Abstract
Introduction
We evaluated a new digital single-use flexible ureteroscope, LithoVue™ with respect to deflection, image quality and maneuverability.
Methods
A prospective cohort study was conducted in eight tertiary reference centers in Europe in December 2015 and January 2016. All consecutive patients included underwent flexible ureteroscopy and were 18 years or older. Deflection and image quality pre- and post-use and maneuverability were rated with a Likert scale.
Results
A total of 40 procedures were performed (five per institution). The indication for FURS was treatment of renal stones in 92.5 % of the cases. Before LithoVue™ usage, the median measured upward and downward deflections were both 270°. Image quality was rated as “very good” in 65 % of cases and “good” in 30 %. Maneuverability was “very good” in 77.5 % and “good” in 17.5 %. At the final evaluation, median upward and downward deflections were both 270°. Image quality was still “very good” in 65 % of cases and “good” in 30 % with no significant difference compared with preoperative data (p = 1). Maneuverability was “very good” in 72.5 % and “good” in 17.5 %, with no significant difference compared with preoperative data (p = 0.92). Two LithoVue™ broke during surgery (5 %): one occurring in extreme deflection with acute infundibulopelvic angle and spontaneous loss of vision for the second one.
Conclusion
The LithoVue™ displayed good image quality, active deflection and maneuverability. Further evaluation of surgical outcomes and cost analysis will help to present the best utility of this single-use FURS in current practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It was as early as 1964 that Marshall presented the first flexible ureteroscope (FURS). This instrument did not gain popularity since it was only passively deflectable and did not include a working channel. Although the first successful procedure using FURS with active deflection in humans has been reported by Takayasu, it was not until 1987 that Demetrius Bagley introduced flexible ureteroscopy as we know it today [1–3]. FURS currently firmly positioned in the urologists’ armamentarium for modern stone management [4, 5]. Since its introduction, FURS developed in many aspects such as fiberoptic bundles for light transmission and image relay, miniaturization of the outer diameter, passive and active deflections in upward and downward directions and working channel. One of the latest developments was the introduction of a digital imaging system which has improved the image quality substantially. Currently, FURS is fiberoptic or digital. The difference between these two types of endoscopes is the light transmission and image relay. In fiberoptic scopes, light and image are transmitted in analog format through fiberoptic whereas illumination in digital scopes is made by fiberoptics or by a diode (DEL) and image capture charged by a digital sensor located at the distal end of the endoscope: either complementary metal oxide semiconductor (CMOS) or charged coupled device (CCD). In both cases, most manufacturers have fiberoptic and digital models with a working channel of 3.6 Fr (for irrigation and the use of accessory instruments) and at least one 270° active deflection of the tip. Despite advancements in the durability of ureteroscopes, they are nonetheless fragile instruments and must be handled with care. Several studies evaluated the durability of FURS and reported variable usage time before breakage or repair [6–15]. The economics of reuseable flexible ureteroscopy use is dependent on the number of uses before repair is required and is also affected by the initial purchase cost, and these costs may limit its use in centers [16, 17]. Besides the financial aspect, reusable FURS undergoes high-level disinfection between procedures, requiring a dedicated staff and equipment and resulting in the use of a non-sterile instrument [18].
For these reasons, single-use endoscopes have been developed. The most recent one is the LithoVue™ (Boston Scientific).
The objective of the current study was to evaluate the first clinical performance of the LithoVue™ endoscope.
Materials and methods
Study design and participants
A prospective cohort study was conducted in eight tertiary reference centers in Europe (Denmark, France, Germany, two in Italy, Spain, the Netherlands, and UK) in December 2015 and January 2016. All consecutive patients included were 18 years or older and underwent a flexible ureterorenoscopic procedure (either diagnostic or therapeutic). The following preoperative data were prospectively collected (see “Appendix”): gender, age, indication for flexible ureteroscopy (stone or tumor), location and size of stone or tumor evaluated by preoperative CT scan, anatomical specificities and presence of preoperative ureteral stent. All patients gave informed consent to undergo an ureterorenoscopic procedure, and instead of a formal ethics committee approval, the principles of the Declaration of Helsinki were followed.
LithoVue™
LithoVue™ is a single-use digital FURS, CE approved, with a 7.7-Fr tip diameter, 9.5-Fr outer diameter at the main part, a 3.6-Fr working channel for insertion of instruments and irrigation, 270° deflection in upward and downward directions and a length of 68 cm (a total of 82 cm with handle) (Figs. 1, 2). This digital camera is made of a complementary metal oxide semiconductor (CMOS) sensor located at the tip of the endoscope and provides 0° direct view with 85° field of vision. The scope can be connected via a cable to an all-in-one touchscreen computer, which includes monitor workstation and image processing software (Fig. 3). If preferred, it can be connected to the operating room’s monitor via a DVI connection (Fig. 3). The LithoVue™ cannot be sterilized, and the usage time available per scope is limited to 4 h.
Procedures
Preoperative urine analysis and culture were performed, and appropriate antibiotics were given before intervention following local protocol. Patients were placed in the lithotomy position under spinal or general anesthesia. All procedures were conducted by experienced endourologists. Each procedure began with the placement of a hydrophilic guidewire in the renal pelvis under fluoroscopic guidance. According to local protocol, a retrograde pyelography and/or a semirigid ureterorenoscopy and/or directly placement of ureteral access sheath (UAS) were performed. Subsequently, the LithoVue™ was placed. In case of UAS use, size, length and location of the tip were recorded. Otherwise, the scope was placed besides or over a safety guidewire.
Evaluation criteria
A checklist with the different criteria to evaluate was provided to each participant (see “Appendix”). The following data were collected: use of ureteral access sheath, use of laser fiber, laser fiber size, single use or reusable fiber, number of passes with fiber, laser settings (energy, frequency and pulse duration), laser time, total laser energy usage, use of basket, number of passes with basket, breakage of scope, operative time (from the time of cystoscope insertion to the completion of ureteral stent placement), number of passes through the UAS with scope, irrigation. Also, the following criteria were evaluated before and after procedure:
-
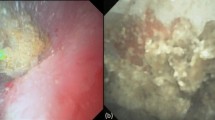
Image quality: evaluated by a picture taken with the endoscope before and after the procedure using the monitor from the manufacturer and rated according to a Likert scale by two independent urologists experienced in endourology.
-
Active deflection: Upward and downward deflections were calculated before and at the end of the procedure by photographing the ureteroscope while completely deflected in both directions (Fig. 2). Two independent urologists experienced in endourology measured the intersection angle between the tangents to the active deflection segment and the deflected tip with a protractor. The final angle values were the mean angle measured by reviewers.
-
Maneuverability: Participants rated the maneuverability on a Likert scale of "bad" to "very good".
No data were captured on stone-free rate or postoperative complications.
Statistical analysis
Qualitative variables were described as numbers and percentage. Quantitative variables were described as median [interquartile range] values. Univariate analysis was conducted using the Fisher’s exact test in case of qualitative explaining variables. The Wilcoxon rank sum test was used for repeated measures. All tests were conducted using the R Software, version 3.2.4. A p value of 0.05 or less was considered significant.
Results
A total of 40 procedures were performed (five per institution) with LithoVue™. The study included 24 men (60 %) and 16 women (40 %). The indication for FURS was treatment of stone disease in 92.5 % of the cases (37/40). Median stone size and density were 104.5 mm2 [60.25; 212.5] and 1034 Hounsfield units [522; 1257], respectively (Table 1). In two cases, the LithoVue™ was unable to reach the target because of a tight ureter in one case and a narrow ureteropelvic junction in the second one. Laser lithotripsy was performed in 30 cases (79 %) and stone basketing without the need for laser lithotripsy in 4 patients (11 %) (Table 2). In one case, no stone was found during the procedure. Diagnostic procedures for upper urinary tract tumor were performed in the remaining 7.5 % of the cases (3/40). Fifty-five percentages of the patients was pre-stented, and an UAS was used in 77.5 % of the procedures (11/13 Fr in 58 %, 10/12 Fr in 22.6 % and 12/14 Fr in 19.4 %).
Two LithoVue™ endoscopes broke during surgery (5 %). One occurred secondarily to high pressure applied on the deflection in a narrow lower calyx (225°). The consequence of this breakage was a loss of visibility and deflection (180°/180°). The second endoscope broken resulted in a spontaneous loss of vision after 39 min of use.
The median energy used was 1 Joule, and the frequency was 10 Hertz. The mean total energy used was 3.67 kV. The median operative time was 40 min [20; 55] (Table 2).
Before LithoVue™ usage, the median measured upward and downward deflections were 270° and 270°, respectively. Image quality was rated as “very good” in 65 % of cases and “good” in 30 %. Maneuverability was “very good” in 77.5 % and “good” in 17.5 % (Table 3).
At the final evaluation, median upward and downward deflections were both 270°. Image quality was still “very good” in 62.5 % of cases and “good” in 30 % with no significant difference compared with preoperative data (p = 0.7). Maneuverability was “very good” in 72.5 % and “good” in 17.5 %, with no significant difference compared with preoperative data as listed in Table 3 (p = 0.92).
Overall performance satisfaction was “very good” in 70 %, “good” in 17.5 % and “acceptable” in 12.5 %.
Discussion
Despite the technological improvements in FURS since the first models, there is still concern regarding their durability. Durability relates also to quality of image and/or deflection and/or torque of ureteroscopes. Several factors can influence the resistance of these instruments including cleaning process, experience of the surgeon and operating room team and type of procedures performed [6, 9, 11, 13, 16, 19, 20]. Recent studies evaluated and compared the durability of the new generation of FURS, either fiberoptic or digital, and a huge variation in time of usage before repair can be noted [9–17]. Concerning the fiberoptic FURS, Knudsen et al. compared four current FURS in 2010: the Wolf Viper, Olympus URF-P5, Gyrus-ACMI DUR-8 Elite (DUR-8E) and Stryker FlexVision U-500 [10]. The average number of cases before a scope was damaged to an extent that repair was needed ranged from an average of 17.3 for the Viper, 17.6 for the FlexVision U-500, 5.3 for the DUR-8E and 18 cases for the URF-P5. The average time of usage before repair was 107.6 min for DUR-8E, 624 min for the FlexVision U-500, 600.3 min for the Viper and 456 min for the URF-P5. Recently, Kramolowsky et al. presented data on the Olympus URF-P5 which needed repair after an average of 21 procedures [12]. With the introduction of digital FURS, an increased durability was expected compared to the fiberoptic endoscopes because of the replacement of fiberoptic bundles. In 2015, Shah et al. prospectively compared the durability and the quality of imaging of two digital FURS: The (CMOS) GyrusACMI/Olympus Invisio DUR-D and the (CCD) URF-V1 obtained an average number of procedures between repair of 11.25 and 14, respectively [15]. Karaolides et al. demonstrated that the overall longevity of the digital FURS Olympus URF-V1 depends on the correct handling of the scopes [12]. With the introduction of thorough guidelines for usage in their clinic, they were able to double the number of uses before damage occurred to the scope (10.6 vs. 21.6 uses). In another study evaluating the digital FURS Olympus URF-V1, the latter needed repair after 59 procedures [21]. Multescu et al. evaluated the use of Flex-XC FURS and found that the average number of cases performed before repair varied from 96 to 159 [14]. Compared to the recent generation of fiberoptic FURS, the digital ureteroscopes did not appear to provide a durability advantage. Furthermore, because of the frequency of FURS repairs, several studies focused on the cost of the procedure. Kramolowsky et al. found an average cost of $7521 per repair and an average cost of repair per procedure of $355 [17]. Another study evaluated direct and indirect costs associated with ureteroscopy, and the authors reported an average cost of $4852 per procedure and a cost of endoscope repair reaching $605 per case [22]. On the other hand, net revenue generated per procedure was $5446. The total cost per procedure was found to be $4470 in the study performed by Cone et al. [23]. For these reasons, as well as the limited availability of repair options for FURS in developing countries, there has been a drive to develop a single-use FURS. Bagley firstly described the concept of a disposable flexible ureteroscope in 1987 with the use of disposable flexible tips [24]. Subsequently, Boylu et al. evaluated in 2009 the SemiFlex™ Scope, a disposable fiberoptic ureteroscope made of a reusable eyepiece and a semiflexible shaft with a 3.3-Fr working channel and deflections in upward and downward directions [25]. They concluded that the SemiFlex™ Scope had acceptable active tip deflection, field of view and flow rate compared to conventional fiberoptic FURS. However, this scope did not gain in popularity, and no further evaluation has been done. The second ureteroscope introduced on the market was the PolyScope™ [26, 27]. This fiberoptic endoscope has a modular design, which allows the repair of individual parts, without disturbing the other components. PolyScope™ is composed of a single-use flexible catheter, reusable 10,000 pixel fiberoptic bundles but only has a unidirectional deflection of 180°. Ding et al. compared this endoscope to the Olympus URF-P5 for the treatment of renal stones and found similar results except for lower pole stones where the URF-P5 had better results [28]. Finally, Cook Medical launched in 2013 the Flexor Vue™ including a one-time-use disposable sheath and a visualization source that may be reused up to ten times with careful handling. However, no evaluation has been published regarding this endoscope.
As the evolution of conventional FURS shifted from fiberoptic to digital technology, disposable FURS has also moved to digital components. The only digital single-use FURS currently available on the market is LithoVue™. Compared to the previous disposable FURS, LithoVue™ does not have a modular design. This endoscope is made of one single-use piece. The present study confirmed that the LithoVue™ performed very well in terms of image quality, active deflection and maneuverability. However, two LithoVue™ endoscopes broke during surgery. Both cases were challenging cases with the need of extreme deflection due to acute infundibulopelvic angles which is also known to severely challenge the durability of reusable FURS. Might reusable FURS have also broken in these situations, resulting in significant repair costs. Did the operators stress the scope more than they would have done usually because it was single use? Did the procedures need to be completed with another scope? Did other LithoVue™ endoscopes break if more complex and longer cases performed in the cohort? The two endoscopes were sent back to the manufacturer in order to analyze the causes of breakage.
Our study has several limitations. We did not compare the LithoVue™ to the current digital FURS, which may impact the robustness of our results. However, this study should be considered a preliminary evaluation of this new endoscope. Furthermore the number of procedures performed was limited, which may affect the number of issues encountered.
With the release of LithoVue™, some questions may be addressed. First of all, what place will LithoVue™ take compared to conventional FURS? As discussed earlier, reusable FURS indeed is fragile instruments that need to be handled carefully. In complex cases where damage to a reusable scope is most likely, such as in patients with calyceal diverticula, non-relocatable large lower pole stones or cases with an acute infundibulopelvic angle, LithoVue™ could be an alternative to conventional FURS. Furthermore, in countries with limited resources where there is limited manpower and where facilities for endoscope repair are limited, LithoVue™ could provide an option to allow FURS. In numerous endourology departments, urologists have access to 1–2 FURS at a time. Since repair and replacement is not always time efficient, the use of the LithoVue™ could be an alternative in such cases. And finally, and importantly reusable FURS can only undergo high-level disinfection (HLD) rather than sterilization between patients. The question of whether this is safe given that there is now an alternative and that the urinary tract, unlike many other body cavities where scopes which undergo HLD are used, is sterile, needs to be further explored [29, 30]. These concerns highlight the need of a cost-effectiveness analysis of LithoVue™ compared to conventional FURS. Furthermore, prospective randomized trials comparing this new single-use FURS with traditional digital FURS are needed to find the place for LithoVue™ in current practice.
Conclusions
This study evaluated the first digital single-use FURS LithoVue™. The endoscope had good image quality, active deflection and maneuverability. Further evaluation of surgical outcomes and cost analysis will help delineate the position of this single-use FURS in current practice.
References
Takayasu H, Aso Y, Takagi T, Go T (1971) Clinical application of fiber-optic pyeloureteroscope. Urol Int 26(2):97–104
Bagley DH, Huffman JL, Lyon ES (1987) Flexible ureteropyeloscopy: diagnosis and treatment in the upper urinary tract. J Urol 138(2):280–285
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T (2016) EAU guidelines on interventional treatment for urolithiasis. Eur Urol 69(3):475–482
de la Rosette J, Denstedt J, Geavlete P, Keeley F, Matsuda T, Pearle M, Preminger G, Traxer O, CROES URS Study Group (2014) The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 28(2):131–139
Afane JS, Olweny EO, Bercowsky E, Sundaram CP, Dunn MD, Shalhav AL, McDougall EM, Clayman RV (2000) Flexible ureteroscopes: a single center evaluation of the durability and function of the new endoscopes smaller than 9Fr. J Urol 164(4):1164–1168
Pietrow PK, Auge BK, Delvecchio FC, Silverstein AD, Weizer AZ, Albala DM, Preminger GM (2002) Techniques to maximize flexible ureteroscope longevity. Urology 60(5):784–788
Monga M, Best S, Venkatesh R, Ames C, Lee C, Kuskowski M, Schwartz S, Vanlangendock R, Skenazy J, Landman J (2006) Durability of flexible ureteroscopes: a randomized, prospective study. J Urol 176(1):137–141
Traxer O, Dubosq F, Jamali K, Gattegno B, Thibault P (2006) New-generation flexible ureterorenoscopes are more durable than previous ones. Urology 68(2):276–279
Carey RI, Gomez CS, Maurici G, Lynne CM, Leveillee RJ, Bird VG (2006) Frequency of ureteroscope damage seen at a tertiary care center. J Urol 176(2):607–610
Knudsen B, Miyaoka R, Shah K, Holden T, Turk TM, Pedro RN, Kriedberg C, Hinck B, Ortiz-Alvarado O, Monga M (2010) Durability of the next-generation flexible fiberoptic ureteroscopes: a randomized prospective multi-institutional clinical trial. Urology 75(3):534–538
Defidio L, De Dominicis M, Di Gianfrancesco L, Fuchs G, Patel A (2012) Improving flexible ureterorenoscope durability up to 100 procedures. J Endourol 26(10):1329–1334
Karaolides T, Bach C, Kachrilas S, Goyal A, Masood J, Buchholz N (2013) Improving the durability of digital flexible ureteroscopes. Urology 81(4):717–722
Carey RI, Martin CJ, Knego JR (2014) Prospective evaluation of refurbished flexible ureteroscope durability seen in a large public tertiary care center with multiple surgeons. Urology 84(1):42–45
Multescu R, Geavlete B, Georgescu D, Geavlete P (2014) Improved durability of flex-Xc digital flexible ureteroscope: how long can you expect it to last? Urology 84(1):32–35
Shah K, Monga M, Knudsen B (2015) Prospective randomized trial comparing 2 flexible digital ureteroscopes: aCMI/Olympus invisio DUR-D and Olympus URF-V. Urology 85(6):1267–1271
Landman J, Lee DI, Lee C, Monga M (2003) Evaluation of overall costs of currently available small flexible ureteroscopes. Urology 62(2):218–222
Kramolowsky E, McDowell Z, Moore B, Booth B, Wood N (2016) Cost analysis of flexible ureteroscope repairs: evaluation of 655 procedures in a community-based practice. J Endourol 30(3):254–256
Semins MJ, George S, Allaf ME, Matlaga BR (2009) Ureteroscope cleaning and sterilization by the urology operating room team: the effect on repair costs. J Endourol 23(6):903–905
Sung JC, Springhart WP, Marguet CG, L’Esperance JO, Tan YH, Albala DM, Preminger GM (2005) Location and etiology of flexible and semirigid ureteroscope damage. Urology 66(5):958–963
Abraham JB, Abdelshehid CS, Lee HJ, Box GN, Deane LA, Le T, Jellison F, Borin JF, Manipon A, McDougall EM, Clayman RV (2007) Rapid communication: effects of steris 1 sterilization and Cidex ortho-phthalaldehyde high-level disinfection on durability of new-generation flexible ureteroscopes. J Endourol 21(9):985–992
Al-Qahtani SM, Geavlete B, de Medina SG, Traxer OP (2011) The new Olympus digital flexible ureteroscope (URF-V): initial experience. Urol Ann 3(3):133–137
Tosoian JJ, Ludwig W, Sopko N, Mullins JK, Matlaga BR (2015) The effect of repair costs on the profitability of a ureteroscopy program. J Endourol 29(4):406–409
Cone EB, Eisner BH, Ursiny M, Pareek G (2014) Cost-effectiveness comparison of renal calculi treated with ureteroscopic laser lithotripsy versus shockwave lithotripsy. J Endourol 28(6):639–643
Bagley DH (1987) Flexible ureteropyeloscopy with modular, “disposable” endoscope. Urology 29(3):296–300
Boylu U, Oommen M, Thomas R, Lee BR (2009) In vitro comparison of a disposable flexible ureteroscope and conventional flexible ureteroscopes. J Urol 182(5):2347–2351
Bader MJ, Gratzke C, Walther S, Schlenker B, Tilki D, Hocaoglu Y, Sroka R, Stief CG, Reich O (2010) The Polyscope: a modular design, semidisposable flexible ureterorenoscope system. J Endourol 24(7):1061–1066
Bansal H, Swain S, Sharma GK, Mathanya M, Trivedi S, Dwivedi US, Singh PB (2011) Polyscope: a new era in flexible ureterorenoscopy. J Endourol 25(2):317–321
Ding J, Xu D, Cao Q, Huang T, Zhu Y, Huang K, Chen Y, Liang C, Qi J, Huang Y (2015) Comparing the efficacy of a multimodular flexible ureteroscope with its conventional counterpart in the management of renal stones. Urology 86(2):224–229
Noronha AM, Brozak S (2014) A 21st century nosocomial issue with endoscopes. BMJ 19(348):g2047
Chang CL, Su LH, Lu CM, Tai FT, Huang YC, Chang KK (2013) Outbreak of ertapenem-resistant Enterobacter cloacae urinary tract infections due to a contaminated ureteroscope. J Hosp Infect 85(2):118–124
Acknowledgments
The authors would like to thank Boston Scientific for providing LithoVue endoscopes in each center in order to evaluate its performance.
Authors’ contribution
Doizi contributed to protocol/project development, data collection or management, data analysis and manuscript writing/editing; Kamphuis contributed to protocol/project development, data collection or management, data analysis and manuscript writing/editing; Giusti contributed to protocol/project development, data collection or management and manuscript writing/editing; Knoll contributed to protocol/project development, data collection or management and manuscript writing/editing; Osther contributed to protocol/project development, data collection or management and manuscript writing/editing; Scoffone contributed to protocol/project development, data collection or management and manuscript writing/editing; Pérez Fentes contributed to protocol/project development, data collection or management and manuscript writing/editing; Proietti contributed to protocol/project development, data collection or management and manuscript writing/editing; Wiseman contributed to protocol/project development, data collection or management and manuscript writing/editing; de la Rosette contributed to protocol/project development, data collection or management and manuscript writing/editing; and Traxer contributed to protocol/project development, data collection or management and manuscript writing/editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Steeve Doizi, None; Guido Kamphuis, None; Guido Giusti, Boston Scientific, Coloplast, Cook Medical, Olympus, Karl Storz, Rocamed; Thomas Knoll, Boston Scientific, Palle Jörn Osther, Boston Scientific, Coloplast, Olympus, Karl Storz; Cesare Scoffone, Boston Scientific, Coloplast, Cook Medical, Lumenis, Karl Storz; Daniel Pérez-Fentes, Boston Scientific, Coloplast; Silvia Proietti, None; Oliver Wiseman, Boston Scientific, Coloplast, EMS, Olympus; Jean de la Rosette, Boston Scientific, Coloplast, Olympus, Karl Storz; Olivier Traxer, Boston Scientific, Coloplast, Lumenis, Olympus, Rocamed.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.”
Informed consent
“Informed consent was obtained from all individual participants included in the study.”
Additional information
Steeve Doizi and Guido Kamphuis have contributed equally.
Appendix: Checklist used during each procedure for LithoVue™ evaluation
Appendix: Checklist used during each procedure for LithoVue™ evaluation


.
Rights and permissions
About this article
Cite this article
Doizi, S., Kamphuis, G., Giusti, G. et al. First clinical evaluation of a new single-use flexible ureteroscope (LithoVue™): a European prospective multicentric feasibility study. World J Urol 35, 809–818 (2017). https://doi.org/10.1007/s00345-016-1936-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1936-x