Abstract
Purpose
Endoscopic resection is a widely used technique for treatment of large colorectal adenomas, but few data are available including only lesions larger than ≥2 cm. The aim of this study is to evaluate the complication and recurrence rate after endoscopic resection of high-risk colorectal adenomas ≥3 cm in size.
Methods
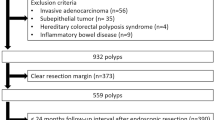
Retrospective analysis of a prospectively maintained database of patients undergoing polypectomy of large colorectal polyps of ≥3 cm.
Results
In 341 patients, 360 colorectal adenomas with a mean size of 3.9 cm were resected endoscopically. In 25 patients, a complication including 22 delayed bleedings (6.5 %) and three perforations (0.9 %) occurred. Single-variate analysis showed an increasing risk of complications for larger adenomas (3.9 vs. 4.6 cm; p ≤ 0.05). Two hundred twelve patients with 224 adenomas had undergone at least one documented follow-up endoscopy with a medium follow-up period of 16 months. In 95 resected lesions (42.4 %), a residual adenoma occurred in the first follow-up colonoscopy (n = 88, 92.6 %) or a recurrent adenoma occurred after at least one negative follow-up colonoscopy (n = 7, 7.4 %). In multivariate analysis, risk factors were lesion size, sessile growth pattern, and the performing endoscopist. The complication and recurrence rate correlated inversely between endoscopists.
Conclusions
The present study is the largest study showing complication and recurrence rates after colorectal polypectomy of advanced colorectal adenomas of ≥3 cm in size. Polyp size was identified as the most important risk factor for complications. For the first time, this study shows that the complication rate after colorectal polypectomy of large adenomas is correlated inversely with the residual and/or recurrence rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Colorectal cancer is a leading cause of cancer death in westernized societies, and for a long time, screening programs have been shown to reduce mortality from this disease [1]. Current strategies for reducing the toll from colorectal cancer focus on early detection and removal of potential precancerous lesions. Therefore, colonoscopy is currently regarded as the gold standard for the detection of polyps and cancers located in the colorectum and is the preferred method of screening for colorectal cancer in Europe and the USA. However, evidence shows that polyps and other lesions can be missed during colonoscopy due to several reasons. Nowadays, an adenoma detection rate of at least 20 % is required to reduce so-called post-colonoscopy cancers [2, 3]. Colonoscopy also allows removal of adenomatous polyps, the precursor of invasive carcinoma. In a recent study, it was shown that after a median of 7.7 years of follow-up, the mortality rate for colorectal cancer was lower among patients who had had low-risk adenomas removed but on the other hand moderately higher among those who had had high-risk adenomas (adenomas with high-grade dysplasia, a villous component, or a size ≥10 mm) removed, as compared to the general population [4]. This illustrates the need for a complete and save endoscopic resection, especially for large high-risk colorectal adenomas.
In general, the complication rate of endoscopic polypectomy is rather low but increases with the size of the polyp and in right-sided polyps [5–7]. Furthermore, recent studies show that with the increasing size of colorectal adenomas, there is a non-negligible, endoscopist-dependent number of residual neoplasia after endoscopic resection particularly of sessile adenomas [8].
Up to now, piecemeal endoscopic mucosal resection (EMR) is the widely used resection technique of large sessile adenomas (so-called lateral spreading adenomas) [7, 9] but shows a higher rate of recurrent adenomas compared to en bloc resection techniques such as colorectal endoscopic submucosal dissection (ESD). Recent studies have shown that local recurrence after EMR of non-pedunculated colorectal lesions occurs in 3 % of en bloc resections and in 20 % up to 55 % of piecemeal resections [10–14]. However, in daily clinical practice, recurrence is not a significant clinical problem following piecemeal EMR, as with strict colonoscopic surveillance, it can be managed endoscopically with high success rates [9, 15].
Most of the described studies concerning the complication and recurrence rate after the resection of large colorectal adenomas are dealing with adenomas ≥2 cm in size, and so far, only a few studies are available with even larger adenomas. Therefore, the purpose of the present study is to evaluate the complication and recurrence rate after endoscopic resection of high-risk colorectal adenomas of ≥3 cm in size and to define risk factors for complications as well as for residual and/or recurrent neoplasia.
Material and methods
Between January 2006 and March 2014, 4557 colorectal polypectomies in 3527 consecutive patients were performed in the Asklepios Hospital Barmbek, a tertiary endoscopic referral center. According to the underlying digital endoscopic database, 360 of these polyps in 341 patients were ≥3 cm in size and therefore fulfilled the inclusion criteria of this study. The following data were retrospectively recorded for each patient in whom an endoscopic resection of a polyp of ≥3 cm in size was performed: age, gender, polyp data (location, pedunculated or sessile, size of the polyp), polypectomy technique (en bloc EMR, piecemeal EMR, ESD), and histopathology data (type of polyp, grade of intraepithelial neoplasia, growth pattern, carcinoma, or other histology).
All participating endoscopists were experts who had previously performed more than 1000 polypectomies (W.C.; R.B.; U.W.; S.F.) or were senior endoscopy fellows who performed polypectomies under direct supervision of one of the experts. Polypectomies were carried out either on an inpatient or an outpatient basis, depending on the presumed risk factors in individual cases. From all of the patients, written informed consent was obtained. Before colonoscopy, split-dose bowel preparation was used. Colonoscopy and the endoscopic resection of the large polyps were performed under conscious sedation using propofol. Only endoscopes with high-definition television (HDTV) and narrow band imaging (NBI) function (Olympus 180 and 190 series; Olympus; Tokyo) for a better delineation of the neoplastic lesion were used.
The size of the polyps was estimated by the endoscopist before resection as was the location in the colorectum. Many patients were seen in referral after recently undergoing colonoscopy by another physician, with or without attempted polypectomy.
Lesions which were highly suggestive of submucosal invasion (e.g., lateral spreading adenoma non-granular type) were not attempted for polypectomy, EMR and/or ESD respectively, and consequently these lesions were biopsied. All other lesions were removed by conventional snare polypectomy (in case of pedunculated polyps) or EMR technique with normal saline used as the submucosal injection fluid in cases of sessile adenomas (see Fig. 1). Resection was performed predominantly with a 20-mm-sized spiral snare. Complete snare excision was the goal in each case. Only when complete snare resection was not possible, ablative techniques were used to treat residual adenoma, e.g., by argon plasma coagulation (at 20–40 W depending on lesion location). Radiofrequency and APC systems by Martin were used (MB1; Martin GmbH, Tuttlingen, Germany).
Example of a successful piecemeal EMR of an advanced colorectal adenoma. a Granular lesion (40 mm) of the sigmoid colon. b Elevation of the right-sided part of the lesion by submucosal injection. c The first part of the lesion was snared. d Visible submucosal layer after the first cut. e Continuing piecemeal EMR. f Successful EMR with entirely resected lesion
Excised tissue was completely retrieved for histological analysis. Histopathological evaluation was performed by one experienced pathologist (B.F.).
Immediate complications were recorded by the endoscopist. To assess later complications, information was taken from the patients’ charts and by retrospective telephone contact to all of the involved general practitioners and gastroenterologists.
Post-interventional bleeding was recorded as a complication when it required any form of intervention in the form of a repeated endoscopy, with or without hemostasis, hospital (re-)admission, blood transfusion, or surgery. The mode of endoscopic treatment and the further course of the patient were documented.
Intraprocedural bleeding during the primary endoscopic resection of the polyp was not recorded as bleeding.
Perforation was defined by the observation of an unequivocal macroscopic appearance of this complication during the endoscopic resection of the adenoma and by the post-interventional finding of free or retroperitoneal air and/or fluid on plain abdominal radiography, computed tomography, or abdominal ultrasound.
Patients with successful endoscopic resection of their large colorectal adenoma and without invasive cancer underwent endoscopic surveillance starting at 2–6 months after the initial resection. The polypectomy/EMR scar was examined with white light followed by NBI. In cases of doubt regarding the presence of residual adenoma, first biopsies were taken for histology, and then, the suspicious residual adenoma was treated. In contrast to residual adenomas, recurrent adenomas were defined as recurrent neoplasia after a documented first adenoma-free control colonoscopy.
Treatment of either residual or recurrent adenomas was performed in a non-standardized way by snare polypectomy, EMR, argon-plasma coagulation, or by hot biopsy forceps according to the size and location of the residual/recurrent adenoma and the endoscopists’ experience.
Statistical analysis
Data collection and statistical analysis were performed by means of descriptive statistics (mean and range) and analyzed with Microsoft Office Excel 2010 and IBM SPSS Statistics 22.
The two-sample t test was used to compare differences in means of continuous variables complemented by the Pearson’s x 2 test to compare distributions of categorical variables. Differences were considered to be significant if the two-sided p value was ≤0.05. The binary logistic regression analysis was used to identify independent predictors of outcomes.
Results
Between January 2006 and March 2014, a total of 360 colorectal endoscopic resections of colorectal high-risk adenomas of ≥3 cm in 341 patients were performed at Asklepios Hospital Barmbek. The mean age of the patients was 68.2 years (range 22–94 years) and includes 184 men (54.0 %) and 157 women (46.0 %).
Lesion characteristics and histology
The mean size of the resected polyps was 3.9 cm (range 3–12 cm). Three hundred one of the resected polyps (83.6 %) were sessile (e.g., lateral spreading adenomas) and 59 pedunculated (16.4 %). One hundred sixty-three polyps (45.3 %) were located in the right colon, 108 polyps (30.0 %) in the left colon, and 89 polyps (24.7 %) in the rectum. Three hundred nineteen out of the 360 polyps (88.6 %) were resected in piecemeal technique, whereas 35 polyps (9.7 %) could be resected en bloc. Only six resections (1.7 %) were performed as ESD. Three out of these six ESDs were completed in one piece, whereas the other three resections were completed as “piecemeal ESD.”
Two hundred ninety-eight (82.8 %) of the endoscopically resected polyps of ≥3 cm were classified as “classical” colorectal adenomas, 16 polyps (4.4 %) as sessile serrated adenomas (SSA), another 16 polyps (4.4 %) as mixed-type adenomas or traditional sessile adenomas (TSA), whereas 30 (8.3 %) polyps showed signs of an invasive tumor growth and were therefore classified as adenocarcinomas. Table 1 gives an overview of the patients and lesion characteristics.
Complications of endoscopic resections of colorectal adenomas ≥3 cm
In 316 out of 341 patients (91.8 %), an endoscopic resection of a colorectal adenoma ≥3 cm in size was performed without any adverse event. In 25 out of the 341 patients, a complication (perforation, bleeding) occurred. The overall complication rate therefore was 7.3 %. Delayed bleeding occurred in 22 patients (6.5 %) whereas a colorectal perforation occurred in 3 patients (0.9 %). In the 22 patients with a post-interventional hemorrhage, endoscopic re-intervention was necessary. For hemostasis in nine patients (40.9 %), endoscopic clipping of the bleeding site and in eight patients (36.4 %) injection therapy was preferred. In five patients (22.7 %), no further endoscopic therapy was indicated. In all of the patients, colorectal hemorrhage stopped after the endoscopic procedure. Only one of the three patients with colorectal perforation had to be operated, whereas the perforation site in the two other patients could be closed successfully by endoscopic clipping. Therefore, the need for surgical intervention due to bleeding or perforation after an endoscopic resection of a colorectal polyp of ≥3 cm in size is 0.3 % in total. The mortality was zero in the whole series.
In patients with complications, the mean size of the resected adenomas (4.6 cm) was significantly higher compared to those without complications (3.9 cm, p ≤ 0.05). Patients’ age, sessile or pedunculated tumor growth, localization of the lesion, endoscopic resection technique, and histology showed no significant differences between patients with and without complications in univariate analysis.
Between the two main endoscopists (endoscopist no. 1 and no. 2), a difference in the complication rate occurred. Whereas after endoscopic resection of an advanced adenoma by endoscopist no. 1, a complication occurred in only 4.4 %, the complication rate of endoscopist no. 2 is 11.0 %. However, this difference is not statistically significant (p = 0.089). Table 2 gives an overview of the different parameters and their consecutive complication rates.
Follow-up data
Two hundred twelve of the 341 patients (62.2 %) with an endoscopic resection of a high-risk colorectal adenoma ≥3 cm had at least one documented follow-up endoscopy during the reviewed period of 8.5 years with a medium follow-up period of 16 months (range 1–96 months). Initially, 224 adenomas were removed in these patients, and the mean number of follow-up endoscopies was 1.9 (±1.1).
During the follow-up period, 129 of the resected 224 high-risk adenomas (57.6 %) showed no recurrence of neoplastic tissue. In contrast, in 95 cases (42.4 %), a residual adenoma during the first follow-up examination (n = 88, 92.6 %) or a recurrent adenoma after at least one negative follow-up colonoscopy (n = 7, 7.4 %) occurred. One patient developed invasive cancer in a recurrent polyp. Two patients developed an interval carcinoma after 2 and 17 months, respectively. Both carcinomas were successfully resected surgically.
Treatment of residual and recurrent neoplasia
In 49 patients, the residual or recurrent adenoma was treated endoscopically by one (n = 35, 36.8 %) or by two or more (n = 14, 14.7 %) sessions. The mean number of required endoscopic sessions was 1.39 (±0.75). Only in ten of the patients (10.5 %) with residual or recurrent adenomas, surgical resection was necessary. In the other 36 patients, endoscopic re-examination is still pending (31.6 %) or patients dropped out (6.3 %). Figure 2 gives an overview of residual and recurrent adenomas as well as their treatment.
Diagram showing the detection of recurrences by number of follow-up classified in residual and recurrent adenomas (first section), the total recurrence rate (second section), and the treatment of recurrences differentiated by surgical and number of endoscopic re-treatments resulting in a mean number of endoscopic treatments to eradicate index lesion (third section). The right column is showing the total successful treatments verified by at least one negative follow-up after re-treatment (fourth section). Patients with re-examination still pending after a medium of one endoscopic re-treatment and dropouts are shown on top of the column
Risk factors for residual or recurrent neoplasia
In univariate analysis, residual and/or recurrent neoplasia is associated with a bigger size of the resected adenoma, a sessile growth pattern, and a location in the right-sided colon. In a multivariate approach, only the size of the polyp and a sessile growth pattern showed significant differences. The endoscopist has a major and significant impact in both univariate and multivariate analysis on the definite result of the endoscopic resection of large high-risk adenomas. Table 3 gives an overview of the risk factors for residual or recurrent neoplasia after the endoscopic resection of large colorectal adenomas ≥3 cm.
Correlation between endoscopist, complications, and residual and/or recurrent adenomas
In comparison with the abovementioned complication rate and the two main endoscopists, Table 4 shows that the endoscopist with the lower complication rate had significantly more residual or recurrent adenomas, and in contrast, the endoscopist with lesser residual and/or recurrent neoplasia had more complications. However, the endoscopist with the higher rate of residual and/or recurrent adenomas requires more endoscopic sessions (1.67 vs. 1.19, p ≤ 0.001) to achieve an equal rate of complete resections.
Discussion
Since many years, colonoscopy with polypectomy of all detected polyps was established in order to achieve an adenoma-free colon, and consequently, colonoscopy with polypectomy was regarded as an effective method to reduce the incidence of colorectal cancer [1]. However, worrisome data about so-called interval or post-colonoscopy cancers [2, 3, 16] and data about incomplete and recurrent adenomas after endoscopic resection of especially advanced colorectal adenomas [4, 9] demand attention especially for the endoscopic resection of large colorectal adenomas and their complication and recurrence rate.
The present study, which includes 360 advanced colorectal adenomas ≥3 cm in size in 341 patients, consists of 83.6 % of sessile, so-called lateral spreading adenomas. Of the resected adenomas, 89.4 % were resected in piecemeal EMR technique. Histologically, 8.3 % of the resected polyps were classified as adenocarcinoma which is within the range reported elsewhere [6, 7].
The major bleeding rate in the present study (7.3 %) appears to be relatively high. However, all of the polyps in this study were ≥3 cm. Regarding another study including a subgroup of polyps with more than 3 cm, authors reported about a bleeding rate of 25.8 % [5], and in another previous paper on large polyps, bleeding rate was given as 23.7 % [17]. More recent studies showed recurrent bleeding after polypectomy of colorectal adenomas with more than 2 cm in size in only 2.9 % respectively in 3.8 % [6, 18]. In accordance with existing literature, also our study shows that the complication/bleeding rate is correlated to the size of the resected lesion [5].
The perforation rate in our study (0.9 %) is rather low compared to other studies with a documented perforation rate of 1.1 % [5] and 1.6 % [6], respectively, after the resection of even smaller polyps.
With 0.3 %, the need for surgical intervention due to bleeding or perforation seems to be extremely low in our study. In an elder study, the need for surgical therapy was given as 0.8 % after endoscopic polypectomy of colorectal polyps of only 1.1 cm in average [5]. Also in a recent study, the need for surgical re-intervention due to complications was given as 0.8 % for colorectal adenomas of 3.5 cm in size [6].
In total, the residual and/or recurrence rate in our study was 42.4 %. However, most of the detected adenomas were residual adenomas (92.6 %) detected at the first follow-up endoscopy, whereas recurrent adenomas detected from the second follow-up endoscopy on occurred in only 7.4 %.
In accordance with our study also in the literature, large sessile colorectal adenomas (≥2 cm in size) resected piecemeal have an up to 55 % rate of residual adenoma at the first follow-up examination [14]. In other studies with lower residual (16 %) and late recurrence rates (4 %), independent predictors of recurrence after effective EMR were lesion size greater than 4 cm [6, 9]. In a recent meta-analysis, the mean recurrence risk after EMR was 15 % in general. Recurrence risk was significantly higher after piecemeal resection than after en bloc resection for lesions >2 cm (20 vs. 3 %) and <2 cm (22 vs. 3 %) [10]. In 15 of the included studies that differentiated between early and late recurrences, 88 % occurred early [10] which is also in line with our study.
Our recent data and the data from existing literature mentioned above show the particular necessity of an adequate first follow-up examination after piecemeal resection of large sessile colorectal adenomas in a 3–6-month period. In addition, a recent study from Seo et al. suggest that patients who are found to have advanced colorectal adenomas with two or more predictive factors (≥1 cm in diameter, and/or villous component, and/or high-grade dysplasia) at index colonoscopy are at higher risk for local recurrence, and follow-up colonoscopy should be performed even sooner [19].
To reduce local recurrence after piecemeal resection of large colorectal adenomas, ESD seems to be a better treatment option. In the last years, several comparative studies have shown the benefit of the ESD technique [11, 12, 20]. In another recent study, the size of the colorectal tumor, rate of en bloc resection, and curative resection were higher, and the rate of recurrence was lower in the ESD group versus the EMR group. However, in the ESD group, the procedure was longer and the rate of additional surgery and perforation was higher, suggesting that the indications for colorectal ESD should therefore be rigorously determined in order to avoid such problems [13]. For lateral spreading adenoma with a granular surface (granular-type LST), piecemeal EMR seems to be acceptable due to a low risk of submucosal cancerous invasion [6, 9, 21, 22]. On the other hand, it is well accepted that for lateral spreading adenomas non-granular type or mixed type, particularly those with diameters >2 cm, en bloc removal is preferable for sufficient histological evaluation [22].
Special attention should be drawn to the result that the different preferences in terms of technique lead to significant differences in the outcome of the performing endoscopists’ polypectomies. One endoscopist resecting greater adenomas has a significantly lower recurrence rate (29.1 vs. 54.1 %) but a doubled complication rate (9.3 vs. 4.5 %) compared to another endoscopist who needs significantly more endoscopic sessions (1.67 vs. 1.19) to achieve the equal rate of complete resections. The fact that different endoscopists have different rates of complete resection is well known in the literature [8], but for the first time, this study highlights that the rate of adenoma recurrence is inversely correlated with the complication rate. This can be explained by the hypothesis that with a “more aggressive” endoscopic technique during the first session, the recurrence rate will be lower accompanied by an increased number of complications. This higher complication rate (mainly bleeding complications) needs more additional colonoscopies in order to achieve post-interventional hemostasis. On the other hand with a “less aggressive” technique during the initial therapeutic colonoscopy, also additional colonoscopies with difficult, scar-conditioned re-treatment of remaining adenomas are necessary to achieve the same rate of complete resections. Therefore, it remains unclear which is the superior strategy.
The main limitations of our study are the retrospective design of the study performed in one single endoscopy center only and the lack of routine biopsies to exclude residual and/or recurrent neoplasia histologically. Another limitation is that we do not have complete follow-up data of all of the resected cases, yet. We will continue to follow up on our patients in order to achieve complete follow-up. Another limitation is the potential for bias inherent in all cohort studies; however, this is limited by the absence of exclusion criteria in this and other comparable studies [9].
In summary, with 341 patients, the present study is—to our knowledge—the largest study showing complication as well as recurrence rates after colorectal polypectomy of advanced colorectal adenomas of ≥3 cm in size. As in previous studies, polyp size was identified as the most important risk factor for complications. The recurrence rate after piecemeal resection of particularly large lateral spreading adenomas is high. However, these residual and/or recurrent adenomas can be managed endoscopically with high success rates. For the first time, this study shows that the complication rate after colorectal polypectomy of large adenomas is correlated inversely with the residual and/or recurrence rate. As shown for other indications, especially in abdominal surgery, the impact of the examiners’ experience on the quality of outcome in colorectal polypectomy becomes also evident in the present study. In contrast to the study from Masci et al. [23], we therefore recommend that endoscopic resection of large colorectal adenomas should only be performed in high-volume centers.
References
Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD et al (1997) Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 112:594–642
Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U et al (2010) Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 362:1795–1803
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK et al (2014) Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 370:1298–1306
Løberg M, Kalager M, Holme Ø, Hoff G, Adami HO, Bretthauer M (2014) Long-term colorectal-cancer mortality after adenoma removal. N Engl J Med 371:799–807
Heldwein W, Dollhopf M, Rösch T, Meining A, Schmidtsdorff G, Hasford J, Hermanek P, Burlefinger R, Birkner B, Schmitt W (2005) Munich Gastroenterology Group. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy 37(11):1116–1122
Moss A, Bourke MJ, Williams SJ, Hourigan LF, Brown G, Tam W, Singh R, Zanati S, Chen RY, Byth K (2014) Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 140(7):1909–1918
Maguire LH, Shellito PC (2014) Endoscopic piecemeal resection of large colorectal polyps with long-term follow up. Surg Endosc 28(9):2641–2648
Pohl H, Srivastava A, Bensen SP, Anderson P, Rothstein RI, Gordon SR, Levy LC, Toor A, Mackenzie TA, Rosch T, Robertson DJ (2013) Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology 144(1):74–80
Moss A, Williams SJ, Hourigan LF, Brown G, Tam W, Singh R, Zanati S, Burgess NG, Sonson R, Byth K, Bourke MJ (2015) Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut 64(1):57–65
Belderbos TDG, Leenders M, Moons LMG, Siersema PD (2014) Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy 46:388–400
Wang J, Zhang XH, Ge J, Yang CM, Liu JY, Zhao SL (2014) Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal tumors: a meta-analysis. World J Gastroenterol 20(25):8282–8287
Oka S, Tanaka S, Saito Y, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisabe T, Tsuruta O, Sano Y, Yamano H, Shimizu S, Yahagi N, Watanabe T, Nakamura H, Fujii T, Ishikawa H, Sugihara K (2015) Colorectal Endoscopic Resection Standardization Implementation Working Group of the Japanese Society for Cancer of the Colon and Rectum, Tokyo, Japan. Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110(5):697–707
Fujiya M, Tanaka K, Dokoshi T, Tominaga M, Ueno N, Inaba Y, Ito T, Moriichi K, Kohgo Y (2015) Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc 81(3):583–595
Khashab M, Eid E, Rusche M, Rex DK (2009) Incidence and predictors of “late” recurrences after endoscopic piecemeal resection of large sessile adenomas. Gastrointest Endosc 70(2):344–349
Knabe M, Pohl J, Gerges C, Ell C, Neuhaus H, Schumacher B (2014) Standardized long-term follow-up after endoscopic resection of large, nonpedunculated colorectal lesions: a prospective two-center study. Am J Gastroenterol 109(2):183–189
Samadder NJ, Curtin K, Tuohy TM, Pappas L, Boucher K, Provenzale D, Rowe KG, Mineau GP, Smith K, Pimentel R, Kirchhoff AC, Burt RW (2014) Characteristics of missed or interval colorectal cancer and patient survival: a population-based study. Gastroenterology 146(4):950–960
Binmoeller KF, Bohnhacker S, Seifert H et al (1996) Endoscopic snare excision of “giant” colorectal polyps. Gastrointest Endosc 43:183–188
Wu XR, Church JM, Jarrar A, Liang J, Kalady MF (2013) Risk factors for delayed postpolypectomy bleeding: how to minimize your patients’ risk. Int J Color Dis 28(8):1127–1134
Seo JY, Chun J, Lee C, Hong KS, Im JP et al (2015) Novel risk stratification for recurrence after endoscopic resection of advanced colorectal adenoma. Gastrointest Endosc 81:655–664
Saito Y, Fukuzawa M, Matsuda T, Fukunaga S, Sakamoto T, Uraoka T et al (2010) Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 24(2):343–352
Belle S, Haase L, Pilz LR, Post S, Ebert M, Kaehler G (2014) Recurrence after endoscopic mucosal resection-therapy failure? Int J Color Dis 29(2):209–215
Imai K, Hotta K, Yamaguchi Y, Tanaka M, Kakushima N, Takizawa K, Matsubayashi H, Kawata N, Igarashi K, Sugimoto S, Yoshida M, Oishi T, Mori K, Ono H (2014) Should laterally spreading tumors granular type be resected en bloc in endoscopic resections? Surg Endosc 28(7):2167–2173
Masci E, Viale E, Notaristefano C, Mangiavillano B, Fiori G, Crosta C, Dinelli M, Maino M, Viaggi P, Della Giustina F, Teruzzi V, Grasso G, Manes G, Zambelli S, Testoni PA (2013) Endoscopic mucosal resection in high- and low-volume centers: a prospective multicentric study. Surg Endosc 27(10):3799–3805
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Seidel and E. Färber contributed equally to this work.
Rights and permissions
About this article
Cite this article
Seidel, J., Färber, E., Baumbach, R. et al. Complication and local recurrence rate after endoscopic resection of large high-risk colorectal adenomas of ≥3 cm in size. Int J Colorectal Dis 31, 603–611 (2016). https://doi.org/10.1007/s00384-015-2498-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2498-x