Abstract
Objective
Symptom recurrence remains a problem for some patients after surgical decompression for Chiari I malformation. We set out to identify variables at presentation that could identify subgroups most likely to experience incomplete symptom relief after hindbrain decompression for Chiari I malformation.
Materials and methods
We retrospectively reviewed the records of all pediatric patients undergoing first-time suboccipital decompression for Chiari I malformation over a 10-year period. Measured outcomes included (1) persistence or recurrence of symptoms regardless of severity and (2) need for revision decompression.
Results
Two hundred fifty-six children (10 5years old) underwent surgery for Chiari I malformation and were followed up for a mean of 27months. Presenting symptoms included headache in 192 (75%) patients and brainstem or cranial nerve symptoms in 68 (27%) patients. Fifty-seven (22%) patients experienced mild to moderate symptom recurrence. Nineteen (7%) patients required revision decompression for significant symptom recurrence. Headache was 70% more likely to persist or recur versus cranial nerve or brainstem symptoms (relative risk 1.70, p < 0.05). Vertigo and frontal headache independently increased the odds of symptom recurrence 2.9- and 1.5-fold, respectively. Each increasing year of preoperative headache duration was independently associated with 15% increase in likelihood of symptom persistence (p < 0.05). Severe tonsilar ectopia (caudal to C2 lamina) was twice as likely to require revision decompression (14% versus 6%).
Conclusion
In our experience, recurrence of mild symptomatology not severe enough to justify revision surgery may occur in nearly a fifth of patients after surgery. Headache was more likely to recur than objective cranial nerve or brainstem symptoms. Increasing duration of headaches, frontal headaches, and vertigo may be more refractory symptoms of Chiari I malformation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type I Chiari malformation was originally described in 1891 as caudal displacement of the cerebellar tonsils through the foramen magnum [5]. Since its initial description, many symptoms of cerebellar, brainstem, and spinal cord pathology have been attributed to this complex disease [13, 22, 23]. The standard treatment for Chiari I malformation remains to be posterior fossa decompression [2, 8, 12]. Selection criteria for surgical intervention at many institutions remain solely based on degree of tonsillar ectopia and character of presenting symptoms. While short-term improvement of symptoms and physical signs have been reported in up to 75–90% of Chiari I patients following decompression, as many as 35% of patients may experience symptom recurrence years after surgery [3, 4, 6, 7, 10, 15–17, 19, 21]. Hence, identification of novel predictors of outcome is needed to better select patients most likely to benefit from surgical intervention.
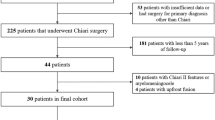
Many authors have reported large patient series of outcomes following surgical management of Chiari I malformation [3, 4, 6, 7, 10, 15–17, 19, 21]. However, studies assessing independent predictors of symptom recurrence are few and limited by smaller sample size, lack of multivariate analysis, and failure to account for cases of initial treatment response followed by subsequent symptom recurrence. Furthermore, most prior series define symptom failure as need for revision decompression, neglecting symptoms recurring or persisting to a less severe degree. In our series of 256 consecutive patients undergoing first-time hindbrain decompression for Chiari I malformation, we set out to assess the incidence of both treatment failure (need for revision decompression) and partial persistence of symptomatology. Furthermore, we attempt to identify preoperative signs, symptoms, and radiographic findings that may independently identify patient subgroups most likely to respond to surgical management versus those that are less responsive to surgery.
Materials and methods
Presenting symptomatology, neurological deficits, demographics, co-morbidities, pre- and postoperative radiological studies, operative records, and follow-up clinical records were reviewed in 256 consecutive patients undergoing first-time posterior fossa decompression for Chiari I malformation at the Johns Hopkins Hospital between 1995 and 2005. An electronic database was recorded by cataloging patient demographics, presenting symptoms, and degree of tonsil herniation. Additionally, the presence of syringomyelia, scoliosis, hydrocephalus, basilar invagination, fused cervical vertebrae, platybasia, atlanto-occipital assimilation, or cervico-medullary kinking on MRI were also identified and recorded. Patients with cranial, facial, or skeletal syndromes were not included in this analysis. All patients in this series were offered surgical decompression if they presented with symptoms consistent with Chiari I malformation (tussive headache, cervical pain, central apnea, dysphagia, aspiration, vertigo, vocal cord paralysis, motor/sensory deficits, nystagmus, ataxia, uncoordination, and syringomyelia) and demonstrated cerebellar tonsil herniation at least 5mm below the foramen magnum. Appropriate otolaryngology, pulmonary, and ophthalmological consultations were obtained to determine a central etiology of apnea, cranial nerve, and ophthalmological findings. All studied patients underwent bony decompression of the foramen magnum and C1 cervical laminectomy.
Surgical technique
The surgical technique for craniectomy and duraplasty was standardized for all reviewed patients performed by three surgeons (J.W., B.C., G.J.). All patients underwent surgery in the prone position with the head fixed in a Mayfield or a horseshoe head holder. A small suboccipital craniectomy and a C-1 laminectomy were performed. The craniectomy usually extended from the foramen magnum upward, including the inferior nuchal line of the occipital bone, covering the insertion area of the rectus capitis posterior minor muscle, and the medial insertion area of the rectus capitis posterior major muscle. This typically measured 3cm in width and 3cm in height. The surgeons ensured an adequate decompression of the rim of the foramen. The tonsils were visualized using intraoperative ultrasonography. If the tip of the tonsils could not be sufficiently exposed, a C-2 laminectomy was additionally performed. C2 laminectomy was avoided whenever possible. When performing duraplasty, the dura was opened in a Y-shaped fashion spanning the majority of the 3 × 3-cm craniectomy. The dura was closed with a triangular synthetic dural graft (Dura-Guard; Bio-Vascular, Inc., St. Paul, MN, ISA), pericranium, or Goretex patch ensuring the reconstruction of open CSF space at the craniospinal junction. The preoperative surgical plan for all cases was to perform duraplasty unless evidence of adequate bony hindbrain decompression was evident on intraoperative ultrasound (Prosound SSD 1000, Aloka Inc.). The intraoperative decision not to perform duraplasty was subjectively based on their interpretation of the intraoperative ultrasonography findings. Only patients that felt to have evidence of physiological systolic tonsilar pulsations and decompression of the subarachnoid spaces ventral and dorsal to tonsils after bony decompression did not receive duraplasty.
Outcome assessment
Patients’ response to surgery was first assessed at their 3-month follow-up visit to the clinic. If patients continued to demonstrate their preoperative symptoms consistent with Chiari malformation to any degree (excluding surgery related complaints) on consecutive follow-up visits, they were recorded as symptom recurrence. Symptomatology that was not considered to be related to Chiari malformation or associated with other identifiable factors was not considered symptom recurrence. The time of symptom recurrence was recorded as a function of months after surgery. Patients that never reported improvement with surgery were documented as such on their first (1-month) postoperative clinic visit. If symptoms persisted or recurred to a level of severity thought to be equivalent to the patient’s preoperative level, conservative management was first attempted. In patients with shunted hydrocephalus, recurrent Chiari-associated headache was only considered after head CT, Shunt X-rays, and radionucleotide shunt patency studies ruled out shunt malfunction. When marked symptom recurrence persisted and MRI suggested continued hindbrain crowding, revision decompression was offered. In cases of Chiari-associated syringomyelia, revision decompression was also offered if there was both clinical and radiographic evidence of worsening syrinx to any degree. The incidence of mild symptomatology not warranting revision surgery and more marked recurrent symptoms that resulted in reoperation were both documented and recorded. The incidence and time of radiographic change of Chiari-associated syrinx was also documented.
The Chiari I database was retrospectively analyzed to assess the independent association of presenting symptomatology, physical exam findings, radiological variables, and operative variables to postoperative symptom recurrence and revision surgery. Univariate comparison of symptom-improved survival was expressed as Kaplan–Meier plots and assessed via log-rank analysis for stratified co-variables and proportional-hazards regression analysis for continuous variables. A multivariate proportional-hazards regression model was then created to model symptom recurrence containing only variables demonstrating p values <0.1 in univariate analysis. Variables demonstrating a p value >0.1 in multivariate analysis were removed from the model (Fig. 1).
Results
Patient population
Two hundred fifty-six children underwent first-time surgery for Chiari I malformation over the reviewed time period. Mean ± SD age at time of surgery was 10 ± 5years, and 121 (47%) patients were male. Presenting symptoms are summarized in Table 1. Presenting symptoms included headache in 192 (75%) patients (mean duration, 12months) and brainstem or cranial nerve symptoms in 68 (23%; mean duration, 8months). Forty (15%) patients had headaches with a frontal component. In these cases, frontal headache was tussive with tonsil ectopia below C1 in all cases. Tonsil herniation did not descend below C1 in 38 (15%) patients, descended between C1 and C2 in 195 (76%) patients, and below C2 in 23 (9%) patients. Eight (3%) patients had epilepsy, 35 (14%) had shunted hydrocephalus, 69 (27%) had syringomyelia, and 29 (11%) patients had scoliosis at the time of surgical decompression. Of Chiari I patients with shunted hydrocephalus, 12 (34%) presented with headaches, six (17%) with syringomyelia, and 17 (48%) with lower cranial nerve dysfunction. All patients undergoing hindbrain decompression with concurrent Chiari I and shunted hydrocephalus demonstrated normal shunt function and intracranial pressure. Duraplasty was performed in 116 (45%) cases. Tonsil coagulation was performed in 17 (7%) cases.
Long-term symptom recurrence and revision surgery
Patients were followed up for a mean of 2 ± 1years. Seventy-four (27%) patients were followed up for >3years, and 42 (15%) were followed up for >4years postoperatively. Four (2%) patients developed perioperative surgical site infection. Two (1%) patients experienced an incisional CSF leak following duraplasty and required reoperation.
Fifty-eight (22.6%) patients experienced symptom recurrence postoperatively. Recurrent symptoms were considered mild (decreased from preoperative severity) in 39 (15%) patients. Recurrent symptoms were considered severe, requiring revision decompression in 19 (7%) patients. Of these, 16 patients had MRI evidence of recurrent hindbrain crowding (Fig. 2a), while three demonstrated clinically and radiographically worsening syringomyelia. Thirty-nine (15%) patients with recurrent symptoms demonstrated adequate hindbrain decompression on MRI (Fig. 2b). Headache was 70% more likely to recur than cranial nerve and brainstem symptoms [relative risk (95%CI); 1.7 (1.01 – 3.34), p < 0.05; Fig. 1]. For the 19 (7%) patients undergoing revision decompression, nine had not received prior duraplasty, which was then performed at revision surgery. Of these, seven (78%) experienced resolution of their symptoms after duraplasty at revision surgery. The other ten patients undergoing revision decompression had duraplasty performed at primary surgery; however, thick extradural bands and multiple intradural adhesions were found and transected at revision surgery.
Axial T2-weighted MRI 6 months after hindbrain decompression in a a patient with severe recurrent symptoms that required revision decompression for the persistent hindbrain crowding demonstrated here versus b a patient with mild to moderate recurrent symptoms that demonstrated adequate hindbrain decompression and was not offered revision decompression
For the 69 patients with Chiari-associated syrinx, syringomyelia improved in 43 (62%) cases and remained stable in 23 (34%) cases. Three (4%) patients experienced clinical and radiographic worsening of syringomyelia requiring revision hindbrain decompression.
Predictors of treatment failure
In univariate analysis, patients with frontal headache, increasing duration of headache, with vertigo, and not undergoing duraplasty were at increased risk of symptom recurrence (Table 1). Age, degree of tonsilar herniation, headache alone, length of hospital stay, and presence of syringomyelia or scoliosis were not associated with increased symptom recurrence. In univariate analysis, severe tonsilar ectopia was the only variable associated with an increased incidence of revision decompression. Although the incidence of mild to moderate symptom recurrence was not increased with tonsilar ectopia caudal to C2 (p = 0.29, Table 1), the incidence of revision decompression was greater in patients with severe tonsilar herniation (caudal to C2) versus mild or moderate herniation (rostral to C2; revision decompression: 14% versus 6%).
In multivariate analysis, frontal headache [relative risk (95%CI); 1.55 (1.02–3.31), p = 0.050] and vertigo [relative risk (95%CI); 2.89 (1.12–6.79), p = 0.017] independently increased the odds of subsequent symptom recurrence 1.5- and 2.9-fold, respectively (Table 2). Each increasing year of preoperative headache duration was associated with a 15% increase in the likelihood of symptom recurrence (p = 0.019; Table 2). While non-duraplasty cases were associated with increased symptom recurrence in univariate analysis, non-duraplasty was not associated with symptom recurrence independent of specific symptomatology (vertigo, frontal headache) in multivariate analysis.
No preoperative variables were independently associated with an increased risk of revision decompression in multivariate analysis. While tonsilar ectopia caudal to C2 was associated with revision decompression in univariate analysis, it was not independently associated with treatment failure in multivariate analysis for this sample size.
Discussion
Analysis of our surgical experience with pediatric Chiari I malformation has shown that among patients undergoing hindbrain decompression for Chiari I malformation, a fifth of patients may experience mild to moderate symptom recurrence by 2 years after surgery. Similar to prior studies, our more classic definition of treatment failure (need for reoperation) was low (7%). Headache was most likely to recur postoperatively, almost twice as often as symptoms attributed to cranial nerve or brainstem compression. Furthermore, the risk of treatment failure was highest within the first 18 months, with a decreased risk beyond 18 months postoperatively. Patients experiencing continued symptom relief after 4 years of follow-up rarely experienced delayed symptom failure. However, only 15% of patients were followed up beyond 4 years, making definitive conclusions regarding late symptom recurrence difficult. Patients with longer durations of headache, with frontal headaches, or presenting with vertigo were subgroups most likely to experience recurrence after surgical treatment of Chiari I malformation.
The incidence of symptom recurrence observed in our study is similar to that previously reported [9, 11, 16, 19]. However, many prior studies have either focused primarily on improvement in symptoms, investigated only short-term treatment response, defined treatment failure as revision decompression, or have not accounted for symptom recurrence after initial treatment success [1, 3, 4, 6, 7, 10, 15–17, 19, 21]. Our experience shows that a subset of children will experience initial relief, which is followed by subsequent recurrence. Hence, it may be vital to outcome studies of Chiari I malformation to assess not absolute incidence of treatment response by revision surgery but rather long-term incidence of symptom recurrence to any degree as a function of time after surgery. Of particular interest was the fact that only one-third of patients with recurrent symptoms demonstrated a pathological explanation (recurrent hindbrain crowding or increased syrinx) on MRI. In fact, two-thirds of patients experiencing any degree of symptom recurrence demonstrated adequate hindbrain decompression on MRI. The former finding likely represents true surgical failure, while the latter finding may represent poor patient selection, highlighting the importance of precise surgical selection.
Headache, the most common symptom in our series, as well as in previously published series [1, 11, 16], was more likely to recur than symptoms attributed to hindbrain compression and cranial nerve dysfunction. This is likely a result of the more subjective nature of this symptom. The etiology of headache may also be multifactorial in patients with Chiari I malformation. Tonsilar ectopia may have been an incidental and non-contributory finding in this subgroup of headache patients experiencing treatment failure. Similarly, benign radiographic abnormalities such as nonspecific white matter abnormalities, arachnoid cysts, and venous angiomas are also incidentally found in up to 85% of patients with common migraines [14, 20]. The etiology of cranial nerve and brainstem symptoms may be a more specific and direct result of tonsilar ectopia given its decreased recurrence rate in our and other series [1]. In our practice, the vast majority of patients presenting with tonsilar ectopia and headache alone are not offered surgery. Only for cases where the headache is suboccipital in location, tussive, reproducible in clinic, and have failed prolonged conservative medical management will surgery be considered. The majority of patients presenting with headache alone will improve with conservative management, cannot be reproduced consistently, are frontal in location, and are never considered for surgery.
Patients with shunted hydrocephalus can also be a challenge. Because tonsilar ectopia may be a result of shunt malfunction and a cranial–spinal pressure gradient, shunt malfunction and slit ventricle syndrome must be ruled out prior to considering hindbrain decompression. In our series, all patients underwent radionucleotide shunt patency studies along with shunt tapping in order to document normal pressure and shunt flow. However, the presence of aspecific symptoms like headache may better correlated to the anomalous cranial growth microcrania and progressive thickening of the vault than hindbrain compression. In cases where shunt failure and slit ventricle syndrome have been ruled out, surgical procedures aiming at eliminating the pressure gradient across the foramen magnum, such as cranial expansion, may also lead to similar or even better symptomatic relief than posterior cranial fossa decompression by removing the cause rather than the effect of the condition. Nevertheless, the challenge for appropriate identification of secondary tonsilar ectopia versus true Chiari I malformation in order to guide the appropriate intervention remains.
Increased duration of preoperative headache was associated with an increased risk of treatment failure in our analysis. Dyste et al. similarly found that preoperative duration of symptoms greater than 2 years was associated with poor outcomes [7]. This effect may be due in part to the diversity of headache etiologies mentioned previously [20] or that a prolonged course of chronic pain may have detrimental psychological, behavioral, or pain tolerance effects that may subsequently predispose to postsurgical treatment failure [1]. Patient selection plays a large role in subsequent treatment failure rates. Offering surgery only to patients with tonsilar ectopia of 7 mm or more, with headaches that are exclusively suboccipital, tussive, and reproducible, may yield improved results for long-term headache control.
Vertigo in the Chiari population is often a result of pathology of the cerebellum and brainstem, respectively [18]. Though described as a common presenting complaint in patients with Chiari I malformations [13, 16], the specific responsiveness of these symptoms to surgical decompression have not been well studied. Severe, hindbrain crowding and compression has been postulated to disrupt cerebellar function, as well as peripheral and long-tracts of vestibular and cerebellar function. It is unclear why vertigo, which likely localizes to the hindbrain, was less responsive to surgery in our series. This may identify patients with more significant hindbrain crowding that may need more marked hindbrain decompression than was surgically implemented or the consequence of compressive pathology of these pathways may be less reversible. Regardless of etiology, our patients presenting with preoperative vertigo as a major symptom demonstrated a greater incidence of symptom recurrence.
The observed effect of duraplasty versus craniectomy alone on outcome is of particular interest. Directly comparing non-duraplasty versus duraplasty cases, revision surgery rate was higher in non-duraplasty cases. However, this association was lost when adjusting for other independent risk factors, suggesting that non-duraplasty patients had a higher failure rate due to their higher incidence of vertigo and long-standing and frontal headaches. Likewise, patients with severe tonsilar herniation caudal to the C2 lamina demonstrated an increased reoperation rate. However, there were many differences in baseline characteristics between the severe and mild–moderate herniation cohorts. Hence, adjusting for relevant difference in multivariate analysis resulted in a non-significant association with treatment failure, suggesting that either the model was underpowered with too few patients or that the increased failure rate of severe ectopia was an epiphenomenon resulting from differences in the patient population.
Patient age, syringomyelia, scoliosis, hydrocephalus, C2 laminectomy, or tonsilar coagulation was not associated with symptom recurrence or revision surgery in our practice experience. This was likely due to precise differentiation between shunt- and Chiari-related headaches, as well as the high incidence of syrinx improvement (62%) observed with hindbrain decompression alone. However, the retrospective nature of this study and non-standardized treatment paradigms (duraplasty, tonsil coagulation) make definitive conclusions on the efficacy of these treatment measures difficult. The observed associations of vertigo, frontal headache, and long-standing headache with symptom recurrence are likely applicable to surgeons with similar treatment algorithms but may be less applicable to those with varied practices. Future prospective prognostic studies are needed to validate these observations of our experience.
Conclusions
In reviewing our 10-year institutional experience, recurrence of mild symptomatology not severe enough to justify revision surgery may occur in nearly a fifth of patients after surgery, suggesting that reoperation alone may not be a sufficient outcome measure in future studies. Headache was more likely to recur than cranial nerve or brainstem dysfunction. Increasing duration of headache, frontal headache, and vertigo independently increased the likelihood of symptom recurrence after surgical decompression. These patients may represent a symptom etiology that is not localized to hindbrain compression or is less responsive to hindbrain decompression and may be appropriate for more prolonged conservative management. These observations may help contribute to patient education on postoperative expectations.
References
Alzate JC, Kothbauer KF, Jallo GI, Epstein FJ (2001) Treatment of Chiari I malformation in patients with and without syringomyelia: a consecutive series of 66 cases. Neurosurg Focus 11:E3
Bindal AK, Dunsker SB, Tew JM Jr (1995) Chiari I malformation: classification and management. Neurosurgery 37:1069–1074
Cahan LD, Bentson JR (1982) Considerations in the diagnosis and treatment of syringomyelia and the Chiari malformation. J Neurosurg 57:24–31
Caldarelli M, Novegno F, Vassimi L, Romani R, Tamburrini G, Di Rocco C (2007) The role of limited posterior fossa craniectomy in the surgical treatment of Chiari malformation Type I: experience with a pediatric series. J Neurosurg 106:187–195
Chiari H (1891) Uber Veranderungen des Kleinhirns infolge von Hydrocephalie des Grosshirns [in German]. Dtsch Med Wochenschr 17:1172–1175
Dones J, De Jesus O, Colen CB, Toledo MM, Delgado M (2003) Clinical outcomes in patients with Chiari I malformation: a review of 27 cases. Surg Neurol 60:142–147 discussion 147–148
Dyste GN, Menezes AH, VanGilder JC (1989) Symptomatic Chiari malformations. An analysis of presentation, management, and long-term outcome. J Neurosurg 71:159–168
Elster AD, Chen MY (1992) Chiari I malformations: clinical and radiologic reappraisal. Radiology 183:347–353
Fagan LH, Ferguson S, Yassari R, Frim DM (2006) The Chiari pseudotumor cerebri syndrome: symptom recurrence after decompressive surgery for Chiari malformation type I. Pediatr Neurosurg 42:14–19
Levy WJ, Mason L, Hahn JF (1983) Chiari malformation presenting in adults: a surgical experience in 127 cases. Neurosurgery 12:377–390
McGirt MJ, Nimjee SM, Fuchs HE, George TM (2006) Relationship of cine phase-contrast magnetic resonance imaging with outcome after decompression for Chiari I malformations. Neurosurgery 59:140–146 discussion 140–146
Meadows J, Kraut M, Guarnieri M, Haroun RI, Carson BS (2000) Asymptomatic Chiari Type I malformations identified on magnetic resonance imaging. J Neurosurg 92:920–926
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, Speer MC (1999) Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 44:1005–1017
Nevo Y, Kramer U, Rieder-Groswasser I, Harel S (1994) Clinical categorization of 312 children with chronic headache. Brain Develop 16:441–444
Park JK, Gleason PL, Madsen JR, Goumnerova LC, Scott RM (1997) Presentation and management of Chiari I malformation in children. Pediatr Neurosurg 26:190–196
Paul KS, Lye RH, Strang FA, Dutton J (1983) Arnold–Chiari malformation. Review of 71 cases. J Neurosurg 58:183–187
Pillay PK, Awad IA, Little JR, Hahn JF (1991) Symptomatic Chiari malformation in adults: a new classification based on magnetic resonance imaging with clinical and prognostic significance. Neurosurgery 28:639–645
Ropper AH, Adams RD, Victor M, Brown RH, Victor M (2005) Adams and Victor’s principles of neurology. McGraw-Hill Medical, New York
Saez RJ, Onofrio BM, Yanagihara T (1976) Experience with Arnold–Chiari malformation, 1960 to 1970. J Neurosurg 45:416–422
Schwedt TJ, Guo Y, Rothner AD (2006) “Benign” imaging abnormalities in children and adolescents with headache. Headache 46:387–398
Stevens JM, Serva WA, Kendall BE, Valentine AR, Ponsford JR (1993) Chiari malformation in adults: relation of morphological aspects to clinical features and operative outcome. J Neurol Neurosurg Psychiatry 56:1072–1077
Tubbs RS, McGirt MJ, Oakes WJ (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg 99:291–296
Weinberg JS, Freed DL, Sadock J, Handler M, Wisoff JH, Epstein FJ (1998) Headache and Chiari I malformation in the pediatric population. Pediatr Neurosurg 29:14–18
Acknowledgment
This work was supported by the American Syringomyelia Alliance Project, Monktin Institute Fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McGirt, M.J., Attenello, F.J., Atiba, A. et al. Symptom recurrence after suboccipital decompression for pediatric Chiari I malformation: analysis of 256 consecutive cases. Childs Nerv Syst 24, 1333–1339 (2008). https://doi.org/10.1007/s00381-008-0651-3
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0651-3