Abstract
The superior thyroid artery (STA) is the dominant arterial supply of the thyroid gland, upper larynx and the neck region. The knowledge of variations in possible patterns of origin, courses, and branching pattern of the STA is also important for surgical procedures in the neck region, such as emergency cricothyroidotomy, radical neck dissection, catheterization, reconstruction of aneurysm and carotid endarterectomy. The surgical anatomy of the STA was studied in 20 adult Anatolian preserved cadavers between the age of 40 and 70 years. The outer diameter of the STA origin was observed to be 3.53 ± 1.17 mm. The location of the origin of the STA according to the carotid bifurcation was evaluated as above (25%), below (35%) and at the same level (40%). The distribution patterns of the STA were classified into six types depending on the branching pattern. The outer diameter of the infrahyoid branch, superior laryngeal artery, sternocleidomastoid artery and cricothyroid branch at their origins were observed to be 1.13 ± 0.14, 1.42 ± 0.47, 1.54 ± 0.96 and 1.30 ± 0.41 mm, respectively. Typical and variant glandular branching patterns were observed in 85 and 15% of the specimens, respectively. The outer diameters of anterior, anteromedial, anterolateral and posterior glandular branches were measured as 2.05 ± 0.46, 1.41 ± 0.43, 1.51 ± 0.41 and 1.73 ± 0.53 mm, respectively. It is necessary to understand the surgical anatomy of the STA to carry out successful radical neck dissection and to minimize postoperative complications in a bloodless surgical field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The superior thyroid artery (STA) is the main source of artery for the thyroid gland, upper larynx and neck region, so the anatomic features of the arteries and neighborhoods are important in surgical attempts and approaches, which will be performed in this region [2, 26, 28, 30, 32].
In the treatment of metastasis cancer cases, microcatheterization, congenital wastes, aneurysm, penetrative device and an expansive trauma that require neck dissections and tracheotomy, which cause hemorrhage, is concomitant with high mortality and risk of disability [3, 11, 27, 28]. The surgical procedures for thyroid pathology are total bilateral lobectomy, total unilateral with partial contralateral lobectomy, and partial or subtotal lobectomy. Distruption of the STA or its branches by trauma or malignant invasion of the vessel wall can result in death by bleeding. Each surgical technique has inherent risks and complications including air leaks, bleeding, chylous fistula, facial and cerebral edema, coma and mortality [3, 7, 11, 15, 22, 23]. Therefore, understanding the anatomy of the STA and its possible variations is paramount to safe and effective surgery.
Several anatomic studies have described in detail such as the diameters of the origin of STA in detail; however, a detailed description of topoanatomic relations with the neck region is limited. Distances between STA and its surrounding landmarks are important including carotid bifurcation (CB), internal branch superior laryngeal nerve, thyroid cartilage, origin locations of the facial and lingual arteries and hypoglossal nerve. In this way, the incision may be mapped in an accurate fashion, and overall orientation may be maintained throughout the procedure. Lack of experience with possible variations could lead to fatal errors, if one blood vessel should be mistaken for another [3, 11, 21].
The aim of these anatomic dissections was to study the anatomic variations of the STA, origin differences, its branches and their measurements of diameters variability. The data will provide a guideline for otolaryngologist, neurosurgeons and neck surgeons. To decrease the complication risk to a minimum, the most important term which can be observed in the patient during and after the surgical attempt is to have a good knowledge of the anatomic features of the origin of the STA and its branches in neck region in order to help the patient return to his turn active life in a short time and lead a life of good quality.
Materials and methods
In this study, 40 Anatolian cadaver samples, right and left sides, taken from 17 men and 3 women cadavers, aged between 40 and 70 years, and kept in 10% formalin in the macroscopic laboratory, Department of Anatomy, Faculty of Medicine of the Ege University, have been studied. The skin overlying the neck, the superficial layer of the cervical fascia, platysma and sternocleidomastoid muscle were removed, carotid sheath was gently peeled off from the structures it covers and the part of the external carotid artery (ECA) in the neck was brought out. Micrometric values of the origin features of the STA and their relations to the surrounding structures, measurements belonging to the carotid bifurcation (CB) and thyroid cartilage (TC) and metric data pertaining to the origin locations of the lingual artery (LA) and facial artery (FA) have been evaluated by means of linear measures. The STA was dissected in order to determine its distribution pattern of the glandular thyroid branch. Measurements for this study were recorded as a digital ruler micrometer caliper 0.01 mm 0.0005 inch. In order to compare the values obtained from the right and left side measurements of the samples statistically, Mann–Whitney U test has been applied. P < 0.05 was considered to be significant.
The dissection was approved by a suitably constituted ethics committee of the institution within which the work was undertaken, and study conforms to the previous of the Declaration of Helsinki in 1964.
Results
Origin of the STA
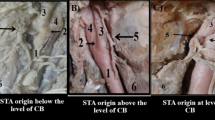
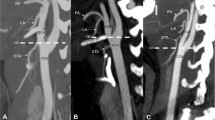
The outer diameter of the STA at its origin was observed to be 3.53 ± 1.17 mm. The location of the origin of the STA according to the CB was evaluated as above (25%), below (35%) and at the same level (40%) (Fig. 1a–c). The distance from the origin of the STA to the CB was 3.29 ± 4.27 mm, the distance from the origin of the STA to that of the LA was 10.45 ± 5.16 mm, and the distance from the origin of the STA to that of the FA was 18.20 ± 8.81 mm. The comparison of the right and left side values of the parameters of the STA in millimeter have been given in Tables 1 and 2. No differences were observed in the right–left side comparison of the data about the STA at a significance level of P > 0.01.
Regarding the evaluation of the stemming location of the STA from its originating artery, 82.5% of the cases had a medial location (Figs. 1c, 2b), 10% were anterior (Figs. 1b, 4b) and 5% were anteromedial (Figs. 1a, 2a). Topographic details of the STA origin to the ECA have been demonstrated in Table 3.
a Thyrolingual trunk case, STA’ inferomedial exit from the artery it originates (right side). 1 thyrolingual trunk, 2 lingual artery, 3 superior thyroid artery, 4 anterior glandular branch, 5 infrahyoid branch, 6 posterior glandular branch, 7 superior laryngeal artery. b The origin of STA and upper pole of right lobe closely positioned case (right side). 1 external carotid artery, 2 superior thyroid artery, 3 superior laryngeal artery, 4 anterior glandular branch
Regarding the evaluation of the branching types of the ECA (Fig. 2a–b), the cases where the STA, LA and FA originated as separate branches were categorised as Type I (90%) (Fig. 2b), linguofacial trunk cases as Type II (7.5%), thyrolingual trunk cases as Type III (2.5%) (Fig. 2a). In one thyrolingual trunk case determined, the STA was observed to originate from the common trunk with an inferomedial location (Fig. 2a). Regarding the evaluation of the origin of the STA according to the horizontal plane passing from the top side of the thyroid cartilage, it was found to be above in 60% (Figs. 2a, 4a), below in 22.5%, and at the same level in 17.5%. The details of the origin of the STA has been given in Table 4.
Branching type
The STA was classified into six categories based on branching patterns (Fig. 3a–f). In seven cases (17.5%), the infrahyoid branch and SLA were divided, followed by the sternocleidomastoid artery and the glandular thyroid branch (Fig. 3a).
In seven cases (17.5%), the infrahyoid branch was divided and then the three branches (superior laryngeal, thyroid glandular and sternocleidomastoid branches) were divided at one point (Fig. 3b).
In six cases (15%), the infrahyoid branch was divided first and then the sternocleidomastoid artery was divided second from the STA, followed by the SLA and the thyroid glandular branch (Fig. 3c).
In six cases (15%), the SLA was originated from the ECA and the sternocleidomastoid artery was arose from the SLA (Fig 3d).
In six cases (15%), the infrahyoid branch was originated from the ECA and the SLA was divided first and then the sternocleidomastoid artery was divided second from the STA, followed by the thyroid glandular branch (Fig. 3e).
In eight cases (20%), the sternocleidomastoid branch was divided from the ECA and infrahyoid branch was divided first and then the SLA was divided second from the STA, followed by the thyroid glandular branch (Fig. 3f).
Diameters of the branches
The comparison of the diameters of the right and left side values concerning branches of the STA has been given in millimeter in Table 5. No differences at a significance level of P > 0.01 were observed in the right–left side comparison of the data in Table 5.
Branches
Infrahyoid branch
In 85% of specimens (34), the infrahyoid branch originated from the STA while in the remaining 15% (6), it had origin from ECA. The infrahyoid branch was identified as a vascular pedicle of the sternohyoid, sternothyroid and superior belly of omohyoid muscles. In all specimens, infrahyoid artery ran along the border of the hyoid bone deep to thyrohyoid membrane. They anastomosed with its fellow of the opposite side to supply the infrahyoid strap muscles (Figs. 2a, 4a, 5a).
a Classical branching form of superior thyroid artery (right side). 1 infrahyoid branch, 2 anterior glandular branch, 3 posterior glandular branch, 4 anterolateral glandular branch, 5 anteromedial glandular branch, 6 cricothyroid branch, b posterior glandular branch’s high-bifurcation case (left side). 1 external carotid artery, 2 superior thyroid artery, 3 posterior glandular branch, 4 anterior glandular branch, 5 pyramidal lobe branch, 6 anterolateral glandular branch
a The form of superior thyroid artery presence of pyramidal lobe. 1 superior thyroid artery, 2 posterior glandular branch, 3 anterolateral glandular branch, 4 anteromedial glandular branch, 5 infrahyoid branch, 6 pyramidal lobe branch. b Course of posterior glandular branch on thyroid gland (left side). 1 superior thyroid artery, 2–3 posterior glandular branch, 4 anteromedial glandular branch
Superior laryngeal artery
In 85% of specimens (34), the SLA originated from the STA while in the remaining 15% (6), it had origin from ECA. The SLA ran down towards the larynx with the internal branch of the superior laryngeal nerve lying above it (Fig. 2a–b).
Sternocleidomastoid artery
In 80% of specimens (32), the sternocleidomastoid artery was originated from the STA while in the remaining 20% (8), it had origin from ECA. The sternocleidomastoid artery descended laterally across the carotid sheath and supplied the middle region of sternocleidomastoid.
Cricothyroid artery
In 70% of specimens (28), the cricothyroid branch was originated from anterior glandular branch while in the remaining 30% (12), it had origin from STA. The cricothyroid branch crossed high on the anterior cricothyroid ligament, anastomosed with its fellow of the opposite side (Fig. 4a).
Glandular branches
The anterior glandular branches (AGB) classically run along by branching through the medial side of the upper pole of the lateral lobe to supply mainly the anterior surface as anteromedial and anterolateral glandular branches (Figs. 3a, 4a). The AGB branch crossed above the isthmus to anastomose with its fellow of the opposite side; and a posterior glandular branch (PGB), descends on the posterior border to supply the medial and lateral surfaces (Figs. 2a, 4b, 5a, b).
Along with classical branching (85%), AGB which separate from STA were observed as well as PGB cases which separate from STA before reaching the upper pole of the lobes of thyroid gland and scattered on the posterior surface of the gland (Figs. 2a, 4b). There were 15% of the cases where anterolateral branch and anteromedial branch were double. Three posterior branches, two posterior branches were observed in two cases bilaterally (Fig. 5b). Differences were observed in AGB structures separated from STA in the presence of pyramidal lobe (Figs. 4b, 5a). In these cases, AGB was observed as two or more branches, one of which went to pyramidal lobe. The average diameter of arteries of the pyramidal lobe were 1.31–1.49 mm. The number of cases where increased vascularization occur with pyramidal lobe structure were 11 out of 20 (55%). Ectopic thyroid tissue was not observed macroscopically in the cases studied. In the case without isthmus, anastomosis was not observed between anteromedial glandular branches on the anterior surface of the gland (Fig. 4b).
Discussion
The morphology and embryology of the circulatory system of the STA have been included in many textbooks and review articles [6, 9, 30, 32]. The variational courses of the branches of TSA, their morphometric values, their relationship with the neighbouring anatomic structures and all the variations related to these details have a great role in the interventions for the diagnosis and treatment of the upper larynx, parathyroid and thyroid glands. Injury to the STA during neck surgery may result in a life-threatening acute hemorrhage as the varitions of the STA, was not apparent pre-operatively. The surgeon should be careful in performing routine surgical procedures in the area of the larynx, which generally represent the most frequent interventions carried out by inexperienced surgeons as the first steps of their training.
Origin
The STA, as shown in the anatomic literature, is usually the first branch of the anterior wall of the ECA but it can arise at the level of the bifurcation or also from the common carotid artery. The STA typically arises from the anterior surface of the ECA just below the level of the greater cornu of the hyoid bone [6, 14, 32]. The authors found an ECA origin of the STA in 30–70% of the cases [11, 26]. In literature, there are reports of the TSA originating from the CCA, and the thyrolinguofacial trunk from the ECA [2–4, 11, 14, 17, 24–26, 31]. There are also reports of the origin of the STA, and vertebral and inferior thyroid arteries from the CCA [1, 16, 19, 25]. Toni et al. [31] reported that a higher frequency of origin from the ECA was present in Caucasoids than in East Asians. In contrast, a higher frequency of origin from common carotid artery was observed in East Asians versus Caucasoids. Regarding our Anatolian specimens, the STA arising from the level of the CB was more common (40%) and that arising from the ECA and common carotid artery occurred at frequencies of 25 and 35%, respectively.
The origin of the thyrolingual trunk being the ECA has been reported with an incidence of range between 0.7 and 3% [12, 20, 28]. Nevertheless, various researchers have reported the case of thyrolingual trunk originating from the CCA and its frequency was presented as 0.1% [31]. In this study, a thyrolingual trunk originating from the ECA was detected and the thyrolingual trunk originating from the CCA was not observed.
Previous authors reported that the STA is occasionally double and unilateral [28]. An unusually large STA may replace the contralateral vessel or inferior thyroid artery on the same side. It can be so small that it is represented only by the infrahyoid branches or by the SLA. In our study, no such case has been observed.
Former investigators reported that average outer diameter of the STA is 3.2 mm (range 1.5–4.5 mm). The data gathered in our study and in those presented in literature are in accordance with each other. The STA usually has a sharp downward angle at its origin. By exaggerating the distal curve of the catheter to point downward, or by using a small J guide wire, catheterization of the STA and its branches is facilitated [32]. The awareness of anatomic variation of the origin may also warn the surgeon that during thyroid surgery, ECA ligation in an uncontrollable upper pole bleeding will not always be sufficient to stop hemorrhage.
Branches
The STA usually parallels the external branch of the superior laryngeal nerve, coursing anteroinferiorly and slightly toward the apex of the thyroid gland [3, 24, 25, 28, 29]. There are five branches of the STA: the infrahyoid, sternocleidomastoid, SLA, cricothyroid, and terminal branches of the artery for the blood supply of the thyroid and parathyroid glands.
Although various branching types were mentioned, detailed studies concerning the branching types of the STA were quite insufficient. Hu et al. [12] demonstrated the branching pattern of the STA is classified into six categories. They found that in type I, 36%, the superior SLA is divided first, followed by sternocleidomastoid branch and thyroid branch. In type II, 16%, the three branches are divided at one point. 10% of the cases are observed as type III, where the sternocleidomastid is divided first from the STA, followed by the superior laryngeal branch and the glandular thyroid branch.
Superior laryngeal artery
The main blood vessel that is significantly distributed in the larynx (epiglottid, ary-epiglottic fold, anterior wall of the larynx, arytenoids region) is the SLA [3, 5, 8, 13, 32]. They found that the arteries distributed in the upper part of the larynx are also branches of the arteries entering the larynx from the lower margin of the thyroid cartilage. The previous authors reported that the origin of the SLA is variable. It arises from the STA in about 80% of the cases [10, 32]. It might also directly arise from the ECA or the ascending pharyngeal artery [18, 29]. They also measured that the average outer diameter of the SLA is 1.2 mm on the right and 1.4 mm on the left (range 0.7–1.9 mm).
It is essential to identify the SLA arising from the STA for superselective intraarterial infusion and partial larygectomy [31]. Terayama et al. [29] showed that for most cases of glottic and supraglottic cancers, without or with minimum tumor spread across the midline, chemotherapeutic agents were delivered via the ipsilateral STA to the entire tumor. For a few cases, in which the SLA arose from the proximal portion of the STA, a microcatheter was unsettled and readily advanced more distal than the origin of the SLA. For cases, in which the SLA arises from the external carotid artery, direct catheterization into the SLA is also required [29].
In the methods of partial laryngectomy and partial reconstruction, it is important to designe to sustain phonation with the healthy vocal fold on the side opposite to the affected side and form the glottis with the wall and vestibular fold of larynx, which are constructed with the peripheral structure or flap at the site of laryngectomy [13]. The management of the SLA should be considered for conservation of the functions of the arytenoid region and laryngeal part of pharynx on partial laryngectomy and partial reconstruction of the larynx.
Infrahyoid branch
Previous reporters demonstrated that the infrahyoid branch originated from the STA (70–100%) and measured its diameter as 1 mm (range 0.5–2) [10]. Since the application of infrahyoid muscle flaps is versatile, reliable and convenient for repairing defects in the head and neck region, the knowledge of exact entering sites of the vascular pedicles supplying these muscles may guide surgeons in carrying out safe and efficient flap elevations [10].
Sternocleidomastoid branch
Former authors reported the sternocleidomastoid branch as the first branch in 20%, as the second branch 36% and the three branches divided at one point in 16% [1, 14, 18]. They measured its diameter as 1.1 mm. The knowledge of sternocleidomastoid branch will provide useful information for the clinical applications in the fields of oral and maxillofacial flap surgery.
Cricothyroid branch
Numerous studies have been published advocating cricothyroidotomies as a safe and effective option for emergency airway management. Tracheotomy is performed following the extensive operative procedures upon the neck when postoperative laryngeal edema, obstruction by a foreign body or postoperative vocal cord paralysis exists, or as a concurrent procedure when a total laryngectomy is performed, or following a severe facial trauma. Most literature agree that the cricothyroid branch usually arises from the STA and commonly has rich anastomoses with the SLA deep to the lamina of the thyroid cartilage. Dover et al. [8] demonstrated that a transverse cricothyroid branch is present, 93% of these are seen coursing across the upper one-third of the cricothyroid membrane, while the remaining 5% cross the lower portion of the membrane.
The cricothyroid branch may arise from the anterior branch of the STA (66%) [5]. Previous authors reported that the outer diameter of cricothyroid branch is average 1.15 mm. In some cases, enlarged right and left cricothyroid arteries anastomose in the midline and give rise to a median descending vessel that supplies the middle lobe of the thyroid gland, if present [28].
Glandular branch
Usually, there are two branches to the thyroid glandular (the anterior and posterior), but occasionally there may be a third, so called, a lateral branch. At the superior pole, the anterior branch divides into anterolateral and anteromedial branches. The anterolateral and anteromedial branches anastomose with branches of the inferior thyroid artery. From the posterior branch, a small parathyroid artery passes to the superior parathyroid gland [8, 10, 12, 13, 24].
Bleeding during thyroglossal cyst surgery, pyramidal lobe excision, or division of a thick thyroid isthmus during thyroid surgery or tracheotomy is most likely due to the injury of the cricothyroid artery. This artery springs from the STA or from its anterior branch. It follows the upper border of the cricothyroid muscle and membrane [28]. The disadvantages of some methods include an increased risk of damage on the cricoid cartilage as well as haemorrhage from the cricothyroid artery [5]. Execution of horizontal procedure using either technique requires knowledge of local anatomy in order to minimise the chance of complications. Such a study would serve to clarify the patterns of anatomic variation in the STA and cricothyroid branches and provide a more accurate base of knowledge for the guidelines for emergency airway management procedures.
Congenital anomalies of the thyroid gland (lobes unequal, persistent remmants of thyroglossal duct, absence of pyramidal lobe, lingual thyroid, accessory ectopic thyroid tissue, lateral aberrant thyroid) may cause an alteration in vascularization and a difference in surgical approach. However, detailed information concerning the branching types is quite insufficient. Skandalakis stated a single anterior branch with 67% frequency, and two or more branches in the rest of the cases [28].
The laryngeal cancer is frequently supplied by the ipsilateral or the bilateral STAs. Superselective intra-arterial chemotherapy for laryngeal cancer from the STA is appropriate. To accomplish contrast enhancement of the entire tumor, intra-arterial infusion via other arteries than the STA is necessary. The STA must be ligated carefully; the STA tends to retract, thus filling the field with blood. The STA should not be clamped above the upper pole of the thyroid because the external laryngeal nerve may be injured. If the STA is clamped at the pole, a branch may escape, with resulting hemorrhage. The superior pole, together with the artery, should be clamped and ligated [28]. Awareness of this particular anatomic variation may also warn the surgeon that during thyroid surgery, external carotid artery ligation in uncontrollable upper pole bleeding will not always be sufficient to stop hemorrhage in cases of high-originated double STA.
This study has provided measured objective criteria for the features of the STA, which are crucial during neck surgery. Findings about the landmarks of the arteries and side symmetry are to be carefully considered. No differences at a significance level of P > 0.01 were observed in the right-left side comparison of the data about all the parameters. Especially, the pattern of the branches of the STA showed a wide diversity and various investigators have not come to agree upon this. It has been further seen that the results of this study, are compatible with the results of those in literature.
Radical neck dissection is carried out to extract cancer masses, which hold neckpieces of the carotid body, thyroid gland, parathyroid gland, hypopharynx, larynx, trachea and oesophagus, and to clean metastatic lymph nodes [1]. During radical neck surgery, the most feared complication is the rupture of the STA and its branches. Iatrogenic injury can be avoided with this knowledge as well as the possible anatomic and pathological variations that may exist. A profound knowledge of the anatomic characteristics and variations of the STA such as its branching patterns, lengths, and outer diameters is an important value for a safe attempt in a suitable position for catheterization and approaches for surgeons in planning and performing procedures in neck region. Since anomalies of the STA of the neck region have been observed during a cadaveric study, the course of the STA must be preoperatively confirmed by Doopler examination, and great care should be taken during operations so as to not to damage vessel wall. It is helpful to assess the patterns of the STA located in the infrahyoid region on the angiogram before surgery.
References
Adachi B (1929) Das Arteriensystem der Japaner, vol 1. Kenkyusha, Kyoto, pp 58–62
Akyol MU, Koc C, Ozcan M, Ozdem C (1997) Superior thyroid artery arising from the common carotid artery. Otolaryngol Head Neck Surg 116:701
Anthony JP, Argenta P, Trabulsy PP, Lin RY, Mathes SJ (1996) The arterial anatomy of larynx transplantation: Microsurgical revascularization of the larynx. Clin Anat 9(3):155–159
Babu BP (2001) Anomalous origin of thyrolingual trunk from right common carotid artery—a case report. J Anat Soc India 50:47–49
Cole RR, Aguilar EA (1988) Cricothyroidotomy versus tracheotomy: an otolaryngologists perspective. Laryngoscope 98:131–135
Czerwinski F (1981) Variability of the course of external carotid artery and its rami in the light of anatomical and radiological study. Folia Morphol (Warsz) 40:449
Dedecjus M, Tazbir J, Kaurzel Z, Lewinski A, Strozyk G, Brzezinski J (2007) Selective embolization of thyroid arteries as a preresective and palliative treatment of thyroid cancer. Endocr Relat Cancer 14(3):847–852
Dover K, Howdieshell TR, Colborn GL (1996) The dimensions and vascular anatomy of the cricothyroid membrane: relevance to emergent surgical airway access. Clin Anat 9:291–295
Fujimoto Y, Suwa F, Kimura K (1974) A case of the left superior thyroid artery arising from the left common carotid artery and the a. thyroidea ima. Okajimas Folia Anat Jpn 51(5):219–230
Gormus G, Bayramoglu A, Aldur M, Celik H, Maral T, Sargon MF, Demiryurek D, Aksit MD (2004) Vascular pedicles of infrahyoid muscles. Clin Anat 17:214–217
Hayashi N, Hori E, Ohtani Y, Ohtani O, Kuwayama N, Endo S (2005) Surgical anatomy of the cervical carotid artery for carotid endarterectomy. Neurol Med Chir 45(1):25–29
Hu KS, Song WC, Kim SH, Choi SW, Han SH, Paik DJ, Kim HJ, KOh KS (2006) Branching patterns of the arterial branches supplying the middle vascular pedicle of the sternocleidomastoid muscle: a topographic anatomical study with surgical applications for the use of pedicles osteomuscular flaps. Surg Radiol Anat 28:7–12
Iimura A, Itoh M, Terayama H, Nakamura Y, He G, Kondo Y, Takahashi T, Shimada K (2004) Anatomical study of meandering and functions of human intralaryngeal artery. Okajimas Folia Anat Jpn 81(5):85–92
Issing PR, Kempf HG, Lenarz T (1994) A clinically relevant variation of the superior thyroid artery. Laryngorhinootologie 73(10):536–537
Jeganath V, McElwaine JG, Stewart P (2001) Ruptured superior thyroid artery from central vein cannulation: treatment by coil embolization. Br J Anaesth 87(2):302–305
Kaneko K, Akita M, Murata E, Imai M, Soma K (1996) Unilateral anomalous left common carotid artery: a case report. Ann Anat 178(5):477–480
Kukwa A, Zbrodowski A (1966) A rare case of the superior thyroid artery from the left common carotid artery. Folia Morphol (Warsz) 25(4):641–643
Lasjaunias P, Berenstein A (1987) Thyrolaryngeal arteries. In: Lasjaunias P, Berenstein A (eds) Surgical neuroangiography, vol I. Functional anatomy of craniofacial arteries. Springer, Berlin, pp 207–219
Lemaire V, Jacquemin G, Medot M (2001) Thyrolingual trunk arising from the common carotid artery: a case report. Surg Radiol Anat 23:135–137
Loukas M, Louis RG, Cruz GS (2004) A case of an anomalous cricothyroid artery. Folia Morphol 64(3):253–260
Lucev N, Bobinac D, Maric I, Drescik I (2000) Variations of the great arteries in the carotid triangle. Otolaryngol Head Neck Surg 122(4):590–591
Luo CB, Teng MM, Chang FC, Chang CY (2006) Transarterial embolization of acute external carotid blowout syndrome with profuse oronasal bleeding by N-butyl-cyanoacrylate. Am J Emerg Med 24(6):702–708
Matsumura M, Kakegawa T, Shibasaki T (1987) Traumatic giant aneurysm of the external carotid artery. Surg Neurol 27:487–490
Moriggl B, Sturm W (1996) Absence of three regular thyroid arteries replaced by an unusual lowest thyroid artery (a. thyroidea ima): a case report. Surg Radiol Anat 18(2):147–150
Nizankowski C (1972) Common truncus thyrolinguofacialis. Anat Anz 132(5):530–534
Shima H, Von Luedinghausen M, Ohno K, Michi K (1998) Anatomy of microvascular anastomosis in the neck. Plast Reconstr Surg 101:33–41
Shimotakahara SG, Lampe HB, Harris K (1988) External carotid—internal carotid crossover anastomosis for reconstruction of common carotid resection. J Otolaryngol 18:62–67
Skandalakis J (2004) Skandalakis’ surgical anatomy. The embriyologic and anatomic basis of modern surgery. PMP, Athens, pp 7–108
Terayama N, Sanada J, Matsui O, Kobayashi S, Kawashima H, Yamashiro M, Tanaka T, Kumano T, Yoshizaki T, Furukawa M (2006) Feeding artery of laryngeal and hypopharyngeal cancers: role of the superior thyroid artery in superselective intraarterial chemotherapy. Cardiovasc Intervent Radiol 29:536–543
Todd NW (1993) Common congenital anomalies of the neck. Surg Clin North Am 73(4):599–610
Toni R, Della Casa C, Castorina S, Malaguti A, Mosca S, Roiti E, Valenti G (2004) A meta—analysis of superior thyroid artery variations in different human groups and their clinical implications. Ann Anat 186(3):255–262
Trotoux J, Germain MA, Bruneau X (1986) Vascularization of the larynx. Update of classical anatomic data from an anatomical study of 100 subjects. Ann Otolaryngol Chir Cervicofac 103(6):389–397
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ozgur, Z., Govsa, F., Celik, S. et al. Clinically relevant variations of the superior thyroid artery: an anatomic guide for surgical neck dissection. Surg Radiol Anat 31, 151–159 (2009). https://doi.org/10.1007/s00276-008-0405-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-008-0405-7