Abstract
When making a sternocleidomastoid (SCM) osteomuscular flap to include the clavicle and determining the rotation arc of the osteomuscular flap, it is very important to know the location and the origin of the superior thyroid artery and the distribution pattern of the SCM branch. Accordingly, in this study, the 50 SCM muscles and their arteries were dissected in 26 Korean cadavers, and the results were analyzed. The average distances from the origin of the superior thyroid artery to the clavicular and sternal heads of the SCM muscle were 87.6 mm (57.7–123.8 mm) and 131.2 mm (99.7–166.8 mm), respectively. The average distance from the origin of the superior thyroid artery to the SCM branch entering the SCM muscle was 30.1 mm (16.0–37.7 mm). After entering the SCM muscle, the SCM branches of the superior thyroid artery bifurcated into the clavicular and sternal branches at a point located an average of 58.8 mm (28.4–130.4 mm) above the clavicle. The distribution patterns of the superior thyroid artery were classified into six types based on the branching order and the dual supplies to the SCM muscle. Among them, type I in which the laryngeal branch first divided from the superior thyroid artery was the most common case (36%).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Understanding the anatomy of the arteries that are distributed to the sternocleidomastoid (SCM) muscle, the clavicle and the thyroid gland is necessary not only because this muscle can be used as a pedicle for flaps, such as osteomuscular flaps, but also because it is involved in other types of head and neck surgical procedures such as orofacial and oromaxillofacial surgery. The SCM musculocutaneous flap was first introduced by Jianu [11] as a treatment for facial paralysis, but it has subsequently been used for a variety of different purposes such as the reconstruction of the trachea or esophagopharyngeal fistula [6–8, 22], ensuring the continuity of the trachea after a tracheotomy [13], intraoral reconstruction that includes the floor of the mouth [2, 3, 20], mandible reconstruction [5] and the repair of large defects after parotidectomy [4, 12, 14, 23]. Although the SCM osteomuscular flap has many advantages with its long rotational arc, its use is limited by the variations in the course and distribution pattern of the artery supplying the SCM muscle. Mathes and Eshima [18] noted that the results of the SCM osteomuscular flap are not always satisfactory, with 20% of their surgical procedures being unsuccessful, and the proportion of postoperative complications reaching 30%. Yugueros and Woods [24] concluded that the infrequent use of this flap was due not only to the frequent complications but also to the limited rotation arc when the two blood vessels are preserved. Moreover, Larson and Goepfert [15] stated that too much tension on the flap might be the cause of failure of flap surgery because the rotation arc may be limited not only by the superior thyroid artery but also by the accessory nerve. These results indicate the necessity of knowing the precise course and branching pattern of the arteries supplying the SCM muscle. Although there are many studies on the practical importance of the SCM osteomuscular flap, the anatomy of the blood supply of the SCM, its distribution pattern within the SCM and the flap length, which determines the length of the rotation arc, have not been examined in detail.
This study examined the branching pattern of the superior thyroid artery supplying the SCM muscle and the clavicle, and evaluated the rotation arc for a mandibular reconstruction, with the aim of providing essential information for oral and maxillofacial surgery.
Materials and methods
Fifty sides from 26 Korean adult cadavers (24 bilateral specimens and two unilateral specimens) were carefully dissected. Thirty-three sides of the specimens were males and 17 were females (average age 58 years, range 17–93 years).
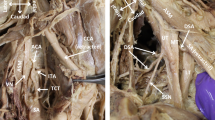
The skin overlying the neck, the superficial layer of the cervical fascia and the platysma were removed to expose the SCM muscle. The superior thyroid artery, which is the first branch of the external carotid artery, was dissected. The SCM branch, the thyroid branch and the superior laryngeal branch of the superior thyroid artery were found at the medial margin of the SCM muscle. In order to determine the distribution pattern of the SCM branch of the superior thyroid artery, the SCM branch was dissected in detail by retracting the SCM muscle.
The topographic course of the superior thyroid artery was investigated by measuring the following six distances using digital calipers (Fig. 1).
-
1.
The distance from the origin of the superior thyroid artery to the anterior margin of the SCM, parallel to the sagittal plane.
-
2.
The distance from the origin of the superior thyroid artery to its point of division into the SCM branch and the thyroid branch.
-
3.
The distance from the origin of the superior thyroid artery to the point where the SCM branch enters the SCM.
-
4.
The distance from the origin of the superior thyroid artery to the origin of the clavicular head of the SCM.
-
5.
The distance from the origin of the superior thyroid artery to the origin of the sternal head of the SCM.
-
6.
The distance from the point of division of the SCM branch into the clavicular branch and the sternal branch in SCM to the clavicle.
The distribution patterns of the superior thyroid artery were classified into six categories according to the branching order of the superior laryngeal branch, the thyroid branch and the SCM branch (Fig. 2).
Results
Among the branches of the external carotid artery, the major branches supplying the SCM muscle were the occipital and the superior thyroid arteries. The SCM branch of the occipital artery entered the SCM muscle at its superior and posterior portions, and supplied the upper half of the muscle. The SCM branch of the superior thyroid artery entered at the middle portion of the medial margin of the SCM muscle and ran down to the periosteum of the clavicle. This branch supplied the lower half of the SCM muscle. The branch of the thyrocervical trunk was found distributed to the lower portion of the SCM muscle, but its diameter was quite small.
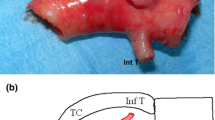
The distances from the origin of the superior thyroid artery to the three points—anterior margin of the SCM, the point where the artery bifurcates into the SCM branch and the thyroid branch and the point where the SCM branch enters the SCM muscle—were 34.4, 20.6 and 30.1 mm, respectively (Table 1; Fig. 3). The distances from the origin of the superior thyroid artery to the origin of the clavicular and sternal heads of the SCM muscle were 87.6 and 131.2 mm, respectively. The point where the SCM branch bifurcated into the clavicular and sternal branches was 58.8 mm above the clavicle (Table 1). The clavicular branch continued to the clavicle to form a periosteal branch that supplied the periosteum of the clavicle (Figs. 4, 5). Most of the SCM branches of the superior thyroid artery entered the muscle through only one branch (60%), with the incidences of two and three branches entering the muscle being 34 and 6%, respectively.
Measurements of the superior thyroid artery. The explanations regarding the number are described in the Materials and methods section. SCM sternocleidomastoid muscle
The superior thyroid artery was classified into six categories based on the branching patterns. In 18 cases (type I, 36%), the superior laryngeal branch was divided first, followed by the SCM branch and the thyroid branch. In eight cases (type II, 16%), the three branches were divided at one point. Five cases (10%) were observed as type III, where the SCM branch was divided first from the superior thyroid artery, followed by the superior laryngeal branch and the thyroid branch. In six cases (type IV, 12%), the SCM branch was divided at two points above and below the superior laryngeal branch. In seven cases (type V, 14%), the SCM branch was divided directly from the external carotid artery. Six cases (type VI, 12%) showed that the SCM branch was divided directly from both the external carotid artery and the superior thyroid artery (Fig. 6).
Discussion
The major complications of an SCM osteomuscular flap are ischemia, partial necrosis and fistula formation, which are attributed to the pre-operative radiation therapy or an incomplete blood supply to the flap [10, 18]. Therefore, preserving the blood vessels in the SCM osteomuscular flap is one of the most important methods for minimizing the number of complications and successfully preparing for surgery.
The SCM branch of the occipital artery is usually the largest and plays a major role in supplying blood to the SCM [9]. Also, the branches of the posterior auricular artery, superior thyroid artery and thyrocervical trunk are known as the other three minor arteries supplying the SCM [2, 10, 16, 17]. Therefore, the SCM was classified as a type II muscle [19]. Froes et al. [9] reported that the SCM branch of the occipital artery supplied the upper two-thirds of the SCM in 43.3% of cases, the upper five-sixths in 36.6% of cases and the upper half in only 20% of cases. However, in the Korean specimens investigated in the present study, the superior thyroid artery entered the SCM at the height of the middle part of the muscle and supplied the lower half of the SCM, while its upper half was supplied by the branch of the occipital artery. In many cases, the occipital artery and the superior thyroid artery were anastomosed, and the area supplied by the superior thyroid artery could be misinterpreted as the area supplied by the occipital artery.
In contrast, the surgical planning of an SCM osteomuscular flap should be limited in cases where two arteries are supplied to the SCM separately without anastomosis. The SCM muscle could become necrotic if the superior thyroid artery is cut since it supplies the lower half of the muscle.
According to the branching pattern of the branch of the superior thyroid artery, type I (36%) has many advantages such as minimal limitations of the rotational arc and a better possibility of preserving the superior laryngeal and thyroid branches of the superior thyroid artery in flap surgery. In contrast, it would be difficult to preserve the superior laryngeal and thyroid branches of the superior thyroid artery in type III cases (10%). In cases where the SCM branches directly divide from the external carotid artery (type V and type VI; 26%), the superior laryngeal and thyroid branches do not affect the rotational arc in the SCM osteomuscular flap surgery, including the clavicle.
The distance from the origin of the superior thyroid artery to the SCM muscle is important in the construction of an osteomuscular flap because of its possible limitation in the length when the muscle is rotated or flipped over. In this study, the most important measurement was the distance from the origin of the superior thyroid artery to the point where the SCM branch enters the SCM. As the distance increased, it became easier to relocate the flap. This length was 30.1 mm, and was long enough to relocate the osteomuscular flap.
In order to recover a defect of the neck after SCM osteomuscular flap surgery, Siemssen et al. [21] suggested a method using only the clavicular head of the SCM, leaving the sternal head of the SCM intact. Moreover, Alvarez et al. [1] reported that the method using only one head of the SCM has many advantages in preventing a neck deformity in cases of a benign tumor in the face and neck. If the dividing point of the SCM branch of the superior thyroid artery into the clavicular and sternal branches is located lower in the SCM, the rotational arc for osteomuscular flap surgery might be limited. Likewise, the use of the clavicular head or the sternal head for flap surgery could be easily carried out, if the dividing point is located higher. The distance of the dividing point through which the SCM branch of the superior thyroid artery runs into the SCM is an important factor. The mean distance from the bifurcation point of the SCM branch into the clavicular branch and the sternal branch to the clavicle was 58.7 mm. This length was sufficient to rotate the only clavicular head of the SCM and the clavicle towards the mandible. However, if this point is located too close to the clavicle, as was found in a few cases in this study, the rotation of the flap with one head might be difficult to perform.
In conclusion, the superior thyroid artery that supplies the SCM lower half should be preserved in order to minimize the number of complications after SCM flap surgery. It is believed that a study on the distribution and branching pattern of the branches of the superior thyroid artery will provide useful information for clinical applications in the fields of oral and maxillofacial flap surgery and an alternative option to bone free flaps (fibula, iliac crest, scapula), when such microsurgical transfers should not be performed for local or general disfavorable reasons.
References
Alvarez G, Escamilla J, Carranza A (1983) The split sternocleidomastoid myocutaneous flap. Br J Plast Surg 36:183–186
Ariyan S (1979) One stage reconstruction for defects of the mouth using a sternomastoid myocutaneous flap. Plast Reconstr Surg 63:618–625
Ariyan S (1980) The sternocleidomastoid myocutaneous flap. Laryngoscope 98:676–679
Bugis SP, Young JE, Archibald SD (1990) Sternocleidomastoid flap following parotidectomy. Head Neck Surg 12:430–435
Conley J, Gullane PJ (1980) The sternocleidomastoid muscle flap. Head Neck Surg 2:308–311
Friedman M, Grybaieskas V, Skolnick E, Toriumi D, Chilis T (1987) Sternomastoid myoperiosteal flap for reconstruction of the subglottic larynx. Ann Otol Rhinol Laryngol 96:163–169
Friedman M, Mayer AD (1992) Laryngotracheal reconstruction in adults with the sternocleidomastoid myoperiosteal flap. Ann Otol Rhinol Laryngol 101:897–908
Friedman M, Toriymi D, Strorigl T (1988) The sternocleidomastoid myoperiosteal flap in esophagopharyngeal reconstruction and fistula repair: clinical and experimental study. Laryngoscope 98:1084–1091
Froes LB, Tolosa EM, Camargo RS, Pompeu E, Liberti EA (1999) Blood supply to the human sternocleidomastoid muscle by the sternocleidomastoid branch of the occipital artery. Clin Anat 12:412–416
Jabaley ME, Heckler FR, Wallace WH, Knott LH (1979) Sternocleidomastoid region flaps: a new look at an old concept. Br J Plast Surg 32:106–113
Jianu J (1908) Paralizac faciale dupa extirparea unei tumori a parotidei tratata prin operatia. Olui Gomoiu. Soc de Chir de Bucharest 22
Jost G, Guenon, Gentil S (1999) Parotidectomy: a plastic approach. Aesth Plast Surg 23:1–4
Kinishi M, Amatsu M (2000) Sternocleidomastoid muscle suspension at end-to-end tracheal anastomosis. Laryngoscope 110:2047–2049
Kornblut AD, Westphal P, Miehlke A (1974) The effectiveness of a sternocleidomastoid muscle flap in preventing post parotidectomy occurrence of the Frey syndrome. Acta Otolaryngol 77:368–373
Larson DL, Goepfert H (1982) Limitations of the sternocleidomastoid musculocutaneous flap in head and neck cancer reconstruction. Plast Reconstr Surg 70:328–335
Littlewood M (1967) Compound skin and sternomastoid flaps for repair in extensive carcinoma of the head and neck. Plast Reconstr Surg 20:403–419
Marx RE, McDonald DK (1985) The sternocleidomastoid muscle as a muscular or myocutaneous flap for oral and facial reconstruction. J Oral Maxillofac Surg 213:155–162
Mathes SJ, Eshima I (1990) The principle of muscle and musculocutaneous flap. In: McCarthy JG (ed) Plastic surgery. W.B. Saunders, Philadelphia, pp 379–411
Mathes SJ, Nahai F (1981) Classification of the vascular anatomy of muscles: experimental and clinical correlation. Plast Reconstr Surg 67(2):177–187
Sasaki CT (1980) The sternocleidomastoid myocutaneous flap. Arch Otolaryngol 106:74–76
Siemssen S, Kirkby B, O’Connor T (1978) Immediate reconstruction of a resected segment of the lower jaw using a compound flap of clavicle and sternomastoid muscle. Plast Reconstr Surg 61:724–735
Tovi F, Gittot A (1983) Sternocleidomastoid myoperiosteal flap for the repair of laryngeal and tracheal wall defects. Head Neck Surg 5:447–451
Wechselberger G, Schoeller T, Otto A (1998) Treatment of chronic thoracicduct fistula with the sternocleidomastoid muscle flap. Am J Surg 176:471
Yugueros P, Woods JE (1996) The sternocleidomastoid myocutaneous flap. Br J Plast Surg 49:93–96
Acknowledgements
This study was supported by a grant no. R01-2002-000-00565-0 from Korea Science and Engineering Foundation, Republic of South Korea.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hu, K.S., Song, W.C., Kim, S.H. et al. Branching patterns of the arterial branches supplying the middle vascular pedicle of the sternocleidomastoid muscle: a topographic anatomical study with surgical applications for the use of pedicles osteomuscular flaps. Surg Radiol Anat 28, 7–12 (2006). https://doi.org/10.1007/s00276-005-0053-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-005-0053-0