Abstract
Introduction
Description of syrinx resolution after posterior fossa decompression (PFD) in patients with scoliosis secondary to Chiari malformation type I (CMI) and syringomyelia (SM) has been rarely reported in the literature. This study was performed to investigate the outcome of PFD in patients with scoliosis secondary to CMI and to identify potential predictive factors for better outcome after PFD.
Material and methods
Patients with scoliosis secondary to CMI and SM, who had undergone PFD during the period 2000 through 2009, were recruited. Inclusion criteria were (1) age ≤ 18 years, (2) diagnosis of SM associated with CMI, (3) scoliosis as the first complaint, (4) having undergone preoperative and follow-up magnetic resonance imaging (MRI). Patients with acquired CMI anomalies or who had received syringosubarachnoid shunting were excluded. The maximal S/C ratio and syrinx length were measured to evaluate syrinx resolution after PFD. A 20% decrease in S/C ratio or length at the latest follow-up was defined as a significant radiographic improvement and complete resolution was used to describe the syrinx disappearing after PFD.
Results
44 patients were recruited. Follow-up MRI was conducted for all 44 patients at 6 ± 3 months postoperatively, for 37 patients at 2 years ± 3 months, for 26 patients at 4 years ± 3 months, and for 15 patients at 6 years ± 3 months. 97.7% (43 of 44) of patients showed significant radiographic improvement by MRI. The distance of tonsillar descent (mm) was correlated significantly with the surgical outcome (r = 0.116, P = 0.013). Significant improvement was observed within 6 months postoperatively, with continued slow improvement after that.
Conclusion
Syringes showed significant improvement after PFD in most patients with scoliosis secondary to CMI. Resolution generally occurred within 6 months follow-up and continued at a slow rate for several years. In addition, the severity of tonsillar descent is a potential predictor for better improvement after standard PFD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Understanding of the pathomechanism of syrinx formation and progression is crucial for surgeons in their selection of a surgical approach for syringomyelia (SM) secondary to Chiari malformation type I (CMI). There is broad consensus on the role of mechanical blockage of cerebrospinal fluid flow at the craniocervical junction in the pathogenesis of SM secondary to CMI [1, 2]. Posterior fossa decompression (PFD) is currently preferred by most surgeons as the standard surgical option in the treatment of SM secondary to CMI [3–6]. This results in decompression of the cerebellar tonsil restores the normal cerebrospinal fluid flow [7]. Several studies have shown the effectiveness of PFD for treatment of syrinx in these patients: 50–100% experienced a decrease in size of spinal cavity [5, 8–11]. Recently, Wetjen et al. [12] performed a serial magnetic resonance imaging (MRI) study to establish the time course for syrinx resolution after PFD and found that the syrinx began to resolve within 3.6 months after decompression and continued to decrease for months to years. However, these studies included patient populations with a broad age range, resulting in lack of consideration of the age influence on syrinx resolution. In addition, a wide variety of surgical procedures as adjuvants to standard PFD, including syringosubarachnoid shunting, obex plugging and resection of the cerebellar tonsil, have been advocated in previous studies, which potentially induce bias with respect to the evaluation of syrinx resolution. To date, few reports have quantitatively evaluated syrinx resolution after PFD or identified predictive factors for better improvement. In addition to occipital pain and vertigo, scoliosis is one of the most frequent clinical presentations in children and adolescents with CMI; it is sometimes the first symptom leading to clinical consultation. The present study focused on pediatric patients with CMI and scoliosis as their chief complaint. The aim was to perform a serial investigation of the time course of syrinx resolution in the absence of syrinx shunting and to identify potential predictive factors for better improvement after standard PFD.
Patients and methods
Patients
This retrospective study included patients with CMI who underwent PFD for SM at our center during the period from September 2000 to April 2009. Patients were selected according to the following inclusion criteria: (1) age ≤ 18 years, (2) diagnosed with SM secondary to CMI, (3) scoliosis as the first complaint, (4) having undergone preoperative and follow-up MRI. Patients with acquired CMI anomalies, any form of syrinx shunting, congenital spinal cord deformity or congenital spinal deformity were excluded.
A total of 44 patients who met the above-mentioned inclusion criteria were recruited, including 26 men and 18 women with a mean age of 12.1 years (range 6–18 years) and a mean follow-up duration of 3.8 years (range 3 months–6.3 years) (Table 1). The mean Cobb angle of the major curve at surgery was 47.1° (range 25°–92°). A single thoracic curve was identified in 30 patients (68.2%), in whom 15 were left-sided. There were one patient with a left thoracolumbar curve, two with a left lumbar curve, one with a right thoracolumbar curve, and one with a right lumbar curve. The remaining nine patients had double major curves.
Surgical procedure
The surgical technique for PFD, which consisted of suboccipital craniectomy, C-1 laminectomy and duraplasty, was standardized for all recruited patients, as described by Isu [13]. Patients were placed in the prone position with the head fixed in a horseshoe head holder. The craniectomy usually extended from the foramen magnum upward to the inferior nuchal line of the occipital bone. This area typically measured 3 cm in width and 3 cm in height. It was necessary to ensure adequate decompression of the rim of the foramen magnum. The posterior arch of C-1 was also resected until the maximal diameter of the C-1 arch was exposed. The dura was opened in a Y-shaped fashion in a cranial to spinal direction, keeping as much of the arachnoid membrane intact as possible. The dura was subsequently closed with a piece of deep fascia, and the midline incision was sutured to complete the surgical procedure.
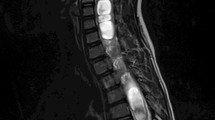
Radiographic evaluation
All patients underwent preoperative MRI of the entire spinal cord with a 1.5-T MRI system (Gyroscan Intera; Philips Medical Systems, Best, The Netherlands). Sagittal images were obtained using T1-weighted and T2-weighted spin-echo techniques with 3-mm sections and 2.5-mm intersectional gaps, which were set as a routine imaging protocol. Follow-up MRI was conducted with the same technique at 6 months (±3 months), 2 years (±3 months), 4 years (±3 months), and 6 years (±3 months) after decompression surgery. The severity of cerebellar tonsillar descent and features of the syrinx were evaluated via measurement of the following indices on the T1-weighted sagittal MRI: the distance of cerebellar tonsillar descent (mm), the configuration of the syrinx, the maximal syrinx/cord (S/C) ratio and length of the syrinx (Fig. 1). The extent of cerebellar tonsillar descent was further classified into three grades (Fig. 2) [14]: grade I, in which the tonsil descended beyond the foramen magnum but did not reach the C-1 arch; grade II, in which the tonsil reached the C-1 arch; and grade III, in which the tonsil descended beyond the C-1 arch. Syrinx configuration was categorized into distended, moniliform, slender, and circumscribed types (Fig. 3) [14]. The maximal anteroposterior diameter of the syrinx (S) divided by the anteroposterior diameter of the spinal cord (C) at the same level provided the maximal S/C ratio [15]. Syrinx length was defined as the number of vertebral segments spanned by the syrinx. Syrinx resolution was defined as any demonstrable decrease in maximal S/C ratio or length. Any postoperative decrease in the maximal S/C ratio or syrinx length divided by the preoperative value was calculated as a radiographic improvement rate. A radiographic evaluation was performed with the above-mentioned indices for each patient before decompression and at each follow-up. Significant improvement of syrinx was defined as any more than 20% decrease in maximal S/C ratio or length on follow-up MRI, and complete resolution was used to describe the syrinx disappearing after PFD.
Data analysis
The craniocervical junction was considered to be decompressed when a wider cisterna magna was detected on postoperative sagittal MRI. Descriptive statistics, independent-sample t test, and multiple linear regression analysis were performed. The improvement rate after PFD was calculated for each patient, and an independent-sample t test was performed to investigate the influence of age and sex on the outcome of PFD. Associations between improvement rate and the distance of cerebellar tonsil descent (mm), curve magnitude, and particularly, preoperative size of the syrinx were explored by multiple linear regression. Statistical analyses were performed with SPSS 13 software (SPSS, Chicago, IL, USA). For all analyses, statistical significance was set at P < 0.05.
Results
Based on detailed history-taking and physical examination at presentation, the following symptoms and signs were identified: occipital pain in 10 patients (22.7%), vertigo in 5 (11.4%), unilateral absence of abdominal reflex in 14 (31.8%), paresthesia in 6 (13.0%) and extremity weakness in 5 (11.4%). Relief of symptoms and physical signs was achieved in 21 patients (47.7%) immediately after surgery and in 37 patients (84.1%) at the final follow-up. No neurologic complications occurred in this series of patients. Superficial infection occurred in four cases (9.1%). In addition to the above, nine patients (20.5%) experienced transient headache, two (4.5%) experienced incisional cerebrospinal fluid leakage, and one (2.3%) experienced transient intracranial hypertension after surgery.
In our series, the Cobb angle of the main curve ranged from 25° to 92°. There were 18 patients, in whom the Cobb angle of main curve was more than 50°, receiving surgical correction of scoliosis six months after PFD. The 26 remaining patients received a bracing treatment for their scoliosis after PFD. After the mean follow-up duration of 2.3 years, 15 patients had no obvious progression of scoliosis while 11 patients had a curve progression. Of these 11 patients, 10 patients underwent surgical correction of scoliosis when Cobb angle of scoliosis progressed over 50°.
Preoperative MRI demonstrated tonsillar herniation of grade I in 24 patients, grade II in 18, and grade III in 2 (Table 1). Syrinx configuration was identified as distended type in 6 patients, moniliform type in 11, slender type in 11 and circumscribed type in 16.
Follow-up MRI was conducted for all 44 patients at 6 ± 3 months postoperatively, for 37 patients at 2 years ± 3 months, for 26 patients at 4 years ± 3 months, and for 15 patients at 6 years ± 3 months. 81.8% (36/44) of these patients achieved the criteria of significant improvement within 6 months after surgery, and 97.7% (43/44) achieved significant improvement by the final follow-up. The time course for syrinx resolution, in terms of syrinx size, among these patients is shown in Figs. 4, 5 and 6. The syrinx resolved substantially in most patients within 6 months. 17 patients showed complete syrinx resolution within 6 months after surgery, and 20 patients showed complete resolution at 6 years. No significant syrinx improvement was observed in some patients at 6 months after decompression; however, this was followed by a significant improvement at the next visit.
A 6-year-old girl with Chiari malformation type I and left thoracic scoliosis. Preoperative magnetic resonance images (a, f) showed that the cerebellar tonsils descended 8.7 mm below the foramen magnum and also showed a syrinx with a maximal S/C ratio of 0.866 and a length of 11 vertebrae. The 6-month postoperative (b, g), 2-year postoperative (c, h), 4-year postoperative (d, i), and 6-year postoperative (e, j) magnetic resonance images showed that the volume of the posterior fossa had increased and the syrinx had disappeared by the first postoperative follow-up. An X-ray image (k) showed that the patient had a left thoracic curve with a Cobb angle of 50° at diagnosis
A 7-year-old girl with Chiari malformation type I and right thoracic scoliosis. Preoperative magnetic resonance images (a, e) showed that cerebellar tonsils had descended 15.2 mm below the foramen magnum and also showed a syrinx with a maximal S/C ratio of 0.900 and a length of 11 vertebrae. The 6-month postoperative magnetic resonance images (b, f) showed that the volume of the posterior fossa had increased, the S/C ratio had decreased to 0.263, and the length of the syrinx had decreased to 4 vertebrae. The 2-year postoperative magnetic resonance images (c, g) showed that the S/C ratio was 0.261, and the length of the syrinx was 3 vertebrae. The 4-year postoperative magnetic resonance images (d, h) showed that the S/C ratio was 0.151, and the length of the syrinx was 1 vertebra
Correlation analyses were conducted to assess associations between syrinx improvement rate and potential predictors including age, sex, syrinx configuration, cerebellar tonsillar descent, follow-up duration, and curve magnitude. Multiple linear regression analysis revealed that only the distance of cerebellar tonsillar descent (mm) before surgery was positively correlated with improvement rate (P = 0.013), but it contributed only a little to the improvement rate (r cerebellar tonsillar descent = 0.116) (Table 2). Other factors, such as syrinx configuration, curve magnitude, and follow-up duration, were found to have no correlation with improvement rate.
Discussion
The outcome of PFD for the treatment of SM secondary to CMI has varied widely in previous studies in terms of maximal S/C ratio and syrinx length. Hida et al. [8] reported that 30 of 33 patients with SM secondary to CMI exhibited obvious syrinx resolution after PFD. Depreitere et al. [16] reported that 80% of patients (16/20) showed a favorable result consisting of complete syrinx resolution in 8 patients and obvious syrinx reduction in another 8. Wetjen et al. [12] documented the time course of syrinx resolution after PFD and found that the syrinx resolved significantly over a short period of time after decompression. Significant improvement was also reported in 7 of 7 patients in a study by Feldstein and Choudhri [17] and 11 of 12 in a study by Ghanem et al. [18]. However, low rates of significant improvement have also been reported. In studies by Caldarelli and colleagues and McGirt and colleagues, syrinx resolution after PFD was found only in 50 and 62% of patients, respectively [10, 19]. This discordance may be related to broad age range, different surgical procedures, or variability in the definition of significant improvement. In general, pediatric patients have a better response to PFD than adults [5], implying that the more pediatric patients recruited for a study, the better the surgical outcome. Different surgical procedures might decompress the cerebellar tonsils to different extents or even exert a direct effect on the syrinx, resulting in different rates of significant syrinx improvement [4, 8, 20–23]. Variability in the definition of significant improvement also may have led to contrary results among previous reports.
To explore the course of syrinx resolution after PFD in a scoliosis population, patients with a complaint of scoliosis were recruited for the present study. To avoid the influence of age and surgical procedure on syrinx resolution, we recruited CMI patients with the age of less than or equal to 18 years and excluded patients with any form of syrinx shunting to quantitatively evaluate the outcome of PFD.
In the present study, patients with a >20% decrease in syrinx size were defined as having significant improvement. Significant syrinx improvement was identified in 43 of 44 patients (97.7%) approximately 6 years after decompression. This was relatively higher than that reported by Munshi and colleagues and Depreitere and colleagues [16, 24]. This is consistent with the fact that pediatric patients experience less permanent neurologic injury and higher improvement rates after PFD, owing to their enhanced repair capability and short clinical history [5, 25, 26].
The time course of syrinx resolution after PFD has not been well documented, although it is known that syrinx can resolve within weeks of this procedure [8]. Results of the present study showed significant syrinx improvement in 81.8% (36/44) of patients, with stable syrinx in 18.2% (8/44) within 6 months after surgery. Stable syringes improved with time, with significant improvement in 97.7% (43/44) of patients by 6 years after surgery. Interestingly, it was noted that in most patients, syrinx size continued to decrease slowly over time. This is consistent with the results of the Wetjen et al. [12].
Several factors, such as sex, preoperative size and syrinx length, have been reported as predictors of better surgical outcome after PFD [4, 5, 20]. Badie et al. [27] reported that female patients have a better response to PFD than male patients because female patients have a lower posterior fossa volume. In a study by Park et al. [20], it was found that the longer the syrinx, the better the outcome. To identify other potential predictive factors, we used multiple linear regressions. With the exception of distance of cerebellar tonsil descent, which showed a small contribution to the improvement rate at the last follow-up (P = 0.013, r the degree of cerebellar tonsil descending = 0.116), no association between the factors assessed, including sex, syrinx configuration, follow-up duration, curve magnitude, or improvement rate at the final follow-up, was found. Patients with more severe cerebellar tonsillar descent often have a worse cerebrospinal fluid abnormality. After PFD, the cerebellar tonsils are decompressed and cerebrospinal fluid flow is restored, resulting in more benefit from PFD. Considering that the patients in the present study were relatively young, we suggest that extrapolation of the above findings should be restricted to pediatric patients with CMI.
A potential limitation of the present study was the retrospective nature, such that the follow-up duration varied widely. This limitation would influence the power of the study. Nonetheless, we believe that the present results can document the time course of syrinx resolution in patients with scoliosis secondary to CMI and SM. We found significant syrinx improvement after PFD in most pediatric patients with CMI, particularly within the initial several months after surgery. Severe tonsillar descent might be a predictor of better surgical outcome after PFD
References
Milhorat TH, Nishikawa M, Kula RW, Dlugacz YD (2010) Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as guide to clinical management. Acta Neurochir (Wien) 152:1117–1127. doi:10.1007/s00701-010-0636-3
McGirt MJ, Atiba A, Attenello FJ, Wasserman BA, Datoo G, Gathinji M, Carson B, Weingart JD, Jallo GI (2008) Correlation of hindbrain CSF flow and outcome after surgical decompression for Chiari I malformation. Childs Nerv Syst 24:833–840. doi:10.1007/s00381-007-0569-1
Tubbs RS, Lyerly MJ, Loukas M, Shoja MM, Oakes WJ (2007) The pediatric Chiari I malformation: a review. Childs Nerv Syst 23:1239–1250. doi:10.1007/s00381-007-0428-0
Durham SR, Fjeld-Olenec K (2008) Comparison of posterior fossa decompression with and without duraplasty for the surgical treatment of Chiari malformation Type I in pediatric patients: a meta-analysis. J Neurosurg Pediatr 2:42–49. doi:10.3171/PED/2008/2/7/042
Navarro R, Olavarria G, Seshadri R, Gonzales-Portillo G, McLone DG, Tomita T (2004) Surgical results of posterior fossa decompression for patients with Chiari I malformation. Childs Nerv Syst 20:349–356. doi:10.1007/s00381-003-0883-1
Xie J, Wang Y, Zhao Z, Zhang Y, Si Y, Yang Z, Liu L, Lu N (2011) One-stage and posterior approach for correction of moderate to severe scoliosis in adolescents associated with Chiari I malformation: is a prior suboccipital decompression always necessary? Eur Spine J 20:1106–1113. doi:10.1007/s00586-011-1717-6
Hankinson TC, Klimo P Jr, Feldstein NA, Anderson RC, Brockmeyer D (2007) Chiari malformations, syringohydromyelia and scoliosis. Neurosurg Clin N Am 18:549–568. doi:10.1016/j.nec.2007.04.002
Hida K, Iwasaki Y, Koyanagi I, Sawamura Y, Abe H (1995) Surgical indication and results of foramen magnum decompression versus syringosubarachnoid shunting for syringomyelia associated with Chiari I malformation. Neurosurgery 37:673–678 (discussion 678–679)
Alzate JC, Kothbauer KF, Jallo GI, Epstein FJ (2001) Treatment of Chiari I malformation in patients with and without syringomyelia: a consecutive series of 66 cases. Neurosurg Focus 11:1–9. doi:10.3171/foc.2001.11.1.4
Caldarelli M, Novegno F, Vassimi L, Romani R, Tamburrini G, Di Rocco C (2007) The role of limited posterior fossa craniectomy in the surgical treatment of Chiari malformation type I: experience with a pediatric series. J Neurosurg 106:187–195. doi:10.3171/ped.2007.106.3.187
Takayasu M, Takagi T, Hara M, Anzai M (2004) A simple technique for expansive suboccipital cranioplasty following foramen magnum decompression for the treatment of syringomyelia associated with Chiari I malformation. Neurosurg Rev 27:173–177. doi:10.1007/s10143-004-0338-5
Wetjen NM, Heiss JD, Oldfield EH (2008) Time course of syringomyelia resolution following decompression of Chiari malformation type I. J Neurosurg Pediatr 1:118–123. doi:10.3171/PED/2008/1/2/118
Isu T, Sasaki H, Takamura H, Kobayashi N (1993) Foramen magnum decompression with removal of the outer layer of the dura as treatment for syringomyelia occurring with Chiari I malformation. Neurosurgery 33:844–849 (discussion 849–850)
Ono A, Ueyama K, Okada A, Echigoya N, Yokoyama T, Harata S (2002) Adult scoliosis in syringomyelia associated with Chiari I malformation. Spine (Phila Pa 1976) 27:E23–E28
Qiu Y, Zhu ZZ, Wang B, Yu Y, Qian BP, Zhu F (2008) Radiological presentations in relation to curve severity in scoliosis associated with syringomyelia. J Pediatr Orthoped 28:128–133
Depreitere B, Van Calenbergh F, van Loon J, Goffin J, Plets C (2000) Posterior fossa decompression in syringomyelia associated with a Chiari malformation: a retrospective analysis of 22 patients. Clin Neurol Neurosurg 102:91–96. doi:10.1016/S0303-8467(00)00073-1
Feldstein NA, Choudhri TF (1999) Management of Chiari I malformations with holocord syringohydromyelia. Pediatr Neurosurg 31:143–149. pii: pne31143
Ghanem IB, Londono C, Delalande O, Dubousset JF (1997) Chiari I malformation associated with syringomyelia and scoliosis. Spine (Phila Pa 1976) 22:1313–1317 (discussion 1318)
McGirt MJ, Attenello FJ, Atiba A, Garces-Ambrossi G, Datoo G, Weingart JD, Carson B, Jallo GI (2008) Symptom recurrence after suboccipital decompression for pediatric Chiari I malformation: analysis of 256 consecutive cases. Childs Nerv Syst 24:1333–1339. doi:10.1007/s00381-008-0651-3
Park YS, Kim DS, Shim KW, Kim JH, Choi JU (2009) Factors contributing improvement of syringomyelia and surgical outcome in type I Chiari malformation. Childs Nerv Syst 25:453–459. doi:10.1007/s00381-008-0763-9
Attenello FJ, McGirt MJ, Gathinji M, Datoo G, Atiba A, Weingart J, Carson B, Jallo GI (2008) Outcome of Chiari-associated syringomyelia after hindbrain decompression in children: analysis of 49 consecutive cases. Neurosurgery 62:1307–1313 (discussion 1313). doi:10.1227/01.neu.0000333302.72307.3b
Nishikawa M, Ohata K, Baba M, Terakawa Y, Hara M (2004) Chiari I malformation associated with ventral compression and instability: one-stage posterior decompression and fusion with a new instrumentation technique. Neurosurgery 54:1430–1434 (discussion 1434–1435)
Tubbs RS, McGirt MJ, Oakes WJ (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg 99:291–296. doi:10.3171/jns.2003.99.2.0291
Munshi I, Frim D, Stine-Reyes R, Weir BK, Hekmatpanah J, Brown F (2000) Effects of posterior fossa decompression with and without duraplasty on Chiari malformation-associated hydromyelia. Neurosurgery 46:1384–1389 (discussion 1389–1390)
Milhorat TH, Johnson WD, Miller JI, Bergland RM, Hollenberg-Sher J (1992) Surgical treatment of syringomyelia based on magnetic resonance imaging criteria. Neurosurgery 31:231–244 (discussion 244–235)
Cai C, Oakes WJ (1997) Hindbrain herniation syndromes: the Chiari malformations (I and II). Semin Pediatr Neurol 4:179–191
Badie B, Mendoza D, Batzdorf U (1995) Posterior fossa volume and response to suboccipital decompression in patients with Chiari I malformation. Neurosurgery 37:214–218
Acknowledgments
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. This work was supported by the National Natural Science Foundation of China (Grant No. 81171672).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
T. Wu and Z. Zhu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wu, T., Zhu, Z., Jiang, J. et al. Syrinx resolution after posterior fossa decompression in patients with scoliosis secondary to Chiari malformation type I. Eur Spine J 21, 1143–1150 (2012). https://doi.org/10.1007/s00586-011-2064-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-2064-3