Abstract
Background: Since the laparoscopic treatment of incisional hernia developed in the beginning of the 1990s, several studies and meta-analyses were performed to compare to the outcome of open repair. Despite the results seem to favor the laparoscopic approach, most of the meta-analysis failed to differ between ventral, incisional, and umbilical hernia.
Methods: Up to now, only two published meta-analyses focused selectively on the comparison of incisional hernias in open and laparoscopic repair. Additional to the results of these meta-analyses, the data of Herniamed registry were included in this chapter to merge the analysis of clinical studies and the daily practice for representing the genuine rate of complication rates in open and laparoscopic incisional hernia repair.
Results: In the meta-analysis except the significant less wound infection rate in the laparoscopic group, no differences concerning intra- and postoperative complications, as well as recurrence rates, were seen. In addition to the meta-analysis, the data of Herniamed registry confirmed these results.
Conclusion: Thus there seem no major differences in complications and outcome comparing open and laparoscopic repair in incisional hernias; the selective tailoring in each case is the crucial part of decision before surgery. Beyond that new upcoming techniques combine the advantages of laparo−/endoscopic approach with retromuscular mesh position of the classical open sublay repair and the minimally invasive approach leading to promising results in patients’ outcome.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Hernia
- Incisional
- Abdominal wall
- Surgery
- Hernia surgery
- Laparoscopic hernia repair
- Outcome
- Complication
- Pain
1 Introduction
Even though the laparoscopic approach to general surgery started in the early 1990s to minimize trauma to the abdominal wall and pain, we have to consider that actually today a high percentage of surgery is still done in an open approach. The risk of development of incisional hernia, especially after midline laparotomies, is found to be up to 44% in the literature. Though new techniques for closure of the midline like the “small bite technique” seem very promising [1, 2], the percentage of incisional hernias after 1-year follow-up with 21% are quite high. After 2 years of surgery, the rate of incisional hernia is only about 50% and 75% within 3 years. Not surprisingly, the increase of the hernia incidence from 1 year to 3 years of follow-up is about 60% [3].
The complications associated with incisional hernias are most likely chronic pain and discomfort but can lead also to incarceration and life-threatening strangulation.
Whereas all laparoscopic incisional hernia repairs are performed with the use of a mesh mostly in a bridging technique, predominantly the mesh provides a reinforcement of the direct closure of the defect in open repair. Mesh-associated complication like infections, shrinkage, and pain as well as complications due to mesh fixation and finally the recurrence rate have to be analyzed and compared to the different techniques of open and laparoscopic approach especially in terms of the long-term results.
2 Material
To address the current issues of complications in open and laparoscopic incisional hernia repair, two meta-analyses [4, 5] focusing the comparison of the outcome in both techniques based on RCTs and data of the Herniamed registry were analyzed in this chapter. The aim of merging the analysis of clinical studies and the daily practice was to represent the genuine rate of complication rates in open and laparoscopic incisional hernia repair. The analysis of the different variables of outcome mainly focused on the intra- and postoperative complications, as well as chronic pain and recurrence.
3 Results
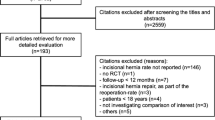
In the meta-analysis of Awaiz et al. [4], six RCTs comparing laparoscopic versus open mesh repair for elective incisional hernia were included [6,7,8,9,10,11].
The overall complication rate in the laparoscopic group (LG) was 38.9% compared to 41.53% in the open group (OG) without any significant difference (OR 1.07, 95% CI 0.33, 3.42, p = 0.91). Concerning the bowel complication, a significant less percentage was found in OG with 2.11% compared to 5.89% in the LG (OR 2.56, 95% CI 1.15, 5.72, p = 0.02). The infection rate of 2.41% detected in the LG a significant lower percentage compared to 12.16% in the OG (OR 0.21, 95% CI 0.07, 0.64, p = 0.01), which was corrected after a comment by Jensen et al. [12] in the final analysis of Awaiz et al. [13].
The incidence of wound hematoma or seroma with 15.28% in the LG versus 12.69% in the OG (OR 1.54, 95% CI 0.58, 4.09, p = 0.38), as well as the reoperation rate with 0.48% in the LG versus 3.41% in the OG (OR 0.32, 95% CI 0.07, 1.43, p = 0.14), was analyzed without any significant difference (Table 64.1). Regarding the variables of length of hospital stay (SMD −0.83, 95% CI −2.22, 0.56, p = 0.24) and time back to work (SMD −3.14, 95% CI −8.92, 2.64, p = 0.29), also no significant differences were found (Table 64.2). The analysis of postoperative pain obtained no significant difference between both groups (OR 1.41, 95% CI 0.81, 2.46, p = 0.23). Finally also rate of recurrence in the LG with 8.74% compared to 6.92% of OG was without any significance (OR 1.41, 95% CI 0.81, 2.46, p = 0.23) (Table 64.1).
In summary, the results of the analysis of both techniques seem to be comparable in terms of complication rates except wound infection, which was in favor of the laparoscopic repair.
Albeit the results of this review seem to reflect the evidence, some basic limitation has to be taken into account. For most of the outcomes in the included studies except for bowel complications, recurrence rate, reoperation, and neuralgia, a high degree of heterogeneity has to be considered.
Another meta-analysis published by Al Chalabi et al. [14] included four RCTs comparing open versus laparoscopic repair of incisional hernias [8,9,10,11] and one RCT [5] with ventral hernias. A total number of 611 patients, 306 patients in the laparoscopic group and 305 patients in the open repair group, were enrolled in the final analysis. The range of follow-up in the studies was from 2 months to 35 months. The recurrence rate was similar (p = 0.30), wound infection was higher in the open repair group (p < 0.001), length of hospital stay was not statistically different (p = 0.92), and finally the operation time was longer in the laparoscopic group but did not reach statistical significance. The drawback of this systematic review may be the inclusion of one study in ventral hernias (Pring et al.; [5]), which could bias the results of the meta-analysis due to the fact of crucial difference in the results of repair in primary and incisional hernias.
In the Herniamed registry, which was founded in 2009 by Köckerling [15], 47,580 data of incisional hernia repairs out of 417,147 hernia cases enrolled between 01 September 2009 and 24 April 2017 were analyzed concerning the different methods of repair as well as associated complications.
The distribution of the different repair techniques is shown in Table 64.3. The highest percentage of operation method was found in the sublay mesh repair with 10.5% followed by laparoscopic IPOM (29.9%), open IPOM (13.7%), suture repair (10.5%), and component separation (2.1%). Regarding the operation time, the suture repair was the fastest (49 min) and the component separation the longest (143 min). The median time for the laparoscopic IPOM with 78 min was nearly the same as for the onlay repair (80 min) and the open IPOM (84 min) compared to the sublay mesh repair lasting 99 min. The median hospital stay for open IPOM, sublay, and onlay was 8 days whereas 21 days for the component separation.
The intraoperative complication rate ranged between 1% and 3% (onlay 1.5%, sublay 1.6%, suture 2.2%, open IPOM 2.4%, laparoscopic IPOM 2.7%, CS 2.8%).
The postoperative rate of complication on the contrary differed significantly between the different procedures. The lowest rates were found after suture repair and laparoscopic IPOM with 4.8% and 4.3%, respectively, whereas 9.8% and 11.4% after onlay and sublay were detected. After component separation, the highest rate of 23.4% was described.
Similar distribution of the reoperation rates due to complications was seen: 2% in the group after suture repair and laparoscopic IPOM followed by open IPOM (4.3%), onlay (4.4%), and sublay (5.3%). Again the component separation was found to be associated with the highest reoperation rate (13.3%).
Following the reviews of Awaiz [4] and Al Chalabi [14], the comparison of open sublay versus laparoscopic IPOM was also analyzed for the data of Herniamed registry.
Looking at the size of defect (W1, W2, and W3, EHS classification) comparing laparoscopic IPOM and open sublay, the distribution is quite different, 38%, 49%, and 13% versus 25%,54%, and 21%, respectively (Table 64.4). The interpretation of these analyses detects the tailored approach concerning the chosen procedure in association with the defect size. Therefore, the results have to be seen very carefully and can be valued only in case of multivariable analysis or after propensity score matching.
The rate of wound infection in laparoscopic IPOM with 1.9% was significantly lower in comparison to the sublay with 4.7%. These results confirm the analysis of the reviews [4, 14]. Chronic pain and pain at rest or during exercise after 1 year of follow-up are without any difference between laparoscopic IPOM and sublay. The recurrence rate after laparoscopic IPOM after 1 year was 7.2% and after sublay 7.8% (Table 64.4).
4 Conclusions
In summary, the analysis of Herniamed registry data confirms the results of the reviews of Awaiz [4, 13] and Al Chalabi [14] in terms of the higher risk of wound complications in open repair of incisional hernias compared to the laparoscopic technique. Furthermore, the analysis of the registry data detected lower rates of overall complications and reoperations in favor of the laparoscopic method. Since the tailoring of the surgical method in association with the size of the defect in the registry data could be seen, obviously, the members of the Herniamed registry are following the guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias of the International Endoscopic Hernia Society (IEHS) [15,16,18] in terms of limitation for laparoscopic repair up to a defect size of 8–10 cm. With respect to the defect size, the laparoscopic IPOM repair seems to obtain excellent results.
5 Discussion
The laparoscopic technique of repair of ventral and incisional hernia first described by Le Blanc developed not only in terms of technical equipment but also in mesh technologies. The everlasting discussion of the size of mesh overlap started with the first recommendation of Le Blanc in 2003 [19] and leads to the recent published review by Le Blanc [20]. In this review, an analysis was performed to determine the relationship between hernia recurrence rate and area of mesh overlap in open and laparoscopic repair including 45 prospective studies and 50 retrospective studies, enrolling 8864 patients in total. In laparoscopic procedures, the pooled estimation of risk for each group based on the extent of mesh overlap obtained incidence rates of 8.6%, 4.6%, and 1.4% for <3, 3–5, and >5 cm mesh overlap, respectively, whereas in open repair, no trend between hernia recurrence rate and mesh overlap could be seen (6.5%, 7.0%, and 6.0% for <3, 3–5, and >5 cm mesh overlap). These results reflect the importance of mesh overlap in laparoscopic repair especially in respect of the bridging technique.
According to the recommendation of the IEHS guidelines, “the mesh used for laparoscopic repair of a ventral hernia should overlap the hernia defect by at least 3 to 4 cm in all directions” (Grade B—Level of Evidence) and “a large overlap of the defect by mesh is necessary, with a minimum of 5 cm if the mesh is fixed without transfascial sutures. A larger overlap is recommended for larger hernias than the overlap used for small hernias” (Grade C). Another main issue of recurrence in the repair of incisional hernia is the relationship between mesh and fixation. In the guidelines of the IEHS [16], the recommendations are stated: “Suture fixation alone or a combination with tacks should be performed” (Grade B) and “The tacks-only fixation can be considered the technique of choice, taking into account the increased risk of postoperative pain due to the number of devices and the need for an additional overlap of mesh (at least 5 cm) to prevent recurrence caused by shrinkage” (Grade C). All these recommendations are predominantly based on the studies of Le Blanc [19] and could be extended to the results of the experimental studies of Kallinowsky et al. [21, 22], which revealed a direct association of mesh-type, overlap, and fixation according to the defect size.
Berler et al. [23] published an overview of new technologies of fixation models like pushpins, screws, or barbs associated with different mechanisms of fixation aiming the prevention of mesh migration and at the end a potential recurrence. The trend of minimizing the trauma of fixation, as already seen in the laparo−/endoscopic repair in inguinal hernias, seems to follow the use of glue and self-adhering meshes to achieve less chronic pain and better long-term outcome.
Another discussion is arising by the implementation of new laparo−/endoscopic techniques with the purpose to place the mesh in a retromuscular position to prevent any kind of complication associated with mesh or fixation. The mini/less open sublay (MILOS) and endoscopic MILOS (eMILOS) technique developed by Reinpold and Bittner et al. [24], endoscopic-assisted linea alba reconstruction (ELAR) by Köckerling [25, 26], stapled Rives-Stoppa by Costa et al. and Moore et al. [27, 28], and finally robotic approaches by Carbonell et al. [29] provide the advantages of minimally invasive approach in combination with the safest place of mesh implantation.
The reports of these brand-new hybrid techniques are very promising, but have to be proved in the long-term results.
Including all the developments and progress in incisional hernia repair, the old two main opposing techniques of open and laparoscopic repair will be replaced by tailoring each incisional hernia case with the best available technique including all new operation methods.
References
Millbourn D, Cengiz Y, Israelsson LA. Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg. 2009;144(11):1056–9. https://doi.org/10.1001/archsurg.2009.189. PubMed PMID: 19917943
Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J, Wijnhoven BP, Schouten WR, Cense HA, Stockmann HB, Berends FJ, Dijkhuizen FP, Dwarkasing RS, Jairam AP, van Ramshorst GH, Kleinrensink GJ, Jeekel J, Lange JF. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet. 2015;386(10000):1254–60. https://doi.org/10.1016/S0140-6736(15)60459-7. Epub 2015 Jul 15. PubMed PMID: 26188742.
Fink C, Baumann P, Wente MN, Knebel P, Bruckner T, Ulrich A, et al. Incisional hernia rate 3 years after midline laparotomy. Br J Surg. 2014;101:51–4. https://doi.org/10.1002/bjs.9364.
Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, Memon MA. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia. 2015;19(3):449–63. https://doi.org/10.1007/s10029-015-1351-z. Epub 2015 Feb 4. Review. PubMed PMID: 25650284
Pring CM, Tran V, O’Rourke N, Martin IJ. Laparoscopic versus open ventral hernia repair: a randomized controlled trial. ANZ J Surg. 2008;78(10):903–6. https://doi.org/10.1111/j.1445-2197.2008.04689.x. PubMed PMID: 18959646
Olmi S, Scaini A, Cesana GC, Erba L, Croce E. Laparoscopic versus open incisional hernia repair: an open randomized controlled study. Surg Endosc. 2007;21:555–9.
Navarra G, Musolino C, De Marco ML, Bartolotta M, Barbera A, Centorrino T. Retromuscular sutured incisional hernia repair: a randomized controlled trial to compare open and laparoscopic approach. Surg Laparosc Endosc Percutan Tech. 2007;17:86–90.
Asencio F, Aguilo´ J, Peiro´ S, Carbo´ J, Ferri R, Caro F, Ahmad M. Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc. 2009;23:1441–8.
Itani KM, Hur K, Kim LT, Anthony T, Berger DH, Reda D, Neumayer L. Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Arch Surg. 2010;145:322–8.
Eker HH, Hansson BM, Buunen M, Janssen IM, Pierik RE, Hop WC, Bonjer HJ, Jeekel J, Lange JF. Laparoscopic vs. open incisional hernia repair: a randomized clinical trial. JAMA Surg. 2013;13:259–63.
Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D, Smedberg S, Osterberg J, Montgomery A. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the Pro LOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. 2013;258:37–45.
Jensen KK, Jorgensen LN. Comment to: Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Awaiz A et al. Hernia 2015;19:449–463. Hernia. 2015;19(6):1025–6. https://doi.org/10.1007/s10029-015-1412-3. Epub 2015 Aug 4. PubMed PMID: 26238399
Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, Memon MA. Reply to comment to Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Jensen K, Jorgensen LN. Hernia. 2015;19(6):1027–9. https://doi.org/10.1007/s10029-015-1432-z. Epub 2015 Oct 26. PubMed PMID: 26496998
Al Chalabi H, Larkin J, Mehigan B, McCormick P. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg. 2015;20:65–74. https://doi.org/10.1016/j.ijsu.2015.05.050. Epub 2015 Jun 12. Review. PubMed PMID: 26074289
Köckerling F, Schug-Pass C, Adolf D, Reinpold W, Stechemesser B. Is pooled data analysis of ventral and incisional hernia repair acceptable? Front Surg. 2015;2:15. https://doi.org/10.3389/fsurg.2015.00015.
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F, Kukleta J, Leblanc K, Lomanto D, Misra MC, Bansal VK, Morales-Conde S, Ramshaw B, Reinpold W, Rim S, Rohr M, Schrittwieser R, Simon T, Smietanski M, Stechemesser B, Timoney M, Chowbey P, International Endohernia Society (IEHS). Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-part 1. Surg Endosc. 2014;28(1):2–29. https://doi.org/10.1007/s00464-013-3170-6. Epub 2013 Oct 11. PubMed PMID: 24114513; PubMed Central PMCID: PMC3872300
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F, Kukleta J, LeBlanc K, Lomanto D, Misra MC, Morales-Conde S, Ramshaw B, Reinpold W, Rim W, Rohr M, Schrittwieser R, Simon T, Smietanski M, Stechemesser B, Timoney M, Chowbey P. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias International Endohernia Society [IEHS]—part 2. Surg Endosc. 2014;28:353–79. https://doi.org/10.1007/s00464-013-3171-5.
Bittner R, Bingener-Casey J, Dietz U, Fabian G, Fortelny RH, Köckerling F, Kukleta J, LeBlanc K, Lomanto D, Misra M, Morales-Conde S, Ramshaw B, Reinpold W, Rim S, Rohr M, Schrittwieser R, Simon T, Smietanski M, Stechemesser B, Timoney M, Chowbey P. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS]) Part III. Surg Endosc. 2014;28:380–404. https://doi.org/10.1007/s00464-013-3172-4.
LeBlanc KA, Whitaker JM, Bellanger DE, Rhynes VK. Laparoscopic incisional and ventral hernioplasty: lessons learned from 200 patients. Hernia. 2003;7(3):118–24. https://doi.org/10.1007/s10029-003-0117-1.
LeBlanc K. Proper mesh overlap is a key determinant in hernia recurrence following laparoscopic ventral and incisional hernia repair. Hernia. 2016;20(1):85–99. https://doi.org/10.1007/s10029-015-1399-9. Epub 2015 Jul 5. Review. PubMed PMID: 26143072
Kallinowski F, Baumann E, Harder F, Siassi M, Mahn A, Vollmer M, Morlock MM. Dynamic intermittent strain can rapidly impair ventral hernia repair. J Biomech. 2015;48(15):4026–36. https://doi.org/10.1016/j.jbiomech.2015.09.045. Epub 2015 Oct 8. PubMed PMID: 26476761
Kallinowski F, Harder F, Silva TG, Mahn A, Vollmer M. Bridging with reduced overlap: fixation and peritoneal grip can prevent slippage of DIS class A meshes. Hernia. 2017. https://doi.org/10.1007/s10029-017-1583-1. [Epub ahead of print] PubMed PMID: 28132109
Berler DJ, Cook T, LeBlanc K, Jacob BP. Next generation mesh fixation technology for hernia repair. Surg Technol Int. 2016;XXIX:109–17. PubMed PMID: 27466869
Schwarz J, Reinpold W, Bittner R. Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbeck's Arch Surg. 2017;402(1):173–80. https://doi.org/10.1007/s00423-016-1522-0. Epub 2016 Oct 20. PubMed PMID: 27766419
Köckerling F, Botsinis MD, Rohde C, Reinpold W, Schug-Pass C. Endoscopic-assisted linea alba reconstruction: new technique for treatment of symptomatic umbilical, trocar, and/or epigastric hernias with concomitant rectus abdominis diastasis. Eur Surg. 2017;49(2):71–5. https://doi.org/10.1007/s10353-017-0473-1. Epub 2017 Mar 10. PubMed PMID: 28408920; PubMed Central PMCID: PMC5368206
Köckerling F, Botsinis MD, Rohde C, Reinpold W. Endoscopic-assisted linea alba reconstruction plus mesh augmentation for treatment of umbilical and/or epigastric hernias and rectus abdominis diastasis—early results. Front Surg. 2016;3:27. https://doi.org/10.3389/fsurg.2016.00027. eCollection 2016. PubMed PMID: 27243016; PubMed Central PMCID: PMC4865488
Costa TN, Abdalla RZ, Santo MA, Tavares RR, Abdalla BM, Cecconello I. Transabdominal midline reconstruction by minimally invasive surgery: technique and results. Hernia. 2016;20(2):257–65. https://doi.org/10.1007/s10029-016-1457-y. Epub 2016 Jan 22. PubMed PMID: 26801185
Moore AM, Anderson LN, Chen DC. Laparoscopic stapled sublay repair with self-gripping mesh: a simplified technique for minimally invasive extraperitoneal ventral hernia repair. Surg Technol Int. 2016;XXIX:131–9. PubMed PMID: 27728955
Carbonell AM, Warren JA, Prabhu AS, Ballecer CD, Janczyk RJ, Herrera J, Huang LC, Phillips S, Rosen MJ, Poulose BK. Reducing length of stay using a robotic-assisted approach for retromuscular ventral hernia repair: a comparative analysis from the Americas Hernia Society Quality Collaborative. Ann Surg. 2018;267:210–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Herniamed Study Group
Herniamed Study Group
1.1 Scientific Board
Köckerling, Ferdinand (Chairman) (Berlin); Bittner, Reinhard (Rottenburg); Fortelny, René (Wien); Jacob, Dietmar (Berlin); Koch, Andreas (Cottbus); Kraft, Barbara (Stuttgart); Kuthe, Andreas (Hannover); Lammers, Bernhard (Neuss); Lippert, Hans (Magdeburg): Lorenz, Ralph (Berlin); Mayer, Franz (Salzburg); Niebuhr, Henning (Hamburg); Peiper, Christian (Hamm); Pross, Matthias (Berlin); Reinpold, Wolfgang (Hamburg); Simon, Thomas (Weinheim); Stechemesser, Bernd (Köln); Unger, Solveig (Chemnitz), Weyhe, Dirk (Oldenburg); Zarras, Konstantinos (Düsseldorf)
1.2 Members
Ahmetov, Azat (Saint-Petersburg); Alapatt, Terence Francis (Frankfurt/Main); Albayrak, Nurretin (Herne); Amann, Stefan (Neuendettelsau); Anders, Stefan (Berlin); Anderson, Jürina (Würzburg); Antoine, Dirk (Leverkusen); Apfelstedt, Heinrich (Solingen); Arndt, Anatoli (Elmshorn); Aschenbrenner, Michael (Spittal/Drau); Asperger, Walter (Halle); Avram, Iulian (Saarbrücken); Baikoglu-Endres, Corc (Weißenburg i. Bay.); Bandowsky, Boris (Damme); Barkus; Jörg (Velbert); Becker, Matthias (Freital); Behrend, Matthias (Deggendorf); Berkhoff, Christian (Fulda); Beuleke, Andrea (Burgwedel); Birk, Dieter (Bietigheim-Bissingen); Bittner, Reinhard (Rottenburg); Blaha, Pavel (Zwiesel); Blumberg, Claus (Lübeck); Böckmann, Ulrich (Papenburg); Böhle, Arnd Steffen (Bremen); Bolle, Ludger (Berlin); Borchert, Erika (Grevenbroich); Born, Henry (Leipzig); Brabender, Jan (Köln); Breitenbuch von, Philipp (Radebeul); Brož, Miroslav (Ebersbach); Brückner, Torsten (Gießen); Brütting, Alfred (Erlangen); Buchert, Annette (Mallersdorf-Pfaffenberg; Buchholz, Torsten (Aurich); Budzier, Eckhard (Meldorf); Burchett, Bert (Teterow); Burghardt, Jens (Rüdersdorf); Cejnar, Stephan-Alexander (München); Chirikov, Ruslan (Dorsten); Claußnitzer, Christian (Ulm); Comman, Andreas (Bogen); Crescenti, Fabio (Verden/Aller); Daniels, Thies (Hamburg); Dapunt, Emanuela (Bruneck); Decker, Georg (Berlin); Demmel, Michael (Arnsberg); Descloux, Alexandre (Baden); Deusch, Klaus-Peter (Wiesbaden); Dick, Marcus (Neumünster); Dieterich, Klaus (Ditzingen); Dietz, Harald (Landshut); Dittmann, Michael (Northeim); Drummer, Bernhard (Forchheim); Eckermann, Oliver (Luckenwalde); Eckhoff, Jörn/Hamburg); Ehmann, Frank (Grünstadt); Eisenkrein, Alexander (Düren); Elger, Karlheinz (Germersheim); Engelhardt, Thomas (Erfurt); Erichsen, Axel (Friedrichshafen); Eucker, Dietmar (Bruderholz); Fackeldey, Volker (Kitzingen); Faddah, Yousif (Kamenz); Farke, Stefan (Delmenhorst); Faust, Hendrik (Emden); Federmann, Georg (Seehausen); Fiedler, Michael (Eisenberg); Fikatas, Panagiotis (Berlin); Firl, Michaela (Perleberg); Fischer, Ines (Wiener Neustadt); Fleischer, Sabine (Dinslaken); Fortelny, René H. (Wien); Franczak, Andreas (Wien); Franke, Claus (Düsseldorf); Frankenberg von, Moritz (Salem); Frehner, Wolfgang (Ottobeuren); Friedhoff, Klaus (Andernach); Friedrich, Jürgen (Essen); Frings, Wolfram (Bonn); Fritsche, Ralf (Darmstadt); Frommhold, Klaus (Coesfeld); Frunder, Albrecht (Tübingen); Fuhrer, Günther (Reutlingen); Garlipp, Ulrich (Bitterfeld-Wolfen); Gassler, Harald (Villach); Gawad, Karim A. Frankfurt/Main); Gehrig, Tobias (Sinsheim); Gerdes, Martin (Ostercappeln); Germanov, German (Halberstadt; Gilg, Kai-Uwe (Hartmannsdorf); Glaubitz, Martin (Neumünster); Glauner-Goldschmidt, Kerstin (Werne); Glutig, Holger (Meissen); Gmeiner, Dietmar (Bad Dürrnberg); Göring, Herbert (München); Grebe, Werner (Rheda-Wiedenbrück); Grothe, Dirk (Melle); Günther, Thomas (Dresden); Gürtler, Thomas (Zürich); Hache, Helmer (Löbau); Hämmerle, Alexander (Bad Pyrmont); Haffner, Eugen (Hamm); Hain, Hans-Jürgen (Gross-Umstadt); Halter, Christian Jörn (Recklinghausen); Hammans, Sebastian (Lingen); Hampe, Carsten (Garbsen); Hanke, Stefan (Halle); Harrer, Petra (Starnberg); Hartung, Peter (Werne); Heinzmann, Bernd (Magdeburg); Heise, Joachim Wilfried (Stolberg); Heitland, Tim (München); Helbling, Christian (Uznach/Schweiz); Hellinger, Achim (Fulda); Hempen, Hans-Günther (Cloppenburg); Henneking, Klaus-Wilhelm (Bayreuth); Hennes, Norbert (Duisburg); Herdter, Christian (Gelsenkirchen); Hermes, Wolfgang (Weyhe); Herzing, Holger Höchstadt); Hessler, Christian (Bingen); Heuer, Matthias (Herten); Hildebrand, Christiaan (Langenfeld); Höferlin, Andreas (Mainz); Hoffmann, Henry (Basel); Hoffmann, Michael (Kassel); Hofmann, Eva M. (Frankfurt/Main); Horbach, Thomas (Fürth); Hornung, Frederic (Wolfratshausen); Hudak, Attila (Suhl); Hübel-Abe, Jan (Ilmenau; Hügel, Omar (Hannover); Hüttemann, Martin (Oberhausen); Hüttenhain, Thomas (Mosbach); Hunkeler, Rolf (Zürich); Imdahl, Andreas (Heidenheim); Iseke, Udo (Duderstadt); Isemer, Friedrich-Eckart (Wiesbaden); Jablonski, Herbert Gustav (Sögel); Jacob, Dietmar (Berlin); Jansen-Winkeln, Boris (Leipig); Jantschulev, Methodi (Waren); Jenert, Burghard (Lichtenstein); Jugenheimer, Michael (Herrenberg); Junge, Karsten (Aachen); Kaaden, Stephan (Neustadt am Rübenberge); Käs, Stephan (Weiden); Kahraman, Orhan (Hamburg); Kaiser, Christian (Westerstede); Kaiser, Gernot Maximilian (Kamp-Lintfort); Kaiser, Stefan (Kleinmachnow); Karch, Matthias (Eichstätt); Kasparek, Michael S. (München); Kastl, Sigrid (Braunau am Inn); Keck, Heinrich (Wolfenbüttel); Keller, Hans W. (Bonn); Kewer, Jans Ludolf (Tuttlingen); Kienzle, Ulrich (Karlsruhe); Kipfmüller, Brigitte (Köthen); Kirsch, Ulrike (Oranienburg); Klammer, Frank (Ahlen); Klatt, Richard (Hagen); Klein, Karl-Hermann (Burbach); Kleist, Sven (Berlin); Klobusicky, Pavol (Bad Kissingen); Kneifel, Thomas (Datteln); Knolle, Winfried (Pritzwalk); Knoop, Michael (Frankfurt/Oder); Knotter, Bianca (Mannheim); Koch, Andreas (Cottbus); Koch, Andreas (Münster); Köckerling, Ferdinand (Berlin); Köhler, Gernot (Linz); König, Oliver (Buchholz); Kornblum, Hans (Tübingen); Krämer, Dirk (Bad Zwischenahn); Kraft, Barbara (Stuttgart); Kratsch, Barthel (Dierdorf/Selters); Krausbeck, Matthias (Schwerin); Kreissl, Peter (Ebersberg); Krones, Carsten Johannes (Aachen); Kronhardt, Heinrich (Neustadt am Rübenberge); Kruse, Christinan (Aschaffenburg); Kube, Rainer (Cottbus); Kühlberg, Thomas (Berlin); Kühn, Gert (Freiberg); Kuhn, Roger (Gifhorn); Kusch, Eduard (Gütersloh); Kuthe, Andreas (Hannover); Ladberg, Ralf (Bremen); Ladra, Jürgen (Düren); Lahr-Eigen, Rolf (Potsdam); Lainka, Martin (Wattenscheid); Lalla, Thomas (Oschersleben); Lammers, Bernhard J. (Neuss); Lancee, Steffen (Alsfeld); Lange, Claas (Berlin); Langer, Claus (Göttingen); Laps, Rainer (Ehringshausen); Larusson, Hannes Jon (Pinneberg); Lauschke, Holger (Duisburg); Lechner-Puschnig, Marina (Klagenfurt am Wörthersee/Österreich); Leher, Markus (Schärding); Leidl, Stefan (Waidhofen/Ybbs); Leisten, Edith (Köln); Lenz, Stefan (Berlin); Liedke, Marc Olaf (Heide); Lienert, Mark (Duisburg); Limberger, Andreas (Schrobenhausen); Limmer, Stefan (Würzburg); Locher, Martin (Kiel); Loghmanieh, Siawasch (Viersen); Lorenz, Ralph (Berlin); Luedtke, Clinton (Kusel); Luther, Stefan (Wipperfürth); Luyken, Walter (Sulzbach-Rosenberg); Mallmann, Bernhard (Krefeld); Manger, Regina (Schwabmünchen); Maurer, Stephan (Münster); May, Jens Peter (Schönebeck); Mayer, Franz (Salzburg); Mayer, Jens (Schwäbisch Gmünd); Mellert, Joachim (Höxter); Menzel, Ingo (Weimar); Meurer, Kirsten (Bochum); Meyer, Moritz (Ahaus); Mirow, Lutz (Zwickau); Mittag-Bonsch, Martina (Crailsheim); Möbius, Ekkehard (Braunschweig), Mörder-Köttgen, Anja (Freiburg); Moesta, Kurt Thomas (Hannover); Mugomba, Gilbert (Dannenberg); Moldenhauer, Ingolf (Braunschweig); Morkramer, Rolf (Radevormwald); Mosa, Tawfik (Merseburg); Müller, Hannes (Schlanders); Müller, Volker (Nürnberg); Münzberg, Gregor (Berlin); Murr, Alfons (Vilshofen); Mussack, Thomas (St. Gallen); Nartschik, Peter (Quedlinburg); Nasifoglu, Bernd (Ehingen); Neumann, Jürgen (Haan); Neumeuer, Kai (Paderborn); Niebuhr, Henning (Hamburg); Nix, Carsten (Walsrode); Nölling, Anke (Burbach); Nostitz, Friedrich Zoltán (Mühlhausen); Obermaier, Straubing); Öz-Schmidt, Meryem (Hanau); Oldorf, Peter (Usingen); Olivieri, Manuel (Pforzheim); Passon, Marius (Freudenberg); Pawelzik, Marek (Hamburg); Pein, Tobias (Hameln); Peiper, Christian (Hamm); Peiper, Matthias (Essen); Pertl, Alexander (Spittal/Drau); Philipp, Mark (Rostock); Pickart, Lutz (Bad Langensalza); Pizzera, Christian (Graz); Pöllath, Martin (Sulzbach-Rosenberg); Pöschmann, Enrico (Thalwil); Possin, Ulrich (Laatzen); Prenzel, Klaus (Bad Neuenahr-Ahrweiler); Pröve, Florian (Goslar); Pronnet, Thomas (Fürstenfeldbruck); Pross, Matthias (Berlin); Puff, Johannes (Dinkelsbühl); Rabl, Anton (Passau); Raggi, Matthias Claudius (Stuttgart); Rapp, Martin (Neunkirchen); Reck, Thomas (Püttlingen); Reinpold, Wolfgang (Hamburg); Renter, Marc Alexander (Moers); Reuter, Christoph (Quakenbrück); Radke, Alexander (Thun/Zweisimmen); Richter, Jörg (Winnenden); Riemann, Kerstin (Alzenau-Wasserlos); Riesener, Klaus-Peter (Marl); Rodehorst, Anette (Otterndorf); Roehr, Thomas (Rödental); Rössler, Michael (Rüdesheim am Rhein); Roncossek, Bremerhaven); Rosniatowski, Rolland (Marburg); Roth Hartmut (Nürnberg); Sardoschau, Nihad (Saarbrücken); Sauer, Gottfried (Rüsselsheim); Sauer, Jörg (Arnsberg); Seekamp, Axel (Freiburg); Seelig, Matthias (Bad Soden); Seidel, Hanka (Eschweiler); Seiler, Christoph Michael (Warendorf); Seltmann, Cornelia (Hachenburg); Senkal, Metin (Witten); Shamiyeh, Andreas (Linz); Shang, Edward (München); Siemssen, Björn (Berlin); Sievers, Dörte (Hamburg); Silbernik, Daniel (Bonn); Simon, Thomas (Weinheim); Sinn, Daniel (Olpe); Sinner, Guy (Merzig); Sinning, Frank (Nürnberg); Smaxwil, Constatin Aurel (Stuttgart); Sörensen, Björn (Lauf an der Pegnitz): Sucke, Jochen Markus (Gießen); Syga, Günter (Bayreuth); Schabel, Volker (Kirchheim/Teck); Schadd, Peter (Euskirchen); Schassen von, Christian (Hamburg); Schattenhofer, Thomas (Vilshofen); Scheibel, Mike (Krefeld); Schelp, Lothar (Wuppertal); Scherf, Alexander (Pforzheim); Scheuerlein, Hubert (Paderborn); Scheyer, Mathias (Bludenz); Schilling, André (Kamen); Schimmelpenning, Hendrik (Neustadt in Holstein); Schinkel, Svenja (Kempten); Schmid, Michael (Gera); Schmid, Thomas (Innsbruck); Schmidt, Ulf (Mechernich); Schmitz, Heiner (Jena); Schmitz, Ronald (Altenburg); Schöche, Jan (Borna); Schoenen, Detlef (Schwandorf); Schrittwieser, Rudolf (Bruck an der Mur); Schroll, Andreas (München); Schubert, Daniel (Saarbrücken); Schüder, Gerhard (Wertheim); Schürmann, Rainer (Steinfurt); Schultz, Christian (Bremen-Lesum); Schultz, Harald (Landstuhl); Schulze, Frank P. Mülheim an der Ruhr); Schulze, Thomas (Dessau-Roßlau); Schumacher, Franz-Josef (Oberhausen); Schwab, Robert (Koblenz); Schwandner, Thilo (Lich); Schwarz, Jochen Günter (Rottenburg); Schymatzek, Ulrich (Eitorf); Spangenberger, Wolfgang (Bergisch-Gladbach); Sperling, Peter (Montabaur); Staade, Katja (Düsseldorf); Staib, Ludger (Esslingen); Staikov, Plamen (Frankfurt am Main); Stamm, Ingrid (Heppenheim); Stark, Wolfgang (Roth); Stechemesser, Bernd (Köln); Steinhilper, Uz (München); Stengl, Wolfgang (Nürnberg); Stern, Oliver (Hamburg); Stöltzing, Oliver (Meißen); Stolte, Thomas (Mannheim); Stopinski, Jürgen (Schwalmstadt); Stratmann, Gerald (Goch); Straßburger, Harald (Alfeld); Stubbe, Hendrik (Güstrow/); Stülzebach, Carsten (Friedrichroda); Tepel, Jürgen (Osnabrück); Terzić, Alexander (Wildeshausen); Teske, Ulrich (Essen); Thasler, Wolfgang (München); Tichomirow, Alexej (Brühl); Tillenburg, Wolfgang (Marktheidenfeld); Timmermann, Wolfgang (Hagen); Tomov, Tsvetomir (Koblenz; Train, Stefan H. (Gronau); Trauzettel, Uwe (Plettenberg); Triechelt, Uwe (Langenhagen); Ulbricht, Wolfgang (Breitenbrunn); Ulcar, Heimo (Schwarzach im Pongau); Ungeheuer, Andreas (München); Unger, Solveig (Chemnitz); Utech, Markus (Gelsenkirchen); Verweel, Rainer (Hürth); Vogel, Ulrike (Berlin); Voigt, Rigo (Altenburg); Voit, Gerhard (Fürth); Volkers, Hans-Uwe (Norden); Volmer, Ulla (Berlin); Vossough, Alexander (Neuss); Wallasch, Andreas (Menden); Wallner, Axel (Lüdinghausen); Warscher, Manfred (Lienz); Warwas, Markus (Bonn); Weber, Jörg (Köln); Weber, Uwe (Eggenfelden); Weihrauch, Thomas (Ilmenau); Weiß, Heiko (Aue); Weiß, Johannes (Schwetzingen); Weißenbach, Peter (Neunkirchen); Werner, Uwe (Lübbecke-Rahden); Wessel, Ina (Duisburg); Weyhe, Dirk (Oldenburg); Wicht, Sebastian (Bützow); Wieber, Isabell (Köln); Wiens, Matthias (Affoltern); Wiesmann, Aloys (Rheine); Wiesner, Ingo (Halle); Withöft, Detlef (Neutraubling); Woehe, Fritz (Sanderhausen); Wolf, Claudio (Neuwied); Wolkersdörfer, Toralf (Pößneck); Yaksan, Arif (Wermeskirchen); Yildirim, Can (Lilienthal); Yildirim, Selcuk (Berlin); Zarras, Konstantinos (Düsseldorf); Zeller, Johannes (Waldshut-Tiengen); Zhorzel, Sven (Agatharied); Zuz, Gerhard (Leipzig).
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Fortelny, R.H., Hofmann, A., Köckerling, F. (2018). Results and Complications of Incisional Hernia Surgery. In: Campanelli, G. (eds) The Art of Hernia Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-72626-7_64
Download citation
DOI: https://doi.org/10.1007/978-3-319-72626-7_64
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72624-3
Online ISBN: 978-3-319-72626-7
eBook Packages: MedicineMedicine (R0)