Abstract
Background
This prospective study quantitatively measured the cerebellar retraction factors, including retraction distance, depth and duration, and evaluated their potential relationship to the development of hearing loss after microvascular decompression (MVD) for hemifacial spasm (HFS).
Methods
One hundred ten patients with primary HFS who underwent MVD in our department were included into this study. The cerebellar retraction factors were quantitatively measured on preoperative MR and timed during MVD. Associations of cerebellar retraction and other factors to postoperative hearing loss were analyzed.
Results
Eleven (10%) patients developed hearing loss after MVD. Compared with the group without hearing loss, the cerebellar retraction distance, depth and duration of the group with hearing loss were significantly greater (p < 0.05). Multivariate regression analysis showed that greater cerebellar retraction depth and longer retraction duration were significantly associated with a higher incidence of postoperative hearing impairment (p < 0.05).
Conclusion
This study strongly suggested a correlation between the cerebellar retraction factors, especially retraction depth and duration, and possibility of hearing loss following MVD for HFS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemifacial spasm (HFS) is generally believed to be caused by vascular compression of the facial nerve root exit zone (REZ). Microvascular decompression (MVD) has been known to be an effective etiological treatment option for HFS with a high success rate (over 85% long-term cure rate) [4, 6, 12, 18]. Although MVD is an effective and safe procedure, neurological complications including facial palsy, hearing loss and vocal cord paralysis still exist for MVD. Among neurological complications, the development of hearing impairment is reported to be the most common in many studies [1, 4, 7, 8, 13, 17]. It was empirically proposed that cerebellar retraction resulting in mechanical stretching may be the main cause of the development of sensorineural hearing loss following MVD.
So far, to our knowledge, no prospective study has revealed the relationship between cerebellar retraction factors and hearing loss after MVD. The aim of this prospective study is to quantitatively measure the degree of cerebellar retraction factors, including retraction distance, depth and duration, and evaluate their potential relationship to the development of hearing loss after MVD.
Methods
Patient demographics
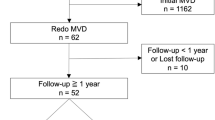
The study included patients with primary HFS who underwent MVD in the neurosurgery department of Rui Jin Hospital from April 2016 to October 2016. All the MVD surgical procedures were performed by one surgeon (W.-G. Zhao). Exclusion criteria included: (1) patients older than 70 years; (2) patients with symptomatic HFS secondary to tumor, epidermoid cysts, Chiari malformation, etc.; (3) patients with preoperative hearing impairment on the surgery side, defined as pure tone audiometry (PTA) > 30 dB and/or Speech Discrimination Score (SDS) < 70% within the speech range of frequencies (AAO-HNS classification system, class B/C/D) [3]. The following subject characteristics were collected from each patient: gender, age, affected side, preoperative MR, pre- and postoperative auditory function, surgical findings, operative outcome and complications. The study design was approved by the Rui Jin Hospital Ethics Committee.
Preoperative MRI
Preoperative MRI and facial nerve MRTA were performed on all patients. MR was obtained at 3.0 T (General Electric Medical System, Milwaukee, WI, USA). The imaging protocol included conventional T1-weighted imaging, T2-weighted imaging, three-dimensional time-of-flight imaging and 3D T2 volume isotropic fast spin echo acquisition imaging.
Evaluation of auditory function
PTA and SDS were performed on all patients 1 day before and 7 days after MVD surgery. PTA was determined for each ear at frequencies from 0.25 kHz to 8 kHz. The average PTA was defined as the mean of the thresholds measured at 0.5, 1, 2 and 4 kHz. Postoperative hearing loss was assessed using the AAO-HNS classification system for non-serviceable hearing loss (class C/D), defined as PTA >50 dB and/or SDS <50% within the speech range of frequencies [3]. We excluded effusion and hemotympanum using otoscopic examination by otologists.
MVD surgery
MVD was performed in the lateral decubitus position through a retromastoid craniectomy. The VIIth and VIIIth cranial nerves were approached inferolaterally. After adequate cerebrospinal fluid drainage, the cerebellum was gently retracted to expose the entire intracranial facial nerve. Persistent cerebellar retraction using a fixed brain retractor was not employed in our MVD procedures. After the offending vessel had been identified, the facial nerve was decompressed by placing an appropriated Teflon pledget at the site of vascular compression. The MVD surgeries were supported by intraoperative electrophysiological monitoring with EMG of the facial nerve and brainstem auditory-evoked potential (BAEP). In this study, persistent decreases in amplitude greater than 50% of wave V and/or delayed latency of peak V more than 1.0 ms were considered alarm criteria. The operator was informed and the surgical manipulation was then paused for a few minutes when alarming BAEP changes appeared.
Measurements
Recently, Lee et al. [8] designed a study to measure the length of cerebellar retraction on MR and retrospectively evaluate its association with the change of intraoperative BAEP. In this study, we designed a modified methodology for MR measurement of cerebellum retraction factors. The neurovascular compression point could be jointly determined by an experienced neurosurgeon and neuroradiologist on a 3D T2 volume isotropic fast spin echo acquisition axial plane. At the level of the neurovascular compression point, a line from the medial aspect of the sigmoid sinus to the neurovascular compression point could be drawn as the assumed surgical route to the neurovascular compression site. As the surgical route could not cross over the sigmoid sinus, this line was regarded as the baseline for measurement. A line parallel to the baseline, going through the highest point of the cerebellar or flocculonodular surface, was regarded as the measure line. In this study, the cerebellar retraction distance was defined as the distance between the medial aspect of the sigmoid sinus and neurovascular compression point. Cerebellar retraction depth was defined as the vertical distance between the measure line and baseline. The measurements were performed on a picture-archiving and communication system (PACS). The measuring procedure was repeated twice, and average values were recorded for analysis. The retraction distance and depth were assumed to correspond to the degree of cerebellar retraction (Figs. 1 and 2).
Illustration of measurement on the level of the neurovascular compression point. Point A: neurovascular compression point. Point B: medial aspect of the sigmoid sinus. Line a (baseline): the line between point A and point B. Line b (measure line): the line parallel to the baseline and going through the highest point of the cerebellar or flocculonodular surface. Cerebellar retraction distance: the distance between point A and B. Cerebellar retraction depth (c): vertical length between the baseline and measure line
The level of the neurovascular compression point on the preoperative MR (3D T2 volume isotropic fast spin echo acquisition axial plane). Point A: neurovascular compression point. Point B: medial aspect of the sigmoid sinus. Line a: baseline. Line b: measure line. Cerebellar retraction distance: the distance between point A and point B. Cerebellar retraction depth (c): the vertical length between line a and line b
Although the fixed brain retractor was not employed in our MVD procedures, cerebellum retraction was still essential for microscopic manipulation despite being discontinuous. Therefore, in the present study, the cerebellar retraction duration was defined as the duration of microscopic manipulation timed from the opening of the dura to finishing of the Teflon felt placement.
Statistical analysis
Categorical and continuous variables were compared by chi-square test and t test, respectively, between the groups with and without postoperative hearing loss. The results were considered significant when P < 0.05. Multivariate logistic regression analysis was designed to determine possible risk factors of postoperative hearing loss. Analyzed variables included gender, age, affected side, preoperative PTA, retraction distance, retraction depth and retraction duration. The dependent variable was postoperative hearing loss. Association was considered statistically significant when P < 0.05. Analyses were performed with commercial software (SPSS, Chicago, IL, USA).
Results
From April 2016 to October 2016, the study enrolled 110 HFS patients. Mean age was 52.5 years (ranging from 36 to 68 years), and the female:male ratio was 2.24 (74/36). HFS affected the right side in 47 patients (42.7%) and left in 63 patients (57.3%). Among these 110 patients, 11, with an incidence of 10%, had non-serviceable hearing loss after MVD according to the AAO-HNS classification system (class C/D).
Table 1 shows the results of the analysis of characteristics grouped by postoperative hearing status. Gender, age, affected side and preoperative hearing PTA were not significantly different between the groups with and without postoperative hearing loss. Compared with the group without hearing loss, the cerebellar retraction distance, depth and duration of the group with postoperative hearing loss were significantly greater (4.54 ± 0.35 cm vs. 4.14 ± 0.29 cm, 0.89 ± 0.28 cm vs. 0.59 ± 0.19 cm and 71.2 ± 14.7 min vs. 55.0 ± 9.7 min, respectively, P < 0.05).
Additionally, multivariate logistic regression analysis showed that a greater cerebellar retraction depth and longer retraction duration were significantly associated with the higher incidence of postoperative hearing loss (P < 0.05). Nevertheless, the cerebellar retraction distance was not associated with the development of hearing loss following MVD in multivariate analysis (Table 2).
Discussion
Sensorineural hearing loss is the most common neurological complication following MVD for HFS. Many studies have shown the development of hearing impairment occurred in 2–20% of patients who underwent MVD for HFS [1, 4, 7, 8, 13, 17]. The 10% incidence in the present study is similar to the results reported by Thirumala (9.5%) [17] and Samii (8.6%) [13]. However, the true incidence of hearing loss after MVD might be even higher if the unreported experience of those medical institutes with less MVD experience were collectively examined.
Mechanisms of damage to the VIIIth cranial nerve during MVD include retraction of the cerebellum resulting in traction on the nerve, manipulation of the blood supply for the VIIIth nerve, direct mechanical/thermal trauma and neurocompression caused by the iatrogenic placement of prosthetic material that compresses the VII/VIII cranial nerve complex. It is empirically suggested that cerebellar retraction may be the most critical component of those factors associated with the development of post-MVD hearing loss. Among all the cranial nerves in CPA, the VIIIth cranial nerve has the longest extracerebral central part and is highly vulnerable to traction. Recently, many studies show that the surgical procedure most frequently associated with BAEP deterioration is traction of the VIIIth cranial nerve during the course of MVD [5, 8, 15, 17]. Cerebellar retraction always has some effect on the VIIIth nerve, usually presenting as flattening of wave V in BEAP, despite controlling the direction of retraction [5, 7,8,9,10,11, 14].
However, few studies have directly researched the relationship between the retraction degree and occurrence of post-MVD hearing loss. Currently, Lee et al. reported such a relationship in their retrospective study [8]. To our knowledge, our present study is the first to prospectively investigate the relationship between retraction factors and post-MVD hearing loss. The results of our study showed that measuring the vertical length of cerebellar retraction on preoperative MR was significantly associated with high occurrence of hearing loss after MVD in both univariate and multivariate analysis. Therefore, although it may not be a unique factor, the cerebellar retraction depth on preoperative MR can be considered an effective assistant tool of choice to evaluate the possibility of postoperative hearing loss, which is valuable in consultation and surgical planning.
Although persistent cerebellar retraction using a fixed brain retractor was not employed in our MVD procedures, cerebellar retraction was still essential for microscopic manipulation in CPA. Our study revealed that there was a significant correlation between cerebellar retraction duration and occurrence of hearing loss. It has been reported that a longer duration of stretching the VIIIth nerve may lead to a greater change in wave V during MVD [2], although the exact etiology is unknown. Nerve stretch studies have supported the notion that increased strain for a long period of time caused irreversible loss of peripheral nerve response [16]. It is possible that a long stretch duration might exceed the outer limit of nerve stretch tolerance, leading to a potential change in the metabolic and structural components of the nerve. By recognizing the risk of hearing complication due to long duration of cerebellar retraction, surgeons should take appropriate precautions to protect the VIIIth cranial nerve during MVD, including pausing the retraction manipulation for a few minutes and application of methylprednisolone.
BAEP characteristics were not discussed in relation to cerebellar retraction in this study because the primary aim was to evaluate the correlation between retraction factors and occurrence of hearing loss. However, to date, the standard for intraoperative BAEP monitoring has been empirically chosen, and the criteria for significant intraoperative BAEP change have still not been universally accepted. Furthermore, intraoperative BAEP waveforms show variability, which may be related to a number of unknown factors. Hence, a robust BAEP monitoring standard needs to be developed and tested in further prospective studies.
This preliminary study has some limitations. Due to the small case number, hearing outcome in patients with preoperative hearing impairment was not investigated. This study lacked long-term follow-up audiograms, although the possibility of return of hearing function is low in sensorineural hearing loss. Also, this study did not investigate the relationship between the cerebellar retraction degree and severity of postoperative hearing loss because of the limited case number. Additionally, since the MR measurement plane was not exactly the same as the dissection plane in the MVD procedure, a difference might exist between the cerebellum retraction measured on MR and that actually applied during the surgery in this study. To overcome these limitations, further well-designed studies with long-term follow-up, a large number of cases and more extensive data on surgery-related elements are needed.
Conclusion
Our results strongly suggested the correlation between the cerebellar retraction factors and possibility of hearing loss after MVD for HFS, especially retraction depth and duration. Therefore, surgeons should design the most appropriate surgical planning and precautions before and during MVD surgery, and cerebellar retraction should be done minimally to minimize the risk of postoperative hearing loss.
References
Acevedo JC, Sindou M, Fischer C. (1997) Microvascular decompression for the treatment of hemifacial spasm. Retrospective study of a consecutive series of 75 operated patients—eletrophysiologic and anatomical surgical analysis. Stereotact Funct Neurosurg 68:260–265
Amagasaki K, Watanabe S, Naemura K, Nakaguchi H (2015) Microvascular decompression for hemifacial spasm: how can we protect auditory function? Br J Neurosurg 29:347–352
American Association of Otolaryngology Head and Neck Surgery Committee on hearing and equilibrium guideline for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma) (1995) Otolaryngol Head Neck Surg 113:179–180
Baker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD (1995) Microvascular decompression for hemifacial spasm. J Neurosurg 82:201–210
Bond AE, Zada G, Gonzalez AA, Hansen C, Giannotta SL (2010) Operative strategy for minimizing hearing loss and other major complications associated with microvascular decompression for trigeminal neuralgia. World Neurosurg 74:172–177
Hector SB, Olivia VH, Emiliano AS, Sergio MJ, Rogelio RG (2015) Hemifacial spasm: 20-year surgical experience, lesson learned. Surg Neurol Int 6:83–87
Lee CC, Liao CH, Lin CF, Yang TF, Hus S, Yen YS, Shih YH (2014) Brain auditory evoked potential monitoring and neuro-endoscopy: two tools to ensure hearing preservation and surgical success during microvascular decompression. J Chin Med Assoc 77:308–316
Lee MH, Lee HS, Jee TK, Jo KI, Kong DS, Lee JA, Park K (2015) Cerebellar retraction and hearing loss after microvascular decompression for hemifacial spasm. Acta Neurochir 157:337–343
Legatt AD (2002) Mechanisms of intraoperative brainstem auditory evoked potential changes. J Clin Neurophysiol 19:396–408
Park K, Hong SH, Hong SD, Cho YS, Chung WH, Ryu NG (2009) Patterns of hearing loss after microvascular decompression for hemifacial spasm. J Neurol Neurosurg Psychiatry 80:1165–1167
Ramnarayan R, Mackenzie I (2006) Brainstem auditory evoked responses during microvascular decompression for trigeminal neuralgia: predicting postoperative hearing loss. Neurol India 54:250–254
Rosenstengel C, Matthes M, Baldauf J, Fleck S, Schroeder H (2012) Hemifacial spasm: conservative and surgical treatment options. Dtsch Arztebl Int 109:667–673
Samii M, Gunther T, laconetta G. (2002) Microvascular decompression to treat hemifacial spasm: long-term results for a consecutive series of 143 patients. Neurosurgery 50:712–718
Sato S, Yamada M, Koizumi H, Onozawa Y, Shimokawa N, Kawashima E, Fujii K (2009) Neurophysiological mechanisms of conduction loss of auditory nerve during cerebellopontine angle surgery. Clin Neurophysiol 120:329–335
Thirumala P, Krishnaiah B, Habeych M, Balzar J, Crammond D (2015) Hearing outcomes after loss of brainstem auditory evoked potentials during microvascular decompression. J Clin Neurosci 22:659–663
Wall EJMJ, Kwan MK, Rydevik BL, Myers RR, Garfin SR (1992) Experimental stretch neuropathy. Changes in nerve conduction under tension. J Bone Joint Surg Br 74:126–129
Ying TT, Thirumala P, Chang YF, Habeych M, Crammond D, Balzar J (2014) Empirical factors associated with brain auditory evoked potential monitoring during microvascular decompression for hemifacial spasm and its correlation to hearing loss. Acta Neurochir 156:571–575
Yuan Y, Wang Y, Zhang SX, Zhang L, Li R, Guo J (2005) Microvascular decompression in patients with hemifacial spasm: report of 1200 cases. Chin Med J 118:833–836
Acknowledgements
We would like to thank Lee et al., whose previous study shared some experience on the MR measurement methodology of cerebellum retraction. Also, we thank Jun Zhu for help with the statistical analysis in this study.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Rui Jin Hospital Ethics Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
The authors present a prospective study in which they quantitatively measured cerebellar retraction factors, including retraction distance, depth and duration, and evaluated their potential relationship to the development of hearing loss after microvascular decompression for hemifacial spasm. Of 110 patients, 11 lost hearing. Compared with the group without hearing loss, the cerebellar retraction distance, depth and duration of the group with hearing loss were significantly greater. Multivariate regression analysis showed that greater cerebellar retraction depth and longer retraction duration were significantly associated with the higher incidence of postoperative hearing impairment. The authors concluded that there is a correlation between cerebellar retraction depth and duration and hearing loss following MVD for HFS.
This is a nice attempt trying to prospectively evaluate the influence of cerebellar retraction on hearing. Although all neurosurgeons who perform MVD for HSF know that cerebellar retraction may quickly lead to changes in the BEAP indicating an increased risk of hearing loss, no prospective study on that topic has been published. One shortcoming is that the authors equate cerebellar retraction duration as the duration of microscopic manipulation defined from the opening of the dura to finishing the Teflon placement. However, there are manipulations during the surgery without cerebellar retraction. Direct manipulation of the hearing nerve and its vascular supply may also lead to hearing impairment. Another drawback of the study is that the measurement of the retraction depth is not in the plane of the dissection. The surgical approach is more in the caudal-to-cranial direction; therefore, the measured cerebellum retraction distance is not the retraction that is actually applied during the surgery. The retraction required to expose the root exit zone of the facial nerve is less.That being said, the authors are to be congratulated for their attempt to quantify the retraction parameters that affect hearing outcome after MVD for hemifacial spasm.
Henry Schroeder,
Greifswald, Germany
Rights and permissions
About this article
Cite this article
Li, N., Zhao, WG., Pu, CH. et al. Quantitative study of the correlation between cerebellar retraction factors and hearing loss following microvascular decompression for hemifacial spasm. Acta Neurochir 160, 145–150 (2018). https://doi.org/10.1007/s00701-017-3368-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3368-9