Abstract
Introduction
Bisphosphonates and denosumab increase bone mineral density (BMD) for osteoporosis treatment in patients with aromatase inhibitor-associated bone loss (AIBL). This study aimed to directly compare bisphosphonates with denosumab in treating patients with AIBL and to determine the effect of denosumab on the trabecular bone score (TBS).
Materials and methods
Thirty-nine patients with AIBL receiving osteoporosis treatment (21 in the bisphosphonates group and 18 in the denosumab group) were retrospectively evaluated for changes in lumbar spine and femoral BMD, lumbar spine bone quality (assessed by TBS), and blood bone metabolic markers. The Mann–Whitney and Wilcoxon tests were used for statistical evaluation.
Results
After 24 months of treatment, the lumbar spine BMD change rate was 5.82 ± 1.10% with bisphosphonates and 10.49 ± 1.20% with denosumab, with the change rate of denosumab significantly increasing over that of bisphosphonates. The change rate in femoral BMD was 2.69 ± 1.16% with bisphosphonates and 2.95 ± 1.26% with denosumab, with no significant difference between the two groups. The rate of decrease in tartrate-resistant acid phosphatase isoform 5b was significantly higher in the denosumab group. The change rate in TBS at 24 months of treatment was 0.53 ± 1.26% in the bisphosphonates group and 1.08 ± 1.33% in the denosumab group, with no significant difference between the two groups. After 24 months, TBS remained stable.
Conclusion
Both bisphosphonates and denosumab may increase BMD, improve bone metabolism, and inhibit bone quality loss in patients with AIBL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer has a high morbidity and survival rate. Maintaining and improving health and quality of life (QOL) after experiencing breast cancer is as important as breast cancer treatment. Cancer treatment-induced bone loss (CTIBL) is an important factor in the decline of women’s QOL and healthy life expectancy. Particularly, aromatase inhibitor (AI) is widely used as postoperative therapy in patients with hormone receptor-positive postmenopausal breast cancer. AI effectively prevents breast cancer recurrence but suppresses residual ovarian function, resulting in reduced bone mineral density (BMD) and increased fractures, which reduces patients’ QOL [1,2,3].
Bone modifying agent (BMA) interventions such as bisphosphonates and denosumab for CTIBL can reduce bone loss and fractures in postmenopausal patients with breast cancer [4, 5]. In addition, BMA reduces the risk of bone metastasis and all-cause mortality in patients with breast cancer, and bone health care for breast cancer has been gaining attention [6,7,8]. The recommended duration of postoperative therapy is longer than 5 years. However, the risk of bone fracture increases as the treatment duration is extended; thus, the safety and efficacy of osteoporosis treatment must also be examined from a long-term perspective [9,10,11,12].
BMD and bone quality are important aspects of osteoporosis treatment. Bone quality is an independent factor of bone strength that cannot be defined by BMD. It encompasses various parameters such as bone microstructure, bone metabolic turnover, microfractures, and calcification of bone tissue [13]. Bone quality is classified into structural and material types, whereas the trabecular bone score (TBS) is an evaluation method of structural properties, with a higher TBS indicating a better microstructure and a lower TBS indicating a degraded microstructure. TBS is an evaluation method that reflects the trabecular bone microstructure in lumbar spine dual-energy X-ray absorptiometry (DXA) images. It can be calculated by importing the measurement data of existing DXA methods into analysis software, which enables retrospective examination. It has the advantages of being simple, versatile, and free from additional patient radiation exposure and medical costs [14, 15]. Clinically, TBS is considered useful in primary osteoporosis and secondary osteoporosis such as aromatase inhibitor-associated bone loss (AIBL) when used in conjunction with BMD assessment as a tool to predict current and future fragility fractures, detect and predict fractures, and monitor the patient’s treatment response [16].
Bisphosphonates have been suggested to improve BMD and maintain TBS in osteoporosis treatment in general, while denosumab improves BMD and TBS. These results suggest that denosumab may have a greater therapeutic effect than bisphosphonates in terms of BMD and bone quality [10, 17].
Bisphosphonates and denosumab have also been used to treat AIBL, with previous studies reporting that each drug increases BMD and prevents fractures [18,19,20,21,22,23,24]. Although bisphosphonates reduce TBS in patients with AIBL [25,26,27], few studies have examined the effect of denosumab on TBS; only one study worldwide has directly compared the two drugs.
This study aimed to directly compare the efficacy of bisphosphonates and denosumab in AIBL treatment based on BMD, bone quality (assessed by TBS), and bone metabolism markers and to determine the effect of denosumab on TBS in Japan.
Materials and methods
Study design
This was a single-center retrospective study. The participants were 39 patients with AIBL treated for osteoporosis at Yokohama City University Medical Center (Yokohama, Kanagawa Prefecture) between September 2015 and March 2021, using bisphosphonates or denosumab formulations.
Participants
Thirty-nine patients were treated with bisphosphonates (21 patients) and denosumab (18 patients). Patients treated with bisphosphonates received alendronate sodium hydrate, risedronate sodium hydrate, or minodronic acid hydrate. Patients treated with denosumab received 60 mg of denosumab every 6 months. Patients chose their drugs after being informed of the efficacy, administration method, and adverse effects of the bisphosphonates and denosumab. Patients who received denosumab were also treated with vitamin D preparation (alfacalcidol 1.0 µg/day), and the dose was reduced as needed, paying attention to Ca metabolism in blood and urine.
All patients met the following selection criteria and none of the exclusion criteria. Selection criteria: (1) postmenopausal women, (2) those older than 40 years of age at the start of osteoporosis treatment, (3) those treated with AI for breast cancer at our hospital, (4) those treated with bisphosphonates or denosumab for osteoporosis treatment at our hospital, (5) those started and continued osteoporosis treatment for at least 2 years, (6) those with a lumbar spine or femoral baseline BMD t-score < − 1.5. Exclusion criteria: (1) patients receiving continuous treatment with osteoporosis drugs before coming to our hospital, (2) patients with bone metastases, (3) patients who used bisphosphonates or denosumab as osteoporosis drugs but changed the drugs during treatment, and (4) patients with severe vertebral or femoral disease.
Clinical data
Clinical data (age, height, weight, body mass index, prevalent fracture, chemotherapy, radiotherapy history, DXA, and blood data) of all patients with AIBL were collected from medical records, patient forms, and DXA data from Yokohama City University Medical Center.
Informed consent for publication was obtained from all individual participants included in the study. This study protocol complied with the Declaration of Helsinki, and approval was obtained from the Ethics Committees of Yokohama City University School of Medicine (IRB number: B200300009).
Assessment of outcomes and statistical analysis
We retrospectively evaluated the change rate of lumbar spine and femoral BMD, lumbar spine TBS score, and bone metabolic markers (tartrate-resistant acid phosphatase isoform 5b (TRACP-5b), N-terminal propeptide of type I procollagen (total P1NP)), before, 6, 12, 18, and 24 months after bisphosphonates and denosumab treatment.
The assessment points were the comparison of the change rate in lumbar spine and femoral BMD and bone metabolic markers between the bisphosphonates and denosumab and the effect after 24 months of treatment. The effect of the denosumab on TBS was also assessed.
Statistical analysis was performed using the software program JMP Pro® 15.0 (SAS Institute Inc., Cary, NC, USA). Mann–Whitney test was used to compare the median values between the two groups, and analysis of covariance was performed to adjust for covariates. The Wilcoxon test with correspondence was used for pre- and post-treatment comparisons for each group. A value of p < 0.05 was considered statistically significant.
Measurement of BMD and TBS
DXA scans were conducted on the QDR 4500A (Hologic, Waltham, MA, USA). The coefficient of variation of the QDR 4500A was 0.52%, and the least significant change was 1.44% [28]. This study evaluated the lumbar spine (L2–L4) and femoral BMD, and the 2001 Osteoporosis Diagnostic Criteria of the Japanese Society for Bone and Mineral Research was used as the standard for osteoporosis [29].
TBS measurements were evaluated retrospectively from DXA spinal images using TBS iNsight software (version 3.0, Medimap, Geneva Switzerland) post-calibration. The following normal ranges for TBS in postmenopausal women have been proposed: TBSs 1.350 and above, normal microarchitecture; TBSs between 1.200 and 1.350; partially degraded microarchitecture represents borderline risk of fracture; and TBSs 1.200 and below, degraded microarchitecture represents the highest risk of fracture [14].
Results
Table 1 presents the background characteristics and results of 39 patients with AIBL, 21 in the bisphosphonates group and 18 in the denosumab group, including age at breast cancer onset in both groups, time from AI start to pre-treatment DXA, physical assessment, history of prior fractures, prior chemotherapy and radiation therapy, DXA levels before bisphosphonates or denosumab treatment, and bone metabolic marker levels. There were three prevalent fractures in the bisphosphonate group (14.3%, two thoracic spine fractures and one distal radius fracture) and two in the denosumab group (11.1%, one thoracic spine fracture and one distal radius fracture). The results did not differ significantly between the groups. No patients used cyclin-dependent kinase inhibitors.
Comparison of lumbar spine BMD change rates between treatment groups
The mean change rate in lumbar spine BMD from baseline was 2.21 ± 1.12% vs. 7.48 ± 1.21% (p < 0.01) in the bisphosphonates vs. denosumab groups at 6 months, 4.60 ± 0.82% vs. 8.47 ± 0.90% (p < 0.01) at 12 months, and 4.27 ± 1.16% vs. 9.70 ± 1.23% (p < 0.01) at 18 months, and 5.82 ± 1.10% vs. 10.49 ± 1.20% (p < 0.01) at 24 months, with all values significantly higher in the denosumab group (Fig. 1).
Lumbar spine BMD change rate of bisphosphonate and denosumab administration over 24 months. The mean changes rate from baseline are 2.21 ± 1.12% vs. 7.48 ± 1.21% (p < 0.01) at 6 months, 4.60 ± 0.82% vs. 8.47 ± 0.90% (p < 0.01) at 12 months, 4.27 ± 1.16% vs. 9.70 ± 1.23% (p < 0.01) at 18 months, and 5.82 ± 1.10% vs. 10.49 ± 1.20% (p < 0.01) at 24 months in the bisphosphonates vs. denosumab groups, with all values significantly higher in the denosumab group. p-values were determined by the Mann–Whitney test to compare the median values between the groups. *Differences at p < 0.05 are considered statistically significant. BMD bone mineral density, vs. versus
Changes in lumbar spine BMD in the first 24 months of treatment
The lumbar spine BMD change from baseline to 24 months after the start of treatment increased significantly in both the bisphosphonates (p < 0.01) and denosumab groups (p < 0.01) (Table 2).
Comparison of femoral BMD change rates between treatment groups
The mean change rate in femoral BMD from baseline was 1.67 ± 0.99% vs. 0.31 ± 1.08% (p = 0.53) in the bisphosphonates vs. denosumab groups at 6 months, 2.84 ± 0.99% vs. 3.11 ± 1.08% (p = 0.87) at 12 months, 2.88 ± 0.91% vs. 2.44 ± 0.96% (p = 0.95) at 18 months, and 2.69 ± 1.16% vs. 2.95 ± 1.26% (p = 0.93) at 24 months, with no significant difference between the two groups at all time points (Fig. 2).
Femoral BMD change rate of bisphosphonate and denosumab administration over 24 months. The mean change rates from baseline are 1.67 ± 0.99% vs. 0.31 ± 1.08% (p = 0.53) at 6 months, 2.84 ± 0.99% vs. 3.11 ± 1.08% (p = 0.87) at 12 months, 2.88 ± 0.91% vs. 2.44 ± 0.96% (p = 0.95) at 18 months, and 2.69 ± 1.16% vs. 2.95 ± 1.26% (p = 0.93) at 24 months in the bisphosphonates vs. denosumab groups, with no significant difference between the groups at all time points. p-values were determined by the Mann–Whitney test to compare the median values between the two groups. *Differences at p < 0.05 are considered statistically significant. BMD bone mineral density, vs. versus
Change in femoral BMD in the first 24 months of treatment
From baseline to 24 months after the start of treatment, femoral BMD significantly improved in both the bisphosphonates (p < 0.05) and denosumab groups (p < 0.05) (Table 2).
Comparison of change rate in bone metabolic markers between treatment groups
TRACP-5b and total P1NP decreased rapidly in both groups after the start of treatment. The mean change rate of TRACP-5b from baseline was − 36.5 ± 6.52% vs. − 59.5 ± 7.86% (p < 0.05) in the bisphosphonates vs. denosumab groups at 6 months, − 39.2 ± 6.93 vs. − 65.2 ± 7.99 (p < 0.05) at 12 months, and − 39.1 ± 4.89 vs. − 66.2 ± 6.07% (p < 0.01) at 24 months, with the change rate significantly declined in the denosumab group in all periods (Fig. 3).
TRACP-5b change rate of bisphosphonate and denosumab administration over 24 months. The mean change rates from baseline are − 36.5 ± 6.52% vs. − 59.5 ± 7.86% (p < 0.05) at 6 months, − 39.2 ± 6.93 vs. − 65.2 ± 7.99 (p < 0.05) at 12 months, and − 39.1 ± 4.89 vs. − 66.2 ± 6.07% (p < 0.01) at 24 months in the bisphosphonates vs. denosumab groups, with the change rate significantly decreased in the denosumab group at all periods. p-values were determined by the Mann–Whitney test to compare the median values between the two groups. *Differences at p < 0.05 are considered statistically significant. TRACP-5b tartrate-resistant acid phosphatase isoform 5b, vs. versus
The mean change in total P1NP from baseline was − 52.5 ± 4.01% vs. − 66.7 ± 4.71% (p = 0.06) in the bisphosphonates vs. denosumab groups at 6 months, − 56.4 ± 4.98% vs − 75.9 ± 5.78% (p < 0.05) at 12 months and − 59.3 ± 3.76% vs − 71.2 ± 4.66% (p = 0.20) at 24 months, showing a significant difference in the change rate at 12 months (Fig. 4).
Total P1NP change rate of bisphosphonate and denosumab administration over 24 months. The mean changes from baseline are − 52.5 ± 4.01% vs. − 66.7 ± 4.71% (p = 0.06) at 6 months, − 56.4 ± 4.98% vs − 75.9 ± 5.78% (p < 0.05) at 12 months, and − 59.3 ± 3.76% vs − 71.2 ± 4.66% (p = 0.20) at 24 months in the bisphosphonates vs. denosumab groups, showing a significant difference in the change rate at 12 months. p-values were determined by the Mann–Whitney test to compare the median values between the two groups. *Differences at p < 0.05 are considered statistically significant. Total P1NP N-terminal propeptide of type I procollagen, vs. versus
Changes in bone metabolic markers from the start of treatment to 24 months
The change rate from baseline to 24 months after the start of treatment was significantly reduced in both the bisphosphonates (p < 0.01) and denosumab groups (p < 0.01) (Table 2). Data on bone metabolic markers 18 months after treatment were excluded because of many missing values.
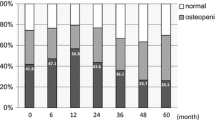
Comparison of the rate of change in TBS between treatment groups and the impact of 24 months of treatment
The mean change rate from baseline in lumbar spine TBS by DXA was − 1.91 ± 1.12% vs. − 1.09 ± 1.22% (p = 0.49) at 6 months, − 0.08 ± 1.08% vs. − 0.27 ± 1.17% (p = 0.96) at 12 months, − 0.97 ± 1.19% vs. 0.29 ± 1.26 (p = 0.47) at 18 months, 0.53 ± 1.26% vs. 1.08 ± 1.33% (p = 0.61) at 24 months in the bisphosphonates vs. denosumab groups. No significant difference was observed between the two groups at any time point (Fig. 5). From baseline to 24 months after the start of treatment, no significant difference existed between the bisphosphonates (p = 0.66) and denosumab groups (p = 0.52).
TBS change rate of bisphosphonate and denosumab administration over 24 months. The mean change rates from baseline are − 1.91 ± 1.12% vs. − 1.09 ± 1.22% (p = 0.49) at 6 months, − 0.08 ± 1.08% vs. − 0.27 ± 1.17% (p = 0.96) at 12 months, − 0.97 ± 1.19% vs. 0.29 ± 1.26 (p = 0.47) at 18 months, and 0.53 ± 1.26% vs. 1.08 ± 1.33% (p = 0.61) at 24 months in the bisphosphonates vs. denosumab groups. No significant difference is observed between the groups at any time point. P0values were determined by the Mann–Whitney test to compare the median values between the two groups. *Differences at p < 0.05 are considered statistically significant. TBS trabecular bone score, vs. versus
Discussion
Although AI agents are widely used as postoperative therapy for postmenopausal patients with hormone receptor-positive breast cancer and are effective in reducing recurrence rates, adverse events such as bone loss impair patients’ QOL. Osteoporosis treatment is considered important for long-term health maintenance; thus, BMD and bone quality are important in determining the therapeutic efficacy of BMA [30].
In this study, TBS was selected as the evaluation method for bone quality. TBS has the advantage of being simple and does not require additional examinations or exposure to radiation because it is calculated using analysis software based on existing lumbar spine DXA image data. However, the disadvantages of TBS are that it evaluates only the lumbar spine region, does not evaluate the proximal femur, and does not directly measure the bone microstructure. Although high-resolution peripheral quantitative computed tomography, which has become popular in recent years, can directly analyze the bone microstructure of cortical bone and cancellous bone by imaging the radius and tibia at high resolution [31], it requires additional examination and associated radiation exposure, as well as the purchase of equipment. Therefore, we considered TBS simple and useful in this study.
Previous studies have suggested that BMD decreases during AI treatment. Hong et al. reported a − 3.12% decrease in lumbar spine BMD and − 2.4% in femoral BMD at 1 year after the start of AI, and a − 1.39% decrease in lumbar spine BMD and − 1.54% in femoral BMD 1–2 years after AI [32]. Conversely, other studies have demonstrated the therapeutic effects of bisphosphonates and denosumab on BMD during AI treatment. In a prospective study by Rodríguez-Sanz et al. that examined the 5 year change in lumbar spine BMD with bisphosphonates for AIBL, lumbar spine BMD increased by 5.3% in patients treated with risedronate or alendronic acid [27]. In a prospective study by Nakatsukasa et al. on changes in lumbar spine BMD over 2 years in patients with AIBL treated with denosumab, lumbar spine BMD increased by 7% [33]. Here, lumbar spine BMD increased by 5.8% with bisphosphonates and 10.4% with denosumab in patients with AIBL at 24 months, showing the superiority of denosumab over bisphosphonates, consistent with the results of previous studies. In contrast, no difference existed in femoral BMD between the two drugs, although there was a significant increase at 24 months for both drugs. In general, the femur is predominantly cortical bone and is less affected by drug effects than the lumbar spine, which is predominantly trabecular bone. This may be why there was no difference in the increase in femoral BMD between the bisphosphonate and denosumab groups in this study.
Regarding bone metabolic markers, TRACP-5b, a bone resorption marker, and total P1NP, a bone formation marker, were suppressed by both bisphosphonates and denosumab. Eastell et al. reported increased bone metabolism and resorption markers after treatment with AI alone [34]. Brown et al. evaluated the effects of bisphosphonates and denosumab on bone metabolic markers in patients with general osteoporosis. They reported that although both drugs significantly decreased bone metabolic markers, the effect of denosumab was more pronounced [35]. In this study, the effect of denosumab on metabolic markers was also more significant than that of bisphosphonates, indicating that the effect of denosumab is also significant in suppressing bone metabolic markers in patients with AIBL.
In patients with general osteoporosis, previous studies have revealed a treatment effect of bisphosphonates and denosumab on TBS and a difference in the effect of each treatment. In a study by Gregorio et al. that examined the 2 year change in TBS in patients with osteoporosis, denosumab significantly improved TBS by + 1.4% in patients treated with alendronic acid or risedronate and by + 2.8% in patients treated with denosumab [36]. Kang et al. also reported a significant increase in TBS changes over 2 years in denosumab-treated patients with postmenopausal osteoporosis compared with zoledronic acid-treated patients [37].
Meanwhile, regarding the effect of treatment on TBS in patients with AIBL, Rodríguez-Sanz et al. reported that TBS was maintained in the risedronate or alendronic acid-treated group compared with a 2.93% reduction in TBS in the untreated AIBL group over 5 years [27]. Additionally, Prasad et al. reported that changes in TBS over 2 years were − 2.35% in the placebo group and − 1.3% in the oral risedronate group, indicating that risedronate is effective in preventing a decrease in TBS in patients with AIBL [38].
Antonini et al. also retrospectively investigated changes in TBS in patients with AIBL and reported that denosumab significantly increased TBSs; however, treatment with bisphosphonate did not significantly change TBS [39].
In the present study, no significant difference in TBS was observed between bisphosphonates and denosumab after 24 months of treatment in patients with AIBL. The reasons for the differences between the present study and the study by Antonini et al. may be due to differences in sample size, race, and TBS baselines. The median TBS in the present study is lower than that of Antonini et al. for both denosumab and bisphosphonate. Gregorio et al. reported that lower TBS may disrupt bone bridge continuity and make it more difficult to improve TBS [36], which may have caused this study to differ from Antonini et al. However, similar to the previous study, both drugs suppressed the decrease in TBS at 24 months after treatment. The change in TBS with bisphosphonates and denosumab was a temporary decrease at 6 months, followed by a gradual increase to an increase exceeding pre-treatment levels at 24 months, which suggests that long-term treatment would further increase TBS.
Differential effects of denosumab and bisphosphonate on TBS may be due to different mechanisms. Specifically, denosumab may preserve the trabecular microstructure by preventing plate perforation and preserving axially aligned trabeculae [40]. It may further improve the trabecular microstructure by preserving modeling-based bone formation despite its potent inhibition of remodeling [41].
One recent study showed that, compared with BMD, TBS does not decrease as rapidly after menopause, but TBS reduction is accelerated in postmenopausal women taking AI agents [42]. Bone loss induced by AI agents is more rapid and more severe than the bone loss that occurs in postmenopausal osteoporosis, and bone quality may be significantly affected by AI therapy.
As inferred from previous studies, the effect of bisphosphonate preparations in improving TBS in patients with osteoporosis in general is attenuated in AIBL, with only a reduction in TBS. In the present study, oral bisphosphonate and denosumab were able to maintain stable TBSs throughout the 2 year treatment period of AI, counteracting the negative effects of AI agents on bone quality.
Consequently, AI agents may affect bone microstructure, and clinically, not only BMD but also bone quality should be assessed. Kaldar et al. reported an independent reduction in BMD and TBS in patients with breast cancer treated with the AI agent exemestane [43]. Thus, assessment of TBS should be performed to evaluate fracture risk and monitor patients receiving AIBL treatment.
This study had some limitations despite obtaining important results. These include the single-center retrospective study design, the lack of randomized selection of patients, missing data, and the short follow-up period of 24 months. This retrospective design and analysis were undertaken for exploratory purposes. Therefore, the problem of patients not being randomized or missing data was inevitable. We believe that larger cohort studies are needed to confirm the findings of this study because the retrospective analysis lacked the accuracy of the results compared to a cohort study. In addition, internationally, DXA is often assessed at L1–L4 in the lumbar spine, whereas in Japan, it is often assessed at L2–L4. Although it is preferable to assess at L1–L4 when directly comparing with other international studies, we believe that this study is also valuable.
Despite these limitations, this is the first study to compare denosumab and bisphosphonates in Japanese patients with breast cancer and to show that denosumab may reduce the decline in TBS better than bisphosphonates. We plan to confirm the validity of this study by accumulating more cases in the future.
References
National Comprehensive Cancer Network clinical practice guidelines in oncology (2023) Breast Cancer. Version 4. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
Chien AJ, Goss PE (2006) Aromatase inhibitors and bone health in women with breast cancer. J Clin Oncol 24:5305–5312
Body JJ (2012) Aromatase inhibitors-induced bone loss in early breast cancer. Bon Key Rep 1:201
Waqas K, Ferreira JL, Tsourdi E, Body JJ, Hadji P, Zillikens MC (2021) Update guidance on the management of cancer treatment-induced bone loss (CTIBL) in pre- and postmenopausal women with early-stage breast cancer. J Bone Oncol 28:1–11
Fukumoto S, Soen S, Taguchi T, Ishikawa T, Matsushima H, Terauchi M, Horie S, Yoneda T, Sugimoto T, Matsumoto T (2020) Management manual for cancer treatment-induced bone loss (CTIBL): position statement of the JSBMR. J Bone Miner Metab 38:141–144
Hadji P, Aapro MS, Body JJ, Gnant M, Brandi ML et al (2017) Management of aromatase inhibitor-associated bone loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: Joint position statement of the IOF, CABS, ECTS, IEG, ESCEO IMS, and SIOG. J Bone Oncol 23:1–12
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2015) Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomized trials. Lancet 386:1353–1361
Suarez-Almazor ME, Herrera R, Lei X, Chavez-MacGregor M, Zhao H, Giordano SH (2020) Survival in older women with early stage breast cancer receiving low-dose bisphosphonates or denosumab. Cancer 126:3929–3938
Chen J, Zhang X, Lu Y, Zhang T, Ouyang Z, Sun Q (2021) Optimal duration of endocrine therapy with extended aromatase inhibitors for postmenopausal patients with hormone recepter-positive breast cancer: a meta-analysis. Breast Cancer 28:630–643
Goldvaser H, Barnes TA, Seruga B, Cescon DW, Ocana A, Ribnikar D (2018) Toxicity of extended adjuvant therapy with aromatase inhibitors in early breast cancer: a systematic review and meta-analysis. J Natl Cancer Inst 110:31–39
Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KA, Giordano SH, Hudis CA, Solky AJ, Stearns V, Winer EP, Griggs JJ (2019) Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Ciln Oncol 37:423–438
Sire A, Lippi L, Venetis K, Morganti S, Sajjadi E, Curci C, Ammendolia A, Criscitiello C, Fusco N, Invernizzi M (2022) Efficacy of antiresorptive drugs on bone mineral density in post-menopausal women with early breast cancer receiving adjuvant aromatase inhibitors: a systematic review of randomizes controlled trials. Front Oncol 11:829875
NIH Consensus Development Panel on Osteoporosis Prevention Diagnosis, and Therapy (2021) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Silva BC, Leslie WD, Resch H, Olivier L, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res 29:518–530
Martineau P, Leislie WD (2017) Trabecular bone score (TBS): method and applications. Bone 104:66–72
Ulivieri FM, Silva BC, Sardanelli F, Hans D, Bilezikian JP, Caudarella R (2014) Utility of the trabecular bone score (TBS) in secondary osteoporosis. Endocrine 47:435–448
Mamounas EP, Bandons H, Lembersky BC, Jeong JH, Geyer CE, Rastogi P (2019) Use of letrozole after aromatase inhibitor-based therapy in postmenopausal breast cancer (NRG Oncology/NSABP B-42): a randomized, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 20:88–99
Van Poznak C, Hannon RA, Mackey JR, Campone M, Apffelstaedt JP, Clack G, Barlow D, Makris A, Eastell R (2010) Prevention of aromatase inhibitor-induced bone loss using risedronate : the SABRE trial. J Clin Oncol 28:967–975
Markopoulos C, Tzoracoleftherakis E, Koukouras D, Venizelos B, Zobolas V, Misitzis J, Xepapadakis G, Gogas H (2012) Age effect on bone mineral density changes in breast cancer patients receiving anastrozole: results from the ARBI prospective clinical trial. J Cancer Res Cln Oncol 138:1569–1577
Greenspan SL, Vujevich KT, Brufsky A, Lembersky BC, van London GJ, Jankowitz RC, Puhalla SL, Rastogi P, Perera S (2015) Prevention of bone loss with resedronate in breast cancer survivors: a randomized, controlled clinical trial. Osteoporos Int 26:1857–1864
Ellis GK, Bone HG, Chlebowski R, Paul D, Spadafora S, Smith J, Fan M, Jun S (2008) Randomized trial of denosumab in patients receiving adjuvant aromatase inhibitors for nonmetastatic breast cancer. J Clin Oncol 26:4875–4882
Pineda-Moncusi M, Garcia-Giralt N, Diez-Perez A, Servitja S, Tusquets I, Prieto-Alhambra D (2019) Increased fracture risk in women treated with aromatase inhibitors versus tamoxifen: beneficial effect of bisphosphonates. J Bone Miner Res 34:632–642
Gnant M, Pfeiler G, Dubsky PC, Hubalek M, Greil R et al (2015) Austrian breast and colorectal cancer study group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicentre, randomized, double-blind, placebo-controlled trial. Lancet 386:433–443
Miyashita H, Satoi S, Kuno T, Cruz C, Malamud S, Kim SM (2020) Bone modifying agents for bone loss in patients with aromatase inhibitors as adjuvant treatment for breast cancer; insights from a network meta-analysis. Breast Cancer Res Treat 181:279–289
Sestak I, Blake GM, Patel R, Coleman RE, Cuzick J, Eastell R (2019) Comparison of risedronate versus placebo in preventing anastrozole-induced bone loss in women at high risk of developing breast cancer with osteopenia. Bone 124:83–88
Hopson MB, Onishi M, Awad D, Buono D, Maurer M, Crew KD, Shane E, Hershman DL, Kalinsky K (2020) Prospective study evaluating changes in bone quality in premenopausal women with breast cancer undergoing adjuvant chemotherapy. Clin Breast Cancer 20:327–333
Rodríguez-Sanz M, Pineda-Moncusí M, Servitja S, Garcia-Giralt N, Martos T, Tusquets I, Martínez-García M, Rodriguez-Morera J, Diez-Perez A, Albanell J, Nogues X (2016) TBS and BMD at the end of AI-therapy: a prospective study of the B-ABLE cohort. Bone 92:1–8
Barthe N, Braillon P, Ducassou D, Basse-Cathakinat B (1997) Comparison of two hologic DXA systems (QDR 1000 and QDR 4500/A). Br J Radiol 70:728–739
Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, Kushida K, Miyamoto S, Soen S, Nishimura J, Oh-Hashi Y, Hosoi T, Gorai I, Tanaka H, Igai T, Kishimoto H (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Mariotti V, Page DB, Davydov O, Hans D, Hudis CA, Patil S, Kunte S, Girotra M, Farooki A, Fornier MN (2016) Assessing fracture risk in early stage breast cancer patients treated with aromatase-inhibitors: an enhanced screening approach incorporating trabecular bone score. J Bone Oncol 18:32–37
Nunes FAP, de Faris MLF, Oliveira FP, Neto LV, Lima LFC, de Paula Paranhos Neto F, de Mendonca LMC, Madeira M (2021) Use of aromatase inhibitors in patients with breast cancer is associated with deterioration of bone microarchitecture and density. Arch Endocrinol Metab 65:505–511
Hong AR, Kim JH, Lee KH, Kim TY, Im SA, Kim TY, Moon HG, Han WS, Noh DY, Kim SW, Shin CS (2017) Long-term effect of aromatase inhibitors on bone microarchitecture and microarchitecture in non-osteoporotic postmenopausal women with breast cancer. Osteoporos Int 28:1413–1422
Nakatsukasa K, Koyama H, Ouchi Y, Ono H, Sakaguchi K et al (2019) Collaborative study group of scientific research of the japanese breast cancer society. Japanese women receiving adjuvant aromatase inhibitors for non-metastatic breast cancer: 24 month results. Breast Cancer 26:106–112
Eastell R, Hannon RA, Cuzick J, Dowsett M, Clack G, Adams JE (2006) Effect of an aromatase inhibitor on BMD and bone turnover markers: 2 year results of the anastrozole, tamoxifen, alone or in combination (ATAC) trial (18233230). J Bone Miner Res 21:1215–1223
Brown JP, Prince RL, Deal C, Recker RR, Kiel DP, de Gregorio LH, Hadji P, Hofbauer LC, Alvalo-Gracia JM, Wang H, Austin M, Wagman RB, Newmark R, Libanati C, Martin JS, Bone HG (2009) Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. J Bone Miner Res 24:153–161
Gregorio SD, Rio LD, Rodriguez-Tolra J, Bonel E, Garcia M, Winzenrieth R (2015) Comparison between different bone treatments on areal bone mineral density (aBMD) and bone microarchitectural texture as assessed by the trabecular bone score (TBS). Bone 75:138–143
Kang T, Park SY, Lee SH, Park JH, Suh SW (2022) Comparison of denosumab and zoledronic acid in postmenopausal women with osteoporosis: bone mineral density (BMD) and trabecular bone score (TBS). J Korean Med Sci 37:e68
Prasad C, Greenspan SL, Vujevich KT, Brufsky A, Lembersky BC, van London GJ, Jankowitz RC, Puhalla SL, Rastogi P, Perera S (2016) Risedronate may preserve bone microarchitecture in breast cancer survivors on aromatase inhibitors: a randomized, controlled clinical trial. Bone 90:123–126
Antonini S, Pedersini R, Birtolo MF, Baruch NL, Carrone F, Jaafar S, Ciafardini A, Cosentini D, Lagana M, Torrisi R, Farina D, Leonardi L, Balzarini L, Vena W, Bossi AC, Zambelli A, Lania AG, Berruti A, Mazziotti G (2024) Denosumab improves trabecular bone score in relationship with decrease in fracture risk women exposed to aromatase inhibitors. J Endocrinol Invest 47:433–442
Dempster DW, Chines A, Bostrom MP, Nieves JW, Zhou H, Chen L, Pannacciulli N, Wagman RB, Cosman F (2020) Modeling-based bone formation in the human femoral neck in subjects treated with denosumab. J Bone Miner Res 35:1282–1288
Hu YJ, Chines A, Shi Y, Seeman E, Guo XE (2022) The effect of denosumab and alendronate on trabecular plate and rod microstruvture at the distal tibia and radius: a post-hoc HR-pQCT study. Bone 154:116187
Pedrazzoni M, Casola A, Verzicco I, Abbate B, Vescovini R, Sansoni P (2014) Longitudinal changes of trabecular bone score after estrogen deprivation: effect of menopause and aromatase inhibition. J Endocrinol Invest 37:871–874
Kalder M, Hans D, Kyvernitakis I, Lamy O, Bauer M, Hadji P (2014) Effects of exemestane and tamoxifen treatment on bone texture analysis assessed by TBS in comparison with bone mineral density assessed by DXA in women with breast cancer. J Clin Densitom 17:66–71
Acknowledgements
This work was conducted independently without financial support from companies or funds. We acknowledge Yokohama City University Medical Center and all the patients with breast cancer who participated in the study. We thank Assistant Professor Dr. Yusuke Saigusa from the Department of Biostatistics, Yokohama City University, for providing appropriate advice in statistical analysis. We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Contributions
EO designed the study and wrote the initial draft of the manuscript. SS, TT, and HY contributed to the analysis and interpretation of the data and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation and critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any potential conflict of interest associated with this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Onuma, E., Saito, S., Tsuburai, T. et al. Effect of bisphosphonate and denosumab treatment on TBS in Japanese breast cancer patients with AIBL. J Bone Miner Metab (2024). https://doi.org/10.1007/s00774-024-01542-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00774-024-01542-2