Abstract
Background
Although microvascular decompression (MVD) surgery has been widely accepted as an effective treatment for hemifacial spasm (HFS), delayed facial palsy (DFP) is not an unusual complication, but it has only been sporadically described in the literature. The purpose of this study was to examine the probability of occurrence, the risk/predisposing factors, and the prognosis and timing of DFP.
Methods
A prospective cohort study was conducted that included patients diagnosed with HFS and treated by MVD at our institution. All patients were followed up at the outpatient department or by telephone from December 2009 to December 2014. Categorical variables were analyzed using the Pearson’s Chi-square test or Fisher’s exact test. Continuous variables were compared using the independent Student’s t test. The Spearman rank test was used to determine the correlation between the time of onset and the duration of DFP. The risk/predisposing factors were analyzed by the logistic regression method.
Results
We enrolled 248 patients who were treated by MVD for HFS. During the follow-up period, 16 patients (6.5 %) developed DFP. Fifteen of those patients had a complete recovery, and in one patient the facial palsy did not resolve. The average onset time was 10.2 days (range, 2–30 days) after surgery, and the mean duration of DFP after MVD, with exclusion of the permanent facial palsy patient, was 59.7 days (range, 7–220 days). The time of onset was correlated with the duration of DFP after MVD (p = 0.036). Furthermore, hypertension contributed to DFP (odds ratio [OR] 4.226, 95 % confidence interval [CI] 1.089–16.401, p = 0.037).
Conclusions
Although the degree of facial palsy was variable, most patients experienced a complete recovery without requiring any special treatment. DFP may be a self-healing disease that resolves spontaneously without any treatment. The time of onset was correlated with the duration of DFP; i.e., an earlier development of DFP corresponded with a shorter duration, whereas a later development of DFP corresponded with a longer duration. Our results also suggest that hypertension contributes to DFP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microvascular decompression (MVD) is currently a highly accepted and effective method for the treatment of hemifacial spasm (HFS), a disease generally believed to be caused by vascular compression of the facial nerve root exit zone. MVD has been reported to have an 85–90 % cure rate for HFS, an 84 % success rate at 10 years after surgery, and an operative morbidity of less than 10 % [8].
However, the results of MVD surgery are not always satisfactory due to complications. The reported complications after MVD include facial palsy, hearing impairment, hoarseness, intracranial hemorrhage, wound infection, meningitis, vertebral artery injury, and CSF leakage [2, 8, 11, 20, 21]. Among those complications, delayed facial palsy (DFP) is the most commonly reported. DFP displays a relatively sudden onset and usually occurs over a 24-h period after the operation. Furthermore, DFP usually has a negative effect on the patient’s psychological status, generating great stress on the patient and causing them to question the efficacy of the operation and be concerned about the prognosis of their DFP. If doctors are not familiar with the characteristics of DFP after MVD, they cannot help alleviate the psychological burden on the patient, which may result in overtreatment. Therefore, the purpose of this study was to examine the probability of occurrence, the risk/predisposing factors, and the prognosis and timing of DFP.
Patients and methods
Cohort definition
This prospective cohort study included consecutive patients treated with MVD for HFS by the senior author of this manuscript (Heng Zhang) at the Neurosurgery Department of West China Hospital between December 2009 and December 2014. These patients presented with an insidious onset of fine twitching of the orbicularis oculi muscle and gradually downward-spreading spasms in their ipsilateral facial expression muscles. All patients underwent preoperative magnetic resonance (MR) examination. The possibility of neurovascular conflict was investigated preoperatively using MR cranial nerve hydrographic imaging [22]. Patients with symptomatic HFS secondary to tumors were excluded from this study. All the patients mentioned in this article gave their consent for inclusion in this submission.
Follow-up and data collection
All patients were followed up at the outpatient department or by telephone for at least 6 months following surgery (mean, 24 months, range, 6–67 months). We investigated the following clinical characteristics: age, sex, spasm side, facial nerve block before MVD (botulinum toxin treatment), duration of symptoms, hypertension, diabetes, HBV infection, HSV infection, smoking status and alcohol use, offending vessels, Chiari’s malformation, electrophysiological monitoring results, postoperative HFS recurrence, and complications. Furthermore, we recorded the onset time and the duration of DFP after MVD.
Surgical techniques
Under general anesthesia, the patient was placed in a lateral park bench position with frame fixation of the head. All procedures were performed via a lateral retrosigmoid suboccipital approach. A tapered retractor blade was placed over the rubber dam, and cottonoid previously placed after a craniectomy and dural incision and drainage of the cerebrospinal fluid. After careful dissection of the arachnoid membrane and gentle retraction of the flocculus, the root exit zone of the facial nerve was observed. When the diagnosis of neurovascular conflict was confirmed, several Teflon threads were inserted between the offending vessels and the facial nerve. During manipulation of the VII and VII nerves, to help achieve complete decompression, brainstem auditory evoked potentials were closely monitored to assess hearing loss, and facial electromyography was used to closely monitor the lateral spread response phenomenon [9, 22].
Statistical analyses
Categorical variables were analyzed using the Pearson’s Chi-square test or Fisher’s exact test and are expressed as frequencies and percentages. Continuous variables were compared using the independent Student’s t test and are expressed as the means ± SD.
The Spearman rank test was used to determine the correlation between the onset time and the duration of DFP after MVD.
A multivariate logistic regression analysis was designed to determine the risk/predisposing factors of DFP after MVD. The analyzed variables included spasm side (left or right), duration of symptoms (years), offending vessels (AICA, PICA, VA, or other vessels), postoperative recurrence of HFS (yes or no), hypertension (yes or no), HBV infection (yes or no), Chiari’s malformation (yes or no), complications (yes or no), smoker (yes or no), and alcohol use (yes or no). The dependent variable was the status of the patient during follow-up (1 = DFP, 0 = no DFP).
SPSS statistics 22.0 software for Mac (IBM Corporation) was used for all analyses. The associations were considered to be statistically significant when p values were <0.05.
Results
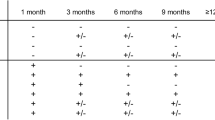
From December 2009 to December 2014, 266 consecutive patients were admitted to the Department of Neurosurgery of West China Hospital for the treatment of HFS. Among them, one patient was diagnosed with HFS secondary to a tumor, and 17 patients were lost to follow-up. Thus, 248 HFS patients were included in the study cohort. We divided the cohort into two groups: the first group (group I) contained patients without DFP, and the second group (group II) contained patients with DFP. The basic characteristics of the cohort are documented in Table 1. Information regarding complications is displayed in Table 2. Facial palsy was graded using House–Brackmann grading. DFP grading information is shown in Table 3. During the follow-up period, 16 patients with a mean age of 51.8 years (range, 37–67 years) suffered from DFP after MVD. The time of onset and the duration of DFP after MVD for those 16 patients are shown in Fig. 1. The average onset time of DFP after MVD in our study was 10.2 days (range, 2–30 days), and the mean duration of DFP, calculated after excluding the permanent facial palsy patient, was 59.7 days (range, 7–220 days). The probability of developing DFP was analyzed using Kaplan–Meier curves (Fig. 2).
The Spearman rank test showed a correlation between the onset time and duration of DFP after MVD (p = 0.039).
The multivariate logistic regression analysis identified one factor that may be related to DFP: hypertension (odds ratio [OR] 4.226, 95 % confidence interval [CI] 1.089–16.401, p = 0.037). The other examined factors (spasm side, duration of symptoms, offending vessels, HBV infection, Chiari’s malformation, postoperative reoccurrence of HFS, complications, smoking, and alcohol use) were not significantly associated with DFP (Table 4).
Discussion
Lovely et al. and Kim et al. reported a DFP incidence of 2.8–8.3 % in patients undergoing MVD for HFS [10, 12, 14, 15, 17, 18], which is similar to the incidence of DFP of 6.5 % observed in our study. The reported average onset time of DFP following MVD is 8.0–12.1 days [10, 12, 14, 15, 17] and the mean duration of DFP following MVD is 39.9–189 days [10, 12, 14, 15, 17]. In our study, the average onset time and duration of DFP were 10.2 and 70.5 days, respectively. Data collected from previously published studies are summarized in Table 5.
Several authors have reported that DFP completely resolves in most patients, even with variable degrees of facial palsy [10, 12, 14, 15, 17, 18]. In our study, 15 patients with DFP experienced complete recovery; however, in one patient, DFP progressed to permanent facial palsy, although the House–Brackmann grade of the facial palsy in that case changed from grade III to grade II during the follow-up period. Two additional patients suffered from permanent facial palsy after MVD, although the onset times were 90 and 180 days after MVD; therefore, we did not define them as having DFP because the times to onset of facial palsy were much longer than the average time described in other studies.
According to the Spearman test (p = 0.036), we found a correlation between the onset time and duration of DFP after MVD. Earlier development of DFP corresponded to a shorter duration, and a later development of DFP corresponded to a longer duration.
Han et al. found that offending vessels and herpes simplex virus (HSV) were significantly associated with DFP [10]. However, when we performed a multivariate logistic regression analysis of the characteristics of all patients and all intraoperative findings, we did not find any factors that were clearly associated with DFP, except for hypertension (OR 4.226, 95 % CI 1.089–16.401, p = 0.037). We believe that the reason our findings differed from those of Han et al. was because they did not exclude co-founders in their study through a multivariate analysis. In our study, according to the logistic analyses, we excluded offending vessels from the analysis of factors possibly associated with DFP. Furthermore, because the sample of patients with HSV infection was small (n = 1), we did not include this variable in our logistic regression analysis. Therefore, hypertension was the only risk factor of DFP identified in our study. A logistic regression analysis performed by Savadi-Oskouei et al. showed that hypertension could not independently predict the occurrence of Bell’s palsy in patients under 40 years of age, whereas for older patients, the odds ratio for hypertensive patients developing Bell’s palsy was 4.5 (95 % CI 2.5–8.1) [19]. Multiple studies have presented physiological theories to explain the relationship between facial paralysis and hypertension [1, 19]. Although the true etiology of facial palsy is unknown, there is sufficient evidence to support a probable association between hypertension and facial palsy. Small hemorrhages into the facial canal (similar to retinal hemorrhages) and partial neural necrosis may explain the association between hypertension and facial palsy [1, 13]. Another study involving a lager population needs to be undertaken to support our results.
The pathophysiological mechanism of DFP remains unclear, particularly because it can occur up to several days after surgery. Lovely et al. reported that DFP is not likely attributable to direct trauma to the nerve. Blood vessel migration can stretch the nerve and result in facial weakness, although the consistent timing and tight window of onset for DFP makes this an unlikely cause of DFP [15]. A viral cause of DFP has been suggested; manipulation of the nerve can stimulate a dormant virus, possibly localized in the geniculate ganglion [3, 5, 15, 18]. Furthermore, surgery is a major stress on the immune system, and this may contribute to viral reactivation [7]. Han et al. and Rhee et al. identified patients infected with HSV following MVD, although none of these patients developed DFP. Unfortunately, the diagnosis of HSV infection in their study was not based on a serological test for specific HSV antibodies but rather was based on clinical symptoms, such as watery blisters on the skin or mucous membranes of the mouth and lips [10, 17]. Kuroki et al. found that not all patients with DFP were positive for the CSF IgM antibody to HSV [14]. Therefore, the possible viral etiology of DFP requires further clarification. Some authors have proposed that neural edema may be the pathophysiological cause of DFP. Neural edema mainly occurs at the level of the meatal foramen, and thus it could have a deleterious function at the fundus of the internal auditory meatus, the narrowest portion of the Fallopian canal [4, 6, 16]. However, the timing of neural edema with respect to surgery is such that delayed swelling is unlikely.
The best method of treatment for patients with DFP remains controversial because the etiology of DFP is unknown, and DFP most commonly spontaneously resolves with excellent outcomes. Rhee et al. used steroid therapy for patients with DFP based on the hypothesis of neural edema as the cause of DFP, and Hengstman et al. treated patients with intravenous acyclovir based on the hypothesis of virus infection as the cause of DFP [7, 17]. Only one patient in our study was infected with HSV (based on clinical symptoms), and antiviral therapy was used to treat that patient. Four patients received acupuncture therapy in our study, and the other patients did not receive any treatment. Therefore, it is unclear whether treatment is necessary for patients with DFP, as most patients with DFP experience complete resolution of the disease. DFP may be a self-healing disease; i.e., DFP may spontaneously resolve without any treatment.
Conclusions
Although the degree of facial palsy was variable, most patients experienced a complete recovery without any special treatment. DFP may be a self-healing disease; i.e., DFP may spontaneously resolve without any treatment. The onset time and duration of DFP after MVD are correlated: an earlier development of DFP corresponds to a shorter duration, and a later development of DFP corresponds to a longer duration. Additionally, our results suggest that hypertension contributes to DFP.
References
Bademosi O, Ogunlesi TO, Osuntokun BO (1987) Clinical study of unilateral peripheral facial nerve paralysis in Nigerians. Af J Med Sci 16:197–201
Barker FGJP, Bissonette DJ (1995) Microvascular decompression for hemifacial spasm. J Neurosurg J Neurosurg 82:201–210
Franco-Vidal V, Nguyen DQ, Guerin J, Darrouzet V (2004) Delayed facial paralysis after vestibular schwannoma surgery: role of herpes viruses reactivation—our experience in eight cases. Otol Neurotol 25:805–810
Franco-Vidal VN, Guerin J, Darrouzet V (2004) Delayed facial paralysis after vestibular schwannoma surgery: role of herpes virus reactivation-our experience in eight cases. Otol Neurotol: Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol 25:805–810
Furukawa K, Sakoh M, Kumon Y, Teraoka M, Ohta S, Ohue S, Hatoh N, Ohnishi T (2003) Delayed facial palsy after microvascular decompression for hemifacial spasm due to reactivation of Varicella zoster virus. Neurol Surg 31:899–902
Gianoli GJ, Kartush JM (1996) Delayed facial palsy after acoustic neuroma resection: the role of viral reactivation. Am J Otol 17:625–629
Hengstman GJ, Gons RA, Menovsky T, Lunel FV, van de Vlasakker CJ, de Vries J (2005) Delayed cranial neuropathy after neurosurgery caused by herpes simplex virus reactivation: report of three cases. Surg Neurol 64:67–69, discussion 69–70
Huh R, Han IB, Moon JY, Chang JW, Chung SS (2008) Microvascular decompression for hemifacial spasm: analyses of operative complications in 1582 consecutive patients. Surg Neurol 69:153–157
Hyun SJ, Kong DS, Park K (2010) Microvascular decompression for treating hemifacial spasm: lessons learned from a prospective study of 1,174 operations. Neurosurg Rev 33:325–334
Han J-S, Lee J-A, Kong D-S, Park K (2012) Delayed cranial nerve palsy after microvascular decompression for hemifacial spasm. J Korean Neurosurg Soc 52:288–292s. doi:10.3340/jkns.2012.52.4.288
Jannette P (1998) Typical or atypical hemifacial spasm. J Neurosurg 89:346–347
Kim BTHS, Chang JC, Shin WH (1999) Delayed facial palsy following microvascular decompression in hemifacial spasm. J Korean Neurosurg Soc 28:1332–1336
Kumar S, Jain S, Diwan SK, Mahajan SN (2011) Severe systemic hypertension presenting with infranuclear facial palsy. Int J Nutr Pharmacol Neurol Dis 1:83. doi:10.4103/2231-0738.77540
Kuroki A, Itagaki S, Nagai O (1991) Delayed facial palsy after microvascular decompression for hemifacial spasm. Facial Nerve Res 11:147–150
Lovely TJ, Getch CC, Jannetta PJ (1998) Delayed facial weakness after microvascular decompression of cranial nerve VII. Surg Neurol 50:449–452
Menovsky TVOJ, Graham MD (1999) On the mechanism of transient postoperative deficit of cranial nerve. Surg Neurol 51:223–226
Rhee DJ, Kong DS, Park K, Lee JA (2006) Frequency and prognosis of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 148:839–843, discussion 843
Samii M, Gunther T, Iaconetta G, Muehling M, Vorkapic P, Samii A (2002) Microvascular decompression to treat hemifacial spasm: long-term results for a consecutive series of 143 patients. Neurosurgery 50:712–718, discussion 718–719
Savadi-Oskouei D, Abedi A, Sadeghi-Bazargani H (2008) Independent role of hypertension in Bell’s palsy: a case–control study. Eur Neurol 60:253–257
Wang A, Jankovic J (1998) Hemifacial spasm: clinical findings and treatment. Muscle Nerve 21:1740–1747
Wilkins RH (1991) Hemifacial spasm: a review. Surg Neurol 36:251–277
Zhang H, Lei D, You C, Mao BY, Wu B, Fang Y (2013) The long-term outcome predictors of pure microvascular decompression for primary trigeminal neuralgia. World Neurosurg 79:756–762
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Lun-Xin Liu and Chang-Wei Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Liu, LX., Zhang, CW., Ren, PW. et al. Prognosis research of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir 158, 379–385 (2016). https://doi.org/10.1007/s00701-015-2652-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2652-9