Abstract
Background
This retrospective study evaluated the length of cerebellar retraction and the changes of intraoperative brainstem auditory evoked potential (BAEP) during microvascular decompression (MVD), and assessed the predictive value of the hearing loss as a prognostic indicator for the treatment outcome of hemifacial spasm (HFS).
Methods
This series included 1,518 consecutive patients affected with HFS who underwent MVD, during which BAEP was monitored. Patients were divided into two groups based on whether hearing loss occurred following decompression or not. Each patient underwent a similar procedure performed by one neurosurgeon. The two patients groups were matched with regard to sex, age, and degree of spasm.
Results
Among the 1,518 patients, 106 (6.98 %) displayed functional hearing changes. Hearing loss was permanent in 12 patients (0.79 %). Of the 1,412 patients with stationary hearing compared with preoperative audiometry, 96 patients were selected who were individually matched with respect to sex, age, and degree of spasm. BAEP changed immediately after cerebellar retraction in 7 of 12 hearing-loss patients, suggesting the importance of retraction on hearing outcomes. The distance from the cerebellar surface of the petrous temporal bone to the neurovascular compression point was measured. The median distance of cerebellar retraction in the hearing-loss group was 13.77 mm, which was longer than the median distance in the control group.
Conclusions
Preoperative measurement of the cerebellar retraction distance can be a valuable clue to predict and prevent postoperative hearing loss in MVD for HFS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of microvascular decompression (MVD) to treat hemifacial spasm (HFS) was first proposed by Gardner in 1962 [4]. MVD has since become widely used to treat HFS. Although MVD is a safe and effective method, complications include facial palsy, hearing impairment, vocal cord paralysis, intracranial hemorrhage, wound infection, meningitis, vertebral artery injury and cerebrospinal fluid leakage [13, 20]. Among them, the development of hearing difficulty is common and is related to the disturbance adjacent to the auditory nerve in 1.9-20 % of cases [13, 20].
Exchange of information with others can seriously be impaired in individuals with hearing loss. These difficulties with communication can diminish quality of life. Of several monitoring methods, intraoperative brainstem auditory evoked potential (BAEP) is useful and reliable for the preservation of hearing function in patients undergoing cerebellopontine angle surgery, including MVD for HFS [19]. Monitoring auditory function via BAEP has been used in MVD for HFS to avoid postoperative hearing loss [1, 24] and the usefulness of BAEP monitoring has been reported [7, 8, 15–17]. Although the accurate incidence rate of BAEP change is unknown, the change is supposedly a good predictor of postoperative hearing impairment. However, to the best of our knowledge, there are no reports of any reliable preoperative evaluation tool that could predict the risk of postoperative hearing loss.
The aim of present study is to predict the possibility of hearing impairment by preoperative magnetic resonance imaging (MRI) and develop better procedures for the prevention of hearing impairment. We analyzed and identified the possible risk factors of postoperative hearing loss by comparing the characteristics of preoperative imaging between a permanent hearing-loss group and hearing-preserved group.
Material and methods
Patient demographics
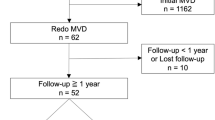
Between January 2001 and January 2011, 1,518 consecutive patients underwent MVD for HFS at Samsung Medical Center. All of the surgical procedures were performed by one surgeon (K.P.). Patients with symptomatic HFS secondary to tumors, aneurysms, or epidermoid cyst were excluded. Among the 1,518 patients, 106 (6.98 %) had immediate postoperative audiometric abnormalities, including mild and transient changes. We divided the patients who had MVD for HFS into two groups according to postoperative assessment of hearing: permanent hearing loss and no hearing abnormality. The 1,412 patients who had stationary hearing compared with preoperative audiometry were matched with the hearing-loss group for sex, age, and degree of spasm. Ninety-six patients had records available for image analysis and intraoperative monitoring. The data of each group and intraoperative findings from MVD procedures are summarized in Table 1.
The study protocol was reviewed and approved by the institutional review board of Samsung Medical Center (SMC 2014-09-008) and adhered to the recommendations for biomedical research involving human subjects of the Declaration of Helsinki (1975). The requirement of informed consent was waived, as the study was based on existing clinical data.
Preoperative MRI
All patients underwent preoperative evaluation by computed tomography (CT) and MRI with the addition of a contrast agent. MRI was obtained at 3.0 T (Achieva; Philips Medical Systems, Best, The Netherlands) with an eight-channel sensitivity-encoding (SENSE) head coil. Imaging protocol included three-dimensional time-of-flight (3-D TOF; TR/TE/flip angle, 25 ms/3.5 ms/20°; section thickness 1.6 mm, slice spacing 0.8 mm, 500 × 348 matrix, acquisition time = 5 min 29 s), and 3-D T2 VISTA (volumetric isotropic T2-weighted acquisition; TR/TE/flip angle, 2,000 ms/228 ms/20°; NSA = 2, ETL = 70, 248 × 250 matrix, voxel size = 0.8 × 0.8 × 0.8 mm3, acquisition time = 4 min 10 s). Neurovascular compression was determined by experienced neuroradiologists.
Evaluation of auditory function
Preoperative and postoperative (usually within 3–10 days after surgery) pure tone audiometry (PTA) and speech discrimination score (SDS) were performed on all patients. The average PTA thresholds for 500, 1,000, 2,000 and 3,000 Hz were calculated. We excluded conductive hearing loss, using an otoscopic examination and PTA with bone conduction, as well as air conduction. A decrease of more than 15 dB of the postoperative average PTA threshold, as judged according to bone conduction, or a decrease of more than 20 % of SDS from baseline for each patient was considered significant. Patients with significant hearing loss underwent audiometric follow-up, usually within 1–4 weeks after their first audiometric evaluation. Permanent hearing loss was defined a significant audiometric change at the 1-year follow-up, which included profound or total deafness (hearing loss ≥90 dB). We retrospectively reviewed the clinical records of all patients, which included preoperative symptoms, intraoperative findings, postoperative outcomes, and complications.
Operation technique and intraoperative monitoring
All of the procedures were performed using the lateral retrosigmoid suboccipital approach, with the intraoperative facial electromyography (EMG) and BAEP being monitored [6, 12, 13, 17]. The patient was placed in a lateral park bench position with the head rotated approximately 10° away from the affected site and the vertex was dropped 15° toward the floor, as described previously [13]. The stimulating needle electrodes were inserted intradermally over the zygomatic branches of the facial nerve and a pulse wave of 0.1–0.2 ms with an intensity of 5–25 mA was used. Lateral spread response (LSR) was recorded during evoked facial EMG monitoring that appeared in the other facial muscles including the orbicularis oculi, orbicularis oris, and mentalis muscles upon stimulation of the main nerve innervating the frontalis muscle.
Following craniectomy, dural incision, and drainage of the cerebrospinal fluid, a tapered retractor blade was placed over a previously placed rubber dam and cottonoid. After careful dissection of the arachnoid membrane and gentle retraction of the flocculus, the REZ of the facial nerve was observed. The compressing vessel, or offender, was identified near the REZ. The fixed retraction (Greenberg retractor system) was used, but it was not used during the entire process. To insert a key piece of Teflon felt, and to manipulate surrounding perforators, fixed retraction was necessary. But the rest of the process, retraction blade was removed and, suction tool was applied. Neurovascular compression was identified during the MVD procedure in every case. Almost all of the lesions had other contributing factors (thick arachnoid trabeculae, perforating arteries, or adjacent collateral arteries) that inevitably caused neurovascular compression.
In all cases, several pieces of Teflon felt were placed between the compressing vessel and the REZ. Following decompression, LSR disappeared in most patients. When the LSR persisted despite decompression, we looked for any suspicious underlying causes, such as possible compression by another vessel. The dura was closed with several muscle pieces interposed between the interrupted sutures to prevent leakage of cerebrospinal fluid [18]. Cranioplasty was performed using polymethylmethacrylate bone cement.
Measurement of cerebellar retraction distance
The neurovascular compression point could usually be found on a 3-D T2 VISTA axial plane. At the level of neurovascular compression point, a parallel line with cerebellar surface of petrous temporal bone could be drawn as the assumed surgical route. This line encountered the medial aspect of sigmoid sinus. As the lateral portion of the surgical route could not cross over the sigmoid sinus, this parallel line was regarded as the base line for measurement. (Fig. 1) The vertical distance between the neurovascular compression and cerebellar surface of the petrous temporal bone was measured. The vertical distance was assumed to correspond to the degree of cerebellar retraction.
At the level of neurovascular compression point, a line parallel with the cerebellar surface of petrous temporal bone could be drawn as the assumed surgical route. This line encountered the medial aspect of sigmoid sinus. The vertical distance between the neurovascular compression and cerebellar surface of the petrous temporal bone was measured. The vertical distance was assumed to correspond to the degree of cerebellar retraction
Statistical analyses
Data were collected on the preoperative period and the severity of HFS, direct and late postoperative outcomes, complications, and intraoperative anatomic and monitoring findings. The operative reports were scrutinized carefully for the impact of the intraoperative monitoring data on the surgical procedure. Categorical variables (sex, side of spasm, degree of spasm, offender vessel, and type of compression) were compared using cross tabs with chi-square test or Fisher’s exact test. Continuous variables (age, and length of retraction) were compared using Mann–Whitney test. A Statistical examination was done by using commercial software (PASW Statistics, version 18; SPSS, Chicago, IL, USA). The results were considered significant for probability values less than 0.05.
Results
The patient population consisted of 440 men and 1,078 women, who ranged in age from 19 to 77 years (mean age, 46.5 years). Among these 1,518 patients, 106 (6.98 %) displayed immediate postoperative audiometric abnormalities including mild and transient changes. Ninety-two patients (6.06 %) had transient hearing impairment that improved to recovery at the last follow-up examination within the 1st year. However, 12 patients (0.79 %) had permanent hearing loss; they comprised 9 woman and 3 men. Deaf patients and the control groups were comparable in sex, age, side of spasm, and degree of spasm. Table 1 shows the results of analysis of characteristics grouped by hearing status. Sex, age, side of spasm, offending vessel, and type of compression were not significantly different between the groups. Compared with the controls, the cerebellar retraction distance from petrous temporal bone of patients with permanent hearing loss was significantly longer. The median length was 13.77 mm in the hearing loss group and 8.0 mm in the control group, indicating that permanent hearing loss frequently occurred in wider retraction length with statistical significance (p < 0.001) (Table 1).
In the hearing-loss group, out of the 12 patients, 9 had an obvious BAEP change. They included delay in latency and decrease in amplitude of peak V. Three patients had no BAEP change, which may have been false-negative results. Among the nine patients with BAEP change, the event occurred during cerebellar retraction in seven patients, after releasing the retraction in one patient, and before retraction in one patient. When the BAEP change occurred at cerebellar retraction, retraction was released immediately. Three of nine patients recovered BAEP up to the initial amplitude. In the cases of BAEP change during craniectomy—before the retraction, the decrease was to 50 % of the initial amplitude at the time of craniectomy, with decrease up to 90 % of initial amplitude at the time of retraction, and continued the decreased amplitude until the end of operation (Table 2).
Illustrative case
A 49-year-old woman was admitted for MVD in HFS on the left side. A preoperative audiogram showed bilateral normal hearing. MRI of the internal auditory canal revealed the left vertebral artery and posterior inferior cerebellar artery were in close proximity to the REZ of the ipsilateral facial nerve and normal brain stem anatomy at the pontomesencephalic junction (Fig. 2). During MVD, the left side BAEP was decreased by 50 % of the initial amplitude at the time of the cerebellar retraction. The decrease did not recover to the initial amplitude (Fig. 3). A postoperative audiogram revealed left ear deafness (Fig. 4). Preoperative internal auditory canal MRI verified that the vertical distance of cerebellar retraction was 19.45 mm. There was no cerebellar atrophy, which might have confounded the long distance of retraction.
A 49-year-old woman, admitted for MVD in HFS on the left side. A preoperative MRI showed the left vertebral artery and posterior inferior cerebellar artery in close proximity to the root exit zone of the ipsilateral facial nerve, and the vertical distance of cerebellar retraction was 19.45 mm. View of measured vertical length from the petrous temporal bone to neurovascular compression point
a Initial BAEP wave. b Wave at the time of the cerebellar retraction; the wave was decrease by 50 % of the initial amplitude. c Final BAEP wave; the wave was not recovered. Same patient as in Fig. 1
a Pre-operative audiometry shows, normal auditory function with PTA 13 dB, SDS 2 100 %. b Post-operative audiometry could not tested with PTA more than 120 dB. Same patient as in Fig. 1
Discussion
Profound sensorineural hearing loss is a recognized complication of MVD for HFS with a reported incidence of 1.9-20 % [1, 2, 3, 20, 22]. These reports may underestimate the true incidence of hearing loss because preoperative and postoperative audiograms are not always available for comparison. The incidence may be even higher if the unreported experience of community hospitals is collectively examined.
Hearing impairment during surgical procedures involving the neural tissues, may arise from (1) stretching of nerve VIII when retracting the cerebellum, (2) injury due to manipulation of the labyrinthine artery and/or the anteroinferior cerebellar artery, (3) direct trauma to the nerve caused by instruments or nearby coagulation, loss of anatomical integrity (transection), and (4) neo-compression of the nerve by the prosthesis interposed between the offending vessel and the VII–VIII nerve complex [25]. Recently, we reported a new possible mechanism of hearing loss due to (5) increased intracranial pressure from over-infusion of saline with dural closure [11].
In terms of stretching injuries, the surgical route to the facial nerve must proceed through the cerebellar surface of petrous temporal bone during the MVD procedure. The REZ of the facial nerve is located immediately medial to cranial nerve VIII in the supraolivary fossette and the flocculus exists just lateral to the nerves. Therefore, with a direct approach in a dorsoventral direction, it is difficult to obtain complete observation of the facial nerve exit zone over cranial nerve VIII and the flocculus. In this respect, cerebellar retraction is necessary during the MVD for HFS. The surgical procedure most frequently associated with BAEP deterioration is traction and/or compression of the nerve during the course of the maneuvers to release the nerve structures from the vascular loop. The manipulation of the nerve is likely to lead to the stretching or spasm of the vasa nervorum and consequent ischemic phenomena. The simultaneous desynchronization of wave I indicates a decrease in the vascularization of the proximal tract of the cochlear nerve, which would considerably increase the risk of hearing loss [9]. These events are usually reversible, demonstrated by the fact that there are intraoperative alterations in BAEP. But, it may be associated with hearing deficits in some cases.
In addition, the cochlea receives its blood supply from the internal auditory artery. And damage to the artery leads to cochlear ischemia, or infarction which may affect wave I [21]. Another maneuver associated with hearing impairment is the coagulation of vessels running parallel to the cochlear nerve, which probably feed the cochlea or the intra-meatal tract of nerve VIII. In rare cases, sudden worsening in BAEP can occur during or immediately after craniectomy, probably due to an edema in the intracanalicular tract of the nerve. In this series, one patient had BAEP worsening during craniectomy. It is likely that the vibrations transmitted to the rocca petrosa, during craniectomy, are apt to cause edema and consequent ischemia of the intracanalicular tract of the cochlear nerve, leading to a reversible blockade of its transmission capacities. In addition, physiologic factors—body temperature or the anesthetics use—may affect the latency of the different components of the BAEP, but these factors are not likely to effect the amplitude consistently [23]. Hypoperfusion should be considered as causative factor, when decreasing of the amplitude without prolongation of the latency [5]. This means that the amplitude of BAEP might be more significant and more valuable than the latencies as an indicator of injury to the auditory nerve. The amplitude shows a variability, which may be related to recording conditions, electrode impedance and a number of unknown factors [10, 14]. And it should be learned and controlled from long experience.
Preoperatively predictive indicator was rarely discussed. The aim of the present study was to predict the possibility of hearing impairment by preoperative MRI and perform more careful procedures. As BAEP changes usually occur during retraction, we suggested that retraction is the most critical component of the many factors associated with hearing impairment. And vertical length measuring of cerebellar retraction proved to be useful for predicting the outcomes. Even in elderly patients, the cerebellar atrophy may reduce the pressure to the cerebellar hemisphere during the retraction, the tension pressure to cranial nerve VIII may not affect. The cranial nerve VIII has the longest extracerebral central part of all the nerves in the cerebellopontine angle and is highly vulnerable to traction. To determine whether measurement of retraction length could be helpful in preserving the auditory function, we retrospectively analyzed the evoked potential data and auditory outcome, and compared these between the two groups of patients who had permanent hearing loss and those who did not. The distance may not be a unique or strong factor, but it might be an effective assistant tool to accomplish safety decompression. By recognizing the possibility of auditory nerve injury by preoperative indicator, we will be able to design more careful procedures for the preservation of auditory nerve.
Conclusion
We retrospectively investigated attempting to correlate the distance of cerebellar retraction and BAEP change with the occurrence of hearing loss after MVD for HFS. BAEP monitoring is a valuable intraoperative indicator for preservation of auditory function, as in previous reported studies [9]. Therefore, we should design the most appropriate approach by knowing individual pathologic anatomy before surgery and the retraction should be done minimally, and in a direction perpendicular, rather than longitudinal, to the axis of the eighth nerve, to minimize the risk of postoperative hearing impairment. Furthermore, according to our experience, individual pathologic anatomy before surgery assessed by MRI is crucial to adapt and design the most appropriate approach for every patient.
References
Acevedo JC, Sindou M, Fischer C, Vial C (1997) Microvascular decompression for the treatment of hemifacial spasm. Retrospective study of a consecutive series of 75 operated patients–electrophysiologic and anatomical surgical analysis. Stereotact Funct Neurosurg 68:260–265
Barker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD (1995) Microvascular decompression for hemifacial spasm. J Neurosurg 82:201–210
Ciriano D, Sindou M, Fischer C (1991) Peroperative monitoring of early auditory evoked potentials in microsurgical vascular decompression for trigeminal neuralgia or hemifacial spasm. Neurochirurgie 37:323–329
Gardner WJ (1962) Concerning the mechanism of trigeminal neuralgia and hemifacial spasm. J Neurosurg 19:947–958
Grundy BL, Jannetta PJ, Procopio PT, Lina A, Boston JR, Doyle E (1982) Intraoperative monitoring of brain-stem auditory evoked potentials. J Neurosurg 57:674–681
Hitotsumatsu T, Matsushima T, Inoue T (2003) Microvascular decompression for treatment of trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia: three surgical approach variations: technical note. Neurosurgery 53:1436–1441, discussion 1442–1443
Ishikawa M, Ohira T, Namiki J, Kobayashi M, Takase M, Kawase T, Toya S (1997) Electrophysiological investigation of hemifacial spasm after microvascular decompression: F waves of the facial muscles, blink reflexes, and abnormal muscle responses. J Neurosurg 86:654–661
Isu T, Kamada K, Mabuchi S, Kitaoka A, Ito T, Koiwa M, Abe H (1996) Intra-operative monitoring by facial electromyographic responses during microvascular decompressive surgery for hemifacial spasm. Acta Neurochir (Wien) 138:19–23, discussion 23
Jo KW, Kim JW, Kong DS, Hong SH, Park K (2011) The patterns and risk factors of hearing loss following microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 153:1023–1030
Jo KW, Kong DS, Park K (2013) Microvascular decompression for hemifacial spasm: long-term outcome and prognostic factors, with emphasis on delayed cure. Neurosurg Rev 36:297–301, discussion 301–302
Jo KW, Lee JA, Park K, Cho YS (2013) A new possible mechanism of hearing loss after microvascular decompression for hemifacial spasm. Otol Neurotol 34:1247–1252
Kong DS, Park K, Shin BG, Lee JA, Eum DO (2007) Prognostic value of the lateral spread response for intraoperative electromyography monitoring of the facial musculature during microvascular decompression for hemifacial spasm. J Neurosurg 106:384–387
McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK (1999) Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg 90:1–8
Moller AR (1995) Intraoperative neurophysiologic monitoring. Am J Otol 16:115–117
Moller AR, Jannetta PJ (1985) Microvascular decompression in hemifacial spasm: intraoperative electrophysiological observations. Neurosurgery 16:612–618
Moller AR, Jannetta PJ (1986) Physiological abnormalities in hemifacial spasm studied during microvascular decompression operations. Exp Neurol 93:584–600
Moller AR, Jannetta PJ (1987) Monitoring facial EMG responses during microvascular decompression operations for hemifacial spasm. J Neurosurg 66:681–685
Park JS, Kong DS, Lee JA, Park K (2007) Intraoperative management to prevent cerebrospinal fluid leakage after microvascular decompression: dural closure with a “plugging muscle” method. Neurosurg Rev 30:139–142, discussion 142
Polo G, Fischer C, Sindou MP, Marneffe V (2004) Brainstem auditory evoked potential monitoring during microvascular decompression for hemifacial spasm: intraoperative brainstem auditory evoked potential changes and warning values to prevent hearing los—prospective study in a consecutive series of 84 patient. Neurosurgery 54:97–104, discussion 104–106
Samii M, Gunther T, Iaconetta G, Muehling M, Vorkapic P, Samii A (2002) Microvascular decompression to treat hemifacial spasm: long-term results for a consecutive series of 143 patients. Neurosurgery 50:712–718, discussion 718–719
Sato S, Yamada M, Koizumi H, Onozawa Y, Shimokawa N, Kawashima E, Fujii K (2009) Neurophysiological mechanisms of conduction impairment of the auditory nerve during cerebellopontine angle surgery. Clin Neurophysiol 120:329–335
Sindou M, Fobe JL, Ciriano D, Fischer C (1990) Intraoperative brainstem auditory evoked potential in the microvascular decompression of the 5th and 7th cranial nerves. Rev Laryngol Otol Rhinol (Bord) 111:427–431
Stockard JJ, Sharbrough FW, Tinker JA (1978) Effects of hypothermia on the human brainstem auditory response. Ann Neurol 3:368–370
Van HT, Deguine O, Esteve-Fraysse MJ, Bonafe A, Fraysse B (1999) Relationship between cochleovestibular disorders in hemifacial spasm and neurovascular compression. Laryngoscope 109:741–747
Watanabe E, Schramm J, Strauss C, Fahlbusch R (1989) Neurophysiologic monitoring in posterior fossa surgery. II. BAEP-waves I and V and preservation of hearing. Acta Neurochir (Wien) 98:118–128
Conflict of interest statement
None of the authors has any conflict of interest in any kind concerning this scientific paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Min Ho Lee and Hyun Seok Lee contributed equally to this article
Rights and permissions
About this article
Cite this article
Lee, M.H., Lee, H.S., Jee, T.K. et al. Cerebellar retraction and hearing loss after microvascular decompression for hemifacial spasm. Acta Neurochir 157, 337–343 (2015). https://doi.org/10.1007/s00701-014-2301-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2301-8