Abstract
Background
Colonoscopic removal of large colorectal polyps is challenging and requires advanced endoscopic technique. Successful endoscopic management not only avoids the morbidity of surgery but also risks perforation, hemorrhage, and recurrence.
Methods
This study is a retrospective review of a prospectively maintained database of all patients undergoing cautery snare piecemeal polypectomy for large colorectal polyps by a single operator over 20 years with long-term followup.
Results
231 patients underwent 269 piecemeal polypectomies over a 20 year period. The complication rate was 4.3 %. Malignancy was identified in 25 (10.8 %) of patients. Local recurrences occurred in 24 % of patients with benign adenomas. The vast majority of these were managed with repeat endoscopy. Overall, benign large polyps were managed successfully endoscopically in 94.4 % of patients.
Conclusions
Piecemeal polypectomy is effective and safe for the management of large colorectal polyps. With long-term followup, the recurrence rate is appreciable, but most recurrences can be successfully managed with further endoscopic intervention. More complex techniques such as endoscopic submucosal dissection are usually unnecessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colonoscopic removal of large (greater than 3 cm) colorectal polyps can be a challenge to the endoscopist in both judgment and technique. When possible, endoscopic removal spares the patient the morbidity of surgery. On the other hand, colonoscopic removal of a large polyp risks perforation, hemorrhage, recurrent disease, and possible incomplete resection of malignancy.
In this report, we present a large series of 231 patients who underwent 269 cautery snare piecemeal polypectomies performed by a single endoscopist (PCS) over 20 years. More complex methods such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) were not used. Most patients had multiple subsequent endoscopies, allowing for long-term followup to assess the risk of complications, recurrence, and malignancy. The objective was to define the complication and long-term recurrence rates for colon polyps treated with colonoscopic piecemeal resection with a cautery snare.
Materials and methods
This study was a retrospective review (from a prospectively maintained database) of all patients between 1987 and 2008 who underwent colonoscopic piecemeal polypectomy by a single endoscopist (PCS). The begin date of 1987 was selected because the endoscopist was well past the learning curve for removing large polyps by then, and the end date of 2008 was selected so that all patients would have at least 5 years followup.
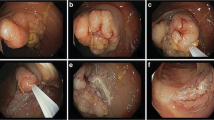
All the polyps were sessile and required piecemeal excision in the clinical judgment of the endoscopist. The decision to attempt piecemeal polypectomy (instead of segmental colectomy or transanal local excision) was based not only on the size of the lesion, but also on the location. For example, a polyp located just proximal to a fold or a flexure can be more difficult to remove, as can a polyp located more proximally in the colon. If there was a gross appearance suggestive of malignancy (induration, ulceration), then polypectomy was not attempted.
The size of the polyps was estimated by the endoscopist before resection as was the location in the colorectum (the rectum was considered to be up to 15 cm from the anal verge). Many patients were seen in referral after recently undergoing colonoscopy by another physician, with or without attempted polypectomy. If any partial polypectomy had been done by a previous endoscopist, then the size recorded was that when the patient was first seen by us.
Polypectomy was performed with multiple passes of the endoscopic cautery snare (often using a jumbo snare) always with the goal of a grossly complete resection (Fig. 1). Other techniques such as argon beam fulguration, submucosal saline injection, and endoscopic ultrasound were not used. An endoscope holding device [1] was very helpful, however.
After polypectomy, the site was marked with an India ink tattoo, unless the location would otherwise be easily identified on followup colonoscopy (such as the cecum or the low rectum). After initial polypectomy, the followup regimen was repeat colonoscopy in 3 months. If no recurrence was seen at 3 months, then colonoscopy was repeated at 1 year. If there was still no local recurrence, then standard followup colonoscopy every 3–5 years was recommended. This was in accordance with numerous published guidelines [2–4].
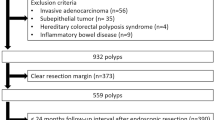
For this study, the patients’ medical records were reviewed for complications, recurrences, and the appearance of invasive cancer. Patients with hereditary colonic polyposis or frank cancer (indurated and/or ulcerated lesions) at initial polypectomy were excluded, as were patients undergoing simple polypectomy (not piecemeal resection) or biopsy alone. Patients who underwent attempted but incomplete piecemeal polypectomy were included.
Following the index colonoscopy and polypectomy, all followup colonoscopy, surgery, and pathology data were recorded. Statistical analysis was performed using SAS Enterprise Guide version 9.2 software. Continuous variables were compared with a Mann–Whitney test and categorical variables with Fischer’s exact test. This study was approved by the Partners Human Research Committee.
Results
Between 1987 and 2008, 231 patients underwent piecemeal polypectomy. The patients were primarily older males. There were 138 males (60 %) and 93 females (40 %), and the average age was 67.8 years (range 20–90 years). The most common indication for the index colonoscopy was a history of colon polyps (Table 1). A total of 269 polyps were removed piecemeal from the 231 patients. 27 patients had more than one piecemeal polypectomy done at different locations within the colon; some were synchronous and some metachronous. Of the 269 polypectomies, 248 (92.2 %) were considered grossly complete.
The polyps were located throughout the colon, but were found with highest frequency (38.3 %) in the rectum (Table 2). The most common histology was tubulovillous (31.2 %). Polyp histology varied from colon to rectum; colonic polyps were more likely to be tubular or hyperplastic than rectal polyps, which demonstrated more villous, tubulovillous, and carcinomatous histologies (Table 2). Among adenomatous polyps, rectal location was significantly negatively correlated with tubular histology (OR 0.143, 95 % CI 0.07–0.30, p < 0.0001), suggesting that more dysplastic polyps were more common distally. During the index colonoscopy, 376 smaller polyps were also removed. An average of 2.5 (range 1–15) smaller synchronous polyps were removed from 148 (64 %) of patients undergoing piecemeal polypectomy. The polyp histology is shown in Table 3. Compared to the synchronous small polyps, those requiring piecemeal polypectomy were more frequently malignant, villous, tubulovillous, or serrated in histology, and less likely to be tubular or hyperplastic.
Unless the pathology report showed invasive cancer, all patients were advised to return for followup colonoscopy after healing of the first polypectomy defect (usually at 3 months). For the 21 grossly incomplete polyp removals, completion polypectomy was attempted at that time.
At index colonoscopy, 10 patients (4.3 %) suffered complications. Typically, patients who had unusual hemochezia or abdominal pain after colonoscopy were admitted for observation. Seven (3.0 %) suffered appreciable bleeding requiring inpatient admission for observation, with two patients requiring blood transfusion. No patient underwent repeat colonoscopy for bleeding. Three (1.3 %) were admitted for antibiotics and observation because of suspected microperforation. No patient required surgery for perforation or any other reason. Patients suffering complications had on average slightly larger polyps than patients without complications (3.1 cm vs. 2.8 cm), but this difference was not significant (p = 0.57). Complication rates were highest in the sigmoid colon (n = 2, 10.0 %), and lowest in the rectum (n = 3, 2.9 %) and transverse colon (0). Complication rates were intermediate in the cecum (n = 2, 6.8 %), ascending (n = 2, 3.8 %), and descending colon (n = 1, 7.1 %). These differences were not statistically significant (p = 0.22).
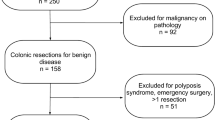
Following polypectomy, patients underwent surgery were followed with endoscopy, or were lost to followup (Fig. 2). 42 patients (18.2 %) were lost to follow up. Twenty-five patients (10.8 %) were found to have invasive cancer and are further discussed below. Four patients (1.7 %) with benign polyps underwent surgery including the polypectomy site because of diverticular disease or synchronous cancer. The remaining 160 patients (69 %) were followed endoscopically, with the first followup colonoscopy at 3 months for most patients. These patients were followed for a mean of 4.5 years (SD 3.6, range 0.25–18.9) with 3.0 followup colonoscopies (SD 1.8, range 1–9) per patient.
Of the 160 patients followed endoscopically, 122 patients (76 %) were effectively treated by their first polypectomy and the large polyp never recurred. Nevertheless, 38 (24 %) patients had 39 locally recurrent polyps; all but five of these (87.2 %) had been considered to have been completely resected at the time of their first polypectomy. Most recurrences (25 patients, 66 %) were noted on the first followup colonoscopy, 3–6 months after the initial resection. The mean time to recurrence was 1.1 years with recurrences noted as late as 4.5 years after index polypectomy. Interestingly, six patients with recurrent polyps had carcinoma-in situ on initial pathology, but none of these patients was found to have invasive cancer or carcinoma-in situ in their recurrent polyps. Univariate regression identified size, rectal location, and carcinoma-in situ as potential predictors of recurrence (Table 4). Sex, age, total number of polyps resected, and other histologies were not associated with recurrence. On multivariate analysis, polyp size was the only significant predictor of polyp recurrence (OR 2.08, 95 % CI 1.42–3.04, p = 0.0002).
Of the 38 patients with local recurrence of their large polyp, only four (10.5 %) were found to have endoscopically unresectable recurrent polyps at this second colonoscopy. Three of these four patients underwent surgical resection, and the final pathology was benign in all cases. One patient was recommended to have surgery for an unresectable adenoma, but declined further intervention. The remaining 34 patients (90 %) underwent repeat endoscopic removal. Five patients (15 %) were lost to follow up after their second polypectomy. The remaining 29 (85 %) were followed for a mean of 5.2 years (SD 3.0, range 0.5–11) with a mean of 3.4 endoscopies (SD 1.8, range 1–7). Eight patients (28 % of these 29 patients) suffered a second local recurrence and were successfully managed endoscopically, with three patients (10 % of the 29 patients) requiring three polypectomies each to achieve permanent eradication. In total, 156 patients (97.5 %) who were followed with at least two colonoscopies were successfully managed endoscopically. 151 patients (94.4 %) who were never lost to followup were successfully managed endoscopically. These recurrences were all adenomas; no patient developed invasive cancer or carcinoma-in situ in a recurrent polyp.
Twenty-five patients (10.3 %) were found to have invasive cancer in the polyp at index colonoscopy. These patients had larger polyps than patients without cancer (3.4 cm vs. 2.8 cm (p = 0.006)). No invasive cancers were found in the cecum or the ascending colon, and the rate of cancer increased distally. Polyp size, male sex, and rectal location were identified as potential predictors of malignancy on univariate analysis (Table 5). Patient age and total number of polyps were not significant predictors of malignancy. On multivariate analysis, male sex and rectal location remained significant predictors of malignancy; size was non-significant (Table 5).
Twenty-one patients (84 % of patients with invasive cancer) underwent surgery for their cancers. Three (12 %) elderly patients with multiple comorbidities elected not to have surgery. One patient, described as having a microscopic focus of invasive cancer, was followed with serial endoscopies and was free of disease at endoscopic followup 3 years after her index colonoscopy.
Twelve patients (48 % of patients with invasive cancer) with their cancers located in the rectum underwent transanal full thickness excision in the operating room. Of these 7 had no residual tumor and 2 had a pT1 tumor. These patients were followed for a mean of 8.7 years (range 3.8–19) with 3.8 endoscopies (range 2–7) and were free from recurrence. The remaining three underwent neoadjuvant therapy and abdominoperineal resection (APR). One patient each was found to have T2N0, T2N2, and T3N1 disease. Three patients underwent APR after the index polypectomy without interval transanal excision. The other six patients (24 % of patients with invasive cancer) with more proximal tumors underwent segmental colectomy; all were node negative. Tumor stages at the time of initial surgery are shown in Table 6.
Of the 21 cancer patients who underwent surgery, eleven (52 %) had no residual carcinoma in their specimen, including one patient who underwent APR. Of these 21 patients, 15 were initially thought to have undergone complete polypectomy. Of these, 5 (33 %) had residual carcinoma in their surgical specimens. One patient had residual adenoma without carcinoma. Patients who had residual cancer in their specimens tended to have larger polyps, (3.56 cm vs. 3.09 cm), but this difference was not statistically significant (p = 0.5).
Discussion
In this study, we present a large report of 231 patients who underwent 269 piecemeal polypectomies by a single endoscopist over 20 years. Since this was a single operator study, there was uniform technique and management. Also, most patients had long followup, with multiple repeat examinations. This long-term followup is unique among studies of colonic polypectomy.
The complication rate was low. Piecemeal polypectomy of a large polyp would be expected to have a higher complication rate than simple polypectomy of smaller polyps. In this study, 4.3 % of patients experienced complications, which is at the low end of the 2.4–25 % range reported by others for large polyp removal [5–12]. No complications required surgery and there was no mortality. Large polyp size and location in the right colon were factors that previously have been shown to predict complications post-polypectomy [13]; these associations were not seen in this study, however.
Predictably, large polyps requiring piecemeal resection were more likely to be malignant than those amenable to simple polypectomy. Furthermore, large adenoma size has been shown to be associated with important mutations in the adenoma–carcinoma sequence, such as p53 overexpression and K-ras mutation [14]. The rate of invasive cancer in our study, 10.3 %, was within the 9–44 % range reported elsewhere [5–12, 15, 16]. In particular, it was comparable to the 7–31 % range of invasive cancer associated with studies of ESD and EMR [17–19]. Thus, our data suggest (especially given the long followup) that the diagnosis of invasive cancer was not compromised by a lack of en-bloc polyp removal. On multivariate analysis, rectal location and male sex were significant predictors of malignancy, attenuating the effect of polyp size. However, it must be remembered that only larger polyps requiring piecemeal polypectomy were included in the analysis.
Prior studies of large polyps have reported a 0 % rate of residual cancer in surgical specimens after endoscopic resection of malignant polyps [11]. In our study, however, half the patients with initial malignant polyps had residual cancer found at surgery, and two patients had lymph node positive cancer, similar to a previous report from our institution [12]. Although most of these patients were recognized to have an incomplete polypectomy, even among the patients who had a grossly complete polypectomy, one-third had residual carcinoma at the time of surgery. A positive or indeterminate margin at polypectomy has been shown to predict residual cancer at colectomy, and lymphovascular invasion on histology has demonstrated an association with positive nodal status [20]. The pathology reports in our study did not report these features consistently enough to make reliable comparisons about this, however.
Local recurrence occurred in a substantial minority of our patients (23 %) after piecemeal polypectomy. This was similar to the 14–28 % rate reported by others [12–16, 21, 22]. Most of these recurrences (89.5 %) were managed endoscopically, and no patient developed a malignancy in a recurrent polyp. Carcinoma in situ was not a contraindication to endoscopic treatment. Overall, 94.4 % of patients with benign polyps were not lost to followup and were successfully managed endoscopically. Again, this long-term outcome compared very favorably with EMR and ESD [23].
As a matter of personal preference (and in the interest of maintaining a consistent technique for long-term evaluation), simple cautery snare piecemeal polypectomy was carried out in these patients, without submucosal fluid injection, and without ESD with a needle tip cautery. Although excellent short-term results have been reported with these techniques [17–19, 24], they add more time, cost, and technical complexity to the procedure (especially ESD). Furthermore, submucosal fluid injection can sometimes make the polypectomy more challenging, by enlarging the overlying sessile polyp, and by creating a mucosal bulge behind which it can be difficult to see. The favorable complication and long-term recurrence rates seen in this study suggest that ESD and EMR are in fact not often necessary. Furthermore, since few previous studies have reported long-term followup data, recurrence rates after ESD and EMR of large adenomas could be falsely low.
When possible, colonoscopic piecemeal polypectomy of course has many advantages compared to surgery. For large colon polyps, it is preferable to segmental colectomy (even with laparoscopy) because it avoids general anesthesia, hospitalization, and intra-abdominal surgery. For rectal polyps, piecemeal polypectomy is preferable to traditional transanal excision (done through an open operating anoscope) because the insufflation and magnification associated with colonoscopy allow a technically more precise excision. Transanal endoscopic microsurgery has similar advantages, but at the cost of a longer procedure, general anesthesia, and possible inpatient hospitalization.
In summary, this study demonstrated that a consistent and relatively simple cautery snare piecemeal polypectomy technique with careful followup produced excellent long-term results. With long-term followup, large sessile benign colorectal polyps were effectively eradicated in the majority of patients, even if carcinoma-in situ was present. Almost all recurrent polyps could be effectively managed endoscopically, and the rate of recurrent polyps undergoing malignant degeneration was low. More complex techniques such as ESD and EMR are usually unnecessary. In patients found to have invasive cancer, a significant minority of patients will have residual disease at surgery despite grossly complete endoscopic resection.
References
Chester JF, Shellito PC (1988) A support brace for the endoscope. Dis Colon Rectum 31:409–411
Winawer SJ, Zauber AG, O’Brien MJ et al (1993) Randomized comparison of surveillance intervals after colonoscopic removal of newly diagnosed adenomatous polyps. N Engl J Med 328:901–906
Patient Care Committee of the Society of Surgery of the Alimentary Tract (1999) Management of colonic polyps and adenomas. J Gastrointest Surg 3:220–222.
Eisen GM, Chutkan R, Goldstein JL et al (2000) Guidelines for colorectal cancer screening and surveillance. Gastrointest Endosc 51:777–782
Bardan E, Bat L, Melzer E, Shemesh E, Bar-Meir S (1997) Colonoscopic resection of large colonic polyps—a prospective study. Isr J Med Sci 33(12):777–780
Kao KT, Giap AQ, Abbas MA (2011) Endoscopic excision of large colorectal polyps as a viable alternative to surgical resection. Arch Surg 146(6):690
Dell’Abate P, Iosca A, Galimberti A, Piccolo P, Soliani P, Foggi E (2001) Endoscopic treatment of colorectal benign-appearing lesions 3 cm or larger: techniques and outcome. Dis Colon Rectum 44(1):112–118
Boix J, Lorenzo-Zúñiga V, Moreno de Vega V et al (2007) Endoscopic removal of large sessile colorectal adenomas: is it safe and effective? Dig Dis Sci 52(3):840–844
Binmoeller KF, Bohnacker S, Seifert H, Thonke F, Valdeyar H, Soehendra N (1996) Endoscopic snare excision of “giant” colorectal polyps. Gastrointest Endosc 43(3):183–188
Stergiou N, Riphaus A, Lange P, Menke D, Köckerling F, Wehrmann T (2003) Endoscopic snare resection of large colonic polyps: how far can we go? Int J Colorectal Dis 18(2):131–135
Doniec JM, Löhnert MS, Schniewind B, Bokelmann F, Kremer B, Grimm H (2003) Endoscopic removal of large colorectal polyps: prevention of unnecessary surgery? Dis Colon Rectum 46(3):340–348
Walsh RM, Ackroyd FW, Shellito PC (1992) Endoscopic resection of large sessile colorectal polyps. Gastrointest Endosc 38(3):303–309
Buddingh KT, Herngreen T, Haringsma J et al (2011) Location in the right hemi-colon is an independent risk factor for delayed post-polypectomy hemorrhage: a multi-center case-control study. Am J Gastroenterol 106(6):1119–1124
Einspahr JG, Martinez ME, Jiang R et al (2006) Associations of Ki-ras proto-oncogene mutation and p53 gene overexpression in sporadic colorectal adenomas with demographic and clinicopathologic characteristics. Cancer Epidemiol Biomarkers Prev 15(8):1443–1450
Seitz U, Bohnacker S, Seewald S, Thonke F, Soehendra N (2003) Long-term results of endoscopic removal of large colorectal adenomas. Endoscopy 35(8):S41–S44
Regula J, Wronska E, Polkowski M et al (2003) Argon plasma coagulation after piecemeal polypectomy of sessile colorectal adenomas: long-term followup study. Endoscopy 35(3):212–218
Moss A, Bourke MJ, Williams SJ et al (2011) Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 140:1909–1918
Byeon JS, Yang DH, Kim KJ et al (2011) Endoscopic submucosal dissection with or without snaring for colorectal neoplasms. Gastrointest Endosc 74:1075–1083
Saito Y, Uraoka T, Yamaguchi Y et al (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosa dissections (with video). Gastointest Endosc 72:1217–1225
Butte JM, Tang P, Gonen M et al (2012) Rate of residual disease after complete endoscopic resection of malignant colonic polyp. Dis Colon Rectum 55(2):122–127
Khashab M, Eid E, Rusche M, Rex DK (2009) Incidence and predictors of “late” recurrences after endoscopic piecemeal resection of large sessile adenomas. Gastrointest Endosc 70(2):344–349
Bedogni G, Bertoni G, Ricci E et al (1986) Colonoscopic excision of large and giant colorectal polyps. Technical implications and results over eight years. Dis Colon Rectum 29(12):831–835
Lee EJ, Lee JB, Lee SH et al (2012) Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. Surg Endosc 26:2220–2230
Tanaka S, Terasaki M, Hayashi N et al (2013) Warning for unprincipled colorectal endoscopic submucosal dissection: accurate diagnosis and reasonable treatment strategy. Dig Endosc 25:107–116
Disclosures
Drs. Maguire and Shellito have nothing to disclose.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maguire, L.H., Shellito, P.C. Endoscopic piecemeal resection of large colorectal polyps with long-term followup. Surg Endosc 28, 2641–2648 (2014). https://doi.org/10.1007/s00464-014-3516-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3516-8