Abstract
Purpose
Trabecular bone score (TBS) is a gray-level textural metric that has shown to correlate with risk of fractures in several forms of osteoporosis. The value of TBS in predicting fractures and the effects of bone-active drugs on TBS in aromatase inhibitors (AIs)-induced osteoporosis are still largely unknown. The primary objective of this retrospective study was to assess the effects of denosumab and bisphosphonates (BPs) on TBS and vertebral fractures (VFs) in women exposed to AIs.
Methods
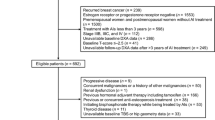
241 consecutive women (median age 58 years) with early breast cancer undergoing treatment with AIs were evaluated for TBS, bone mineral density (BMD) and morphometric VFs at baseline and after 18–24 months of follow-up. During the study period, 139 women (57.7%) received denosumab 60 mg every 6 months, 53 (22.0%) BPs, whereas 49 women (20.3%) were not treated with bone-active drugs.
Results
Denosumab significantly increased TBS values (from 1.270 to 1.323; P < 0.001) accompanied by a significant decrease in risk of VFs (odds ratio 0.282; P = 0.021). During treatment with BPs, TBS did not significantly change (P = 0.849) and incidence of VFs was not significantly different from women untreated with bone-active drugs (P = 0.427). In the whole population, women with incident VFs showed higher decrease in TBS vs. non-fractured women (P = 0.003), without significant differences in changes of BMD at any skeletal site.
Conclusions
TBS variation predicts fracture risk in AIs treated women. Denosumab is effective to induce early increase of TBS and reduction in risk of VFs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most prevalent cancer worldwide [1]. Since cancer’s cells can express estrogen receptors, hormone-deprivation therapies with aromatase inhibitors (AIs) are frequently used as adjuvant therapy of non-metastatic breast cancer, with favorable effects in preventing recurrences and increasing patient’s survival [2, 3]. However, AIs can also induce a progressive deterioration of bone strength with consequent increased risk of fragility fractures in several subjects exposed to AI therapy [4].
Prediction of fractures in women exposed to AIs could be a challenge. Although BMD is a valid surrogate of bone strength in post-menopausal women, in several forms of secondary osteoporosis the diagnostic value of this tool is limited due to predominant alterations in bone quality that could not be captured by dual-energy X-ray absorptiometry (DXA) measurement of BMD [5]. Indeed, bone loss induced by hormone-deprivation therapies is more rapid and severe than that occurring in post-menopausal osteoporosis and bone quality is affected more than bone quality by AI therapy [6]. In this scenario, additional DXA indexes have been developed eventually to improve fracture risk prediction [7]. Trabecular bone score (TBS) is a textural index automatically derived from DXA lumbar spine scan that evaluates local grey-level variations with an experimental variogram of two-dimension projections [8]. This DXA-derived parameter shows a good correlation with vertebral microstructure [9]. As a matter of fact, usefulness of TBS as a predictive tool for fractures in post-menopausal osteoporosis has been demonstrated [10]. Similarly, TBS has been proposed as a reliable and feasible tool in characterizing the alterations in bone quality and predicting fractures in several forms of secondary osteoporosis [5]. However, the effects AIs on TBS resulted to be variable and the impact of TBS degradation on risk of fractures in this clinical setting has not been so far clarified [11,12,13].
Bisphosphonates (BPs) and denosumab are recommended to prevent bone loss and fractures in women treated with AIs [2, 14]. Data available in literature on therapeutic outcomes of these drugs in AI-induced osteoporosis were mainly focused on BMD and more recently on vertebral fractures (VFs), whereas data on TBS changes during BPs or denosumab therapy in women exposed to AIs are scarce and inconclusive [11,12,13].
In this retrospective study, reflecting real-life clinical practice, we aimed at investigating the performance of TBS in predicting VFs and the effects denosumab and BPs on TBS in women under treatment with AIs.
Materials and methods
This study followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [15]. The inclusion criteria were: (1) hormone receptor-positive early breast cancer with indication to AIs (either alone or in combination to GnRH agonists) in adjuvant setting; (2) at least two out-patient visits during a 18–24-month follow-up; (3) duration of hormone-deprivation therapy < 12 months at the time of first visit; (4) availability of DXA analyses longitudinally performed by the same machine during the follow-up; (5) availability of two spine images (either by X-rays or DXA) for vertebral morphometry during the follow-up; (6) written informed consent. The exclusion criteria were: (1) bone metastases; (2) treatment with bone-active drugs (except for calcium and vitamin D) prior to and at time of first DXA examination; (3) spinal surgery; (4) renal insufficiency; (5) liver disease.
Two hundred and forty-one consecutive women with breast cancer, evaluated for skeletal health at out-patient bone clinics in the period between September 2020 and January 2023 and meeting the inclusion and exclusion criteria were retrospectively enrolled in the study. For the study purposes, all participants were assessed two times during 18–24 months of follow-up. The database was locked on February 20th 2023 and data analysis was completed by February 28th 2023.
During the study period, the therapeutic decision making for prevention of fractures was based on national guidelines, current Italian regulation for drug reimbursement, patient’s preference, comorbidities and overall clinical judgment [16]. National guidelines and Italian regulation for drug reimbursement allow to treat all subjects undergoing hormone-deprivation therapies regardless of BMD and WHO Fracture Risk Assessment (FRAX) scores, but in our study treatment with bone-active drugs was decided on an individual basis when T-score was above -1.0 SD and there were not coexistent traditional major risk factors for fractures, due to controversy in defining the optimal therapeutic threshold in these specific conditions [2, 14, 16,17,18]. Moreover, the choice of BPs or denosumab was shared with patients who were informed about effectiveness and risk profile of each drug.
The primary aim of the study was to assess the effects of bone-active drugs (BPs and denosumab) on TBS in women treated with AIs for breast cancer. As secondary end-points, we explored the (1) association between changes in TBS and risk of VFs; (2) differences in TBS changes between denosumab and BPs.
The study was approved by the Ethics Committee of IRCCS Humanitas Research Hospital and the patients gave their informed consent to use the clinical data for research purposes.
Assessment of VFs
VFs were assessed in all 241 patients at first out-patient visit and after 18–24 months of follow-up by a quantitative morphometric assessment using DXA (Hologic Inc, USA) images (152 cases) or conventional spine X-rays radiographs (89 cases) [19, 20]. Six points were manually marked on each vertebral body to describe the vertebral shape. Anterior (Ha), middle (Hm), and posterior (Hp) vertebral heights were measured and height ratios (Ha/Hp, Ha/Hm, Hm/Hp) were calculated for each vertebra from T4 to L4. According to the quantitative morphometry method, the fractures were defined as mild, moderate, and severe based on height ratio decreases of 20–25%, 25–40%, and more than 40%, respectively [21]. Incident VFs were defined as either new fractures (the same vertebrae from no VF at baseline to any grade of VF at follow-up) or progression of pre-existing VFs (from mild to moderate/severe VFs or from moderate to severe VFs between baseline and the follow-up). Spine deformity index (SDI) was calculated by summing the score of each VF after the grade of the fracture (score 1, 2, or 3 for mild, moderate, and severe fractures, respectively) was assigned [22]. Assessment of VFs was retrospectively performed by two observers, who were blinded to the identity of patients.
DXA measurement of BMD and TBS
All subjects were evaluated at the time of first out-patient visit and after 18–24 months of follow-up by DXA (Hologic Inc, USA) measurement of BMD at lumbar spine, femoral neck and total hip. BMD was expressed as T-score, comparing the results with those obtained in a gender-matched Caucasian population at the peak of bone mass [23]. A T-score less than or equal to − 2.5 SD at the hip or spine was defined as osteoporosis, whereas osteopenia was defined as a T-score between − 1 and − 2.5 SD.
TBS was measured in all subjects using lumbar spine DXA images. Based on results of a meta-analysis, subjects were categorized as with degraded TBS when the values were ≤ 1.230 [24].
Assessment of FRAX score
The fracture risk was assessed in 230 women with age ≥ 40 years by the FRAX tool (FRAX® tool) using the online calculator (www.shef.ac.uk/FRAX) with the information collected at the first visit. The calculation of FRAX score was performed including BMD values of women and considering AI therapy as a cause of secondary osteoporosis [25].
Measurement of body mass index (BMI)
BMI was defined by the individual’s weight in kilograms divided by the square of their height in meters. Underweight, overweight and obese were defined by BMI < 18.5 kg/m2, 25–30 kg/m2 and ≥ 30 kg/m2, respectively.
Assessment of vitamin D status
Hypovitaminosis D was defined by serum 25-hydroxy-vitamin D [25(OH)-vitamin D] below 30 ng/ml [26]. Measurement of 25(OH)-vitamin D was not centralized using commercial kits.
Statistical analysis
Normally distributed continuous data, as assessed by Kolmogorov–Smirnov’s test, were presented as mean and 95% confidence interval (95% CI) of the mean, whereas non-normally distributed data were presented as median and range. Categorical data were presented as number and percentage. Unpaired and paired normally distributed data were compared using t-test and ANOVA, with Bonferroni’s corrections. Non-normally distributed parameters were compared by Wilcoxon’s, Mann–Whitney’s and Kruskal–Wallis’ tests, for paired, un-paired and multiple comparisons, respectively. Unpaired and paired frequencies were compared using the Chi-square and McNemar’s tests, respectively. Determinants of incident VFs were assessed by univariate logistic regression analysis. All risk factors significantly associated with incident VFs in the univariate analysis were then submitted to multivariate logistic regression analyses taking into account the first end-point of the study and the minimal guidance criterion of ten events per variable [27]. A P < 0.05 was considered as significant.
Data availability
The datasets generated and analyzed during the current study are available in the ZENODO repository.
Results
Baseline
Ninety-five women (39.4%) were in early post-menopausal phase (< 5 years), and the mean age of the subjects in the whole population was 58.7 years (95% CI 57.2–60.2; range: 30–81). At time of the first visit, all women with estrogen receptor-positive breast cancer were treated with AIs (in combination with gonadotropin-releasing hormone agonist in 35 cases) for less than 12 months, with 79 women (32.8%) being also treated with adjuvant chemotherapy and 29 women (12.0%) also receiving trastuzumab (Table 1).
At time of the first visit, 66 women (27.4%) had osteoporosis, whereas osteopenia and normal BMD at all skeletal sites were found in the remaining 111 (46.1%) and 64 (26.6%) women, respectively. At this time-point, morphometric VFs were diagnosed in 29 women (12.0%), with a median SDI of 2 (range: 1–3). No significant difference in prevalent VFs was found between evaluations performed on DXA and spine X-ray images (11.2% vs. 13.5%; P = 0.597). TBS was degraded in 84 women (34.9%), the prevalence being higher in subjects with morphometric VFs as compared to those without VFs (69.0% vs. 30.2%; P < 0.001).
At time of the first visit, all 241 women were taking cholecalciferol already prescribed by the oncologists after diagnosis of breast cancer. In 132 women, cholecalciferol was combined with calcium carbonate (120 cases) or calcium citrate (12 cases). At this time, hypovitaminosis D was diagnosed in 97 out of 241 women notwithstanding vitamin D supplementation. After the first visit at the out-patient bone clinic, 72 women with persistent hypovitaminosis increased their cholecalciferol doses, whereas in 25 women with hypovitaminosis D cholecalciferol was replaced with calcifediol. The remaining 144 women continued with unchanged cholecalciferol doses.
After the first visit, 139 women (57.7%) started denosumab 60 mg subcutaneously every 6 months, 53 (22.0%) were treated with BPs, 48 with oral BPs (alendronate 70 mg/week or risedronate 35 mg/week or risedronate 75 mg for two consecutive days/month) and 5 with intravenous zoledronate [5 mg/12 months], whereas 49 women (20.3%) were not treated with bone-active drugs because of patient preference, contraindications and/or clinical judgment.
Women treated with BPs were significantly older than those treated with denosumab (P = 0.011) and those who were not treated with bone-active drugs (P = 0.030) (Table 1). No significant differences in baseline BMI, BMD at any skeletal site, TBS, FRAX score, prevalent VFs and adjuvants therapies for breast cancer were found among the three therapeutic groups (Table 1).
Effects of bone-active drugs on skeletal end-points
The median range of follow-up was 18 months (range 18–24). During follow-up, treatment with denosumab induced a significant increase in lumbar spine, femoral neck and total hip BMD, while treatment with BPs reached a significant increase only in total hip BMD. Patients who were not treated with bone-active drugs had a significant decrease of BMD at all skeletal sites (supplemental Table 1).
During follow-up, treatment with denosumab induced a significant increase in TBS values (from 1.270, 95% CI 1.248–1.291 to 1.323, 95% CI 1.300–1.346; P < 0.001) (Fig. 1) with a significant decrease in the number of subjects with degraded TBS (from 52/139 to 37/139; P = 0.001) (Fig. 2). Conversely, TBS values decreased significantly (P = 0.009) in subjects who were not treated with bone-active drugs, whereas they did not change significantly (P = 0.849) in subjects treated with BPs (Fig. 1).
During follow-up, 17 women (7.1%) experienced incident VFs. The incidence of VFs was significantly higher in women untreated with bone-active drugs as compared to those treated with denosumab (14.3% vs. 3.6%; P = 0.008), whereas the difference vs. women treated with BPs was not significantly different (14.3% vs. 9.3%; P = 0.427). Incident VFs was significantly higher in obese and overweight women as compared to those with normal BMI (14.7% vs. 9.2% vs. 2.9%; obese vs. overweight vs. normal BMI, respectively; P = 0.040). No significant difference in incident VFs was found among women with baseline osteoporosis vs. those with osteopenia or normal BMD (P = 0.311). Women with incident VFs showed higher decrease in TBS during the follow-up (Fig. 3a) as compared to women who did not fracture, without significant differences in changes of BMD at lumbar spine (Fig. 3b) and total hip (Fig. 3c). In the univariate logistic regression analysis, risk of incident VFs was significantly associated with higher BMI, pre-existing VFs and greater decrease in total hip BMD and TBS during the follow-up, and resulted to be significantly decreased by denosumab treatment (Table 2). In the multivariate analyses, decrease in TBS maintained the significant association with risk of incident VFs independently of BMI, pre-existing VFs, denosumab treatment and change in total hip BMD (Table 2).
Changes in trabecular bone score (TBS) (A), bone mineral density (BMD) at lumbar spine (B) and total hip (C) in women exposed to aromatase inhibitors therapy stratified according to incident vertebral fractures (VFs). Data are presented as median, 25th and 75th percentile and range and comparisons were performed by Mann–Whitney’s test
At follow-up, all women had serum 25(OH)-vitamin D values above 30 ng/ml.
Discussion
In this retrospective study reflecting the real-life clinical practice, decrease in TBS was significantly associated with high risk of incident VFs during only 2 years of treatment with AIs in women with early breast cancer, independently of age, BMI, pre-existing fractures and changes in BMD. Treatment with denosumab induced concomitant increase in TBS and decrease in incident VFs, whereas BPs did not induce relevant effects on these therapeutic outcomes.
VFs are the hallmark of both primary and secondary osteoporosis and they represent the most frequent fragility fractures with relevant impact on quality of life and risk of future fractures [28, 29]. Our study confirms that VFs are a frequent and early complication of AI therapy and provides a further evidence that fractures could occur even in women with baseline normal BMD and low FRAX score [7, 18, 30]. Indeed, prediction of fractures in women exposed to AIs could be a challenge and the optimal therapeutic threshold has not been so far defined [17, 18]. Our study suggests that TBS might be used as a tool for identifying subjects at higher risk of VFs during the first years of AI therapy. In fact, TBS decreased early in women exposed to AIs and the TBS changes significantly correlated with the risk of morphometric VFs independently of other potential determinants of fractures, such as older age and pre-existing fractures.
There is evidence that anti-resorptive drugs can induce favorable effects on TBS concomitantly to the increase in BMD and reduction of fracture risk in women with post-menopausal osteoporosis [31,32,33,34]. In women exposed to AI therapy, treatment with oral BPs was shown to prevent the impairment of TBS induced by hormone-deprivation therapy [35, 36]. Consistently, in our study, oral BPs enabled to maintain stable TBS values during 2-year treatment with AIs, counteracting the negative effects of hormone-deprivation therapy on bone quality (i.e., TBS decreased significantly in women not treated with bone-active drugs). However, the favorable effect of oral BPs was not accompanied by a significant decrease in risk of VFs, likely because a longer follow-up could be required for the anti-fracture effectiveness of these drugs [37]. Noteworthy, the effects of denosumab resulted to be more clinically relevant than oral BPs. In fact, denosumab induced significant improvement in TBS in close relationship with decrease in risk of VFs. The effect of denosumab on TBS is consistent with previous observation that parameters of bone structure and elasticity as evaluated by phalangeal quantitative ultrasound of bone improved during treatment with this drug in women exposed to AIs for breast cancer [12]. The effect on bone quality, that is expected for anabolic drugs, seems indeed to be peculiar of denosumab in the context of anti-resorptive drugs. Specifically, denosumab may preserve trabecular microstructure by preventing plate perforation and preserving axially aligned trabeculae [38]. Denosumab may further improve trabecular microstructure by preserving modeling-based bone formation despite its potent inhibition of remodeling [39]. Interestingly, these effects of denosumab on bone quality occurred in our women after only 18–24 months of treatment, consistent with the hypothesis that this drug enables to reduce the imminent risk of fracture [37].
In the general population, low BMI is a well-recognized risk factor for fractures while higher BMI might have a beneficial effect [40]. Conversely, in our women under AI therapy, most of VFs occurred in overweight or obese cases. This result is in agreement with previous studies reporting high prevalence of VFs in women with high body fat mass under AI therapy [41, 42], consistent with the hypothesis that increased adiposity might produce invariably detrimental effects on the skeleton exposed to AI therapy due to annihilation of estrogen production induced by the inhibitory action of the drugs on aromatase enzyme in adipose tissue [17]. Therefore, overweight/obese subjects from being protected in basal conditions become at high risk of bone fragility fractures after starting AIs. It is interesting to note that the negative predictive effect of BMI on fracture risk is maintained even in a population treated with bone resorption inhibitors.
This study has some limitations. The lack of a control group of women not treated with AIs did not allow to clarify whether anti-resorptive drugs maintain in the AI-induced osteoporosis the same effectiveness already reported in post-menopausal osteoporosis. The study was retrospective but DXA evaluations of TBS were performed by the same machine. Moreover, the study was observational and adjudication process of treatment was not randomized but physician dependent. However, the study was designed to provide information on TBS changes during treatment with bone-active drugs in the real-life clinical practice. The assessment of VFs was performed by two methods, but as already demonstrated by others [43], we did not find differences between assessment of VFs on DXA and spinal radiographs images. Patients were followed up for 24 months or less, not allowing to investigate the long-term effects of AIs and bone-active drugs on TBS. Another limitation of study was the lack of data on biochemical markers of bone turnover which might have been useful in identifying early subjects with more severe bone loss, guiding the choice of anti-osteoporotic drugs and monitoring the therapeutic effectiveness [44, 45]. Lack of information on body composition did not allow to investigate the relationship between TBS and visceral adiposity that could induce direct negative effects on bone quality especially in the context of hormone deprivation [46, 47]. Moreover, the missing data on body composition and regional distribution of fat and lean mass do not allow to exclude a possible interference of regional soft tissue noise on the DXA images and eventually in the gray-level texture [48]. Indeed, there is recent evidence that denosumab can improve TBS in post-menopausal osteoporosis even when the parameter was corrected by regional soft tissue thickness [49].
In conclusion, this study showed for the first time how in real-life clinical practice, TBS variations correlate with fracture risk in women treated with AIs, and denosumab is effective to induce a clinically relevant increase in TBS associated with a significant reduction in risk of VFs after only 2-year follow-up. These findings provide a strong rationale for including DXA measurement of TBS in the diagnostic and therapeutic workup of women exposed to estrogen-deprivation therapies.
Change history
09 October 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40618-023-02208-y
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Hadji P, Aapro MS, Body JJ, Gnant M, Brandi ML, Reginster JY, Zillikens MC, Glüer CC, de Villiers T, Baber R, Roodman GD, Cooper C, Langdahl B, Palacios S, Kanis J, Al-Daghri N, Nogues X, Eriksen EF, Kurth A, Rizzoli R, Coleman RE (2017) Management of aromatase inhibitor-associated bone Loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: joint position statement of the IOF, CABS, ECTS, IEG, ESCEO IMS, and SIOG. J Bone Oncol 7:1–12. https://doi.org/10.1016/j.jbo.2017.03.001
EBCTCG (2015) Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 386(10001):1341–1352. https://doi.org/10.1016/S0140-6736(15)61074-1
Mazziotti G, Canalis E, Giustina A (2010) Drug-induced osteoporosis: mechanisms and clinical implications. Am J Med 123(10):877–884. https://doi.org/10.1016/j.amjmed.2010.02.028
Cianferotti L, Cipriani C, Corbetta S, Corona G, Defeudis G, Lania AG, Messina C, Napoli N, Mazziotti G (2023) Bone quality in endocrine diseases: determinants and clinical relevance. J Endocrinol Invest 46(7):1283–1304. https://doi.org/10.1007/s40618-023-02056-w
Hadji P (2009) Aromatase inhibitor-associated bone loss in breast cancer patients is distinct from postmenopausal osteoporosis. Crit Rev Oncol Hematol 69(1):73–82. https://doi.org/10.1016/j.critrevonc.2008.07.013
Pedersini R, Cosentini D, Rinaudo L, Zamparini M, Ulivieri FM, di Mauro P, Maffezzoni F, Monteverdi S, Vena W, Laini L, Amoroso V, Simoncini EL, Farina D, Mazziotti G, Berruti A (2023) Assessment of DXA derived bone quality indexes and bone geometry parameters in early breast cancer patients: a single center cross-sectional study. Bone Rep 18:101654. https://doi.org/10.1016/j.bonr.2023.101654
Krohn K, Schwartz EN, Chung YS, Lewiecki EM (2019) Dual-energy X-ray absorptiometry monitoring with trabecular bone score: 2019 ISCD Official Position. J Clin Densitom 22(4):501–505. https://doi.org/10.1016/j.jocd.2019.07.006
Hans D, Barthe N, Boutroy S, Pothuaud L, Winzenrieth R, Krieg MA (2011) Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom 14(3):302–312. https://doi.org/10.1016/j.jocd.2011.05.005
Palomo T, Muszkat P, Weiler FG, Dreyer P, Brandão CMA, Silva BC (2022) Update on trabecular bone score. Arch Endocrinol Metab 66(5):694–706. https://doi.org/10.20945/2359-3997000000559
Hong AR, Kim JH, Lee KH, Kim TY, Im SA, Kim TY, Moon HG, Han WS, Noh DY, Kim SW, Shin CS (2017) Long-term effect of aromatase inhibitors on bone microarchitecture and macroarchitecture in non-osteoporotic postmenopausal women with breast cancer. Osteoporos Int 28(4):1413–1422. https://doi.org/10.1007/s00198-016-3899-6
Catalano A, Gaudio A, Agostino RM, Morabito N, Bellone F, Lasco A (2019) Trabecular bone score and quantitative ultrasound measurements in the assessment of bone health in breast cancer survivors assuming aromatase inhibitors. J Endocrinol Invest 42(11):1337–1343. https://doi.org/10.1007/s40618-019-01063-0
Pedrazzoni M, Casola A, Verzicco I, Abbate B, Vescovini R, Sansoni P (2014) Longitudinal changes of trabecular bone score after estrogen deprivation: effect of menopause and aromatase inhibition. J Endocrinol Invest 37(9):871–874. https://doi.org/10.1007/s40618-014-0125-2
Shapiro CL, Van Poznak C, Lacchetti C, Kirshner J, Eastell R, Gagel R, Smith S, Edwards BJ, Frank E, Lyman GH, Smith MR, Mhaskar R, Henderson T, Neuner J (2019) Management of osteoporosis in survivors of adult cancers with nonmetastatic disease: ASCO clinical practice guideline. J Clin Oncol 37(31):2916–2946. https://doi.org/10.1200/jco.19.01696
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Rossini M, Adami S, Bertoldo F, Diacinti D, Gatti D, Giannini S, Giusti A, Malavolta N, Minisola S, Osella G, Pedrazzoni M, Sinigaglia L, Viapiana O, Isaia GC (2016) Guidelines for the diagnosis, prevention and management of osteoporosis. Reumatismo 68(1):1–39. https://doi.org/10.4081/reumatismo.2016.870
Dalla Volta A, Mazziotti G, Maffezzoni F, Grisanti S, Palumbo C, Pedersini R, Maroldi R, Berruti A (2020) Bone mineral density and FRAX score may not predict fracture risk in patients with cancer undergoing hormone deprivation therapies. J Clin Oncol 38(29):3363–3366. https://doi.org/10.1200/JCO.20.00434
Mazziotti G, Vena W, Pedersini R, Piccini S, Morenghi E, Cosentini D, Zucali P, Torrisi R, Sporeni S, Simoncini EL, Maroldi R, Balzarini L, Lania AG, Berruti A (2022) Prediction of vertebral fractures in cancer patients undergoing hormone deprivation therapies: reliability of who fracture risk assessment tool (frax) and bone mineral density in real-life clinical practice. J Bone Oncol 33:100421. https://doi.org/10.1016/j.jbo.2022.100421
Clark EM, Carter L, Gould VC, Morrison L, Tobias JH (2014) Vertebral fracture assessment (VFA) by lateral DXA scanning may be cost-effective when used as part of fracture liaison services or primary care screening. Osteoporos Int 25(3):953–964. https://doi.org/10.1007/s00198-013-2567-3
Griffith JF, Genant HK (2012) New advances in imaging osteoporosis and its complications. Endocrine 42(1):39–51. https://doi.org/10.1007/s12020-012-9691-2
Engelke K, Stampa B, Steiger P, Fuerst T, Genant HK (2019) Automated quantitative morphometry of vertebral heights on spinal radiographs: comparison of a clinical workflow tool with standard 6-point morphometry. Arch Osteoporos 14(1):18. https://doi.org/10.1007/s11657-019-0577-2
Crans GG, Genant HK, Krege JH (2005) Prognostic utility of a semiquantitative spinal deformity index. Bone 37(2):175–179. https://doi.org/10.1016/j.bone.2005.04.003
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International society for clinical densitometry position development conference on bone densitometry. J Clin Densitom 16(4):455–466. https://doi.org/10.1016/j.jocd.2013.08.004
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, Barkmann R, Boutroy S, Brown J, Chapurlat R, Elders PJM, Fujita Y, Glüer CC, Goltzman D, Iki M, Karlsson M, Kindmark A, Kotowicz M, Kurumatani N, Kwok T, Lamy O, Leung J, Lippuner K, Ljunggren Ö, Lorentzon M, Mellström D, Merlijn T, Oei L, Ohlsson C, Pasco JA, Rivadeneira F, Rosengren B, Sornay-Rendu E, Szulc P, Tamaki J, Kanis JA (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res 31(5):940–948. https://doi.org/10.1002/jbmr.2734
Adami G, Biffi A, Porcu G, Ronco R, Alvaro R, Bogini R, Caputi AP, Cianferotti L, Frediani B, Gatti D, Gonnelli S, Iolascon G, Lenzi A, Leone S, Migliaccio S, Nicoletti T, Paoletta M, Pennini A, Piccirilli E, Tarantino U, Brandi ML, Corrao G, Rossini M, Michieli R (2023) A systematic review on the performance of fracture risk assessment tools: FRAX, DeFRA, FRA-HS. J Endocrinol Investig. https://doi.org/10.1007/s40618-023-02082-8
Bertoldo F, Cianferotti L, Di Monaco M, Falchetti A, Fassio A, Gatti D, Gennari L, Giannini S, Girasole G, Gonnelli S, Malavolta N, Minisola S, Pedrazzoni M, Rendina D, Rossini M, Chiodini I (2022) Definition, assessment, and management of vitamin D inadequacy : suggestions, recommendations, and warnings from the Italian society for osteoporosis, mineral metabolism and bone diseases (SIOMMMS). Nutrients. https://doi.org/10.3390/nu14194148
Pavlou M, Ambler G, Seaman SR, Guttmann O, Elliott P, King M, Omar RZ (2015) How to develop a more accurate risk prediction model when there are few events. BMJ 351:h3868. https://doi.org/10.1136/bmj.h3868
Gates M, Pillay J, Nuspl M, Wingert A, Vandermeer B, Hartling L (2023) Screening for the primary prevention of fragility fractures among adults aged 40 years and older in primary care: systematic reviews of the effects and acceptability of screening and treatment, and the accuracy of risk prediction tools. Syst Rev 12(1):51. https://doi.org/10.1186/s13643-023-02181-w
Lu H, Lei X, Zhao H, Elting L, Siricilla M, Ursani MA, Giordano SH, Suarez-Almazor M (2021) Bone mineral density at the time of initiating aromatase inhibitor therapy is associated with decreased fractures in women with breast cancer. J Bone Miner Res 36(5):861–871. https://doi.org/10.1002/jbmr.4250
Mazziotti G, Pedersini R, Vena W, Cosentini D, Carrone F, Pigni S, Simoncini EL, Torrisi R, Zambelli A, Farina D, Balzarini L, Lania AG, Berruti A (2022) Real-world effectiveness of denosumab and bisphosphonates on risk of vertebral Fractures in women with breast cancer undergoing treatment with aromatase inhibitors. Calcif Tissue Int 111(5):466–474. https://doi.org/10.1007/s00223-022-01011-w
McClung MR, Lippuner K, Brandi ML, Zanchetta JR, Bone HG, Chapurlat R, Hans D, Wang A, Zapalowski C, Libanati C (2017) Effect of denosumab on trabecular bone score in postmenopausal women with osteoporosis. Osteoporosis Int 28(10):2967–2973. https://doi.org/10.1007/s00198-017-4140-y
Senn C, Günther B, Popp AW, Perrelet R, Hans D, Lippuner K (2014) Comparative effects of teriparatide and ibandronate on spine bone mineral density (BMD) and microarchitecture (TBS) in postmenopausal women with osteoporosis: a 2-year open-label study. Osteoporos Int 25(7):1945–1951. https://doi.org/10.1007/s00198-014-2703-8
Cosman F, Hans D, Shevroja E, Wang Y, Mitlak B (2023) Effect of abaloparatide on bone microarchitecture assessed by trabecular bone score in women with osteoporosis: post hoc analysis of ACTIVE and ACTIVExtend. J Bone Miner Res. https://doi.org/10.1002/jbmr.4764
Jeong C, Kim J, Lim Y, Ha J, Kang MI, Baek KH (2022) Effect of romosozumab on trabecular bone score compared to anti-resorptive agents in postmenopausal women with osteoporosis. J Bone Metab 29(4):279. https://doi.org/10.11005/jbm.2022.29.4.279
Rodríguez-Sanz MP-MM, Servitja S, Garcia-Giralt N, Martos T, Tusquets I, Martínez-García M, Rodriguez-M D-P, Albanell J, Nogués X (2016) TBS and BMD at the end of AI-therapy: a prospective study of the B-ABLE cohort. Bone 92:1–8. https://doi.org/10.1016/j.bone.2016.08.008
Prasad C, Greenspan SL, Vujevich KT, Brufsky A, Lembersky BC, van Londen GJ, Jankowitz RC, Puhalla SL, Rastogi P, Perera S (2016) Risedronate may preserve bone microarchitecture in breast cancer survivors on aromatase inhibitors: a randomized, controlled clinical trial. Bone 90:123–126. https://doi.org/10.1016/j.bone.2016.03.010
Iconaru LBF, Charles A, Mugisha A, Benoit F, Surquin M, Karmali R, Body JJ, Bergmann P (2021) Which treatment to prevent an imminent fracture? Bone Rep 15:101105. https://doi.org/10.1016/j.bonr.2021.101105
Hu YJ, Chines A, Shi Y, Seeman E, Guo XE (2022) The effect of denosumab and alendronate on trabecular plate and rod microstructure at the distal tibia and radius: a post-hoc HR-pQCT study. Bone 154:116187. https://doi.org/10.1016/j.bone.2021.116187
Dempster DW, Chines A, Bostrom MP, Nieves JW, Zhou H, Chen L, Pannacciulli N, Wagman RB, Cosman F (2020) Modeling-based bone formation in the human femoral neck in subjects treated with denosumab. J Bone Miner Res 35(7):1282–1288. https://doi.org/10.1002/jbmr.4006
De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16(11):1330–1338. https://doi.org/10.1007/s00198-005-1863-y
Pedersini R, Amoroso V, Maffezzoni F, Gallo F, Turla A, Monteverdi S, Ardine M, Ravanelli M, Vassalli L, Rodella F, Formenti AM, Dalla Volta A, Simoncini EL, Giustina A, Maroldi R, Berruti A (2019) Association of fat body mass with vertebral fractures in postmenopausal women with early breast cancer undergoing adjuvant aromatase inhibitor therapy. JAMA Netw Open 2(9):e1911080. https://doi.org/10.1001/jamanetworkopen.2019.11080
Monteverdi S, Pedersini R, Gallo F, Maffezzoni F, Dalla Volta A, Di Mauro P, Turla A, Vassalli L, Ardine M, Formenti AM, Simoncini EL, Giustina A, Maroldi R, Amoroso V, Berruti A (2021) The interaction of lean body mass with fat body mass is associated with vertebral fracture prevalence in women with early breast cancer undergoing aromatase inhibitor therapy. JBMR Plus 5(2):e10440. https://doi.org/10.1002/jbm4.10440
Diacinti D, Del Fiacco R, Pisani D, Todde F, Cattaruzza MS, Diacinti D, Arima S, Romagnoli E, Pepe J, Cipriani C, Minisola S (2012) Diagnostic performance of vertebral fracture assessment by the lunar iDXA scanner compared to conventional radiography. Calcif Tissue Int 91(5):335–342. https://doi.org/10.1007/s00223-012-9643-0
Confavreux CB, Fontana A, Guastalla JP, Munoz F, Brun J, Delmas PD (2007) Estrogen-dependent increase in bone turnover and bone loss in postmenopausal women with breast cancer treated with anastrozole. Prevention with bisphosphonates. Bone 41(3):346–352. https://doi.org/10.1016/j.bone.2007.06.004
Szulc P (2018) Bone turnover: biology and assessment tools. Best Pract Res Clin Endocrinol Metab 32(5):725–738. https://doi.org/10.1016/j.beem.2018.05.003
Vena W, Carrone F, Delbarba A, Akpojiyovbi O, Pezzaioli LC, Facondo P, Cappelli C, Leonardi L, Balzarini L, Farina D, Pizzocaro A, Lania AG, Mazziotti G, Ferlin A (2023) Body composition, trabecular bone score and vertebral fractures in subjects with Klinefelter syndrome. J Endocrinol Invest 46(2):297–304. https://doi.org/10.1007/s40618-022-01901-8
Dalla Volta A, Palumbo C, Zamboni S, Mazziotti G, Triggiani L, Zamparini M, Maffezzoni F, Rinaudo L, Bergamini M, Di Meo N, Caramella I, Valcamonico F, Borghetti P, Guerini A, Farina D, Antonelli A, Simeone C, Berruti A (2023) Heterogeneity in regional changes in body composition induced by androgen deprivation therapy in prostate cancer patients: potential impact on bone health-the BLADE study. J Endocrinol Invest. https://doi.org/10.1007/s40618-023-02150-z
Amnuaywattakorn S, Sritara C, Utamakul C, Chamroonrat W, Kositwattanarerk A, Thamnirat K, Ongphiphadhanakul B (2016) Simulated increased soft tissue thickness artefactually decreases trabecular bone score: a phantom study. BMC Musculoskelet Disord 17:17. https://doi.org/10.1186/s12891-016-0886-1
Hans D, Shevroja E, McDermott M, Huang S, Kim M, McClung M (2022) Updated trabecular bone score accounting for the soft tissue thickness (TBS(TT)) demonstrated significantly improved bone microstructure with denosumab in the FREEDOM TBS post hoc analysis. Osteoporos Int 33(12):2517–2525. https://doi.org/10.1007/s00198-022-06549-x
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare the following competing financial interests: Dr Pedersini received consultancy fees from Roche, Novartis, Eli Lilly, Daiichi Sankyo, Gilead, Eisai, Accord, outside the submitted work; Dr. Torrisi received research grants from Pfizer, consultancy fees from MSD and lecture fees from Pfizer, Eli Lilly, EISAI and Genomic Health outside the submitted work; Dr. Vena received grants from IBSA Pharmaceutical outside the submitted work; Dr. Zambelli received consultancy fees from Roche, Novartis, Pfizer, Eli Lilly & Co., AstraZeneca, Genomic Health outside the submitted work; Dr. Bossi received research grants from Novo-Nordisk, Eli Lilly, Bayer, Sanofi Italia and advisory board and consultancy fees from MSD, Alfasigma, Boehringer Ingelheim, Astra Zeneca, Mundipharma Italia, Pfizer outside the submitted work; Dr. Lania received grants from Pfizer and consultancy fees from Ipsen, outside the submitted work; Dr. Berruti reports receiving grants and personal fees from Janssen Cilag, grants and personal fees from Astellas, and personal fees from Bayer outside the submitted work; Dr. Mazziotti received consultancy fees from Novartis, Ipsen, Eli Lilly and lecture fees from Amgen and Abiogen, outside the submitted work.
Ethical approval and Research involving human participants and/or animals
The study was approved by the Ethics Committee of IRCCS Humanitas Research Hospital.
Consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and all participants gave their written informed consent.
Informed Consent
No Informed Consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Antonini, S., Pedersini, R., Birtolo, M.F. et al. Denosumab improves trabecular bone score in relationship with decrease in fracture risk of women exposed to aromatase inhibitors. J Endocrinol Invest 47, 433–442 (2024). https://doi.org/10.1007/s40618-023-02174-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02174-5