless trocars (Versa Step™). The trocars were not used in the umbilical region where most TSH is seen.
Several authors advocate different devices to close the fascia in order to prevent TSH [16, 17, 38, 39], but all these studies were not randomised and had poor follow-up. A prophylactic bio-absorbable mesh plug to trocar sites of a minimum of 10 mm revealed no signs of recurrence or other complications to the procedure, but data was based on a case study of 17 patients with only 14 months follow up [40]. Protective mesh may have a future, but more data are needed before recommendations can be made.
Discussion
The present analysis suggests an overall incidence of a trocar site hernia below 1% with a substantially higher incidence when using trocars of ≥10 mm compared with smaller trocars. However, most studies were retrospective with poorly defined or short follow-up periods.
Almost half of the TSH occurred during the first month after laparoscopy. This could be explained by the fact that early onset hernias often present with symptoms from entrapment of bowel or omentum [41], and late onset TSH are often characterised by pain, nausea and discomfort [6] that might not lead to surgery. Since the large retrospective studies are based on the risk of TSH repair rather than objective examination, the true incidence of TSH may be higher than that reported in the literature. After laparotomy, the incidence of incisional hernias continues to appear after 10 years follow-up [42]. No such data are available after laparoscopy.
There were no valid data to support one entry technique over another in order to prevent TSH. When focussing on other trocar entry-related complications, a recent Cochrane review [43] concluded that no laparoscopic entry technique is at higher risk of inducing complications than others.
The literature has not systematically addressed the effect of suturing the trocar site fascia or not [6] but the present analysis supports suturing the fascia in trocar sites of 10 mm or above, especially in the umbilicus region [33]. Thus, it is recommended to use slowly- or non-absorbable suture to close the fascia in trocar sites ≥10 mm.
TSH is located mainly at the umbilical port site. This can be explained by the fact that most trocars used in the umbilicus are large, which in itself predisposes to TSH [10], or by non-recognised umbilical hernias before the laparoscopic procedure [21]. Theoretically, widening of the umbilical port in order to remove, for instance, a gallbladder also increases the incidence of TSH, but a retrospective study including 1,300 cholecystectomies found no correlation on this aspect [21]. During the last decade, case reports referring to TSH have concerned mostly lateral trocar sites [44, 45], which might simply reflect the fact that lateral port site hernias may also exhibit acute onset and lead to emergency operations.
The incidence of TSH in pre-school children is higher (5.3%) than the TSH incidence in juvenile patients, which is in the same range as for adult patients [27–29]. Several other studies and case reports from paediatric surgery have also described herniation through 3–5 mm ports [46] suggesting that trocar sites in young children should be sutured irrespective of trocar size.
The present review revealed the low incidence of TSH in patients undergoing bariatric laparoscopic surgery, with an incidence comparable with patients undergoing other laparoscopic procedures [16, 25, 26]. This is not in accordance with results from incisional hernia surgery after open gastric bypass [47], where morbidly obese patients had a 20% risk of incisional hernias versus 4% in normal weighted patients with ulcerative colitis after laparotomy [47]. In obese patients, the incidence of TSH may be underestimated since it can be difficult to diagnose a small hernia through a thick layer of subcutaneous tissue. Primary mesh reinforcement has been proposed to avoid TSH after bariatric surgery [48], but at present this is not supported by the literature.
Although the current literature shows a low incidence of TSH, we found no large-scale studies describing the proportions of patients having elective TSH repairs and acute surgery for incarcerated or strangulated bowel in a TSH. Such data are essential in order to recommend elective TSH repair to such patients.
Based on current evidence classification [49], we have listed some recommendations to prevent TSH based on the present literature search (Table 2). As shown, the evidence is poor and more studies are needed to confirm these suggestions. It may also be advisable to do a close preoperative examination to detect small umbilical hernias, and, if found, these small fascia defects can be used as access ports in laparoscopic surgery. Such a defect should be treated as an umbilical hernia, with closure of the defect either with non-absorbable suture or a mesh [50].
It would have been optimal to perform a meta-analysis. However, the included studies were very heterogenic, and TSH was not the principal end-point in the RCTs. Furthermore, many studies provided no technical information on the surgical procedure (i.e., trocar type and size, suture type etc.). Therefore, the present study was a qualitative systematic review rather than a meta-analysis.
In conclusion, the current evidence regarding risk factors for TSH is weak. Present data support the view that the larger the trocar, the higher the incidence of TSH, and that TSH is located primarily in the umbilicus area, where most large trocars are placed. The technology provides us with smaller laparoscopes, and in many different surgical procedures a 10 mm (or larger) trocar can be exchanged for a 5 mm port to reduce the incidence of TSH. Despite the poor evidence, the current review supports the use of as small entry ports as possible, and suturing all defects of minimum 10 mm with slow-absorbable or non-absorbable suture material. In pre-school children undergoing laparoscopic surgery, all port sites, regardless of size, should probably be sutured.
References
Andersen LP, Klein M, Gogenur I, Rosenberg J (2008) Incisional hernia after open versus laparoscopic sigmoid resection. Surg Endosc 22:2026–2029
Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96:851–858
Fear RE (1968) Laparoscopy: a valuable aid in gynecologic diagnosis. Obstet Gynecol 31:297–309
Boldo E, Perez de Lucia G, Aracil JP, Martin F, Escrig J, Martinez D, Miralles JM, Armelles A (2007) Trocar site hernia after laparoscopic ventral hernia repair. Surg Endosc 21:798–800
Munro MG (2002) Laparoscopic access: complications, technologies, and techniques. Curr Opin Obstet Gynecol 14:365–374
Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M (2004) Trocar site hernia. Arch Surg 139:1248–1256
Bowrey DJ, Blom D, Crookes PF, Bremner CG, Johansson JL, Lord RV, Hagen JA, DeMeester SR, DeMeester TR, Peters JH (2001) Risk factors and the prevalence of trocar site herniation after laparoscopic fundoplication. Surg Endosc 15:663–666
Hussain A, Mahmood H, Shuaib S, El-Hasani S (2008) Prevention of trocar site incisional hernia following laparoscopic ventral hernia repair. JSLS 12:206–209
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Coda A, Bossotti M, Ferri F, Mattio R, Ramellini G, Poma A, Quaglino F, Filippa C, Bona A (2000) Incisional hernia and fascial defect following laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 10:34–38
Duca S, Bala O, Al-Hajjar N, Lancu C, Puia I, Munteanu D, Graur F (2003) Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB (Oxford) 5:152
Bhoyrul S, Payne J, Steffes B, Swanstrom L, Way LW (2000) A randomized prospective study of radially expanding trocars in laparoscopic surgery. J Gastrointest Surg 4:392–397
Winslow ER, Fleshman JW, Birnbaum EH, Brunt LM (2002) Wound complications of laparoscopic vs open colectomy. Surg Endosc 16:1420–1425
Smith AI, Royston CM, Sedman PC (1999) Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. A prospective randomized trial. Surg Endosc 13:804–806
Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL (2007) The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: mid-term analysis of 400 cases. Surg Endosc 21:391–395
Johnson WH, Fecher AM, McMahon RL, Grant JP, Pryor AD (2006) VersaStep trocar hernia rate in unclosed fascial defects in bariatric patients. Surg Endosc 20:1584–1586
Leibl BJ, Schmedt CG, Schwarz J, Kraft K, Bittner R (1999) Laparoscopic surgery complications associated with trocar tip design: review of literature and own results. J Laparoendosc Adv Surg Tech A 9:135–140
Mayol J, Garcia-Aguilar J, Ortiz-Oshiro E, De-Diego Carmona JA, Fernandez-Represa JA (1997) Risks of the minimal access approach for laparoscopic surgery: multivariate analysis of morbidity related to umbilical trocar insertion. World J Surg 21:529–533
Uslu HY, Erkek AB, Cakmak A, Kepenekci I, Sozener U, Kocaay FA, Turkcapar AG, Kuterdem E (2007) Trocar site hernia after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A 17:600–603
Mahmoud Uslu HY, Ustuner EH, Sozener U, Ozis SE, Turkcapar AG (2007) Cannula site insertion technique prevents incisional hernia in laparoscopic fundoplication. Surg Laparosc Endosc Percutan Tech 17:267–270
Azurin DJ, Go LS, Arroyo LR, Kirkland ML (1995) Trocar site herniation following laparoscopic cholecystectomy and the significance of an incidental preexisting umbilical hernia. Am Surg 61:718–720
Chiong E, Hegarty PK, Davis JW, Kamat AM, Pisters LL, Matin SF (2010) Port-site hernias occurring after the use of bladeless radially expanding trocars. Urology 75:574–580
Hussain A, Mahmood H, Singhal T, Balakrishnan S, Nicholls J, El-Hasani S (2009) Long-term study of port-site incisional hernia after laparoscopic procedures. JSLS 13:346–349
Nezhat C, Nezhat F, Seidman DS (1997) Incisional hernias after operative laparoscopy. J Laparoendosc Adv Surg Tech A 7:111–115
Rosenthal RJ, Szomstein S, Kennedy CI, Zundel N (2007) Direct visual insertion of primary trocar and avoidance of fascial closure with laparoscopic Roux-en-Y gastric bypass. Surg Endosc 21:124–128
Susmallian S, Ezri T, Charuzi I (2002) Laparoscopic repair of access port site hernia after lap-band system implantation. Obes Surg 12:682–684
Chen MK, Schropp KP, Lobe TE (1996) Complications of minimal-access surgery in children. J Pediatr Surg 31:1161–1165
Paya K, Wurm J, Fakhari M, Felder-Puig R, Puig S (2008) Trocar-site hernia as a typical postoperative complication of minimally invasive surgery among preschool children. Surg Endosc 22:2724–2727
Rescorla FJ, West KW, Engum SA, Grosfeld JL (2007) Laparoscopic splenic procedures in children: experience in 231 children. Ann Surg 246:683–687
Taylor GW, Jayne DG, Brown SR, Thorpe H, Brown JM, Dewberry SC, Parker MC, Guillou PJ (2010) Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. Br J Surg 97:70–78
Hass BE, Schrager RE (1993) Small bowel obstruction due to Richter’s hernia after laparoscopic procedures. J Laparoendosc Surg 3:421–423
Horgan PG, O’Connell PR (1993) Subumbilical hernia following laparoscopic cholecystectomy. Br J Surg 80:1595
Montz FJ, Holschneider CH, Munro MG (1994) Incisional hernia following laparoscopy: a survey of the American association of gynecologic laparoscopists. Obstet Gynecol 84:881–884
Chang WT, Yu FJ, Hsieh MY, Huang MC, Lee KT, Chen JS, Kuo KK, Chuang SC, Wang SR, Ker CG (2009) Laparoscopic cholecystectomy in aged patients. Hepatogastroenterology 56:950–955
Neumayer L, Hosokawa P, Itani K, El-Tamer M, Henderson WG, Khuri SF (2007) Multivariable predictors of postoperative surgical site infection after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg 204:1178–1187
Millbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059
Sorensen LT, Hemmingsen UB, Kirkeby LT, Kallehave F, Jorgensen LN (2005) Smoking is a risk factor for incisional hernia. Arch Surg 140:119–123
Calik A, Yucel Y, Topaloglu S, Hos G, Aktas A, Piskin B (2008) Umbilical trocar site closure with Berci’s needle after laparoscopic cholecystectomy. Hepatogastroenterology 55:1958–1961
Di Lorenzo N, Coscarella G, Lirosi F, Gaspari A (2002) Port-site closure: a new problem, an old device. JSLS 6:181–183
Moreno-Sanz C, Picazo-Yeste JS, Manzanera-Diaz M, Herrero-Bogajo ML, Cortina-Oliva J, Tadeo-Ruiz G (2008) Prevention of trocar site hernias: description of the safe port plug technique and preliminary results. Surg Innov 15:100–104
Losanoff JE, Richman BW, Jones JW (2003) Trocar-site hernia complicated by necrotizing fasciitis–case report and review of the literature. Hernia 7:220–223
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Ahmad G, Duffy JM, Phillips K, Watson A (2008) Laparoscopic entry techniques. Cochrane Database Syst Rev CD006583
Kouba EJ, Hubbard JS, Wallen E, Pruthi RS (2006) Incisional hernia in a 12-mm nonbladed trocar site following laparoscopic nephrectomy. ScientificWorldJournal 6:2399–2402
Lowry PS, Moon TD, D’Alessandro A, Nakada SY (2003) Symptomatic port-site hernia associated with a non-bladed trocar after laparoscopic live-donor nephrectomy. J Endourol 17:493–494
Yee DS, Duel BP (2006) Omental herniation through a 3-mm umbilical trocar site. J Endourol 20:133–134
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171:80–84
Sanchez-Pernaute A, Perez-Aguirre E, Garcia Botella A, Rodriguez L, Antona EM, Cabeza J, Valladolid DJ, Rubio MA, Delgado I, Torres A (2008) Prophylactic closure of trocar orifices with an intraperitoneal mesh (ventralex) in laparoscopic bariatric surgery. Obes Surg 18:1489–1491
Eccles M, Freemantle N, Mason J (1998) North of England evidence based guidelines development project: methods of developing guidelines for efficient drug use in primary care. BMJ 316:1232–1235
Helgstrand F, Rosenberg J, Jorgensen LN, Bay-Nielsen M, Friis-Andersen H, Wara P, Kehlet H, Bisgaard T (2010) Surgical treatment of ventral hernia. Ugeskr Laeger 172:1987–1989
Acknowledgments
This study was funded by the foundation for Health Research in Region Zealand, Denmark.
Conflict of interest
F.H. received support from Baxter Healthcare A/S. J.R. has received research grants regarding laparoscopic surgery from Johnson & Johnson, Covidien, and Baxter Healthcare A/S, and had travel/accommodations expenses for international meetings covered or reimbursed from Johnson & Johnson, and Baxter Healthcare A/S. T.B. has received support from Johnson & Johnson, Covidien, and Baxter Healthcare A/S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Helgstrand, F., Rosenberg, J. & Bisgaard, T. Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia 15, 113–121 (2011). https://doi.org/10.1007/s10029-010-0757-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0757-x