Abstract
Background
The number of studies suggesting that en bloc resection of bladder tumor (ERBT) is superior to transurethral resection of bladder tumor (TURBT) for non-muscle-invasive bladder cancer (NMIBC) management is growing. The aim of this review is to discuss the features of these procedures and to determine the prospects of en bloc in NMIBC management.
Materials and methods
We conducted a literature search using two databases (Medline and Scopus) and included any research which reported ERBT outcomes.
Results
The lasers with minimal tissue penetration depth are becoming the main tool for ERBT. Unfortunately, most of the systematic reviews continue to be characterized by high heterogeneity. However, recent studies indicate that ERBT may have the edge when it comes to the detrusor muscle rate and the quality of the histological specimen. ERBT may favor in terms of in-field relapse, but its rate in the studies varies greatly. As for out-field relapse-free survival, the data are still lacking. The strongest evidence supports that ERBT is superior to TURBT in complications rate (bladder perforation). ERBT is feasible irrespective to tumor size and location.
Conclusions
ERBT has gained in momentum with the increasingly widespread use of this kind of laser surgery. The introduction of novel sources (TFL and Thulium:YAG pulsed laser) will definitely affect how the field develops and will result in further improvements in safety and precision. The latest trials make us more certain in our belief that ERBT will be beneficial in terms of histological specimen quality, relapse rate and complications rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transurethral resection of bladder tumor (TURBT) is an endoscopic approach that has been around now for more than a century [1, 2]. For some period of time, it has been recognized as the only standard surgery for the management of non-muscle-invasive bladder cancer (NMIBC). The alternative technique namely en bloc resection of bladder tumor (ERBT) was introduced in 1997 by Kawada et al. who performed en bloc resection of a papillary, sessile bladder tumor using monopolar arched electrode for the first time [3]. After introduction in monopolar technique, ERBT was reproduced using Holmium: YAG laser by Das et al. [4]. However, the technique did not gain momentum. In 2011, a group of authors led by Prof. Herrmann revisited en bloc technique by introducing Thulium: YAG assisted anatomical en bloc resection of bladder tumors [5]. They reported an initial series of 6 ERBT. All of the resected specimens contributed detrusor muscle, and no complications were observed. Since then, a variety of studies aimed to assess this method including oncological and safety outcomes and to compare it with conventional TURBT.
Nowadays, EBRT is an evolving alternative to standard and conventional TURBT. The European Association of Urology (EAU) recommends performing both techniques for non-muscle-invasive bladder tumors (strength rating: strong) [6]. However, several studies show that en bloc enjoys a number of essential advantages over standard TURBT, including a higher muscle detection rate, better quality of pathology specimen, a lower complication rate and a higher recurrence-free survival [7]. The other data showed that TURBT is not inferior to ERBT where muscle layer detection rate and recurrence risk are concerned [8].
Thus, it is still somewhat inconclusive and controversial as to whether the en bloc technique is superior to TURBT. There remains a number of aspects that should be discussed such as oncological outcomes, intraoperative complications, the learning curve, etc. In this narrative review, we would like to raise these relevant issues, shed more light on the pros and cons of en bloc and determine more precisely what might be its future role in NMIBC management.
Materials and methods
We conducted a literature search using two databases (Medline and Scopus) with the following search query: (bladder cancer[MeSH Terms] OR NMIBC) AND “en bloc”. We included any research which reported ERBT outcomes (both original studies and reviews). Only studies in English were included. Additionally, we looked through the references in the selected articles. A narrative synthesis of the obtained data was performed focusing on ERBT advantages and disadvantages compared with the traditional TURBT.
Energy sources for en bloc
As the introduction of lasers reignited interest in ERBT in 2011, it was clear that the novel sources would definitely draw additional further attention to this topic. Novel sources of energy applicable in each field of endourology, including ERBT, comprise Thulium lasers: Thulium fiber laser (TFL) and Pulsed Thulium: YAG laser. They have a theoretical tissue penetration depth of only 0.15 mm and 0.2 mm, respectively, which should result in less tissue being damaged and also helps to determine the surgical margin status. In their clinical trial, Enikeev et al.’s research supported this theory when they compared TFL ERBT with electric TURBT [9]. The authors found that en bloc is superior in terms of recurrence-free survival (RFS) rates at 3 and 6 months (84.5% and 67.2% for conventional TURBT versus 97.2% and 91.5% for TFL ERBT, p = 0.011 and p < 0.001, respectively). They also found that detrusor muscle was present in 58.6% of cases treated with conventional TURBT vs 91.6% for the TFL ERBT group (p < 0.001). The authors point out that en bloc allowed the surgeon to assess both circular and vertical surgical margins and also accurately evaluate the invasion into the bladder wall, as well as perivascular and perineural invasion. What is more, the TFL laser allowed for better cutting and visualization of the tumor margin due to its low penetration depth and quasi-continuous mode which should translate into real clinical benefits [10]. Unfortunately, there are currently no studies available that compare TFL with other lasers for en bloc.
As for laser energy in ERBT, the EBRUC study aimed to compare mono-/bipolar, Ho:YAG or Tm:YAG laser for ERBT [11]. Interestingly, it showed no differences regarding bladder perforation between the use of different energy sources. Other complications comprised acute bleeding rate and overall hemoglobin loss, but this did not significantly differ between the energy groups (6 (3.9%) versus 1 (1.5%); p = 0.68). Hemoglobin was significantly lower after electrical ERBT (p = 0.0013); however, overall hemoglobin loss was not clinically relevant (0.38 g/dl). Therefore, the energy—electrocautery or laser (Holmium: YAG or Thulium: YAG)—used during the surgery had no significant impact on the complication rate. Another aspect influenced by energy type is pathology specimen quality. Some authors stated that eschar in the specimen caused by electric coagulation during TURBT would affect the accuracy of tumor infiltration in terms of its depth, grading, and staging [12].
A promising improvement among outstanding lasers is the Holmium: YAG laser that uses Moses technology. It was initially designed for lithotripsy, but subsequent studies showed that this technology may be advantageous in soft tissue surgery. In particular, Moses HoLEP resulted in shorter enucleation time, shorter hemostasis time and shorter laser use time according to a recent meta-analysis [13]. With this in mind, it is important to assess the differences in ERBT using the Holmium laser with and without the Moses technology. Unfortunately, to date, no such studies were identified.
To date, a number of other energy sources have been tested during ERBT. A group of urologists from China aimed to assess the green-light laser en bloc resection and to compare the results with traditional TURBT [14]. The recurrence rate for the two techniques was comparable. Like the other lasers, green-light laser allowed to avoid the obturator nerve reflex more frequently compared to TURBT. What is more important, patients treated with green-light laser ERBT showed a higher detection rate of detrusor muscle and muscularis mucosae in the specimen [15]. Another available option for ERBT is the 1470 nm/980 nm dual-wavelength laser that has also been used to demonstrate its efficacy and safety [16]. The majority of intra- and post-operative features (e.g. complications, hospitalization time, recurrence and progression rates, etc.) are similar to those of TURBT, but intraoperative blood loss was significantly lower after ERBT and significantly fewer patients required continuous bladder irrigation after surgery. Unfortunately, unlike TFL, both these devices are characterized with increased vaporization rate and deep thermal damage of the tissue with the laser energy [17]. Nagele et al. described the working principles of waterjet hydrodissection using T-type I-Jet Hybrid-Knife [18]. In this paper, the authors presented the results of five patients diagnosed with a superficial papillary bladder tumor. The resection edges were labeled by means of electrical coagulation with the HybridKnife. Subsequently, a submucosal fluid cushion specific to the tissue layer was formed by the waterjet implementation function of the HybridKnife, thereby elevating the tumorous tissue. As a result, lamina propria was intact in all specimens, allowing the pathologist to distinguish between superficial and invasive tumors. A pathological analysis confirmed R0 resection in all the samples.
Oncological outcomes
Besides the removal of the tumor, endoscopic procedures for bladder cancer pursue another important goal—local staging. Within oncological outcomes, we would like to discuss the following features: the quality of the specimen that has been removed (from the pathologists’ point of view), the recurrence rate at the site of resection—«in-field relapse», and the recurrence rate outside the primary tumor—«out-field relapse».
The histological point of view
In case of TURBT, piecemeal resection commonly leads to specimen disorientation and makes it nearly impossible for pathologists to identify the surgical margin. While removing a large tumor, the surgeon might need to make several cuts from its surface till the bottom. Of course, at the end of the procedure, there is an option to obtain a separate specimen from the surgical margin as well as from the bottom. But this approach would allow to assess only a single and a randomly selected part of the resection area. The en bloc technique may help to overcome these difficulties, resecting not only the entire tumor but also the surrounding mucosa and underlying the stroma and the superficial muscularis propria in a single unit. Thus, it should be much easier for pathologists to identify the upper and lower part of the tumor [19].
The presence of muscle in the specimen is the surrogate for the adequate resection quality [20, 21]. Besides muscle invasion, T1-substaging also plays a significant role in prognosis and treatment strategy [22]. A recent randomized trial showed that substaging was possible in 80% TURBT and 100% ERBT cases, p = 0.02 [23]. In another trial, ERBT shortened the diagnostic time and minimized interobserver variability for T1 substaging [24]. A recent study by Yanagisawa et al. [25] provides a propensity score-matched analysis of 202 patients and confirms the previous findings: ERBT was favored in terms of adequate sampling of muscularis propria (93% vs 83%, p = 0.029) and diagnostic rates of pT1a/b substaging (100% vs 90%, p < 0.001). It led to a lower rate of residual tumor finding on re-TUR after ERBT, 15% vs 36%, p = 0.029).
A recent network meta-analysis by Motlagh et al. showed no significant difference in the rate of detrusor muscle presence between ERBT and TURBT [8]. Another meta-analysis by Zhang et al. demonstrated similar findings: no statistically significant difference were found between en bloc and TURBT groups [OR 3.59; 95% [Cl] 0.6–21.63; p = 0.16] [12]. The reason behind such a conclusion may be the low level of evidence that stems from the individual studies included in the analyses. Well-designed prospective trials are needed to support this claim.
Summing up, evidence from original studies is suggesting the superiority of en bloc in terms of histology specimen quality and, in particular, detrusor detection rate in the specimen [19, 23, 24]. However, we have not yet reached the point where the evidence is definitive and should be careful to draw any final conclusions for the reason that the data from the meta-analyses show no significant differences between these procedures.
“In-field” recurrence rate
Wilby et al. in their review of TURBT and other techniques point out that during en bloc, the urologist can see the tumor margins more clearly and maintain therefore the proper resection depth [26]. Potentially, it allows the surgeon to resect the bladder tumor more radically and to avoid second operations. Moreover, it theoretically can decrease the “in-field” relapse and avoid re-resection, as the muscle in tumor bed is removed completely [27].
The rate of in-field relapse after en bloc reported by different authors varied widely: Gao et al. found in-field tumor recurrence to be approximately 4% (1/25), Kramer et al. in 21% (7/33) and Hurle et al. in 30% (4/13) of cases [11, 28, 29]. All the studies were single-arm, and no comparison with TURBT was performed. On the one hand, speaking of in-field relapse, we should always consider the presence of detrusor muscle specimen in order to understand whether the relapse is caused by the technique itself, or by an insufficient resection depth. On the other hand, as we have mentioned previously, the technique may influence detrusor muscle detection rate and resection depth. Migliari et al. found no “in-field” recurrence and identified muscle layer in all 58 cases of ERBT. In contrast, 7/61 patients after TURBT developed short-term relapse. In this group, no detrusor was identified in eight cases [30]. Chen et al. and found no “in-field” recurrence after both en bloc and TURBT within a follow-up period 18 months [31], but the authors did not provide a muscle detection rate.
Meta-analysis by Zhang et al. [12] assessed the “in-field” recurrence based on the results of five studies that evaluated the same site recurrence rate with a follow-up time ranging between 12 and 38 months [32,33,34,35,36]. No significant difference was observed between ERBT and TURBT (OR = 0.49 (95% Cl 0.21–1.14, p = 0.10)). The original article by Bangash et al. presents opposite outcomes: in a group of 82 patients, recurrences at the primary site were 2.4% (1 out of 4 relapses) after EBRT and 19.5% (8 out of 10 relapses) after TURBT (p = 0.013) [37].
Such a substantial differences in original studies may be explained by the characteristics (stage and grade) of the cancer as well as by the surgeons’ experience. The outcomes of meta-analysis in its turn are influenced by the inclusion criteria. These discrepancies limit our ability to draw any conclusions on the impact of a particular technique on the outcome. However, the technique design and specific approach to the surgery may allow us to decrease the in-field recurrence rate in case of en bloc.
“Out-field” recurrence rate
The en bloc technique aims to remove the tumor from the detrusor layer without destroying the integrity of the tumor. The major advantage of ERBT is that the tumor can be directly removed after it is cut off. This limits the tumor contact with the bladder walls. In contrast, piecemeal resection during TURBT may lead to seeding of normal urothelium by tumor cells [38, 39]. Consequently, it would be interesting to look at the oncological results based on differentiating between the “in site” and “out site” recurrence. In particular, this is related to early relapse (usually diagnosed at 3-months follow-up cystoscopy), while late recurrence is more likely to be caused by genetic factors and may indicate another de novo lesion, rather than the continuous growth of the primary tumor. Unfortunately, data on recurrence out of the site of the primary tumor location are limited and can only be found in a few studies.
Chen et al. reported the outcomes of 142 patients with newly diagnosed NMIBC who underwent either ERBT with two-micron continuous-wave laser or monopolar TURBT [31]. The mean tumor multiplicity was 1.8 in ERBT and 1.7 in TURBT group. Immediately after the operation, intravesical chemotherapy with epirubicin was administered. Intention-to-treat comparison showed no significant difference in relapse rate between ERBT (5.63% (4/71)) and TURBT (9.86% (7/71)), respectively (p = 0.373). All the recurrences were found to be out of the first resection site, but the authors did not specify detrusor muscle rate in the specimen. Another research group produced very similar results: after a mean follow-up of 20 months, 20.6% (12 out of 58) patients in en bloc group experienced recurrence. The risk of recurrence was similar to the TURBT control group [30]. Bangash et al. observed no significant difference in relapse rate, its rate was 2.4% [37]. In the prospective observational study of Hurle and colleagues, 13 recurrences after ERBT were observed (14.4%) after a median follow-up time of 27.5 months; nine of them were detected at a new site [28]. In a large multicenter EBRUC study, 33 out of 148 patients (22.3%) experienced recurrences after ERBT. Notably, 63.6% of all recurrences occurred at a new site at 12-month follow-up [11]. Diana et al. [40] report similar 1-year recurrence-free survival rates: 90.9% (95% CI 0.859–0.962) for EBRT and 87% (95% CI 0.804–0.942) for TURBT (p = 0.88). The authors propose to use a checklist while reporting an outcomes in order to provide high-quality data.
Zhang et al. performed a meta-analysis on recurrence rate after ERBT and TURBT according to the different therapy of intravesical instillations [12]. The twelve-month recurrence did not differ between the groups using epirubicin, pirarubicin, or epirubicin combined with BCG. As for mitomycin, en bloc had a lower 12-months recurrence rate than TURBT [OR (fixed effect) 95% Cl 0.10–0.93; p = 0.04]. The 24-months recurrence did not statistically differ between two groups using epirubicin and pirarubicin. However, in mitomycin [OR 0.61; 95% [Cl] 0.41–0.90; p = 0.01] and BCG subgroups [OR 0.24; 95% [Cl] 0.07–0.84; p = 0.03], the pooled results showed that patients treated with EBRT had a lower 24-months recurrence.
It has been proven that chemotherapy agents may help in the prevention of tumor recurrence through the cells re-implantation mechanism [41, 42]. Thereby, it is important to stress that the above-mentioned oncological results presented by the authors were achieved not through surgery alone, but also through intravesical instillation of different agents, including epirubicin, pirarubicin, mitomycin and doxorubicin. The rigorous scheme of intravesical instillations still has not been established, but the EAU recommend performing intravesical chemotherapy for all patients with NMIBC based on the risk groups choosing the drug at the discretion of the surgeon [20].
It should be highlighted that ERBT was designed to decrease the tumor cells spread and thus lowering the risk of contact dissemination of cancer. Unfortunately, this outcome is a hard one to assess. When you have to choose between a technique where you have to slice cancerous lesion into pieces, and a technique which allows you to safely resect it from its base without any additional contacts with mucosa, the latter choice seems naturally to be the most appropriate one.
Complications rate
Strong evidence supports the assumption that ERBT is superior to TURBT in complications rate. Meta-analysis by Zhang et al. which was based on 19 studies with 2651 patients demonstrated that bladder perforation experienced significantly more rarely after en bloc compared to TURBT ([OR 0.17; 95% [Cl] 0.09–0.35; p < 0.00001] [12]. Similar findings were described in another meta-analysis by Yang et al.: bladder perforation was significantly less frequent in the EBRT (0.3%) rather than in TURBT group (5%), OR 0.15 [95% CI 0.05, 0.52], I2 = 0%, as well as obturator nerve reflex—0% vs 15.8%, OR 0.04 [95% CI 0.01, 0.12], I2 = 0%) [7]. Analysis by Teoh et al. [43], incorporating Delphi Survey and a consensus meeting also found a lower risk of bladder perforation for ERBT, RR 0.3, 95% CI 0.11–0.83, I2 = 1%, p = 0.02. Badawy et al. [44] randomized 120 patients between ERBT and TURBT and also observed a dramatically lower bladder perforation rate after Thulium: YAG en bloc—3.3% vs 15%, p = 0.027). Other features such as operation time, muscle detection rate and even relapse-free survival also proved to be better for ERBT.
As for other complications, unfortunately, bleeding rate was not assessed separately in the meta-analyses. However, studies where complications were classified using widely accepted Clavien-Dindo classification system found no significant difference between the two procedures [34, 45, 46]. The percentage of urethral stricture was comparable between the two techniques in the majority of studies and ranged from 0 to 3% after en bloc. A meta-analysis of Yang et al. found no difference in the incidence of urethral stricture between ERBT (1.5%) and TURBT (2.3%), OR 0.57 [0.16, 2.06], I2 = 0%) [7].
A couple of recent meta-analyses by Di et al. (including 28 studies) [47] and by Li et al. (including 7 RCTs) [48] supports the previous findings that en bloc complications (namely bladder perforation rate and obturator nerve reflex rate) occurred less frequently during ERBT.
As an aside, one may mention that an obturator nerve reflex which may cause serious complications (e.g., bladder perforation) and make the procedure more difficult does not rely on any particular technique, but instead predominantly on the use of electric energy. Its rate in laser surgery is up to three times lower than in monopolar [49]. As with bladder perforation, patients treated with EBRT had a significantly lower obturator nerve reflex [12]. The results of systematic reviews and meta-analyses comparing mono- with bipolar energy for NMIBC management vary widely. Some of them stated the use of bipolar technology was associated with a lower bladder perforation rate and lower thermal artifacts during TURBT, thus making that energy source safer and more effective [50, 51]. The others concluded that bipolar TURBT enjoys no significant advantages in terms of efficacy and safety compared to monopolar TURBT [52, 53]. Thus, bipolar TURBT should not be considered a safer and more effective energy source.
Intraoperative features
Traditionally, it is believed that TURBT is quite a simple procedure that can be performed even by young urologists with limited experience. A recent study reported that it is one of the most commonly performed surgery by residents in Italy (as first surgeon or at least performing the main steps of the procedure) [54]. However, despite the widespread recognition that TURBT is a simple procedure, this surgery requires a high degree of expertise on behalf of the surgeon. Mariappan et al. stated that urologists with more than 5 years’ experience in TURBT resected the tumor with muscle layer more frequently than urologists whose experience was less than 5 years [55]. Poletajew et al. also analyzed the learning curve of TURBT in a residency setting [56]. They concluded that the presence of detrusor in the specimen and relapse-free survival improved and increased after 101 operations; the best clinical outcomes were achieved by the surgeons after performing 170 procedures.
As for ERBT, to our knowledge, there is currently no available data on its learning curve which is still to be determined. The study aiming to assess learning curve should ideally include several surgeons and consider possible factors that affect learning. For example, studying learning curve for the prostate enucleation, Enikeev et al. conducted a randomized controlled study with three different sources of energy (thulium fiber and holmium lasers, monopolar instrument) and concluded that laser procedure appears to lend itself to quicker adaptation compared to electric one [57].
We would like to highlight that ERBT is feasible irrespective to tumor size and location. Initially, it has been considered an option for small tumors, which can be removed through the endoscope channel. Yet different approaches have been proposed to overcome these difficulties during ERBT for lesions larger 3 cm. To extract the tumor after ERBT endoscopy sheet, laparoscopic grasp and extraction bags (endobags) are used [58, 59]. One rarely used option for the large tumors is plasma vaporization of the exophytic tumor part leaving only a small portion of it for resection, and this part might be extracted through the resectoscope [60]. Enikeev et al. presented the two-step technique of ERBT for tumors larger than 3 cm [9]. Its first step includes resection of the larger exophytic area while the base of the lesion is left intact. The exophytic part is removed using a morcellator. This part of the specimen is used to determine the morphology and grading of the tumor. The second step is en bloc resection of the tumor base which is typically removed subsequently in one piece through the resectoscope [9]. It enables the surgeon to obtain muscle layer for the pathological examination. The described technique is becoming popular: Iscaife et al. [61] recently reported their initial results from using ERBT for tumor morcellation. They observed no complications higher than Clavien-Dindo grade 1, and in all cases obtained muscle.
Summary
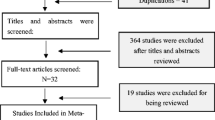
At the moment, the use of ERBT is on the rise and the number of publications that relate to this modality is also on the increase (Fig. 1). En bloc has a number of advantages over conventional TURBT, but in some aspects, the evidence is lacking and it is challenging to objectively assess them. Firstly, ERBT may improve the quality of histology which is crucial for follow-up or future treatment. Secondary, en bloc complies with the fundamental principles of oncology, which are crucial to limit the risk of tumor dissemination. Thirdly, surgeons are prone to perform TURBT with electric loop and ERBT with laser fiber as it is more convenient (although theoretically, ERBT and TURBT can be performed using both electrical and laser energy). Data that were analyzed in the current review demonstrate that both techniques lead to promising oncological outcomes. Nevertheless, surgeons pointed out several moments that made en bloc safer and a more convenient procedure with the use of laser energy, e.g. less damage to the cautery and a lower rate of obturator syndrome. The decreased peak power and the minimal penetration depth of Tm: YAG and TFLs make them the devices of choice when it comes to soft tissue surgery [10]. Still more studies on ERBT with TFL are needed in order for us to make a sound assessment of the respective pros and cons.
Speaking of ERBT’s advantages, we should keep in mind that this technique has been around for 25 years, but has only been widely used the last 10 years whereas TURBT was introduced more than a century ago and has been a standard of care for about 50 years. Therefore, this technique has passed the test of time and brings with it a wealth of experience. For this reason, it is important to conduct robust studies that obtain more data and optimize the procedure’s technique. Existing studies sometimes report controversial outcomes. However, the investigators agree that ERBT is undoubtedly a promising technique which is worthy of further study. Despite the lack of prospective and high-quality data, currently there are several clinical trials that aim to assess efficacy and safety of en bloc. They give us hope that in the nearest future the first level evidence on the topic would be provided. The search at clinicaltrials.gov allowed us to identify the following investigations. Firstly, University of Vienna conducted a multicenter randomized eBLOC trial which aims to determine in site and out of the site relapse as well as adverse events after ERBT of more than 3 cm in diameter with subsequent morcellation or piecemeal resection of tumor. Then, we also expect to see the results from a similar study undertaken by Teoh and colleagues from the Chinese University of Hong Kong where they aim to assess the efficacy of bipolar en bloc for patients with bladder tumors of ≥ 3 cm in size. Both trials were completed in the summer of 2022, so multicenter high-quality data on ERBT results that will dot all the ‘i’s and cross all the ‘t’s are awaited in the nearest future.
Conclusions
ERBT has gained in momentum with the increasingly widespread use of this kind of laser surgery. The introduction of novel sources (TFL and Thulium:YAG pulsed laser) will definitely affect how the field develops and will result in further improvements in safety and precision. The latest trials make us more certain in our belief that ERBT will be beneficial in terms of histological specimen quality, relapse rate and complications rate.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
Abbreviations
- TURBT:
-
Transurethral resection of bladder tumor
- ERBT:
-
En bloc resection of bladder tumor
- TFL:
-
Thulium fiber laser
- NMIBC:
-
Non-muscle-invasive bladder cancer
- EAU:
-
European Association of Urology
- RFS:
-
Recurrence-free survival
References
Jones HC, Swinney J (1962) The treatment of tumours of the bladder by transurethral resection. Br J Urol 34(2):215–220. https://doi.org/10.1111/j.1464-410X.1962.tb06513.x
Herr H (2018) History of transurethral resection and fulguration of bladder tumors. In: Moran ME, Nakada SY, Patel SR (eds) The history of technologic advancements in urology. Springer International Publishing, Cham, pp 59–68. https://doi.org/10.1007/978-3-319-61691-9_6
Kawada T, Ebihara K, Suzuki T, Imai K, Yamanaka H (1997) A new technique for transurethral resection of bladder tumors: rotational tumor resection using a new arched electrode. J Urol. https://doi.org/10.1097/00005392-199706000-00057
Das A, Gilling P, Fraundorfer M (1998) Holmium laser resection of bladder tumors (HoLRBT). Tech Urol 4(1):12–14. http://www.ncbi.nlm.nih.gov/pubmed/9568769
Wolters M, Kramer MW, Becker JU, Christgen M, Nagele U, Imkamp F et al (2011) Tm:YAG laser en bloc mucosectomy for accurate staging of primary bladder cancer: early experience. World J Urol 29(4):429–432. https://doi.org/10.1007/s00345-011-0686-z
Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, Dominguez Escrig JL et al (2021) European Association of Urology guidelines on non-muscle-invasive bladder cancer (Ta, T1, and carcinoma in situ). Eur Urol. https://doi.org/10.1016/j.eururo.2021.08.010
Yang H, Lin J, Gao P, He Z, Kuang X, Li X et al (2020) Is the en bloc transurethral resection more effective than conventional transurethral resection for non-muscle-invasive bladder cancer? A systematic review and meta-analysis. Urol Int. https://doi.org/10.1159/000503734
Sari Motlagh R, Rajwa P, Mori K, Laukhtina E, Aydh A, Katayama S et al (2021) Comparison of clinicopathologic and oncological outcomes between transurethral en bloc resection and conventional transurethral resection of bladder tumor: a systematic review, meta-analysis and network meta-analysis with focus on different energy sources. J Endourol 36(4):535–547
Enikeev D, Taratkin M, Margulis V, Sorokin N, Severgina L, Paramonova N et al (2020) Safety and short-term oncological outcomes of thulium fiber laser en bloc resection of non-muscle-invasive bladder cancer: a prospective non-randomized phase II trial. Bl Cancer. https://doi.org/10.1016/S2666-1683(20)34236-1
Enikeev PD, Babjuk M, Shpikina A, Shariat S, Glybochko P (2022) En bloc resection for nonmuscle-invasive bladder cancer: selecting a proper laser. Curr Opin Urol. https://doi.org/10.1097/MOU.0000000000000968
Kramer MW, Rassweiler JJ, Klein J, Martov A, Baykov N, Lusuardi L et al (2015) En bloc resection of urothelium carcinoma of the bladder (EBRUC): a European multicenter study to compare safety, efficacy, and outcome of laser and electrical en bloc transurethral resection of bladder tumor. World J Urol 33(12):1937–1943
Zhang D, Yao L, Yu S, Cheng Y, Jiang J, Ma Q et al (2020) Safety and efficacy of en bloc transurethral resection versus conventional transurethral resection for primary nonmuscle-invasive bladder cancer: a meta-analysis. World J Surg Oncol 18(1):4
Ramadhani MZ, Kloping YP, Rahman IA, Yogiswara N, Renaldo J, Wirjopranoto S (2022) Comparative efficacy and safety of holmium laser enucleation of the prostate (HoLEP) using moses technology and standard HoLEP: a systematic review, meta-analysis, and meta-regression. Ann Med Surg 81:104280. https://doi.org/10.1016/j.amsu.2022.104280
Fan J, Wu K, Zhang N, Yang T, Liu N, Jiang Y et al (2021) Green-light laser en bloc resection versus conventional transurethral resection for initial non-muscle-invasive bladder cancer: a randomized controlled trial. Int J Urol. https://doi.org/10.1111/iju.14592
de Jong FC, Hoedemaeker RF, Kvikstad V, Mensink JTM, de Jong JJ, Boevé ER et al (2021) T1 substaging of nonmuscle invasive bladder cancer is associated with bacillus calmette-guérin failure and improves patient stratification at diagnosis. J Urol. https://doi.org/10.1097/JU.0000000000001422
Fu J, Fu F, Wang Y (2021) 1470 nm/980 nm dual-wavelength laser is safe and efficient for the en-bloc resection of non-muscle invasive bladder cancer: a propensity score-matched analysis. J Int Med Res. https://doi.org/10.1177/03000605211065388
Enikeev D, Shariat SF, Taratkin M, Glybochko P (2020) The changing role of lasers in urologic surgery. Curr Opin Urol. https://doi.org/10.1097/MOU.0000000000000695
Nagele U, Kugler M, Nicklas A, Merseburger AS, Walcher U, Mikuz G et al (2011) Waterjet hydrodissection: first experiences and short-term outcomes of a novel approach to bladder tumor resection. World J Urol 29(4):423–427
Lodde M, Lusuardi L, Palermo S, Signorello D, Maier K, Hohenfellner R et al (2003) En bloc transurethral resection of bladder tumors: use and limits. Urology 62(6):1089–1091. https://linkinghub.elsevier.com/retrieve/pii/S0090429503007611
Babjuk M, Burger M, Gontero P, Liedberg F, Masson-Lecomte A, Palou J, van Rhijn BWG, Rouprêt M, Sylvester R (2021) EAU guidelines on non-muscle-invasive bladder cancer (TaT1 and CIS). Eur Urol 31:1–56
Sylvester RJ, Rodríguez O, Hernández V, Turturica D, Bauerová L, Bruins HM et al (2021) European Association of Urology (EAU) prognostic factor risk groups for non-muscle-invasive bladder cancer (NMIBC) incorporating the WHO 2004/2016 and WHO 1973 classification systems for grade: an update from the EAU NMIBC guidelines panel[Formula present]. Eur Urol
Orsola A, Werner L, de Torres I, Martin-Doyle W, Raventos CX, Lozano F et al (2015) Reexamining treatment of high-grade T1 bladder cancer according to depth of lamina propria invasion: a prospective trial of 200 patients. Br J Cancer. 112(3):468–474. http://www.nature.com/articles/bjc2014633
Gallioli A, Diana P, Fontana M, Territo A, Rodriguez-Faba Ó, Gaya JM et al (2022) En bloc versus conventional transurethral resection of bladder tumors: a single-center prospective randomized noninferiority trial. Eur Urol Oncol 5(4):440–448. https://linkinghub.elsevier.com/retrieve/pii/S2588931122000682
Yanagisawa T, Yorozu T, Miki J, Iwatani K, Obayashi K, Sato S et al (2021) Feasibility and accuracy of pathological diagnosis in en-bloc transurethral resection specimens versus conventional transurethral resection specimens of bladder tumour: evaluation with pT1 substaging by 10 pathologists. Histopathology 78(7):943–950. https://doi.org/10.1111/his.14307
Yanagisawa T, Matsukawa A, Iwatani K, Sato S, Hayashida Y, Okada Y et al (2023) En bloc resection versus conventional TURBT for T1HG bladder cancer: a propensity score-matched analysis. Ann Surg Oncol. https://doi.org/10.1245/s10434-023-13227-7
Wilby D, Thomas K, Ray E, Chappell B, O’Brien T (2009) Bladder cancer: new TUR techniques. World J Urol. https://doi.org/10.1007/s00345-009-0398-9
Xu J, Xu Z, Yin H, Zang J (2022) Can a reresection be avoided after initial en bloc resection for high-risk nonmuscle invasive bladder cancer? A systematic review and meta-analysis. Front Surg 9:849929
Hurle R, Lazzeri M, Colombo P, Buffi N, Morenghi E, Peschechera R et al (2016) “En Bloc” resection of nonmuscle invasive bladder cancer: a prospective single-center study. Urology 90:126–130
Gao X, Ren S, Xu C, Sun Y (2008) Thulium laser resection via a flexible cystoscope for recurrent non-muscle-invasive bladder cancer: Initial clinical experience. BJU Int. https://doi.org/10.1111/j.1464-410X.2008.07814.x
Migliari R, Buffardi A, Ghabin H (2015) Thulium laser endoscopic en bloc enucleation of nonmuscle-invasive bladder cancer. J Endourol. https://doi.org/10.1089/end.2015.0336
Chen X, Liao J, Chen L, Qiu S, Mo C, Mao X et al (2015) En bloc transurethral resection with 2-micron continuous-wave laser for primary non-muscle-invasive bladder cancer: a randomized controlled trial. World J Urol. https://doi.org/10.1007/s00345-014-1357-7
Yang D, Xue B, Zang Y, Liu X, Zhu J, Zhou Y et al (2014) Efficacy and safety of potassium-titanyl-phosphate laser vaporization for clinically non-muscle invasive bladder cancer. Urol J
Bălan GX, Geavlete PA, Georgescu DA, Ene CV, Bulai CA, Păunescu MA et al (2018) Bipolar en bloc tumor resection versus standard monopolar TURBT—which is the best way to go in non-invasive bladder cancer? Rom J Morphol Embryol 59(3):773–780
Zhang KY, Xing JC, Li W, Wu Z, Chen B, Bai DY (2017) A novel transurethral resection technique for superficial bladder tumor: Retrograde en bloc resection. World J Surg Oncol. https://doi.org/10.1186/s12957-017-1192-6
Xu Y, Guan W, Chen W, Xie C, Ouyang Y, Wu Y et al (2015) Comparing the treatment outcomes of potassium-titanyl-phosphate laser vaporization and transurethral electroresection for primary nonmuscle-invasive bladder cancer: a prospective, randomized study. Lasers Surg Med. https://doi.org/10.1002/lsm.22342
Sureka SK, Agarwal V, Agnihotri S, Kapoor R, Srivastava A, Mandhani A (2014) Is en-bloc transurethral resection of bladder tumor for non-muscle invasive bladder carcinoma better than conventional technique in terms of recurrence and progression?: A prospective study. Indian J Urol 30(2):144–149
Bangash M, Ather MH, Khan N, Mohammad S, Uddin Z (2020) Comparison of recurrence rate between “EN BLOC” resection of bladder tumour and conventional technique for non-muscle invasive bladder cancer. J Ayub Med Coll Abbottabad 32(4):435–440
Mori K, D’Andrea D, Enikeev DV, Egawa S, Shariat SF (2020) En bloc resection for nonmuscle invasive bladder cancer: Review of the recent literature. Curr Opin Urol. https://doi.org/10.1097/MOU.0000000000000697
Kramer MW, Altieri V, Hurle R, Lusuardi L, Merseburger AS, Rassweiler J et al (2017) current evidence of transurethral en-bloc resection of nonmuscle invasive bladder cancer. Eur Urol Focus. https://doi.org/10.1016/j.euf.2016.12.004
Diana P, Baboudjian M, Gallioli A, Territo A, Fontanet S, Izquierdo P et al (2023) Implementing a checklist for transurethral resection of bladder tumor to standardize outcome reporting: when high-quality resection could influence oncological outcomes. Eur Urol Open Sci 48:24–27
Sangeda RZ, Vandepitte J, Huygens A, Van Cleynenbreugel B, Van Poppel H, de Witte PAM (2010) Prevention of tumor cell reimplantation during transurethral resection: the in-vitro antiadhesive and cytotoxic properties of an irrigant containing polyethylene glycol 400. Anticancer Drugs 21(6):645–650
Bryan RT, Collins SI, Daykin MC, Zeegers MP, Cheng KK, Wallace DMA et al (2010) Mechanisms of recurrence of Ta/T1 bladder cancer. Ann R Coll Surg Engl 92(6):519–524
Teoh JY-C, MacLennan S, Chan VW-S, Miki J, Lee H-Y, Chiong E et al (2020) An international collaborative consensus statement on en bloc resection of bladder tumour incorporating two systematic reviews, a two-round Delphi survey, and a consensus meeting. Eur Urol 78(4):546–569. https://linkinghub.elsevier.com/retrieve/pii/S0302283820303274
Badawy A, Sultan SM, Marzouk A, El-Sherif E (2023) Thulium laser en bloc resection versus conventional transurethral resection of urinary bladder tumor: A comparative prospective study. Urol Ann 15(1):88–94
Li K, Xu Y, Tan M, Xia S, Xu Z, Xu D (2019) A retrospective comparison of thulium laser en bloc resection of bladder tumor and plasmakinetic transurethral resection of bladder tumor in primary non-muscle invasive bladder cancer. Lasers Med Sci 34(1):85–92
Hayashida Y, Miyata Y, Matsuo T, Ohba K, Sakai H, Taba M et al (2019) A pilot study to assess the safety and usefulness of combined transurethral endoscopic mucosal resection and en-bloc resection for non-muscle invasive bladder cancer. BMC Urol. https://doi.org/10.1186/s12894-019-0486-0
Di Y, Li H, He C, Peng H (2022) En-bloc transurethral resection vs. conventional transurethral resection for primary non-muscle invasive bladder cancer: a meta-analysis. Actas Urológicas Españolas (English Ed). https://linkinghub.elsevier.com/retrieve/pii/S2173578622000877
Li Z, Zhou Z, Cui Y, Zhang Y (2022) Systematic review and meta-analysis of randomized controlled trials of perioperative outcomes and prognosis of transurethral en-bloc resection vs. conventional transurethral resection for non-muscle-invasive bladder cancer. Int J Surg 104:106777. https://linkinghub.elsevier.com/retrieve/pii/S1743919122005544
Abedi Yarandi V, Khatami F, Aghamir SMK (2020) The obturator nerve reflex after thulium laser vs. monopolar transurethral resection of bladder tumors: a randomized clinical trial. Urol J 18(6):688–692
Krajewski W, Nowak Ł, Moschini M, Mari A, Di Trapani E, Xylinas E et al (2021) Systematic review and meta-analysis on bipolar versus monopolar transurethral resection of bladder tumors. Translat Androl Urol. https://doi.org/10.21037/tau-20-749
Ma Y, Sun L, Lin X, Zhang W, Wang D (2020) Efficacy and safety of bipolar versus monopolar transurethral resection of bladder tumors: a meta-analysis of randomized controlled trials. J Cancer Res Ther 16(7):1588–1595
Xie K, Cao D, Wei Q, Ren Z, Li J, Li Y et al (2021) Bipolar versus monopolar transurethral resection of non-muscle-invasive bladder cancer: a systematic review and meta-analysis of randomized controlled trials. World J Urol. https://doi.org/10.1007/s00345-020-03271-3
Sharma G, Sharma AP, Mavuduru RS, Bora GS, Devana SK, Singh SK et al (2021) Safety and efficacy of bipolar versus monopolar transurethral resection of bladder tumor: a systematic review and meta-analysis. World J Urol. https://doi.org/10.1007/s00345-020-03201-3
Cocci A, Patruno G, Gandaglia G, Rizzo M, Esperto F, Parnanzini D et al (2018) Urology residency training in Italy: results of the first national survey. Eur Urol Focus. https://doi.org/10.1016/j.euf.2016.06.006
Mariappan P, Zachou A, Grigor KM (2010) Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on operator experience. Eur Urol 57(5):843–849
Poletajew S, Krajewski W, Kaczmarek K, Kopczyński B, Stamirowski R, Tukiendorf A et al (2020) the learning curve for transurethral resection of bladder tumour: How many is enough to be independent, safe and effective surgeon? J Surg Educ. https://doi.org/10.1016/j.jsurg.2020.02.010
Enikeev D, Glybochko P, Rapoport L, Gahan J, Gazimiev M, Spivak L et al (2018) A randomized trial comparing the learning curve of 3 endoscopic enucleation techniques (HoLEP, ThuFLEP, and MEP) for BPH using mentoring approach—initial results. Urology 121:51–57. https://doi.org/10.1016/j.urology.2018.06.045
Fritsche HM, Otto W, Eder F, Hofstädter F, Denzinger S, Chaussy CG et al (2011) Water-jet-aided transurethral dissection of urothelial carcinoma: a prospective clinical study. J Endourol 25:1599–1603
Hurle R, Casale P, Lazzeri M, Paciotti M, Saita A, Colombo P et al (2020) En bloc re-resection of high-risk NMIBC after en bloc resection: results of a multicenter observational study. World J Urol 38(3):703–708
Geavlete B, Multescu R, Georgescu D, Stanescu F, Jecu M, Geavlete P (2012) Narrow band imaging cystoscopy and bipolar plasma vaporization for large nonmuscle-invasive bladder tumors-results of a prospective, randomized comparison to the standard approach. Urology. https://doi.org/10.1016/j.urology.2011.08.081
Iscaife A, Ribeiro Filho LA, Aparecido Pereira MW, Gallucci FP, Chade D, Murta CB et al (2022) Holmium laser resection of large bladder tumors: technique description, feasibility, and histopathological quality analysis. Urology. 165:373. https://www.sciencedirect.com/science/article/pii/S0090429522003429
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Enikeev, D., Morozov, A., Shpikina, A. et al. A 10-year renaissance of en bloc resection of bladder tumors (ERBT): Are we approaching the peak or is it back to the trough?. World J Urol 41, 2607–2615 (2023). https://doi.org/10.1007/s00345-023-04439-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04439-3