Abstract
Observing the origin, varied branching configurations of superior thyroid artery (STA) and evaluating morphometric details with its surrounding relations was aimed at in this cadaveric neck dissection study to avoid surgical mishaps and its repercussions. This observational study was conducted on 40 fresh frozen embalmed and colored latex infused cadavers in the Department of Otorhinolaryngology and Head and Neck Surgery in collaboration with Department of Anatomy of our institute, which involved systematic evaluative dissection of both sides of neck especially focusing on superior thyroid artery, its branching variations and morphometric details with its surrounding relations. Details were measured using digital caliper. The collected data was statistically analyzed by applying chi-square test and significance was set at 5% level (p < 0.05). The analysis revealed the location of the origin of the superior thyroid artery of cadavers from carotid bifurcation and above it in 40% and from above the level of superior border of thyroid cartilage in 40% of cases. The distribution patterns of the superior thyroid artery were classified into three types depending on the branching pattern typical and variant glandular branching patterns were observed in 85% and 15% of the specimens respectively. A sound knowledge of the regional anatomy and its possible variations helps the surgeon in isolating and preserving the vital structures and avoid iatrogenic complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Successful surgical outcomes in neck surgeries especially the thyroid region require excellent knowledge of ideal anatomy and the surgeon is expected to be aware of the possible dimensions and variations of all the important structures that can be present in the region to circumvent complications.
The superior thyroid artery (STA) is the first branch from external carotid artery (ECA) which arises close to carotid bifurcation (CB) just below the level greater cornu of hyoid bone, then lies in carotid triangle and runs beneath omohyoid, sternohyoid and sternothyroid muscles. Medially it is related to inferior constrictor muscles of pharynx, travels with superior thyroid vein and pierces the thyroid gland on posteromedial surface underneath the uppermost point of upper pole [1].
It divides into two main branches the artery to sternocleidomastoid muscle and superior laryngeal artery. The latter pierces the thyrohyoid membrane together with the internal laryngeal nerve. There is wide variability regarding the STA location, origin, branching patterns, its relationship to the anatomical structures adjacent to it [2].
It is the mother artery that is main source for the thyroid gland, upper larynx and neck region, frequently used in grafting, embolization for thyroid and other head and neck tumors, emergency cricothyroidotomy, radical neck dissection, and diagnostic and therapeutic catheterization. Injury to it causes dreading complications including torrential bleeding hence, the anatomic features of the arteries and its surrounding relations help in precise incision, dissection and guidance while executing approaches around neck [3].
Distances between STA and its surrounding landmarks such as carotid bifurcation (CB), external branch of superior laryngeal nerve (EBSLN), thyroid cartilage (TC), origin of the facial artery (FA) and lingual artery (LA) and hypoglossal nerve (HN), are important during dissection in order to locate and prevent accidental injury to them [4].
Variations in the origin of STA has been reported in the literature. Our purpose of the study was to describe variations of the STA origin, its branching configurations and distance from surrounding arteries and nerves, which can be observed in humans and to validate the reported findings in the literature. The data was aimed at providing a helpful information to surgeon operating in this region of neck. The anatomical variations may be minor in degree but are important as they may affect the outcome of surgical procedure and the quality of life of patients. Therefore, having a thorough awareness of anatomy safeguards the integrity and protection of the important structures.
Materials and Methods
An institutional based observational study after obtaining ethical clearance was conducted on forty embalmed cadavers, 27 males and 13 females, with Latex mixed with a red colouring agent injected into all the specimens through the common carotid artery (CCA) to observe the topography of the STA. The cadavers were of Indian descent from Belagavi district of North Karnataka. The cadavers had no history of trauma or surgical procedures associated with the cervical region. Through midline incision extending from mentum to manubrium, sub platysmal plane was reached to further dissect the anatomical structures around the STA. after identifying CCA the origin of the STA in relation to it and thyroid lamina determined. By careful dissection, the relation of STA to the surrounding named landmarks and the relative distance to these were measured with digital caliper sensitive to 0.01 mm. The midline on the mid-sagittal plane as a vertical reference and three horizontal lines that is line along the hyoid bone, at the prominence of the thyroid cartilage, and the inferior border of the thyroid cartilage, were used as references. The measured distances was relative to these lines. The data was analyzed by using descriptive statistics and chi-square test for association. The statistical significance was set at 5% level (p < 0.05).
Results
Distance of Origin of STA to Surrounding Structures
The distance from origin of STA to the CB was 3.08 SD1.88 mm, with minimum distance of 0.2 mm and maximum of 6.40 mm. The data of STA origin and its distance to lingual artery, facial artery, superior laryngeal nerve, hypoglossal nerve, upper edge of TC along with mean and standard deviation and the comparison of the right and left side values and no significant difference was observed between right and left side values (p > 0.05) and the results are depicted in Table 1.
Origin of STA in Relation to Carotid Bifurcation (CB)
The location of the origin of the STA according to the CB was evaluated as above (40%), below (20%) and at the same level (40%) and the difference between sides or association was not significant (Chi-square = 0.3752 P = 0.8290) (Table 2, Fig. 1).
Originating Surface of STA from Caroitd Artery
STA had origin from anterior surface of carotid artery in 86.25% of cases 1.25% where from medial surface and in 12.50% of cases the origin was from anteromedial surface (Table 3) and the difference between sides or association was not significant (Chi-square = 0.4570 P = 0.4990).
Location of Origin STA According to Superior Border of Thyroid Cartilage (TC)
We observed 32 (40%) had origin from above the horizontal plane over top of TC, 24(30%) from same level, 24 (30%) origin was below the level of plane over the top side of the TC (Table 4). The difference between sides or association was not significant (p = 1.0000).
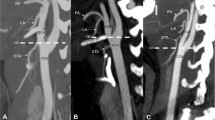
Branching Pattern of Superior Thyroid Artery (STA)
Regarding the branching types of STA in 45 sides (56.25%), the infrahyoid branch and superior laryngeal artery (SLA) were divided, followed by the sternocleidomastoid artery and the glandular thyroid branch (Type 1, Fig. 2A). Similarly, 31 sides (38.75%) where infrahyoid branch was divided first and superior laryngeal and sternocleidomastoid branch divided at same level followed by glandular branch (Type 2, Fig. 2B). Further, 4 sides (5%) showed type 3 pattern where the infrahyoid branch and sternocleidomastoid artery were divided, followed by the SLA and the glandular thyroid branch (Type 3, Fig. 2C). The difference between sides or association was not significant (Chi-square = 1.3622 P = 0.5060) as depicted in Table 5.
STA branching pattern with line diagrams, (1) Common carotid artery, (2) Carotid bifurcation, (3) External carotid artery, (4) Internal carotid artery, (5) Superior thyroid artery, (6) Thyroid gland, (7) Sternocleidomastoid muscle, (8) Sternocleidomastoid branch of STA, (9) Glandular branch of STA, (10) Infrahyoid branch of STA, (11) Vagus nerve, (12) Superior laryngeal artery, (13) Thyroid cartilage (14) Cricothyroid branch of STA
Discussion
The thyroid gland is a vascular organ. The main arterial supply of thyroid gland is STA. The variation in origin and paths of the branches of STA, and their association with surrounding structures play an important role in diagnostic and therapeutic procedures on thyroid gland, larynx, trachea and also during vascular anastomosis [5].
Origin
The first branch of the external carotid artery (ECA) is STA. We observed the ECA origin of STA in 40% of cadavers. It has been reported to have a varied origin, taking origin at the same level of CB, from the common carotid artery (CCA), as thyrolinguofacial trunk and from ECA [6].
The origin of the thyrolingual trunk being the ECA has been reported with an incidence of range between 0.7 and 3% [7]. In our study STA arose from below the level of CB in 20% and at same level of CB in 40%.
Toni et al. (2004) [8] reported that higher frequency of origin was from the ECA. Ozgur et al.(2009)[5] observed STA arose at same level with CB in most of cases (40%), in 35% it arose below the level of CB and in 10% above the level of CB. Other studies by Shima et al. (1998) [6] and Hayashi et al. (2005) [9] found STA originated from ECA in 30–70% of the cases.
STA usually arises from anterior surface of the ECA below the level of the greater cornu of the hyoid. In our study STA was seen arising from anterior surface of carotid artery in 86.25%of cadavers, from medial surface in 1.25% and in 12.50% the origin was from anteromedial surface. Va´zquez T et al. (2009) [10] in their study has reported that STA was arising from anterior surface in 95.2% of cases.
Assessing the origin of STA to superior border of thyroid cartilage in 32 (40%) sides STA had origin from above the parallel plane crossing over top of the thyroid cartilage, 24(30%) from same level, 24 (30%) origin was below the level of plane crossing over top level of TC.
Ozgur et al.(2009) [5] in their study found STA to be above in 60%, below in 22.5%, and at the same level in 17.5% cases which was similar to our observations.
Distance from origin of STA with surrounding relations as observed in our study of 40 cadaver. right and left sides, the distance of STA to the CB was 3.08 SD1.88 mm, with minimum distance of 0.2 mm and maximum of 6.40 mm,which was similar to study conducted by Ozgur et al.(2009) [5] where it was 3.29 SD4.27 mm.
The distance from the origin of the STA to that of the LA in present study ranged from 7.80 SD2.11 mm, the distance from the origin of the STA to that of the FA was 14.73 SD3.00 mm. Ozgur et al. (2009) [5] observed the distance from STA to LA was 10.45 SD 5.16 mm, and the distance from the STA to FA was 18.20 SD8.81 mm.
The distance to superior laryngeal nerve in present study was 5.9 SD4.9 as compared to 8.42 SD1.33 mm observed by Ozgur et al. (2009) [5].
In present study, the distance to hypoglossal nerve was observed as 18.35 SD 2.27 mm and to the thyroid cartilage upper edge was 4.52 SD1.94 when compared with the study by Ozgur et al. (2009) [5] the distance to hypoglossal nerve was 12.8 SD 7.2 and to thyroid cartilage upper edge was 7.1 SD6.4. in our study.
Branches
In literature, five branches of the STA have been observed: the infrahyoid, sternocleidomastoid, SLA, cricothyroid, and terminal glandular branches to supply the gland [9, 11].
The main blood vessel, which is considerably distributed in the larynx, is Superior laryngeal artery (SLA). It has variable origin, mostly it arises from the STA and sometimes can arise directly from ECA. We observed SLA originated from STA in 100% cadavers. Ozgur et al. (2009)[5] in their study observed in 85% (34) of specimens, the SLA arose from the STA and in rest of 15% (6) it originated from ECA.
Infrahyoid branch supplies sternothyroid, sternohyoid and superior belly of omohyoid muscles. We observed in all specimens, it passed parallel to hyoid bone deep to thyrohyoid membrane. It originated from STA in 100% cadavers. In the study by Ozgur et al. (2009) [5] 85% (34) of specimens, the infrahyoid branch had its origin from STA and 15% (6) had origin from ECA.
Cricothyroid artery generally originate from STA, anastomoses with SLA deep to TC. It crosses anterior cricothyroid ligament and anastomose with its branch of the other side. In our study, itoriginated from anterior glandular branch in 100% cadavers as compared to observation by Ozgur et al. (2009) [5] where the cricothyroid branch originated from anterior glandular branch in 70% (28) of specimens, in 30% (12) it had origin from STA.
The anterior glandular branches (AGB) runs along the medial side of the lateral lobe and supplies anterior surface via anteromedial and anterolateral glandular branches. The posterior glandular branch (PGB) descends on posterior border to supply the medial and lateral surfaces. In our study, anterior glandular branch (AGB) ran on medial surface of lobe and anastomosed with its fellow of the other side; and a PGB, ran on the posterior border to supply the medial and lateral surfaces. Ozgur et al. (2009) [5] reported AGB separated from STA and PGB separated from STA before reaching the upper pole of lobes of thyroid gland in 85% and dispersed on glands posterior surface.
Sternocleidomastoid branch descends laterally across the carotid sheath and supplied the middle region of sternocleidomastoid. In our study, it arose from the STA in all cadavers and as first branch in 5%, second branch in 56.25% and in 38.75% the three branches divided at one point. Ozgur et al. (2009) [5] observed in 80% (32) of specimens, the sternocleidomastoid artery arose from STA and in 20% (8), it originated from ECA.
Branching Patterns
In our study out of 40 cadaver, right and left sides, in 45 sides (56.25%), the infrahyoid branch and SLA were divided, followed by the sternocleidomastoid artery and the glandular thyroid branch (Type 1). Ozgur et al. (2009) [5] observed Type 1 in 31 sides (38.75%).
In seven cases (17.5%), the infrahyoid branch was divided and then the three branches (superior laryngeal, thyroid glandular and sternocleidomastoid branches) were divided at one point (Type 2). Ozgur et al. (2009) [5] observed Type 2 in six cases (15%).
4 sides (5%) showed Type 3 pattern where the infrahyoid branch and sternocleidomastoid artery were divided, followed by the SLA and the glandular thyroid branch. Ozgur et al. (2009) [5] Type 3 in seven cases (17.5%).
In our study, data on types of branching pattern did not show any statistical significance between the sides.
Hu et al. (2006) [11] observed that in Type I, 36%, the superior SLA is divided first, followed by sternocleidomastoid branch and thyroid branch. In Type II, 16%, the three branches are divided at one point. 10% of the cases are observed as Type III, where the sternocleidomastid is divided first from the STA, followed by the superior laryngeal branch and the glandular thyroid branch.
Conclusion
Our study validates the fact that the variations are very common in regards to site, surface, level of origin and branching pattern of superior thyroid artery, including its relationship in regards to its distance with the surrounding structures. To conclude STA may not always be the first branch arising from ECA and hence not reliable to use it to identify the ECA, proving that it will not be possible to always ligate the ECA below the origin of the STA. In-depth knowledge of the regional anatomy and refocusing on it will surely prevent or minimize blood loss during the surgery and thereby help to attain better surgical outcomes.
References
Skandalakis J (2004) Surgical anatomy: the embriyologic and anatomic basis of modern surgery. PMP, Athens, pp 7–108
Fancy T, Gallagher D 3rd, Hornig JD (2010) Surgical anatomy of the thyroid and parathyroid glands. Otolaryngol Clin North Am 43:221–227
Mansberger AR Jr, Wei JP (1993) Surgical embryology and anatomy of the thyroid and parathyroid glands. Surg Clin North Am 73:727–746
Lucev N, Bobinac D, Maric I, Drescik I (2000) Variations of the great arteries in the carotid triangle. Otolaryngol Head Neck Surg 122(4):590–591
Ozgur Z, Govsa F, Celik S, Ozgur T (2009) Clinically relevant variations of the superior thyroid artery:an anatomic guide for surgical neck dissection. Surg Radiol Anat 31:151–159
Shima H, Von Luedinghausen M, Ohno K, Michi K (1998) Anatomy of microvascular anastomosis in the neck. Plast Reconstr Surg 101:33–41
Luo CB, Teng MM, Chang FC, Chang CY (2006) Transarterial embolization of acute external carotid blowout syndrome with profuse oronasal bleeding by N-butyl-cyanoacrylate. Am J Emerg Med 24(6):702–708
Toni R, Della Casa C, Castorina S, Malaguti A, Mosca S, Roiti E, Valenti G (2004) A meta-analysis of superior thyroid artery variations in different human groups and their clinical implications. Ann Anat 186(3):255–262
Hayashi N, Hori E, Ohtani Y, Ohtani O, Kuwayama N (2005) Endo S Surgical anatomy of the cervical carotid artery for carotid endarterectomy. Neurol Med Chir 45(1):25–29
Va´zquez T, Cobiella R, Maranillo E, Valderrama FJ, McHanwell S, Parkin I, San˜udo JR (2009) Anatomical variations of the superior thyroid and superior laryngeal arteries. Head & Neck. https://doi.org/10.1002/hed.21077
Hu KS, Song WC, Kim SH, Choi SW, Han SH, Paik DJ, Kim HJ, KOh KS (2006) Branching patterns of the arterial branches supplying the middle vascular pedicle of the sternocleidomastoid muscle: a topographic anatomical study with surgical applications for the use of pedicles osteomuscular flaps. Surg Radiol Anat 28:7–12
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they has no conflict of interest.
Ethical Approval
We agree that our study is ethical and compliant with ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anand, A., Metgudmath, R.B. & Belaldavar, B.P. Topographic Evaluation of Superior Thyroid Artery-A Terrain to be Well Versed for Surgeon’s Knife. Indian J Otolaryngol Head Neck Surg 74 (Suppl 3), 5994–6000 (2022). https://doi.org/10.1007/s12070-021-02643-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02643-4