Abstract
The benefits of osteoplastic suboccipital craniotomies over the traditional suboccipital craniectomies have been recognized. We describe a simple method of expansive suboccipital cranioplastic craniotomy using a free bone flap and report satisfactory clinical results in 16 patients with syringomyelia associated with Chiari I malformation. A free suboccipital bone flap is created from the rostral part of the occiput by placing two to four burr holes and connecting them with a craniotome. The posterior bony margin of the foramen magnum and the posterior arch of C1 are removed thereafter. Then dural plasty using a patch graft of dural substitutes is performed. The expansive suboccipital cranioplasty is performed by positioning the free bone flap caudal to the original location and fixing it with titanium miniplates to construct a bony frame to cover the foramen magnum. The rostral part of the cranial defect is filled with bone chips created during the craniotomy. Sixteen patients underwent this procedure. There was no operative mortality and no major complication, such as persistent pseudomeningocele. Preoperative symptoms improved significantly in all patients except for one who had persistent dysesthetic pain. Our simple method of expansive suboccipital cranioplasty for the treatment of syringomyelia associated with Chiari I malformation proved useful and achieved satisfactory long-term results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefits of suboccipital craniotomies over the traditional suboccipital craniectomies have been recognized. Recently, Gnanalingham et al. have clearly shown that craniotomy significantly decreases postoperative cerebrospinal fluid leakage and pseudomeningoceles compared with craniectomy in surgical procedures for posterior fossa tumors in children [2]. For foramen magnum decompression for syringomyelia associated with Chiari malformation, suboccipital cranioplastic craniotomy has further advantages over conventional craniectomy. The rigid bony frame secures the enlarged cisterna magna and prevents postoperative restenosis by epidural scar tissue formation. In addition, cerebellar ptosis following suboccipital craniectomy, which is rare but carries potentially severe consequences, can be prevented by cranioplasty [4].
A method for expansive suboccipital cranioplastic craniotomy using iliac bone grafts to treat syringomyelia associated with Chiari malformation was reported; however, it was too complicated for routine usage [12, 14]. We have devised a simple method for expansive suboccipital cranioplasty using a suboccipital free bone flap and achieved favorable long-term results [13].
Patients and methods
Operative procedure
To begin, en bloc suboccipital craniotomy, leaving the posterior margin of the foramen magnum, is performed. These patients typically have small posterior cranial fossae with thick internal occipital cristas, making the procedure more difficult than usual [8]. Craniotomy is started by placing two or four burr holes, which then are connected with a craniotome (Fig. 1). The well-developed internal occipital cristae (11 out of 16 patients) are thinned and disconnected at their middle using an air drill to complete the craniotomy. The posterior bony margin of the foramen magnum is removed under an operating microscope using an air drill, Kerrison punches, and rongeurs. The posterior arch of C1 also is resected until the maximum diameter of the C1 arch is exposed. When the tonsilar herniation extends below C2, the upper part of the C2 lamina is also removed. This procedure was required in seven of 16 patients. Bony chips created during these procedures were saved for cranioplasty for the rostral part. Usually a thick layer of epidural fibrosis is found in the interlaminar space between C1 and C2. The dura is opened using a Y-shaped incision from the cranial to the spinal direction, keeping as much of the arachnoid membrane intact as possible. The arachnoid membrane is not opened, except when arachnoiditis is obvious at the dorsal aspect of the foramen magnum cistern. There was no such case in this series. The dura is closed with a patch graft of dural substitutes, which is sealed with fibrin glue (Fig. 1). For dural substitutes, Goatex dura was used for the eight most recent patients, the fascia lata for one, and Lyodura for the initial five patients. Then expansive cranioplasty is carried out as follows (Fig. 2). The bone flap is tailored to fit the caudal part of the cranial window. When the internal crista of the occipital bone is thick, it is removed. The flap is positioned caudal to the original site and fixed with titanium miniplates to construct a bony frame to cover the foramen magnum. The flap was replaced inside-out to achieve a better fit in nine of 16 patients. In more recent cases, the dural substitute was tacked to the center of the bone flap to keep the dorsal cistern of the foramen magnum expanded and to minimize the amount of epidural dead space. The bone chips created during craniotomy are packed into the rostral cranial defect and hardened with fibrin glue, completing the cranioplasty (Fig. 3).
Schematic drawing illustrating osteoplastic craniotomy and dural plasty. Since the internal occipital crista of the occipital bone is well-developed in most patients with Chiari I malformation, the middle parts of both the rostral and caudal craniotomy lines are thinned using an air drill. The dura is expanded with a patch graft of Goatex dural substitute, which is sealed with fibrin glue
Schematic drawing illustrating expansive cranioplasty. The bone flap is tailored to fit the caudal part of the cranial window. When the internal crista of the occipital bone is thick, it is removed. The flap is often replaced inside-out to achieve a better fit. The flap is positioned caudal to the original site and fixed with titanium miniplates and screws to construct a bony frame that covers the foramen magnum. The bone chips created during craniotomy are packed into the rostral cranial defect and hardened with fibrin glue, completing the cranioplasty
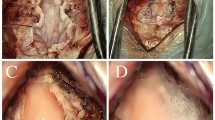
a, b Intraoperative photographs showing a the bone flap positioned caudal to the original site and fixed with titanium miniplates to construct a bony frame to cover the foramen magnum and b the bone chips packed into the rostral cranial defect. c, d Postoperative CT scans of c sagittal and d 3D reconstruction showing expansive suboccipital cranioplasty
Patient data
We have performed expansive suboccipital cranioplasty to syringomyelia associated with Chiari I malformation in 16 patients since 1992. Twelve were female and four were male, with a mean age of 32 years ranging from 13 to 61 years. The follow-up period was 2 months to 11 years. Preoperative symptoms and signs included sensory disturbances in 11 patients (69%), motor weakness in 7 (50%), brainstem and/or cerebellar signs in 5 (31%), and intractable pain in 4 (29%).
The degree of tonsillar herniation and syringomyelia were determined by magnetic resonance imaging (MRI) in all cases. The tonsillar herniation was classified into five categories depending on the position of the tip of the tonsil, i.e., posterior fossa, foramen magnum, C1, C1-2, and C2. Postoperative decrease in syrinx size was evaluated in each case. The clinical presentation and radiologic findings were evaluated periodically after surgery.
Results
The results of surgery were successful. There was no operative mortality and no major complication such as persistent pseudomeningocele. Preoperative symptoms and signs improved significantly within a few weeks in all patients, except for persistent dysesthetic pain in two patients, one of whom improved several months later.
The appearance of the tonsil and the syrinx on neuroimaging improved in all patients. Postoperative improvement of tonsillar herniation and syringomyelia was evaluated in 14 patients who were followed for more than 1 year (20 months to 11 years) (Fig. 4). The position of the tonsillar tip, between the C1 and C2 level preoperatively, ascended to the posterior fossa (71%) or foramen magnum (29%) postoperatively in all patients (Table 1). The size of the syrinx decreased in all patients with complete disappearance of the syrinx in four. Timing of improvement in neuroanatomy also was investigated. The first postoperative MRI was performed between 1 week and 3 months after surgery (mean; 4.5 weeks). Tonsillar ascent was noted in all patients indicating that the tonsillar ascent started earlier than 4.5 weeks on average. On the other hand, the size of the syrinx was unchanged in three patients on the first postoperative MRI (1 week, 3 weeks, and 2 months), although it did decrease in the rest of the patients. The second postoperative MRI was performed in these patients at 3, 4, and 7 months, respectively, by which time the size of the syrinx had decreased, indicating that the process had begun within 7.5 weeks on average.
Images obtained in a 20-year-old woman who presented with mild motor weakness and a bilateral sensory disturbance of the upper extremities. a Preoperative sagittal magnetic resonance imaging (MRI) showing tonsilar herniation at the level of C1 and a large syringomyelia. b,c Postoperative computed tomography shows successful expansive cranioplasty at the level of b the foramen magnum, and c the posterior fossa. d Sagittal MRI obtained 9 years postoperatively showing the persistency of the tonsillar ascent and decrease in the syrinx size
No patients developed recurrent symptoms and signs or a worsening picture on neuroimaging during follow-up except for one, who had recurrence of syringomyelia 3 years later. The cause of recurrence was most likely insufficient decompression of anomalous posterior fossa at the initial surgery. In the second operation, the bony notches at the cerebellar fossa of the occipital bone were resected and a syringo-subarachnoid shunt was placed to ensure that syringomyelia did not recur. Postoperative MRI showed ascent of the tonsils and marked decrease in the size of the syrinx.
Discussion
Foramen magnum decompression is the most effective and widely used procedure for treating syringomyelia associated with Chiari I malformation. However, conventional foramen magnum decompression frequently is accompanied by complications related to CSF leakage, such as persistent pseudomeningocele or meningitis [1, 3, 6]. Isu et al. [5] have advocated dividing only the outer layer of the dura mater in foramen magnum decompression to prevent these complications related to CSF leakage. However, that procedure is technically demanding, and decompression of the foramen magnum cisterns may be inadequate in some patients. Recently, Gnanalingham et al. have clearly shown that craniotomy significantly decreases postoperative cerebrospinal fluid leakage and pseudomeningocele compared with craniectomy in surgical procedures for posterior fossa tumors in children [2]. They proposed that the mechanism of CSF leakage might be related to tearing of the dural closure due to periodic dural bulging after craniectomy, while dural sutures might be prevented from tearing out after osteoplastic craniotomy because of dural bulging being pressed against the bone flap. We have not encountered intractable subcutaneous CSF retention after expansive cranioplasty because the epidural dead space is filled with both a bone flap and bone chips.
Furthermore, relapse of the symptoms has been reported in a significant proportion of patients with foramen magnum decompression [10]. The most common cause of relapse is restenosis of the dorsal cistern of the foramen magnum. Moreover, a complication with potentially severe consequences, cerebellar ptosis, also has been reported following large suboccipital craniectomy [4]. Therefore, posterior fossa reconstruction, rather than simple decompression, has been advocated.
One method of posterior fossa reconstruction has been reported by Sahuquillo et al. [11] in which a dural graft is tented to the fascial plane to avoid epidural scarring after craniectomy and laminectomy. However, the bony structure is not reconstructed in that procedure. The dorsal cistern of the foramen magnum can be held open more effectively using a bony frame constructed from the pieces of bone from the outer layer of the cranium and the ilium, as reported by Sakamoto et al. [12]. However, their method seems too complicated for routine use. For that reason, we developed a simple method for performing expansive suboccipital cranioplasty, in which a free cranial bone flap is simply repositioned to repair the bony defect and to construct a bony frame for the foramen magnum [13].
Radiologic studies confirmed the success of our method. Both tonsillar ascent and a decrease in syrinx size were noted in all patients on postoperative MRI. The average time for the syrinx to collapse was compatible with data reported by Hida et al. following foramen magnum decompression (6.3 weeks), which was slightly longer than after syringo-subarachnoid shunt (1.8 weeks) [3]. These differences in radiologic improvement may be related to the pathogenesis of syringomyelia associated with Chiari I malformation [9, 15]. The appearance of the operative site was acceptable in all patients, without development of wound depression, as commonly occurs after conventional suboccipital craniectomy.
The clinical results were also satisfactory. Symptoms remitted permanently in 13 patients within a few weeks. One patient complained of persistent dysesthetic pain; however, management of dysesthetic pain with causalgia-like features is often problematic, as pointed out by Milhorat et al. [7]. Another patient had recurrence of syringomyelia 3 years later, most likely due to incomplete decompression of the anomalous posterior fossa (bony notches at the cerebellar fossa of the occipital bone) in the initial operation, not related to restenosis of the dorsal cistern of the foramen magnum.
References
Cristane L, Westphal M, Hermann H-D (1994) Cranio-cervical decompression for Chiari I malformation. Acta Neurochir (Wien) 130:94–100
Gnanalingham KK, Lafuente J, Thompson D, Harkness W, Hayward R (2002) Surgical procedures for posterior fossa tumors in children: does craniotomy lead to fewer complications than craniectomy? J Neurosurg 97:821–826
Hida K, Iwasaki Y, Koyanagi I, Sawamura Y, Abe H (1995) Surgical indication and results of foramen magnum decompression versus syringosubarachnoid shunting for syringomyelia associated with Chiari I malformation. Neurosurgery 37:673–679
Holly LT, Batzdorf U (2001) Management of cerebellar ptosis following craniovertebral decompression for Chiari I malformation. J Neurosurg 94:21–26
Isu T, Sasaki H, Takamura H, Kobayashi N (1993) Foramen magnum decompression with removal of the outer layer of the dura as treatment for syringomyelia occurring with Chiari I malformation. Neurosurgery 33:845–850
Matsumoto T, Symon L (1989) Surgical management of syringomyelia—current results. Surg Neurol 32:258–265
Milhorat TH, Kotzen RM, MU HTM, Capocelli AL, Milhorat RH Jr (1996) Dysesthetic pain in patients with syringomyelia. Neurosurgery 38:940–947
Nishikawa M, Sakamoto H, Hakuba A, Nakanishi N, Inoue Y (1997) Pathogenesis of Chiari malformation: a morphometric study of the posterior cranial fossa. J Neurosurg 86:40–47
Oldfield EH, Muraszko K, Shawker TH, Patronas NJ (1994) Pathophysiology of syringomyelia associated with Chiari I malformation. J Neurosurg 80:3–15
Paul KS, Lye RH, Strang FA, Dutton J (1983) Arnold–Chiari malformation. J Neurosurg 58:183–187
Sahuquillo J, Rubio E, Poca M-A, Rovira A, Rodriguez-Baeza A, Cervera C (1994) Posterior fossa reconstruction: a surgical technique for the treatment of Chiari I malformation and Chiari I/syringomyelia complex—preliminary results and magnetic resonance imaging quantitative assessment of hindbrain migration. Neurosurgery 35:874–885
Sakamoto H, Nishikawa M, Hakuba A, Yasui T, Kitano S, Nakanishi N, Inoue Y (1999) Expansive suboccipital cranioplasty for the treatment of syringomyelia associated with Chiari malformation. Acta Neurochir (Wien) 141:949–961
Takayasu M, Nishizawa T, Yoshida J (2001) Simple expansive suboccipital cranioplasty following foramen magnum decompression for the treatment of syringomyelia associated with Chiari I malformation. In: Tamaki N, Batzdorf U, Nagashima T (eds) Syringomyelia, current concepts in pathogenesis and management. Springer, Tokyo, pp 159–163
Tokuno H, Hakuba A, Suzuki T, Nishikawa S (1998) Operative treatment of Chiari malformation with syringomyelia. Acta Neurochir Suppl 43:22–25
Williams B (1986) Progress in syringomyelia. Neurol Res 8:130–145
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takayasu, M., Takagi, T., Hara, M. et al. A simple technique for expansive suboccipital cranioplasty following foramen magnum decompression for the treatment of syringomyelia associated with Chiari I malformation. Neurosurg Rev 27, 173–177 (2004). https://doi.org/10.1007/s10143-004-0338-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-004-0338-5