Abstract
Microtubules, highly dynamic components of the cytoskeleton, participate in diverse cellular activities such as mitosis, cell migration, and intracellular trafficking. Dysregulation of microtubule dynamics contributes to the development of serious diseases, including cancer. The dynamic properties and functions of microtubule network are regulated by microtubule-associated proteins. Paclitaxel, an anti-microtubule agent of the taxane family, has shown a success in clinical treatment of many cancer patients. However, the variable response activity of patients and acquired resistance to paclitaxel limit the clinical use of the drug. Accumulating studies show that microtubule-associated proteins can regulate paclitaxel sensitivity in a wide range of cancer types. In this review, we will describe the roles of various microtubule-associated proteins in the regulation of paclitaxel in cancers. Particularly, we will focus on the modulation of centrosomal proteins in paclitaxel resistance. Improved understandings of how these proteins act might predict treatment responses and provide insights into more rational chemotherapeutic regimens in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As one of the major components of the cytoskeleton, microtubules are key players in cellular processes such as cell migration, intracellular trafficking, and DNA segregation during mitosis [1, 2]. Microtubules are assembled from 13 laterally associating protofilaments, which in turn consist of α- and β-tubulin heterodimers aligned in a head-to-tail pattern (Fig. 1a). The alignment of α- and β-tubulin heterodimers leads to the polarity of the microtubule, with β-tubulin exposed at one end (plus end) and α-tubulin exposed at the other end (minus end) [1]. In most mammalian cells, the minus ends of microtubules are clustered at microtubule organizing centers, while the plus ends face the cell cortex [3]. Most microtubules in the cells are in consistent transitions between growth and shrinkage by associating and dissociating of α/β-tubulin heterodimers at both ends, which is known as dynamic instability (Fig. 1b) [4]. The highly dynamic properties of microtubules are essential for many cellular activities, particularly cell division [1]. Mounting evidence shows that dysregulation of microtubule dynamics contributes to the development of serious diseases, including cancer [5,6,7,8].
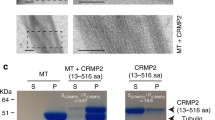
a A schematic illustration showing that microtubule dynamics are regulated by different types of MAPs, including canonical MAPs, microtubule plus-end-tracking proteins, centrosomal proteins, microtubule motor proteins, etc. The action of paclitaxel in the microtubule network occurs through binding to β-tubulin. b, c HeLa cells were stained with anti-tubulin antibody, and then with fluorescein-conjugated secondary antibodies. b Microtubules are highly dynamic structures and undergo frequent transitions between growth and shrinkage, a phenomenon known as dynamic instability. c Paclitaxel promotes microtubule assembly and disrupts microtubule dynamics
Vinca alkaloids and taxanes are two families of anti-microtubule agents wildly used in clinical treatment of cancer including solid tumors and hematological malignancies [9]. Paclitaxel, a member of the taxane family, is a natural alkaloid originally isolated from the bark of a tree, Taxus brevifolia. The anti-tumoral activity of paclitaxel was discovered in the 1970s and it was first approved by the US FDA in 1992 for treatment of ovarian cancer. In addition, paclitaxel has proven to be effective in other solid tumors, including breast cancer and non-small-cell lung cancer [10, 11]. Preliminary mechanism showed that paclitaxel acts by stabilizing cellular microtubules and blocking chromosome segregation (Fig. 1c) [12]. Moreover, it is established that the action of paclitaxel in the microtubule network occurs through interaction with β-tubulin. In the following years, β-tubulin functional domains and the domains containing paclitaxel-binding sites were identified [13].
Despite the great success of paclitaxel, the variable response activity of patients to the drug limits its clinical utility. Acquired resistance to paclitaxel is one of the most significant reasons for its failure in chemotherapy [14]. Previous studies have demonstrated that paclitaxel resistance is attributable to various mechanisms: elevated drug efflux that results from upregulation of membrane transporters such as P-glycoprotein [15, 16]; alterations in the expression of β-tubulin isotypes [17]; and changes in apoptotic regulatory proteins such as Bcl-2 [18,19,20]. In spite of decades of great efforts worldwide, the precise mechanisms underlying paclitaxel activity remain largely unknown. In this review, we will focus on the roles of MAPs (microtubule-associated proteins) in regulation of paclitaxel activity in different types of cancers. Elucidation of these issues might provide significant diagnostic or prognostic value, as well as potential targets for cancer chemotherapy. We categorize MAPs into canonical MAPs, plus-end-binding proteins, centrosomal proteins, and other proteins that might affect the properties and functions of microtubule, and detail their roles in the regulation of paclitaxel activity.
Distinct roles of MAPs in paclitaxel activity regulation
MAPs represent a large number of proteins that act in concert with the microtubule network, and regulate microtubule properties and functions [21,22,23,24]. Canonical MAPs are structural MAPs, such as MAP2 and tau. MAPs regulate microtubule behavior by binding microtubules either at the microtubule ends or on the outside of the microtubule wall or interacting with the soluble tubulin pool (Fig. 1c) [25, 26]. MAPs participate in various microtubule-mediated cellular activities by modulating microtubule behavior such as stability, assembly or bundling [21, 26, 27]. Accumulating evidence shows that changes in the expression or post-translational modification of MAPs lead to the alteration of microtubule dynamics, and are associated with the development of serious diseases including cancer [5, 6, 28, 29]. The dysregulation of microtubule dynamics by MAPs may result in tumor resistance to chemotherapeutic agents that target microtubules, and many MAPs with aberrant expression have been shown to be correlated with susceptibility to paclitaxel [30, 31].
Tau, a microtubule-associated protein, promotes tubulin polymerization and stabilizes microtubules [32]. It is well known that tau plays an essential role in the regulation of nervous system, and is significantly involved in the pathogenesis of Alzheimer’s disease as well as the tauopathies [33]. Overphosphorylation of tau, mainly occurring in the axons, contributes to neurofibrillary degeneration and is associated with cell dysfunction and death. Tau binds to β-tubulin in the same site as paclitaxel, and consequently competes with the drug. An in vitro study shows that preincubation of tubulin with Tau decreases paclitaxel binding and reduces paclitaxel-induced microtubule polymerization in breast cancer cell line [30, 34]. In addition, high expression of Tau shows a significant association with poor response to paclitaxel chemotherapy in patients with metastatic breast cancer [35]. Moreover, reduction of Tau expression sensitizes ovarian carcinoma to the paclitaxel treatment [36]. These studies show that Tau expression may act as a predictor of response to paclitaxel in cancer patients.
MAP2 overexpression has been observed in several types of cancers [37,38,39,40,41]. Similar to tau, MAP2 also binds to and stabilizes microtubules. However, they regulate paclitaxel activity of cancer cells via different mechanisms. Increased expression of MAP2 in breast cancer cell lines leads to increased paclitaxel sensitivity [42]. Gene expression analysis shows that the expression level of MAP2 is significantly higher in breast cancer patients achieving a pathologic complete response to neoadjuvant paclitaxel with radiation, indicating that patients with elevated MAP2 expression might show a better response to paclitaxel treatment. Moreover, MAP7 domain-containing protein 3 (Mdp3), a microtubule binding protein, has been shown to be involved in breast cancer growth and metastasis [7]. Besides, Mdp3 promotes microtubule assembly and stability by interacting with tubulin and microtubules [43]. It will be interesting to investigate the role of Mdp3 in paclitaxel activity modulation in cancers, which might be a novel predicting target in cancer chemotherapy.
Microtubule plus-end-binding proteins that promote paclitaxel sensitivity
Microtubule plus-end-binding proteins (+TIPs) localize to the growing plus ends of microtubules and couple microtubules to cellular structures, such as chromosomes and cell cortex [44, 45]. Microtubule plus-end-binding proteins regulate microtubule dynamics and functions. Amounting studies have emphasized the central role of end-binding family proteins (EB) among the +TIPs [45,46,47,48,49]. Mammals contain three EBs (EB1-3), sharing 57–66% sequence identity, are encoded by various genes [50]. EB proteins bind directly to the growing microtubule plus ends via their N-terminal calponin homology domain, whereas their C terminus is important for associating with other +TIPs [51]. Among EB family proteins, EB1 and EB3 promote microtubule assembly and stabilization [52]. Interestingly, EB1 and EB3 sensitize microtubules to microtubule-targeting agents by regulation of microtubule dynamics [53,54,55].
It is recently reported that the expression of EB1 in breast tumor tissues correlates with the clinical response of the patients to paclitaxel-based chemotherapy [56]. Mechanistic study has showed that EB1 increases paclitaxel activity to cause mitotic arrest and apoptosis in breast cancer cell lines. In addition, EB1 stimulates paclitaxel sensitivity by promoting paclitaxel-microtubule association, thus increasing the activity of paclitaxel to enhance microtubule assembly and stabilization. It is also proved in other studies that EB1 is crucial for regulating the sensitivity of breast cancer cells to paclitaxel, through a mechanism in which it modulates paclitaxel-mediated stabilization of microtubule polymerization and regulates the binding sites of paclitaxel at the growing microtubule ends [57].
Cytoplasmic linker protein 170 (CLIP-170) is another member of the +TIPs family that binds to microtubule plus ends in an EB1-dependent manner [58]. CLIP-170 is regarded as a mediator of paclitaxel sensitivity in breast cancers [31]. The expression of CLIP-170 in breast cancer samples correlates with the pathological response of tumors to paclitaxel-containing chemotherapy. Similar to EB1, CLIP-170 regulates paclitaxel sensitivity in breast cancer cells by modulating the effects of paclitaxel on microtubule assembly, thus affecting cell-cycle retention and apoptosis.
Centrosomal proteins that modulate paclitaxel resistance
Centrosomes, the microtubule organizing centers, nucleate and organize microtubules in animal cells [59]. Centrosome is critical for cell cycle progression, by organizing radial microtubule array in interphase and establishing bipolar spindle during mitosis [3, 60, 61]. Centrosomes undergo maturation and segregation during the cell cycle, and centrosome abnormalities, such as supernumerary centrioles, abnormal centrosome number or volume, and altered expression of centrosomal proteins, have been implicated in tumorigenesis [62,63,64,65,66]. Overall, centrosome aberrations are positively associated with advanced cancer grade and metastasis [67]. It is implied that centrosome abnormalities may have clinical diagnostic and/or prognostic value and centrosomes may also be a potential target for cancer therapy. The correlation between centrosome protein expression and sensitivity to paclitaxel has attracted increasing attention in the field [68,69,70].
Ninein-like protein (Nlp), an important centrosomal protein involved in centrosome maturation, microtubule nucleation, and spindle formation, plays an essential role in tumorigenesis [71]. Nlp is found to be overexpressed in human breast, lung and ovarian carcinomas [72,73,74]. A study has investigated the correlation between Nlp and paclitaxel chemosensitivity, and found that overexpression of Nlp confers breast carcinoma resistance to paclitaxel [72]. By suppressing paclitaxel-induced microtubule polymerization, Nlp overexpression promotes mitotic arrest and suppresses apoptosis elicited by paclitaxel. Moreover, the expression of Nlp in breast cancer patients is highly correlated with their sensitivity to paclitaxel, and patients with high expression of Nlp are likely resistant to the treatment of paclitaxel.
The mammalian transforming acidic coiled coil (TACC) family of centrosomal proteins consists of three members (TACC1-3), which act as important structural components of the mitotic spindle apparatus [75]. TACC proteins are evolutionarily conserved and modulate centrosome integrity, microtubule assembly, and mitotic spindle stability [76,77,78,79]. Mounting evidences indicate that TACCs are involved in the progression of some human malignancies [80]. The expression of TACC1 has been shown to be upregulated in human cancer cell lines, and it is associated with mammary tumorigenesis and gastric carcinoma [81, 82]. TACC2 plays an important role in breast cancer cell proliferation, and its immunohistochemical status might be a candidate of worse prognostic factor in breast cancer cases [83]. Abnormal expression of TACC3 is associated with the etiology of ovarian, bladder and non-small-cell lung cancer [84,85,86]. Knockdown of TACC3 leads to breast cancer cell arrest in G1 through cellular senescence by increasing nuclear p21WAF and reducing retinoblastoma protein (Rb) and extracellular signal-regulated kinase 1/2 (ERK1/2) [87]. Treatment of breast cancer cells with a low concentration of paclitaxel promotes cellular senescence triggered upon TACC3 depletion, showing that blocking of TACC3 regulates paclitaxel sensitivity by modulating a premature senescence program.
Another centrosomal protein, Salt Inducible Kinase 2 (SIK2) has been identified as cell cycle regulator of ovarian cancer cells in a high-content siRNA kinome screen [88]. SIK2 plays a key role in the initiation of mitosis and regulates the localization of the centrosome linker protein, C-Nap1 [89, 90]. Depletion of SIK2 expression induces centrosome splitting in interphase, while it inhibits centrosome separation in mitosis, thus sensitizing ovarian cancers to paclitaxel both in ovarian cancer cells and xenografts. Compared to paclitaxel-sensitive ovarian cancers, the expression of SIK2 is significantly higher in paclitaxel-resistant cancers. These findings imply that SIK2 might be a therapeutic target in ovarian cancers. Centrosomal protein 70 (Cep70) is an important factor that mediates breast cancer growth and metastasis. The expression of Cep70 is upregulated in breast cancer tissues and cell lines, which is closely correlated with several clinicopathologic variables associated with breast cancer progression [8]. It has been shown that Cep70 participates in microtubule polymerization and stability, as well as mitotic spindle orientation [91,92,93,94]. Elucidation of the correlation of Cep70 expression with paclitaxel activity in breast cancer will improve the understanding of the role of centrosomal proteins in cancer chemotherapy [95].
Regulation of paclitaxel activity by other MAPs including spindle assembly checkpoint and microtubule motor proteins
Chromosome instability and aneuploidy are hallmarks of aggressive solid tumors [96, 97]. The spindle assembly checkpoint (SAC) has a crucial function in genetic integrity, which ensures accurate chromosome segregation during mitosis and prevents aneuploidy [98]. Impaired SAC function has been suggested as one of the causes of aneuploidy in human cancers [99]. SAC is a complex of proteins that includes Mad1, Mad2, Bub1, BubR1, Bub3, and MPS1 [100]. Among all SAC components, Mad2 and BubR1 have a pivotal function in checkpoint signaling due to their crucial function in the metaphase-to-anaphase transition by delaying anaphase onset, through inhibition of the anaphase promoting complex/cyclosome (APC/C) [101].
Recent studies have shown that paclitaxel sensitivity is associated with the spindle checkpoint. It has been reported that Mad2 downregulation induces premature senescence in breast cancer cells, and these senescence cells maintain viability, while replicative incompetent [101]. The paclitaxel treatment in Mad2-depleted cells shows a significant further induction of senescence compared with paclitaxel controls, indicating that compromised Mad2 levels lead to paclitaxel resistance of senescent breast cancer cells. Besides, Mad2 and BubR1 are significantly expressed in gastric cancer cells, and contribute to cellular transformation and tumorigenesis [102]. Similarly, paclitaxel treatment increased cell senescence in gastric cancer cells interfered for Mad2 or BubR1 expression. Intriguingly, it is found that reduced expression of BubR1, but not Mad2, is associated with acquired paclitaxel resistance in ovarian carcinoma cells [103].
Another type of key participants during mitosis is kinesin superfamily protein (KIF), which plays crucial roles in chromosomal and spindle movements [104]. KIFs are a conserved class of motor proteins that transport cargoes by walking unidirectionally along microtubule tracks, hydrolyzing one molecule of ATP at each step [105]. KIFs are implicated in a variety of cellular functions, such as mitosis, signal transduction, microtubule polymer dynamics, and intracellular transport [106]. Previous studies suggest that KIFs may play a key role in the development or progression in many types of cancers [107,108,109]. Kinesins have also gained attentions as potential targets for mitotic drugs. It is reported that overexpression of kinesin proteins, including KIFC3, KIF5A, and KIF12 contributes to paclitaxel resistance in BLBC (basal-like breast cancer) cell lines and tissues [110]. Moreover, the expression level of KIF14 is significantly increased in cervical cancer tissues, which is positively correlated with high-tumor stage, lymph node metastasis, paclitaxel chemoresistance as well as poor survival [111]. These findings indicate that KIF14 might serve as a novel prognostic biomarker of chemoresistance to paclitaxel treatment in cervical cancer (Table 1).
Conclusion
In spite of the development of small-molecule pathway inhibitors, chemotherapy remains the treatment of primary choice for patients with cancer. Paclitaxel, a member of the taxane family, has gained some success in treating some solid tumors including breast cancer and non-small-cell lung cancer. However, the variable response activity of patients and acquired resistance to paclitaxel limit its clinical utility. It is outlined in the review that some MAPs promote paclitaxel sensitivity by regulating microtubule dynamics. Altering the expression of these proteins might promote the effects of paclitaxel on microtubule dynamics and contribute to a synergistic inhibition of cancer cell proliferation. Moreover, the expression level of several centrosomal proteins is upregulated in cancer, which confers resistance to the treatment of paclitaxel. In summary, these proteins might act as potential markers to predict response to paclitaxel, as well as be regulated to boost paclitaxel sensitivity. These findings not only provide theoretical evidence into more rational chemotherapeutic regimens in clinical practice but also novel insights into precision cancer treatment.
Abbreviations
- MAPs:
-
Microtubule-associated proteins
- EB:
-
End-binding family protein
- CLIP-170:
-
Cytoplasmic linker protein 170
- Nlp:
-
Ninein-like protein
- TACC:
-
Transforming acidic coiled coil
- Rb:
-
Retinoblastoma protein
- ERK1/2:
-
Extracellular signal-regulated kinase 1/2
- SIK2:
-
Salt Inducible Kinase 2
- Cep70:
-
Centrosomal protein 70
- SAC:
-
Spindle assembly checkpoint
- APC/C:
-
Anaphase promoting complex/cyclosome
- KIF:
-
Kinesin superfamily protein
- BLBC:
-
Basal-like breast cancer
References
Desai A, Mitchison TJ (1997) Microtubule polymerization dynamics. Annu Rev Cell Dev Biol 13:83–117. doi:10.1146/annurev.cellbio.13.1.83
McIntosh JR, Grishchuk EL, West RR (2002) Chromosome-microtubule interactions during mitosis. Annu Rev Cell Dev Biol 18:193–219. doi:10.1146/annurev.cellbio.18.032002.132412
Doxsey S, Zimmerman W, Mikule K (2005) Centrosome control of the cell cycle. Trends Cell Biol 15(6):303–311. doi:10.1016/j.tcb.2005.04.008
Kirschner MW, Mitchison T (1986) Microtubule dynamics. Nature 324(6098):621. doi:10.1038/324621a0
Bhat KM, Setaluri V (2007) Microtubule-associated proteins as targets in cancer chemotherapy. Clin Cancer Res 13(10):2849–2854. doi:10.1158/1078-0432.CCR-06-3040
Liu M, Wang X, Yang Y, Li D, Ren H, Zhu Q, Chen Q, Han S, Hao J, Zhou J (2010) Ectopic expression of the microtubule-dependent motor protein Eg5 promotes pancreatic tumourigenesis. J Pathol 221(2):221–228. doi:10.1002/path.2706
Tala Xie S, Sun X, Sun X, Ran J, Zhang L, Li D, Liu M, Bao G, Zhou J (2014) Microtubule-associated protein Mdp3 promotes breast cancer growth and metastasis. Theranostics 4(10):1052–1061. doi:10.7150/thno.9727
Shi X, Li D, Wang Y, Liu S, Qin J, Wang J, Ran J, Zhang Y, Huang Q, Liu X, Zhou J, Liu M (2017) Discovery of centrosomal protein 70 as an important player in the development and progression of breast cancer. Am J Pathol 187(3):679–688. doi:10.1016/j.ajpath.2016.11.005
Barok M, Joensuu H, Isola J (2014) Trastuzumab emtansine: mechanisms of action and drug resistance. Breast Cancer Res BCR 16(2):209. doi:10.1186/bcr3621
Rowinsky EK, Donehower RC (1995) Paclitaxel (taxol). N Engl J Med 332(15):1004–1014. doi:10.1056/NEJM199504133321507
Rowinsky EK, Eisenhauer EA, Chaudhry V, Arbuck SG, Donehower RC (1993) Clinical toxicities encountered with paclitaxel (Taxol). Semin Oncol 20(4 Suppl 3):1–15
Manfredi JJ, Horwitz SB (1984) Vinblastine paracrystals from cultured cells are calcium-stable. Exp Cell Res 150(1):205–212
Nogales E, Wolf SG, Downing KH (1998) Structure of the alpha beta tubulin dimer by electron crystallography. Nature 391(6663):199–203. doi:10.1038/34465
Yusuf RZ, Duan Z, Lamendola DE, Penson RT, Seiden MV (2003) Paclitaxel resistance: molecular mechanisms and pharmacologic manipulation. Curr Cancer Drug Targets 3(1):1–19
Huang Y, Ibrado AM, Reed JC, Bullock G, Ray S, Tang C, Bhalla K (1997) Co-expression of several molecular mechanisms of multidrug resistance and their significance for paclitaxel cytotoxicity in human AML HL-60 cells. Leukemia 11(2):253–257
Jang SH, Wientjes MG, Au JL (2001) Kinetics of P-glycoprotein-mediated efflux of paclitaxel. J Pharmacol Exp Ther 298(3):1236–1242
Mozzetti S, Ferlini C, Concolino P, Filippetti F, Raspaglio G, Prislei S, Gallo D, Martinelli E, Ranelletti FO, Ferrandina G, Scambia G (2005) Class III beta-tubulin overexpression is a prominent mechanism of paclitaxel resistance in ovarian cancer patients. Clin Cancer Res 11(1):298–305
Gazitt Y, Rothenberg ML, Hilsenbeck SG, Fey V, Thomas C, Montegomrey W (1998) Bcl-2 overexpression is associated with resistance to paclitaxel, but not gemcitabine, in multiple myeloma cells. Int J Oncol 13(4):839–848
Liu JR, Fletcher B, Page C, Hu C, Nunez G, Baker V (1998) Bcl-xL is expressed in ovarian carcinoma and modulates chemotherapy-induced apoptosis. Gynecol Oncol 70(3):398–403. doi:10.1006/gyno.1998.5125
Panvichian R, Orth K, Day ML, Day KC, Pilat MJ, Pienta KJ (1998) Paclitaxel-associated multimininucleation is permitted by the inhibition of caspase activation: a potential early step in drug resistance. Can Res 58(20):4667–4672
Amos LA, Schlieper D (2005) Microtubules and maps. Adv Protein Chem 71:257–298. doi:10.1016/S0065-3233(04)71007-4
Yang Y, Liu M, Li D, Ran J, Gao J, Suo S, Sun SC, Zhou J (2014) CYLD regulates spindle orientation by stabilizing astral microtubules and promoting dishevelled-NuMA-dynein/dynactin complex formation. Proc Natl Acad Sci USA 111(6):2158–2163. doi:10.1073/pnas.1319341111
Gao J, Huo L, Sun X, Liu M, Li D, Dong JT, Zhou J (2008) The tumor suppressor CYLD regulates microtubule dynamics and plays a role in cell migration. J Biol Chem 283(14):8802–8809. doi:10.1074/jbc.M708470200
Li D, Gao J, Yang Y, Sun L, Suo S, Luo Y, Shui W, Zhou J, Liu M (2014) CYLD coordinates with EB1 to regulate microtubule dynamics and cell migration. Cell Cycle 13(6):974–983. doi:10.4161/cc.27838
Etienne-Manneville S (2010) From signaling pathways to microtubule dynamics: the key players. Curr Opin Cell Biol 22(1):104–111. doi:10.1016/j.ceb.2009.11.008
Simeonov DR, Kenny K, Seo L, Moyer A, Allen J, Paluh JL (2009) Distinct Kinesin-14 mitotic mechanisms in spindle bipolarity. Cell Cycle 8(21):3571–3583. doi:10.4161/cc.8.21.9970
Glotzer M (2009) The 3Ms of central spindle assembly: microtubules, motors and MAPs. Nat Rev Mol Cell Biol 10(1):9–20. doi:10.1038/nrm2609
Sun L, Gao J, Dong X, Liu M, Li D, Shi X, Dong JT, Lu X, Liu C, Zhou J (2008) EB1 promotes Aurora-B kinase activity through blocking its inactivation by protein phosphatase 2A. Proc Natl Acad Sci USA 105(20):7153–7158. doi:10.1073/pnas.0710018105
Dong X, Liu F, Sun L, Liu M, Li D, Su D, Zhu Z, Dong JT, Fu L, Zhou J (2010) Oncogenic function of microtubule end-binding protein 1 in breast cancer. J Pathol 220(3):361–369. doi:10.1002/path.2662
Rouzier R, Rajan R, Wagner P, Hess KR, Gold DL, Stec J, Ayers M, Ross JS, Zhang P, Buchholz TA, Kuerer H, Green M, Arun B, Hortobagyi GN, Symmans WF, Pusztai L (2005) Microtubule-associated protein tau: a marker of paclitaxel sensitivity in breast cancer. Proc Natl Acad Sci USA 102(23):8315–8320. doi:10.1073/pnas.0408974102
Sun X, Li D, Yang Y, Ren Y, Li J, Wang Z, Dong B, Liu M, Zhou J (2012) Microtubule-binding protein CLIP-170 is a mediator of paclitaxel sensitivity. J Pathol 226(4):666–673. doi:10.1002/path.3026
Drechsel DN, Hyman AA, Cobb MH, Kirschner MW (1992) Modulation of the dynamic instability of tubulin assembly by the microtubule-associated protein tau. Mol Biol Cell 3(10):1141–1154
Robert M, Mathuranath PS (2007) Tau and tauopathies. Neurol India 55(1):11–16
Wagner P, Wang B, Clark E, Lee H, Rouzier R, Pusztai L (2005) Microtubule Associated Protein (MAP)-Tau: a novel mediator of paclitaxel sensitivity in vitro and in vivo. Cell Cycle 4(9):1149–1152. doi:10.4161/cc.4.9.2038
Tanaka S, Nohara T, Iwamoto M, Sumiyoshi K, Kimura K, Takahashi Y, Tanigawa N (2009) Tau expression and efficacy of paclitaxel treatment in metastatic breast cancer. Cancer Chemother Pharmacol 64(2):341–346. doi:10.1007/s00280-008-0877-5
Gurler H, Yu Y, Choi J, Kajdacsy-Balla AA, Barbolina MV (2015) Three-dimensional collagen type I matrix up-regulates nuclear isoforms of the microtubule associated protein tau implicated in resistance to paclitaxel therapy in ovarian carcinoma. Int J Mol Sci 16(2):3419–3433. doi:10.3390/ijms16023419
Blumcke I, Muller S, Buslei R, Riederer BM, Wiestler OD (2004) Microtubule-associated protein-2 immunoreactivity: a useful tool in the differential diagnosis of low-grade neuroepithelial tumors. Acta Neuropathol 108(2):89–96. doi:10.1007/s00401-004-0873-8
Chen JY, Chang YL, Yu YC, Chao CC, Kao HW, Wu CT, Lin WC, Ko JY, Jou YS (2004) Specific induction of the high-molecular-weight microtubule-associated protein 2 (hmw-MAP2) by betel quid extract in cultured oral keratinocytes: clinical implications in betel quid-associated oral squamous cell carcinoma (OSCC). Carcinogenesis 25(2):269–276. doi:10.1093/carcin/bgh006
Liu Y, Mangini J, Saad R, Silverman AR, Abell E, Tung MY, Graner SR, Silverman JF (2003) Diagnostic value of microtubule-associated protein-2 in Merkel cell carcinoma. Appl Immunohistochem Mol Morphol AIMM 11(4):326–329
Liu Y, Sturgis CD, Grzybicki DM, Jasnosz KM, Olson PR, Tong M, Dabbs DD, Raab SS, Silverman JF (2001) Microtubule-associated protein-2: a new sensitive and specific marker for pulmonary carcinoid tumor and small cell carcinoma. Mod Pathol 14(9):880–885. doi:10.1038/modpathol.3880406
Soltani MH, Pichardo R, Song Z, Sangha N, Camacho F, Satyamoorthy K, Sangueza OP, Setaluri V (2005) Microtubule-associated protein 2, a marker of neuronal differentiation, induces mitotic defects, inhibits growth of melanoma cells, and predicts metastatic potential of cutaneous melanoma. Am J Pathol 166(6):1841–1850. doi:10.1016/S0002-9440(10)62493-5
Bauer JA, Chakravarthy AB, Rosenbluth JM, Mi D, Seeley EH, De Matos Granja-Ingram N, Olivares MG, Kelley MC, Mayer IA, Meszoely IM, Means-Powell JA, Johnson KN, Tsai CJ, Ayers GD, Sanders ME, Schneider RJ, Formenti SC, Caprioli RM, Pietenpol JA (2010) Identification of markers of taxane sensitivity using proteomic and genomic analyses of breast tumors from patients receiving neoadjuvant paclitaxel and radiation. Clin Cancer Res 16(2):681–690. doi:10.1158/1078-0432.CCR-09-1091
Sun X, Shi X, Liu M, Li D, Zhang L, Liu X, Zhou J (2011) Mdp3 is a novel microtubule-binding protein that regulates microtubule assembly and stability. Cell Cycle 10(22):3929–3937. doi:10.4161/cc.10.22.18106
Howard J, Hyman AA (2003) Dynamics and mechanics of the microtubule plus end. Nature 422(6933):753–758. doi:10.1038/nature01600
Akhmanova A, Steinmetz MO (2008) Tracking the ends: a dynamic protein network controls the fate of microtubule tips. Nat Rev Mol Cell Biol 9(4):309–322. doi:10.1038/nrm2369
Honnappa S, Okhrimenko O, Jaussi R, Jawhari H, Jelesarov I, Winkler FK, Steinmetz MO (2006) Key interaction modes of dynamic +TIP networks. Mol Cell 23(5):663–671. doi:10.1016/j.molcel.2006.07.013
Komarova Y, Lansbergen G, Galjart N, Grosveld F, Borisy GG, Akhmanova A (2005) EB1 and EB3 control CLIP dissociation from the ends of growing microtubules. Mol Biol Cell 16(11):5334–5345. doi:10.1091/mbc.E05-07-0614
Askham JM, Vaughan KT, Goodson HV, Morrison EE (2002) Evidence that an interaction between EB1 and p150(Glued) is required for the formation and maintenance of a radial microtubule array anchored at the centrosome. Mol Biol Cell 13(10):3627–3645. doi:10.1091/mbc.E02-01-0061
Dixit R, Barnett B, Lazarus JE, Tokito M, Goldman YE, Holzbaur EL (2009) Microtubule plus-end tracking by CLIP-170 requires EB1. Proc Natl Acad Sci USA 106(2):492–497. doi:10.1073/pnas.0807614106
Su LK, Qi Y (2001) Characterization of human MAPRE genes and their proteins. Genomics 71(2):142–149. doi:10.1006/geno.2000.6428
Xie S, Ogden A, Aneja R, Zhou J (2016) Microtubule-binding proteins as promising biomarkers of paclitaxel sensitivity in cancer chemotherapy. Med Res Rev 36(2):300–312. doi:10.1002/med.21378
Komarova Y, De Groot CO, Grigoriev I, Gouveia SM, Munteanu EL, Schober JM, Honnappa S, Buey RM, Hoogenraad CC, Dogterom M, Borisy GG, Steinmetz MO, Akhmanova A (2009) Mammalian end binding proteins control persistent microtubule growth. J Cell Biol 184(5):691–706. doi:10.1083/jcb.200807179
Tirnauer JS, Grego S, Salmon ED, Mitchison TJ (2002) EB1-microtubule interactions in Xenopus egg extracts: role of EB1 in microtubule stabilization and mechanisms of targeting to microtubules. Mol Biol Cell 13(10):3614–3626. doi:10.1091/mbc.E02-04-0210
Manna T, Honnappa S, Steinmetz MO, Wilson L (2008) Suppression of microtubule dynamic instability by the +TIP protein EB1 and its modulation by the CAP-Gly domain of p150glued. Biochemistry 47(2):779–786. doi:10.1021/bi701912g
Vitre B, Coquelle FM, Heichette C, Garnier C, Chretien D, Arnal I (2008) EB1 regulates microtubule dynamics and tubulin sheet closure in vitro. Nat Cell Biol 10(4):415–421. doi:10.1038/ncb1703
Luo Y, Li D, Ran J, Yan B, Chen J, Dong X, Liu Z, Liu R, Zhou J, Liu M (2014) End-binding protein 1 stimulates paclitaxel sensitivity in breast cancer by promoting its actions toward microtubule assembly and stability. Protein Cell 5(6):469–479. doi:10.1007/s13238-014-0053-0
Thomas GE, Sreeja JS, Gireesh KK, Gupta H, Manna TK (2015) +TIP EB1 downregulates paclitaxel-induced proliferation inhibition and apoptosis in breast cancer cells through inhibition of paclitaxel binding on microtubules. Int J Oncol 46(1):133–146. doi:10.3892/ijo.2014.2701
Honnappa S, Gouveia SM, Weisbrich A, Damberger FF, Bhavesh NS, Jawhari H, Grigoriev I, van Rijssel FJ, Buey RM, Lawera A, Jelesarov I, Winkler FK, Wuthrich K, Akhmanova A, Steinmetz MO (2009) An EB1-binding motif acts as a microtubule tip localization signal. Cell 138(2):366–376. doi:10.1016/j.cell.2009.04.065
Luders J, Stearns T (2007) Microtubule-organizing centres: a re-evaluation. Nat Rev Mol Cell Biol 8(2):161–167. doi:10.1038/nrm2100
Tanenbaum ME, Medema RH (2010) Mechanisms of centrosome separation and bipolar spindle assembly. Dev Cell 19(6):797–806. doi:10.1016/j.devcel.2010.11.011
O’Connell CB, Khodjakov AL (2007) Cooperative mechanisms of mitotic spindle formation. J Cell Sci 120(Pt 10):1717–1722. doi:10.1242/jcs.03442
Nigg EA (2002) Centrosome aberrations: cause or consequence of cancer progression? Nat Rev Cancer 2(11):815–825. doi:10.1038/nrc924
Brinkley BR (2001) Managing the centrosome numbers game: from chaos to stability in cancer cell division. Trends Cell Biol 11(1):18–21
Lingle WL, Barrett SL, Negron VC, D’Assoro AB, Boeneman K, Liu W, Whitehead CM, Reynolds C, Salisbury JL (2002) Centrosome amplification drives chromosomal instability in breast tumor development. Proc Natl Acad Sci USA 99(4):1978–1983. doi:10.1073/pnas.032479999
Godinho SA, Pellman D (2014) Causes and consequences of centrosome abnormalities in cancer. Philos Trans R Soc Lond Ser B Biol Sci 369(1650):20130467. doi:10.1098/rstb.2013.0467
Rida PC, Cantuaria G, Reid MD, Kucuk O, Aneja R (2015) How to be good at being bad: centrosome amplification and mitotic propensity drive intratumoral heterogeneity. Cancer Metastasis Rev 34(4):703–713. doi:10.1007/s10555-015-9590-0
Pannu V, Mittal K, Cantuaria G, Reid MD, Li X, Donthamsetty S, McBride M, Klimov S, Osan R, Gupta MV, Rida PC, Aneja R (2015) Rampant centrosome amplification underlies more aggressive disease course of triple negative breast cancers. Oncotarget 6(12):10487–10497. doi:10.18632/oncotarget.3402
Liu L, Zou P, Zhang M, Tian L, Liu F (2006) Effect of polo-like kinase 1 gene silence on cell cycle and drug resistance in K562/A02 cell. Chin Med J 119(7):605–608
Ro S, Yang LX (2004) Centrosomes–their role in tumors and cancer therapy. Anticancer Res 24(5B):3269–3273
Anand S, Penrhyn-Lowe S, Venkitaraman AR (2003) AURORA-A amplification overrides the mitotic spindle assembly checkpoint, inducing resistance to Taxol. Cancer Cell 3(1):51–62
Casenghi M, Meraldi P, Weinhart U, Duncan PI, Korner R, Nigg EA (2003) Polo-like kinase 1 regulates Nlp, a centrosome protein involved in microtubule nucleation. Dev Cell 5(1):113–125
Zhao W, Song Y, Xu B, Zhan Q (2012) Overexpression of centrosomal protein Nlp confers breast carcinoma resistance to paclitaxel. Cancer Biol Ther 13(3):156–163. doi:10.4161/cbt.13.3.18697
Shao S, Liu R, Wang Y, Song Y, Zuo L, Xue L, Lu N, Hou N, Wang M, Yang X, Zhan Q (2010) Centrosomal Nlp is an oncogenic protein that is gene-amplified in human tumors and causes spontaneous tumorigenesis in transgenic mice. J Clin Investig 120(2):498–507. doi:10.1172/JCI39447
Qu D, Qu H, Fu M, Zhao X, Liu R, Sui L, Zhan Q (2008) Increased expression of Nlp, a potential oncogene in ovarian cancer, and its implication in carcinogenesis. Gynecol Oncol 110(2):230–236. doi:10.1016/j.ygyno.2008.04.015
Gergely F (2002) Centrosomal TACCtics. BioEssays News Rev Mol Cell Dev Biol 24(10):915–925. doi:10.1002/bies.10162
Gergely F, Draviam VM, Raff JW (2003) The ch-TOG/XMAP215 protein is essential for spindle pole organization in human somatic cells. Genes Dev 17(3):336–341. doi:10.1101/gad.245603
Cassimeris L, Morabito J (2004) TOGp, the human homolog of XMAP215/Dis1, is required for centrosome integrity, spindle pole organization, and bipolar spindle assembly. Mol Biol Cell 15(4):1580–1590. doi:10.1091/mbc.E03-07-0544
Schneider L, Essmann F, Kletke A, Rio P, Hanenberg H, Wetzel W, Schulze-Osthoff K, Nurnberg B, Piekorz RP (2007) The transforming acidic coiled coil 3 protein is essential for spindle-dependent chromosome alignment and mitotic survival. J Biol Chem 282(40):29273–29283. doi:10.1074/jbc.M704151200
Yao R, Natsume Y, Noda T (2007) TACC3 is required for the proper mitosis of sclerotome mesenchymal cells during formation of the axial skeleton. Cancer Sci 98(4):555–562. doi:10.1111/j.1349-7006.2007.00433.x
Ha GH, Kim JL, Breuer EK (2013) Transforming acidic coiled-coil proteins (TACCs) in human cancer. Cancer Lett 336(1):24–33. doi:10.1016/j.canlet.2013.04.022
Cully M, Shiu J, Piekorz RP, Muller WJ, Done SJ, Mak TW (2005) Transforming acidic coiled coil 1 promotes transformation and mammary tumorigenesis. Can Res 65(22):10363–10370. doi:10.1158/0008-5472.CAN-05-1633
Lv J, Yao YS, Zhou F, Zhuang LK, Yao RY, Liang J, Qiu WS, Yue L (2014) Prognosis significance of HER2 status and TACC1 expression in patients with gastric carcinoma. Med Oncol 31(11):280. doi:10.1007/s12032-014-0280-5
Onodera Y, Takagi K, Miki Y, Takayama K, Shibahara Y, Watanabe M, Ishida T, Inoue S, Sasano H, Suzuki T (2016) TACC2 (transforming acidic coiled-coil protein 2) in breast carcinoma as a potent prognostic predictor associated with cell proliferation. Cancer Med 5(8):1973–1982. doi:10.1002/cam4.736
Lauffart B, Vaughan MM, Eddy R, Chervinsky D, DiCioccio RA, Black JD, Still IH (2005) Aberrations of TACC1 and TACC3 are associated with ovarian cancer. BMC Women’s Health 5:8. doi:10.1186/1472-6874-5-8
Jung CK, Jung JH, Park GS, Lee A, Kang CS, Lee KY (2006) Expression of transforming acidic coiled-coil containing protein 3 is a novel independent prognostic marker in non-small cell lung cancer. Pathol Int 56(9):503–509. doi:10.1111/j.1440-1827.2006.01998.x
Kiemeney LA, Sulem P, Besenbacher S, Vermeulen SH, Sigurdsson A, Thorleifsson G, Gudbjartsson DF, Stacey SN, Gudmundsson J, Zanon C, Kostic J, Masson G, Bjarnason H, Palsson ST, Skarphedinsson OB, Gudjonsson SA, Witjes JA, Grotenhuis AJ, Verhaegh GW, Bishop DT, Sak SC, Choudhury A, Elliott F, Barrett JH, Hurst CD, de Verdier PJ, Ryk C, Rudnai P, Gurzau E, Koppova K, Vineis P, Polidoro S, Guarrera S, Sacerdote C, Campagna M, Placidi D, Arici C, Zeegers MP, Kellen E, Gutierrez BS, Sanz-Velez JI, Sanchez-Zalabardo M, Valdivia G, Garcia-Prats MD, Hengstler JG, Blaszkewicz M, Dietrich H, Ophoff RA, van den Berg LH, Alexiusdottir K, Kristjansson K, Geirsson G, Nikulasson S, Petursdottir V, Kong A, Thorgeirsson T, Mungan NA, Lindblom A, van Es MA, Porru S, Buntinx F, Golka K, Mayordomo JI, Kumar R, Matullo G, Steineck G, Kiltie AE, Aben KK, Jonsson E, Thorsteinsdottir U, Knowles MA, Rafnar T, Stefansson K (2010) A sequence variant at 4p16.3 confers susceptibility to urinary bladder cancer. Nat Genet 42(5):415–419. doi:10.1038/ng.558
Schmidt S, Schneider L, Essmann F, Cirstea IC, Kuck F, Kletke A, Janicke RU, Wiek C, Hanenberg H, Ahmadian MR, Schulze-Osthoff K, Nurnberg B, Piekorz RP (2010) The centrosomal protein TACC3 controls paclitaxel sensitivity by modulating a premature senescence program. Oncogene 29(46):6184–6192. doi:10.1038/onc.2010.354
Ahmed AA, Lu Z, Jennings NB, Etemadmoghadam D, Capalbo L, Jacamo RO, Barbosa-Morais N, Le XF, Australian Ovarian Cancer Study G, Vivas-Mejia P, Lopez-Berestein G, Grandjean G, Bartholomeusz G, Liao W, Andreeff M, Bowtell D, Glover DM, Sood Jr AK, Bast RC (2010) SIK2 is a centrosome kinase required for bipolar mitotic spindle formation that provides a potential target for therapy in ovarian cancer. Cancer Cell 18(2):109–121. doi:10.1016/j.ccr.2010.06.018
Fry AM, Mayor T, Meraldi P, Stierhof YD, Tanaka K, Nigg EA (1998) C-Nap1, a novel centrosomal coiled-coil protein and candidate substrate of the cell cycle-regulated protein kinase Nek2. J Cell Biol 141(7):1563–1574
Mayor T, Hacker U, Stierhof YD, Nigg EA (2002) The mechanism regulating the dissociation of the centrosomal protein C-Nap1 from mitotic spindle poles. J Cell Sci 115(Pt 16):3275–3284
Shi X, Liu M, Li D, Wang J, Aneja R, Zhou J (2012) Cep70 contributes to angiogenesis by modulating microtubule rearrangement and stimulating cell polarization and migration. Cell Cycle 11(8):1554–1563. doi:10.4161/cc.19954
Shi X, Sun X, Liu M, Li D, Aneja R, Zhou J (2011) CEP70 protein interacts with gamma-tubulin to localize at the centrosome and is critical for mitotic spindle assembly. J Biol Chem 286(38):33401–33408. doi:10.1074/jbc.M111.252262
Shi X, Wang J, Yang Y, Ren Y, Zhou J, Li D (2012) Cep70 promotes microtubule assembly in vitro by increasing microtubule elongation. Acta Biochim Biophys Sin 44(5):450–454. doi:10.1093/abbs/gms017
Shi X, Yao Y, Wang Y, Zhang Y, Huang Q, Zhou J, Liu M, Li D (2015) Cep70 regulates microtubule stability by interacting with HDAC6. FEBS Lett 589(15):1771–1777. doi:10.1016/j.febslet.2015.06.017
Shi X, Wang Y, Sun X, Wang C, Jiang P, Zhang Y, Huang Q, Liu X, Li D, Zhou J, Liu M (2017) Centrosomal protein 70 is a mediator of paclitaxel sensitivity. Int J Mol Sci 18(6):1267. doi:10.3390/ijms18061267
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100(1):57–70
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674. doi:10.1016/j.cell.2011.02.013
Kops GJ, Weaver BA, Cleveland DW (2005) On the road to cancer: aneuploidy and the mitotic checkpoint. Nat Rev Cancer 5(10):773–785. doi:10.1038/nrc1714
Fang X, Zhang P (2011) Aneuploidy and tumorigenesis. Semin Cell Dev Biol 22(6):595–601. doi:10.1016/j.semcdb.2011.03.002
Lara-Gonzalez P, Westhorpe FG, Taylor SS (2012) The spindle assembly checkpoint. Curr Biol CB 22(22):R966–R980. doi:10.1016/j.cub.2012.10.006
Prencipe M, Fitzpatrick P, Gorman S, Tosetto M, Klinger R, Furlong F, Harrison M, O’Connor D, Roninson IB, O’Sullivan J, McCann A (2009) Cellular senescence induced by aberrant MAD2 levels impacts on paclitaxel responsiveness in vitro. Br J Cancer 101(11):1900–1908. doi:10.1038/sj.bjc.6605419
Bargiela-Iparraguirre J, Prado-Marchal L, Pajuelo-Lozano N, Jimenez B, Perona R, Sanchez-Perez I (2014) Mad2 and BubR1 modulates tumourigenesis and paclitaxel response in MKN45 gastric cancer cells. Cell Cycle 13(22):3590–3601. doi:10.4161/15384101.2014.962952
Fu Y, Ye D, Chen H, Lu W, Ye F, Xie X (2007) Weakened spindle checkpoint with reduced BubR1 expression in paclitaxel-resistant ovarian carcinoma cell line SKOV3-TR30. Gynecol Oncol 105(1):66–73. doi:10.1016/j.ygyno.2006.10.061
Hirokawa N, Noda Y (2008) Intracellular transport and kinesin superfamily proteins, KIFs: structure, function, and dynamics. Physiol Rev 88(3):1089–1118. doi:10.1152/physrev.00023.2007
Miki H, Setou M, Kaneshiro K, Hirokawa N (2001) All kinesin superfamily protein, KIF, genes in mouse and human. Proc Natl Acad Sci USA 98(13):7004–7011. doi:10.1073/pnas.111145398
Hirokawa N (1998) Kinesin and dynein superfamily proteins and the mechanism of organelle transport. Science 279(5350):519–526
Rath O, Kozielski F (2012) Kinesins and cancer. Nat Rev Cancer 12(8):527–539. doi:10.1038/nrc3310
Yu Y, Feng YM (2010) The role of kinesin family proteins in tumorigenesis and progression: potential biomarkers and molecular targets for cancer therapy. Cancer 116(22):5150–5160. doi:10.1002/cncr.25461
Miki H, Okada Y, Hirokawa N (2005) Analysis of the kinesin superfamily: insights into structure and function. Trends Cell Biol 15(9):467–476. doi:10.1016/j.tcb.2005.07.006
Tan MH, De S, Bebek G, Orloff MS, Wesolowski R, Downs-Kelly E, Budd GT, Stark GR, Eng C (2012) Specific kinesin expression profiles associated with taxane resistance in basal-like breast cancer. Breast Cancer Res Treat 131(3):849–858. doi:10.1007/s10549-011-1500-8
Wang W, Shi Y, Li J, Cui W, Yang B (2016) Up-regulation of KIF14 is a predictor of poor survival and a novel prognostic biomarker of chemoresistance to paclitaxel treatment in cervical cancer. Biosci Rep 36(2):e00315. doi:10.1042/BSR20150314
Acknowledgements
This work was supported by Grants from the National Natural Science Foundation of China (31301113 and 31601089), the Natural Science Foundation of Jiangsu Province (BK20130607), and the Fundamental Research Funds for the Central Universities. Xingjuan Shi was supported by a scholarship from the China Scholarship Council.
Author information
Authors and Affiliations
Contributions
XS and XS designed the study and wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Shi, X., Sun, X. Regulation of paclitaxel activity by microtubule-associated proteins in cancer chemotherapy. Cancer Chemother Pharmacol 80, 909–917 (2017). https://doi.org/10.1007/s00280-017-3398-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3398-2