Abstract
Background
Seroma formation remains a common complication after an incisional hernia repair. The use of surgical drains is widespread, but evidence for their use and other adjuncts is limited. Our aim was to perform a systematic review of the literature on techniques used to reduce the incidence of post-operative seroma formation.
Methods
A systematic search of PubMed and Embase databases was conducted using terms including “incisional hernia” and “seroma”. All studies on adults undergoing open incisional hernia repair with at least one intervention designed to reduce seroma formation were included.
Results
Of the 1093 studies identified, 9 met the inclusion criteria. Medical talc: one cohort study of 74 patients undergoing talc application following pre-peritoneal mesh placement found a significantly decreased rate of seroma formation of 20.8 versus 2.7% (p < 0.001), but a retrospective study including 21 patients with onlay mesh found an increased rate of 76% seroma formation from 9.5% (p = 0.001). Fibrin glue: one comparative study including 60 patients found a reduction in seroma formation from 53 to 10% (p = 0.003), whereas a retrospective study of 250 patients found no difference (11 vs. 4.9% p = 0.07). Negative pressure wound therapy: four retrospective studies including a total of 358 patients found no difference in seroma outcome. Others: one randomised study of 42 patients undergoing either suction drainage or “quilting” sutures found no difference in seroma formation.
Conclusions
There is currently insufficient quality evidence to recommend any of the investigated methods, some of which incur significant additional cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incisional hernia is a common and sometimes inevitable complication following midline laparotomy and is reported to occur in up to 20% of patients 1 year post-operatively [1]. Hernias can also occur following other abdominal surgery including Pfannenstiel incisions for caesarian section and other gynaecological surgery, appendicectomy, cholecystectomy as well as those related to laparoscopic port sites. Repairs using mesh lead to a lower rate of recurrence, but wound complications, including haematoma and seroma, are common [2, 3]. A seroma has been described as, “a collection of serous fluid in a body cavity, organ or tissue, which occurs following surgery or trauma,” but a formal widely accepted definition is lacking. Rates of seroma formation vary depending on whether radiological or clinical methods of assessment are used and the length of the follow-up [4,5,6]. Seroma formation is most common following surgery that involves extensive tissue dissection resulting in a “dead space” (e.g. abdominoplasty, mastectomy), as well as following surgery that disrupts lymphatics (e.g. axillary and groin lymph node dissections) [7, 8]. There may be other differences in the aetiology of seroma formation between these different procedures, but there is a paucity of evidence to confirm or refute this.
There is a variable individual inflammatory response to different implanted prostheses that may contribute to a patient’s risk of developing seroma following incisional hernia repair and this may also relate to the positioning of the material in the abdominal wall [9]. A retrospective study of patients undergoing incisional hernia repair found that the only pre-operative factor associated with an increased risk of seroma was a higher number of previous abdominal incisions [10]. Symptomatic seromas are common in open and laparoscopic incisional hernia repairs and are present in 8–12.5% of patients having undergone open repair at clinical assessment 8 weeks post-operatively [10, 11]. A systematic review of laparoscopic repair identified a seroma rate of 5.4% [12] when diagnosed on clinical criteria, but it has been suggested that some degree of seroma formation may be inevitable as the rate approaches 100% when diagnosed on radiological criteria alone. [13, 14].
It has been demonstrated that seroma volume decreases over time when routinely measured after abdominoplasty and many resolve with conservative management alone [8]. However, some patients develop a chronic seroma, and repeated aspiration to relieve symptoms may contribute to the risk of infection [10]. These patients with symptomatic seroma require investigations and treatment using considerable health-care resources. Consequently, many surgeons will perform an intra-operative technical step (e.g. quilting sutures) or adjunct procedure (e.g. drain placement) during the incisional hernia repair with the specific aim of reducing the likelihood of seroma development. These technical steps, which are non-essential to the hernia repair itself, differ from additional procedures (e.g. panniculectomy) in that they serve no other intended purpose than seroma prevention. It is uncertain to what extent these various adjuncts reduce seroma formation and which option may be most effective. Therefore, the aim of this review was to evaluate the various intra-operative adjuncts used to reduce seroma formation in open incisional hernia repair.
Methods
The review was registered prospectively at the PROSPERO International Register of Prospective Reviews with the study ID CRD42017058106 [15]. An electronic search of PubMed and Embase (1947–29th January 2017) was performed independently by LHM and SP. The search terms used were “incisional hernia”, “abdominal wall hernia”, “ventral hernia”, “mesh” “seroma”, “talc”, “negative pressure wound therapy”, “fibrin sealant”, “quilting” and “abdominal drain”. Bibliographic references were searched to identify relevant studies that were not found by electronic search.
All citations identified by our search strategy were reviewed independently by LHM and SP, by sequential review of title, abstract and then full text to establish inclusion or exclusion as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidance (PRISMA) [16].
Inclusion criteria
Studies included for analysis were retrospective or prospective comparative human studies in peer-reviewed journals describing at least one intervention designed to decrease the rate of seroma formation following open incisional hernia repair, with post-operative seroma formation as a measured outcome.
Exclusion criteria
Search results were carefully analysed to exclude duplicate studies or a second study using the same data set. Studies on laparoscopic methods of repair, primary abdominal wall hernias, inguinoscrotal hernias, abdominoplasty alone without hernia repair, prophylactic mesh placement following primary surgery and hernias from a myocutaneous flap donor site were excluded, as were studies in children less than 18 years old and those not available in the English language. Laparoscopic repairs were not included, as the repair technique is very different: it is rare for large skin flaps to be raised, the midline defect is often not closed and the mesh is effectively used to bridge the defect. Case reports, case series without a comparison group and studies with less than five patients in each group were also excluded. Conference abstracts were screened, but excluded if there was no associated peer-reviewed publication.
Outcome measures
The primary outcome measure was seroma formation. Secondary outcome measures were recurrence, pain and quality of life.
Definitions
Seroma formation
Clinical or radiological assessment indicating the presence of fluid in the subcutaneous space. There is no standard definition for clinical assessment, so seroma requiring intervention was the most commonly used method.
Recurrence
Clinical or radiological evidence of a recurrent hernia detected during the follow-up period.
Negative pressure wound therapy (NPWT)
Application of a vacuum suction dressing over a closed wound, secured with an adhesive dressing.
Medical talc
Medical talc is a mineral composed of hydrated magnesium silicate and has an established use as a sclerosing agent to achieve pleurodesis in recurrent pleural effusions and there is much evidence for its overall safety in humans [17]. There are some data on its use to prevent seroma in abdominal wall hernia and axillary dissection [18]. It can be spread over tissues in an aerosolised or slurry form.
Fibrin sealant
These are used as a non-traumatic method of fixation. They comprise a mix of human fibrinogen with aprotinin (an anti-fibrinolytic agent) and thrombin reconstituted with calcium chloride, and their mechanism of action is via the later stages of the coagulation cascade [19]. They are available in different thrombin concentrations, and application for this purpose is via a droplet or spray applicator.
Surgical drains
At suction drain secured in the subcutaneous space post-operatively. Size and number of drains used and the criteria for their removal are variable.
Quilting sutures
Up to 40 interrupted absorbable sutures placed between the undermined flap and the anterior rectus sheath with the intention of closing the dead space in this plane.
Quality assessment and data extraction
Observational studies were assessed using the MINORS criteria [20] and the single randomised trial was assessed using the Cochrane Collaboration’s risk of bias tool at study level [21].
Statistical analysis
RevMan 5.3 (Review Manager Version 5.3 Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used for meta-analysis of the NPWT subgroup. Results of the meta-analysis were assessed using odds ratios (OR) with 95% confidence intervals (CI) within a Mantel–Haenszel random effects model. The variability in study outcome was assessed by calculating statistical heterogeneity using χ2 and inconsistency (I2) statistics. I2 values ≥ 50% represented considerable heterogeneity and p ≤ 0.05 was considered to be statistically significant.
Numerous operative strategies have been proposed that aim to reduce the risk of seroma. An initial search identified articles describing NPWT for closed incisions, fibrin sealant, medical talc, quilting sutures and suction drainage.
Results
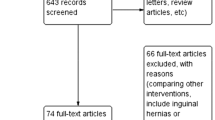
The database searches identified 1443 citations. After removing duplicates and screening titles, 41 abstracts were included for review and after application of inclusion/exclusion criteria to these 12 full text articles were assessed and 9 were included for final analysis [5, 6, 22,23,24,25,26,27,28]. The PRISMA statement of search results is shown (Fig. 1).
Eight were retrospective cohort studies: four on NPWT with a total of 358 patients, two on fibrin sealant with a total of 310 patients and two on medical talc with a total of 317 patients. There was one randomised controlled trial on surgical drains versus quilting sutures with a total of 42 patients. A summary of the patient demographics and study design differences is shown in Tables 1, 2, 3 and 4. The studies varied in repair technique and assessment method, including the post-operative time point at which seroma was assessed for and measured, and in some cases the volume of the fluid was used to define the presence of a seroma. None of the included studies contained any data for post-operative pain or quality-of-life assessment, and four included recurrence data.
Negative wound pressure therapy (NPWT)
Four studies reported seroma outcomes in NPWT compared to conventional dressings. Three studies used the KCI VAC system for 5 days [23], 7 days [24] or for 48 h after the wicks were dry [28]. One study used a Prevena dressing at 125 mmHg for 7 days [26]. Pooling results demonstrated a 6.4% rate of seroma in patients receiving NPWT compared to 11.3% of controls with an odds ratio of 0.63. This was not statistically significant on meta-analysis (Fig. 2) (OR 0.63 [95% CI 0.28–1.4]; p = 0.36; I 2 = 0%; p = 0.69).
Medical talc
Two studies reported seroma outcomes using medical talc in the subcutaneous space compared to standard procedure. Klima et al. [25] found a 2.7% rate of seroma in the talc group and 20.8% in the control group, whereas Parameswaran et al. [27] found a 76% rate of seroma formation in the talc group and 9.5% in the control group.
Fibrin sealant
Two studies reported seroma outcomes using fibrin sealant in the subcutaneous space compared to standard procedure, although one of the studies [22] also applied NPWT to both groups. One study used TISSEEL™ in droplet form, 500 IU thrombin/ml per 5 cm2 defect area [22], and the other study used ARTISS™, 4 IU thrombin/ml per 20 cm2 defect area [6]. The study by Azoury et al. [22] found that the rate of seroma was 11% in the fibrin sealant group and 4.9% in controls, whereas Kohler et al. [6] found a rate of 3.3% in the sealant group and 23% in controls.
Drains vs quilting sutures
There was one randomised controlled trial on surgical drains versus quilting sutures. The rates of seroma formation were high in both groups in this study at three different time points on ultrasound criteria, varying from 19% early (4–6 days post-operative) to 52% late (29–31 days post-operative) in the drain group to 29% early and 43% late in the quilting sutures group [5].
Study quality
The eight retrospective studies were assessed according to the MINORS criteria. Only one study scored 16 (high quality) on the MINORS criteria (median 13.5, range 8–16) [24]. The one randomised controlled trial was assessed according to the Cochrane risk of bias tool [5]. The main source of bias identified was the lack of outcome blinding; however, it was a small study with no power calculation performed to estimate the numbers needed to achieve a reliable result [5].
There was frequent variation in patient baseline characteristics between intervention and control groups within the studies, including BMI, smoking status, defect size and proportion of clean contaminated wounds.
Discussion
The aim of this study was to review the evidence on intra-operative adjuncts designed to prevent seroma following open incisional hernia repair. The only studies identified were low-quality retrospective studies and the lack of availability of higher-quality evidence limits our review. The intervention about which there was data in the largest number of patients was NPWT and this was the only subgroup on which it was possible to perform a meta-analysis that demonstrated no statistically significant difference in outcome. Studies on medical talc and fibrin sealant reached divergent findings that are likely to reflect variability in operative technique as much as any true effect of the adjunct per se. It is not possible to recommend the use of any of the investigated adjuncts based on current evidence.
There were no standard reporting criteria or classification systems used when describing seroma outcome in any of the studies. Patient-related outcome and quality-of-life data are absent in these studies which contain clinician-centred data with little use of validated classification systems such as Clavien–Dindo [29]. Seroma-specific classification systems have been derived [14] and recommended for use [30], but they are based on expert opinion and their validity and correlation to other outcome scores such as patient-reported outcome measures and quality of life have not been established. Control groups were frequently historical, which introduces confounders including operative volumes and experience, patient selection and reporting bias. Patient-reported outcome measures and quality-of-life tools have not been widely used or reported within the field and consequently no studies have reported a comprehensive cost analysis of the different interventions compared to control.
Our review was limited to studies with an intra-operative adjunct and was not designed to examine whether there may be an effect from different surgical meshes or the layer of placement within the abdominal wall. A review and meta-analysis [31] of biologic and synthetic mesh in inguinal hernia repair found a significantly increased risk of seroma in the biologic group. This finding is likely applicable to incisional hernia repair, but has not been demonstrated as there are only data on a small number of patients [32]. Mesh type may therefore have a significant effect on seroma outcome, but investigating this was beyond the scope of our study.
A further limitation of our review is the restriction of operative technique to open repairs only. We excluded laparoscopic repair, as the technique used is entirely different from that used in open incisional hernia repair and the results from our review could not be meaningfully applied to laparoscopic repair. Other studies were excluded as seroma was not included as a separate outcome and obfuscated by reporting of “surgical site occurrences” [33, 34].
Subcutaneous suction drains are commonly used during open incisional hernia repair to allow fluid, including haematoma and seroma to drain in the early post-operative period. It has been associated with a decreased rate of seroma formation in retrospective case series [10]. There has been a Cochrane review of the use of surgical drains following open incisional hernia repair, which identified no randomised controlled trials comparing wound drainage to no wound drainage [35]. Drain fluid volume in the early post-operative period following mesh repair is significantly increased in patients who subsequently develop seroma. It is therefore possible that the prolonged use of drains may help prevent later seroma formation. Patients with a mesh who developed a seroma had both a lower drain fluid lactate and a lower drain fluid pH value than those who do not develop seroma [36]. They also expressed different amounts of some cytokines in the drain fluid, which may have acted to delay wound healing. The seroma fluid contained high levels of a procollagen and fibronectin compared to the drain fluid, but low levels of lactate, which is normally high in healing tissues [37].
The use of quilting sutures to reduce the rate of seroma formation has been demonstrated in abdominoplasty [8, 37] and mastectomy [38]. The underlying principle of quilting sutures is that reduction of dead space reduces the incidence of seroma and the volume of those seromas that do occur. Their main disadvantage is the increased operation time required, which may be reduced with a modified technique, but otherwise can add up to 50 min [37]. The study comparing surgical drains to quilting sutures did not find any significant difference in seroma between the two groups. The numbers were small and this study was very likely underpowered to detect a significant difference [5].
Extrapolations from other fields of surgery have highlighted other intra-operative adjuncts that may be suitable for further study of seroma prevention in incisional hernia surgery. Triamcinolone acetonide is a topical corticosteroid that is licensed for use in humans for intra-articular injection and as a dermal cream. Its use for seroma reduction has been studied in an animal mastectomy model where it was found to perform better than fibrin glue [39]. There has also been a study of its use in established seroma at the latissimus dorsi flap donor sites to reduce the need for repeated aspiration, but it has not been used to prevent seroma [40]. Topical methylprednisolone has also been used following human mastectomy with mixed results [41], as has erythromycin in a small case series of refractory seroma in plastic surgery [42]. A comparative series in abdominoplasty found that using sutures or clips instead of diathermy to seal the abdominal wall perforators lead to a decreased rate of seroma formation [43]. This has also been studied previously in mastectomy patients, but has not been repeated in surgery involving mesh.
There are some post-operative adjuncts that have also been investigated. Abdominal binders are in frequent use in some parts of the world, including at least occasional use by more than 90% of French abdominal surgeons according to a recent survey [44]. Their historic use has been aimed at reducing post-operative pain and preventing abdominal wall dehiscence, and it has been theorised that they may be able to reduce post-operative seroma. However, there is at best only weak evidence for their use for these indications [10].
Conclusion
High-quality studies were lacking in all the interventions identified and there was considerable variability across studies in the outcome definitions used. We cannot recommend any method for use based on the current available evidence. Consistent reporting of seroma outcome using a standard classification system is essential for future studies.
References
Diener MK, Voss S, Jensen K, Buchler MW, Seiler CM (2010) Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg 251(5):843–856
den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW (2008) Open surgical procedures for incisional hernias. Cochrane Database Syst Rev 3:CD006438. doi:10.1002/14651858.CD006438.pub2
Deerenberg EB, Timmermans L, Hogerzeil DP, Slieker JC, Eilers PH, Jeekel J, Lange JF (2015) A systematic review of the surgical treatment of large incisional hernia. Hernia 19(1):89–101
Klinge U, Conze J, Krones CJ, Schumpelick V (2005) Incisional hernia: open techniques. World J Surg 29(8):1066–1072
Westphalen AP, Araujo AC, Zacharias P, Rodrigues ES, Fracaro GB, Lopes Filho GD (2015) Repair of large incisional hernias. To drain or not to drain. Randomized clinical trial. Acta Cir Bras 30(12):844–851
Kohler G, Koch OO, Antoniou SA, Lechner M, Mayer F, Emmanuel K (2014) Prevention of sub-cutaneous seroma formation in open ventral hernia repair using a new low-thrombin fibrin sealant. World J Surg 38(11):2797–2803
de Vries M, Hoekstra HJ, Hoekstra-Weebers JE (2009) Quality of life after axillary or groin sentinel lymph node biopsy, with or without completion lymph node dissection, in patients with cutaneous melanoma. Ann Surg Oncol 16(10):2840–2847
Bercial ME, Sabino Neto M, Calil JA, Rossetto LA, Ferreira LM (2012) Suction drains, quilting sutures, and fibrin sealant in the prevention of seroma formation in abdominoplasty: which is the best strategy? Aesthetic Plast Surg 36(2):370–373
Schachtrupp A, Klinge U, Junge K, Rosch R, Bhardwaj RS, Schumpelick V (2003) Individual inflammatory response of human blood monocytes to mesh biomaterials. Br J Surg 90(1):114–120
Kaafarani HM, Hur K, Hirter A, Kim LT, Thomas A, Berger DH, Reda D, Itani KM (2009) Seroma in ventral incisional herniorrhaphy: incidence, predictors and outcome. Am J Surg 198(5):639–644
Pring CM, Tran V, O’Rourke N, Martin IJ (2008) Laparoscopic versus open ventral hernia repair: a randomized controlled trial. ANZ J Surg 78(10):903–906
Bedi AP, Bhatti T, Amin A, Zuberi J (2007) Laparoscopic incisional, ventral hernia repair. J Minim Access Surg 3:83–90
Susamallian S, Gewurtz G, Ezri T, Charuzi I (2001) Seroma after laparoscopic repair of hernia with PTFE patch: is it really a complication? Hernia 5:139–141
Morales-Conde S (2012) A new classification for seroma after laparoscopic ventral hernia repair. Hernia 16(3):261–267
PROSPERO international register of systematic reviews. York University. https://www.crd.york.ac.uk/PROSPERO/
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Shaw P, Agarwal R (2004) Pleurodesis for malignant pleural effusions. Cochrane Data-base Syst Rev 1(1):CD002916. doi:10.1002/14651858.CD002916.pub2
Klima DA, Belyansky I, Tsirline VB, Lincourt AE, Lipford EH, Getz SB, Heniford BT (2012) Application of subcutaneous talc after axillary dissection in a porcine model safely reduces drain duration and prevents seromas. J Am Coll Surg 214(3):338–347
Dunn CJ, Goa KL (1999) Fibrin sealant. Drugs 58(5):863–886
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Azoury SC, Rodriguez-Unda N, Soares KC, Hicks CW, Baltodano PA, Poruk KE, Hu QL, Cooney CM, Cornell P, Burce K, Eckhauser FE (2015) The effect of TISSEEL fibrin sealant on seroma formation following complex abdominal wall hernia repair: a single institutional review and derived cost analysis. Hernia 19(6):935–942
Conde-Green A, Chung TL, Holton LH, Hui-Chou HG, Zhu Y, Wang H, Zahiri H, Singh DP (2013) Incisional negative-pressure wound therapy versus conventional dressings following abdominal wall reconstruction: a comparative study. Ann Plast Surg 71(4):394–397
Gassman A, Mehta A, Bucholdz E, Abthani A, Guerra O, Maclin MM, Esposito T, Thomas C (2015) Positive outcomes with negative pressure therapy over primarily closed large abdominal wall reconstruction reduces surgical site infection rates. Hernia 19(2):273–278
Klima DA, Brintzenhoff RA, Tsirline VB, Belyansky I, Lincourt AE, Getz S, Heniford BT (2011) Application of subcutaneous talc in hernia repair and wide subcutaneous dissection dramatically reduces seroma formation and postoperative wound complications. Am Surg 77(7):888–894
Olona C, Duque E, Caro A, Jimenez A, Moreno F, Coronas JM, Vicente V (2014) Negative-pressure therapy in the postoperative treatment of incisional hernioplasty wounds: a pilot study. Adv Skin Wound Care 27(2):77–80
Parameswaran R, Hornby ST, Kingsnorth AN (2013) Medical talc increases the incidence of seroma formation following onlay repair of major abdominal wall hernias. Hernia 17(4):459–463
Soares KC, Baltodano PA, Hicks CW, Cooney CM, Olorundare IO, Cornell P, Burce K, Eckhauser FE (2015) Novel wound management system reduction of surgical site morbidity after ventral hernia repairs: a critical analysis. Am J Surg 209(2):324–332
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Muysoms FE, Deerenberg EB, Peeters E, Agresta F, Berrevoet F, Campanelli G, Ceelen W, Champault GG, Corcione F, Cuccurullo D, DeBeaux AC, Dietz UA, Fitzgibbons RJ Jr, Gillion JF, Hilgers RD, Jeekel J, Kyle-Leinhase I, Kockerling F, Mandala V, Montgomery A, Morales-Conde S, Simmermacher RK, Schumpelick V, Smietanski M, Walgenbach M, Miserez M (2013) Recommendations for reporting outcome results in abdominal wall repair: results of a Consensus meeting in Palermo, Italy, 28-30 June 2012. Hernia 17(4):423–433
Fang Z, Ren F, Zhou J, Tian J (2015) Biologic mesh versus synthetic mesh in open inguinal hernia repair: system review and meta-analysis. ANZ J Surg 85(12):910–916
Satterwhite TS, Miri S, Chung C, Spain D, Lorenz HP, Lee GK (2012) Outcomes of complex abdominal herniorrhaphy: experience with 106 cases. Ann Plast Surg 68(4):382–388
Petro CC, Novitsky YW (2016) Classification of hernias. In: Novitsky YW (ed) Hernia surgery. Springer, Cham, pp 15–21. doi:10.1007/978-3-319-27470-6_2
Muysoms F (2017) Evaluating outcomes and evidence in hernia repair. In: Cobb WS, Adrales GL, Hope WW (eds) Textbook of hernia. Springer, Cham, pp 15–21
Gurusamy KS, Allen VB (2013) Wound drains after incisional hernia repair. Cochrane Database Syst Rev 12:CD005570. doi:10.1002/14651858.CD005570.pub4
Klink CD, Binnebosel M, Lucas AH, Schachtrupp A, Klinge U, Schumpelick V, Junge K (2010) Do drainage liquid characteristics serve as predictors for seroma formation after incisional hernia repair? Hernia 14(2):175–179
Sforza M, Husein R, Andjelkov K, Rozental-Fernandes PC, Zaccheddu R, Jovanovic M (2015) Use of quilting sutures during abdominoplasty to prevent seroma formation: are they really effective? Aesthet Surg J 35(5):574–580
Ouldamer L, Bonastre J, Brunet-Houdard S, Body G, Giraudeau B, Caille A (2016) Dead space closure with quilting suture versus conventional closure with drainage for the prevention of seroma after mastectomy for breast cancer (QUISERMAS): protocol for a multicentre randomised controlled trial. BMJ Open 6(4):e009903
Choi MS, Kim HK, Kim WS, Bae TH, Kim MK (2012) A comparison of triamcinolone acetonide and fibrin glue for seroma prevention in a rat mastectomy model. Ann Plast Surg 69(2):209–212
Taghizadeh R, Shoaib T, Hart AM, Weiler-Mithoff EM (2008) Triamcinolone reduces seroma re-accumulation in the extended latissimus dorsi donor site. J Plast Reconstr Aesthet Surg 61(6):636–642
Qvamme G, Axelsson CK, Lanng C, Mortensen M, Wegeberg B, Okholm M, Arpi MR, Szecsi PB (2015) Randomized clinical trial of prevention of seroma formation after mastectomy by local methylprednisolone injection. Br J Surg 102(10):1195–1203
Ali-Khan AS, Orlando A, Kenealy J (2009) Erythromycin sclerotherapy in the management of seroma. J Plast Reconstr Aesthet Surg 62(3):e55–e58
Skillman JM, Venus MR, Nightingale P, Titley OG, Park A (2014) Ligating perforators in abdominoplasty reduces the risk of seroma. Aesthetic Plast Surg 38(2):446–450
Bouvier A, Rat P, Drissi-Chbihi F, Bonnetain F, Lacaine F, Mariette C, Ortega-Deballon P (2014) Abdominal binders after laparotomy: review of the literature and French survey of policies. Hernia 18(4):501–506
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LM declares no conflict of interest. SP declares no conflict of interest. AB declares conflict of interest not directly related to the submitted work (speaker’s fees from Medtronic). NS declares conflict of interest not directly related to the submitted work (speaker’s fees from Medtronic). ID declares conflict of interest not directly related to the submitted work (grants, personal fees and non-financial support from Medtronic).
Ethical approval
This study design conformed to ethical standards.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
There were no individual participants included in this study.
Rights and permissions
About this article
Cite this article
Massey, L.H., Pathak, S., Bhargava, A. et al. The use of adjuncts to reduce seroma in open incisional hernia repair: a systematic review. Hernia 22, 273–283 (2018). https://doi.org/10.1007/s10029-017-1690-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1690-z