Abstract
Transurethral resection (TURB) is the essential surgical procedure used to diagnose, stage and treat bladder tumors. TURB is an ideal operation—focal, targeted, patient-centered, single-port, minimally invasive through a natural orifice (the urethra), safe, and repeatable. Urologists today are armed with a dazzling array of sophisticated endoscopic instruments. Modern flexible digital cystoscopes and video-assisted resectoscopes combine the essentials—access, superior optics, working elements, and energy—to detect, decipher and destroy tumors growing in the bladder. Current endoscopes provide magnified high-definition views of the bladder interior, permitting visual removal of bladder tumors using panoply of cutting loops, forceps or graspers and their targeted destruction by electrocautery or laser energy. The methods, means and skills we enjoy today began in the nineteenth century and refined in the 20th owing to collective genius and ingenuity of many surgeons, scientists, inventors, and visionary entrepreneurs.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Introduction
Transurethral resection (TURB) is the essential surgical procedure used to diagnose, stage and treat bladder tumors. TURB is an ideal operation—focal, targeted, patient-centered, single-port, minimally invasive through a natural orifice (the urethra), safe, and repeatable. Urologists today are armed with a dazzling array of sophisticated endoscopic instruments. Modern flexible digital cystoscopes and video-assisted resectoscopes combine the essentials—access, superior optics, working elements, and energy—to detect, decipher and destroy tumors growing in the bladder. Current endoscopes provide magnified high-definition views of the bladder interior, permitting visual removal of bladder tumors using panoply of cutting loops, forceps or graspers and their targeted destruction by electrocautery or laser energy. The methods, means and skills we enjoy today began in the nineteenth century and refined in the 20th owing to collective genius and ingenuity of many surgeons, scientists, inventors, and visionary entrepreneurs.
Bladder Tumors from Antiquity to Endoscopic era
Although likely they were recognized in antiquity , bladder tumors were mentioned first by Lacuna in 1551. Despite scattered reports of excision of an occasional tumor found during lithotomy, the first operations targeting bladder tumor were performed in the 16th and 17th centuries. Up to the eighteenth century, surgeons removed bladder tumors blindly through a dilated urethra, or open suprapubic or lateral perineal incision, using ligatures, ecrasement (steel-wire loop), arrachement (tearing out), enucleation, or cauterization.
During the eighteenth century, the so-called carnosities of the bladder became more clearly understood in scattered works on the pathologic anatomy of bladder tumors, polyps, ulcerations, and carcinomas. The first landmark in the history of bladder tumors was Chopart’s classical work, “Traite des Maladies des Voies Urinaires.” He noted essential differences between various kinds of bladder tumors and regarded “fungosities of the bladder” as benign tumors subject to cancerous degeneration. As a result, the nineteenth century witnessed a marked advance in the knowledge of bladder tumor pathology soundly based on histologic structure. For example, Civiale differentiated papillary fungoid type of growths from solid cancerous tumors. Definition of these lesions, now described as low-grade papillary tumors separate from high-grade solid tumors, was highly relevant because the more common papillary growths were the only tumors early endoscopists could treat successfully. Solid tumors were usually invasive and far too advanced for local excision [1].
Early Endoscopic Era
Table 6.1 lists landmark developments in the endoscopic access and improved treatment surgical treatments of bladder tumors [2]. Beginning with Bozzini in 1806, physicians, armed only with speculum, candle and mirror, began to explore body cavities and learn endoscopic anatomy by practical experience. The urinary tract was first explored by inspection through crude specula inserted into the urethral meatus, chiefly in women. Surgeons attempted to seize pedunculated growths transurethrally, tie the pedicle and blindly tear away as much tissue as possible, usually with unsatisfactory results.
In the mid-nineteenth century, Desormeaux introduced his endoscope, and cystoscopy became established as a practical, although difficult, means of clinical investigation. He designed his instrument around a paraffin flamed that burned more brightly by the addition of turpentine. In 1853, Desormeaux was able to perform the first true endoscopic operation when he extracted a papilloma through the urethra using his urethroscope [3]. Trouve made a critical contribution to cystoscopy in 1873 when he moved the light source (a glowing hot platinum wire) to the inner tip of his “Polyscope.” In 1876, Rutenberg, attempting to improve vision within the female bladder, designed his “Blasenspiegel” through which he was the first to observe the larger surfaces of the bladder. Later, the dermatologist Grunfeld improved endoscopic surgery in the urethra and bladder. He developed a urethroscope , as well as endoscopic loop threaders, scissors, forceps, and knives, and was the first to operate in the bladder under direct control of the eye when he removed a bladder papilloma through his urethroscope in 1881. In 1885, Grunfeld developed the “Polypenkneipe ,” the first cystoscope specifically designed to remove tumors from the urethra and bladder [4].
Max Nitze and the Operating Cystoscope
Maximilian Nitze introduced the first direct-vision cystoscope in 1877, which markedly improved vision inside the bladder but offered limited operating capability [5]. Never satisfied, from 1891 to 1894, Nitze designed and constructed the first practical operating cystoscope (Fig. 6.1). He became the first to coagulate a bladder polyp visualized with Edison’s new light bulb and using cold and hot wire loops for galvanocautery. He initiated systematic cystoscopic treatment of bladder tumors and reported removal of tumors from 150 cases with only 1 death and 20 recurrences. Using curette, cutting forceps, cautery, and wire loop, he was able to remove many papillary tumors cleanly [6]. Others followed his lead, and in 1905, Weinrich reported treating 101 cases of bladder tumors by the Nitze method with 71% recoveries without a recurrence. The procedure was mostly excision of pedunculated tumors with a portion of mucosa or else twisting off the pedicle at its base. For most European and American urologists, however, the Nitze cystoscope was cumbersome to manipulate, and galvanic cautery using the wire loop proved to be an unreliable means of tissue destruction. With advent of diathermy in the United States, surgery of bladder tumors using Nitze’s operating cystoscope was practically abandoned.
Cystofulguration
Nagelschmidt and Doyen in the United States were the first to advocate use of electrically induced heat to treat cancerous growths. Nagelschmidt devised an adequate apparatus for this purpose and is credited with originating the term diathermy. But it was Edwin Beer of New York who really founded electrosurgery of the bladder.
In 1908, Beer, convinced that Nitze’s earlier transurethral treatment of bladder tumors was superior to open surgery, conceived the idea of using high-frequency electric current through a catheterizing-cystoscope to coagulate bladder tumors. He used a two-channel Nitze cystoscope (one channel for a 6F copper electrode and the other for irrigation of the bladder) and a monopolar (Oudin) current derived from a resonator made by the American cystoscope maker, Reinhold Wappler. Direct current was applied at various points to papillary growths for 15–30 s at a time, while the bladder was distended with sterile water. Beer treated two women and saw no spark when the full current was thrown on without resistance. Tumor tissue was dessicated at cautery points even under water, and patients experienced no more discomfort than during ordinary cystoscopy. Beer concluded that coagulation was simpler than loop treatment, and in 1910, he reported his successful cases in a landmark article, claiming fulguration to be “proven effective in the cure of bladder papilloma” [7].
For the next 25 years, Beer devoted much of his time to the study of bladder neoplasms and continued to develop and improve his method of treatment, eventually reporting his aggregated experience of cases in 1935. After Beer died in 1938, Reed Nesbit wrote, “Development of this technique by its brilliant discoverer marked one of the greatest advances in the history of urology; it led not only to radical change in the therapeutic management of bladder tumors, but also paved the way for subsequent electroresection methods by proving that high-frequency current could be employed effectively under water” [1]. It did all that and more. Based largely on Beer’s pioneering concept, outpatient cystoscopic fulguration of recurrent papillary bladder tumors remains common practice today.
Transurethral Resection
Although cystofulguration was used around the world to destroy benign papillomas and small papillary carcinomas, it was known that not all papillary tumors behaved in an indolent manner. Compounding the problem was that pathologists could not always distinguish between benign, malignant or invasive neoplasms. Even Beer became pessimistic about the efficacy of endoscopic diathermy because it was applicable only to small tumors, did not prevent recurrences, and was ineffective against invasive bladder tumors. Clearly, a more effective means to remove and destroy bladder tumors was needed.
Transurethral resection of bladder tumors could not have developed without the first practical incandescent lamp invented by Thomas Edison in 1879, high frequency electric current devised by Heinrich Hertz in 1888, the vacuum tube permitting continuous current introduced in 1908 by Lee DeForest, application of high-frequency electrical current underwater by Beer in 1910, the fenestrated tube conceived by Hugh Young in 1909, the first practical cutting current by George Wyeth in 1924, and cutting and coagulation current combined into one by Reinhold Wappler in 1931.
In 1926, a urologist in New York named Maximilian Stern introduced a revolutionary new instrument he called a resectoscope. Stern’s resectoscope consisted of a sheath and working parts assembled in a compact bundle made up of a direct-vision telescope, a light carrier, a water conduit, and a cutting loop or active electrode using a bipolar current. Stern devised a manually controlled gear mechanism to slide a tungsten wire loop back and forth through a fenestra with even movement using the attached control handle (Fig. 6.2). Designed as a punch operation for the prostate, the moveable wire was able to whittle away obstructing prostatic tissue with ease, but the instrument was cumbersome to use in the bladder because it was difficult to engage bladder tissue in the recessed fenestra. However, the cutting loop offered the obvious advantage of removing rather than simply cauterizing bladder tumors [8].
Theodore Davis, who had been an electrical engineer before entering urology, combined the cutting current with a diathermy machine for hemostasis, and in 1931 reported good results. Davis improved the loop by using a larger tungsten wire on Stern’s resectoscope, and he provided better insulation (Fig. 6.3). More importantly, working with Bovie, he incorporated cutting and coagulation diathermy, inventing a duel-foot pedal allowing him to switch between either current during surgery.
In 1931, Joseph McCarthy, also of New York, made significant improvements in the resectoscope. McCarthy fashioned a lens system that widened the visual field, used a nonconducting Bakelite sheath, added a rack-and-pinion lever to move an electric-arc cutting loop, incorporated separate currents for coagulation and cutting, and most importantly, moved the wire loop and cutting window to the tip of the instrument. However, the key to success of this instrument was the foroblique telescope developed by Wappler. It provided both a wide-angle view and sufficient magnification allowing precise placement and manipulation of the cutting loop. The chief difference from the Stern instrument, cutting was done toward the bladder (amputating tissue away from the surgeon), while using the McCarthy resectoscope, one cut from within the bladder outward. McCarthy found that his modifications were better adapted to resect vesical neoplasms because with the extended loop, it was easier to engage bladder tumors and to cut slices of tissue back toward the operator under direct visual control [9].
The Stern-McCarthy resectoscope, as it became known, was the first practical cutting-loop resectoscope, and it quickly replaced fulguration to become the dominant method used to diagnose and treat bladder neoplasms for the rest of the twentieth century (Figs. 6.4a, b and 6.5). Numerous modifications of the Stern-McCarthy resectoscope followed, but they were all based on the original design. The most significant of these was a novel one-handed resectoscope devised by Reed Nesbit in 1938 [10]. Nesbit attached a rotating thumb hole and movable carriage with spring for return of the loop, and foreshortened the fenestrum, allowing the loop to extend 1 cm beyond the beak of the sheath to evacuate tissue. Having one hand free allowed the surgeon to elevate the bladder base through the rectum or apply suprapubic pressure to bring tumors within reach of the resectoscope (Fig. 6.6).
Nesbit’s resectoscope became the forerunner to current modern resectoscopes, which maintain the same concept and design. Although his, like the Stern-McCarthy resectoscope, was developed primarily for transurethral resection of the prostate, TURP has given way to newer methods to relieve prostatic obstruction, whereas TURB remains today a standard operation for bladder tumors. The reasons are obvious: tumors are better removed by resection than destroyed by fulguration, tissue is provided for accurate pathologic evaluation, virtually all superficial and some minimally invasive neoplasms can be cured, and the method can be repeated indefinitely to access the bladder and control recurrent tumors.
Past, Present, and Future
Over the century and a quarter since endoscopy was first conceived in 1806 to the development of the first modern resectoscope in 1931, endoscopic surgery of bladder tumors advanced from an idea to practical reality. Noteworthy individuals and their innovations each built on discoveries of the past to advance endoscopic treatment of bladder tumors founded on four landmark inventions: a cystoscope, incandescent light bulb, the fenestrated tube, and the application of high-frequency electrical current active in a water environment.
In the second half of the twentieth century, further improvements were created, none more important than introduction of zoom lens and rod-lens system by the physicist Harold Hopkins [11]. Use of glass fibers (fiberoptics), first for illumination and later for flexible optics, was able to carry true video images, and allowed for the creation of flexible endoscopy. Video cameras soon followed, which improved the ergonomics, safety and success rates of tumor resections.
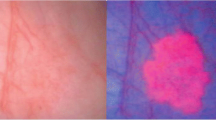
In 1970, Boyle and Smith created the charge-coupled device (CCD) —a semiconductor chip that could record images as a grid of pixels, leading to a move from fiberoptic endoscopy to distal sensor (digital) image-based endoscopy [12]. Digital endoscopes can identify lesions as small as 1 mm at greater distances than was previously possible with fiberoptic technology. Light weight digital cameras were soon attached to the eyepiece of resectoscopes and connected to high definition TV screens to provide superb magnified vision inside the bladder and to facilitate facile transurethral resection. The CCD chip also made possible narrow-band imaging (NBI), a filter that restricts wavelengths of white light to highlight mucosal microvessels, which are enhanced in urothelial tumors in contrast to bland normal mucosa. NBI improves detection and mucosal extent of tumors, facilitating more complete destruction.
Real-time endoscopic histologic tissue and molecular characterization of bladder tumors is on the horizon, with Raman spectroscopy, optical coherence tomography, confocal endomicroscopy, and their disciples projected to become routine in the near future. Enhanced imaging technology represents technical improvements, based on the premise that if one sees better, one resects better, but they are not designed as replacements for the well-established and proven TURB. The basic TURB remains the same as conceived by Stern, Davis, McCarthy and Nesbit nearly a century ago—using a cystoscopic sheath, wide-angle telescope, single-handed working element to guide assortments of loops and coagulating devices into the bladder used to remove and destroy tumors, direct vision light and lens sources within the bladder, saline irrigation (replacing water), separate cutting and coagulation currents and a foot switch to control both. None of this would have happened if not for the genius displayed by countless individuals from multiple disciplines in the twentieth century, who combined their talents to transform Nitze’s original concept of an operating cystoscope into today’s sophisticated and successful endoscopic treatment of many maladies involving the urinary tract. Arguably, bladder neoplasms are the most significant of these, and suffering patients are the ultimate beneficiaries of their discoveries.
References
Zorgniotti A. Bladder cancer in the pre-cystoscopic era. Prog Clin Biol Res. 1984;162A:1–9.
Herr HW. Early history of endoscopic treatment of bladder tumors. From Grunfeld’s polypenkneipe to Stern-McCarthy resectoscope. J Endourol. 2006;20:85–91.
Desormeaux AJ. Del’Endoscope et de ses Applications au Diagnostic et au Traitement des Affections de l’Urethre et de la Vessie. Paris; 1865.
Grunfeld J. Polypen der Harnblase, auf endokopischem Wege diagnostiziert und operiert. Wien Med Presse; 1885. p. 89.
Herr HW. Max Nitze, the cystoscope and urology. J Urol. 2006;176:1313–6.
Nitze M. Ueber intravesicale Operationen von Blasengeschwulsten. Centr Chir. 1895;22:971.
Beer E. Removal of neoplasms of the urinary bladder: a new method, employing high frequency (Oudin) currents. JAMA. 1910;54:1768.
Stern M. A new cystoscopic instrument employing a cutting current capable of operation in a water medium. Read before the New York Academy of Medicine, January 20, 1926.
McCarthy JF. A new apparatus for endoscopic surgery of the prostate, diathermia, and excision of vesical growths. J Urol. 1931;26:695–7.
Nesbit RMA. Modification of the Stern-McCarthy resectoscope permitting third dimensional perception during transurethral prostatectomy. J Urol. 1938:646–8.
Gow JG. Harold Hopkins and optical systems for urology—an appreciation. Urology. 1998;52:152–7.
Boyle WS, Smith GS. Charge coupled semiconductor devices. Bell Syst Tech J. 1970;49:587–93.
Acknowledgement
Assistance and illustrations kindly provided by Tupper Stevens, archivist, William P. Didusch Center for Urologic History, Linthicum, Maryland.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Herr, H. (2018). History of Transurethral Resection and Fulguration of Bladder Tumors. In: Patel, S., Moran, M., Nakada, S. (eds) The History of Technologic Advancements in Urology. Springer, Cham. https://doi.org/10.1007/978-3-319-61691-9_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-61691-9_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61689-6
Online ISBN: 978-3-319-61691-9
eBook Packages: MedicineMedicine (R0)