Abstract
Objective
To evaluate feasibility, safety and efficacy of a combination of screw fixation and cementoplasty for pathologic bone fracture.
Methods
In this single-center prospective study, all consecutive percutaneous screw fixations under assisted CT guidance for palliation and fracture treatment of pathologic bone fracture were reviewed from July 2019 to February 2021. The primary outcome measure was the procedures’ technical success, defined as the correct placement of the screw(s), without any complications. Secondary outcome measures were the safety, the procedures’ early analgesic effects and impacts on quality of life at 4 weeks.
Results
Technical success was achieved in 11/11 procedures (100%) among 11 patients. No major complications attributable to the procedure were noted. The mean pain scored significantly decreased at the initial follow-up: 8.0 ± 2.7 versus 1.6 ± 2.5 (p < 0.05). Opioid doses were statistically lower after procedure: 70.9 ± 37 versus 48.2 ± 46 mg/day (p < 0.05). The mean EQ5D score had significantly increased by the early post-procedure consultation: 42.5 ± 13.6 vs 63.6 ± 10.3 (p < 0.05).
Conclusion
Combination of percutaneous screw fixation and cementoplasty for pathologic bone fracture is feasible and safe. It is efficient to reduce pain, decrease the consumption of opioids and improve the quality of life at 4 weeks after the procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In oncology, therapeutic progress has allowed a significant increase in life expectancy. A growing number of cancer survivors live to more advanced metastatic stages [1]. Secondary bone lesions are increasing, which are responsible for pain, especially in case of a pathologic fracture [2].
Analgesics, radiotherapy and surgery are widely used in this context, but are not without side effects [3, 4]. Cementoplasty is an interventional radiology procedure that has improved the palliative management of bone lesions [5], providing resistance to compressive stress during weight-bearing activities [6, 7]. However, one of the main disadvantages of cement is its low resistance to torsional stress [8, 9]. Thus, cementoplasty alone is less effective on bones that are subjected to torsional stresses [5, 10,11,12,13].
Fixation using a combination of metal screws and cement provides resistance to torsional and compressive stress [14, 15]. In addition, it has been shown that combined use of cement significantly lowers the risk of secondary screw displacement in secondary bone lesions [16,17,18]. Combination of percutaneous screw fixation and cementoplasty is a mini-invasive procedure; it typically results in early mobilization, almost no blood loss, reduced risk of venous thromboembolism (VTE) [9, 19,20,21,22,23,24].
The aim of this prospective study was therefore to evaluate feasibility, safety and efficacy of combination of percutaneous screw fixation and cementoplasty for pathologic bone fracture.
Materials and Methods
Study Population
It is a single-center prospective observational study. The inclusion criteria for this study include participants selected for having percutaneous osteosynthesis with cementoplasty on a secondary fractured bone lesion in an oncologic setting. Medical decisions were based on patient pain and quality of life, patient oncology projections, the patients’ general conditions and ineligibility for surgical management.
Data Collection
The clinical evaluation included the evaluation of the performance status. The evaluation of the quality of life was conducted with the EQ5D (EuroQol 5 Dimensions) score [25]. The type and intensity of pain according to the Numerical Pain Rating Scale (NPRS) from 0 to 10 were assessed. The consumption of analgesics by step and by dosage was also evaluated. The opioid equivalent dose was calculated with an equianalgesic conversion table [26]. After the procedure, all patients had post-procedure consultations planned (at 1 month) together with systematic CT scans.
The objectives were to evaluate the feasibility, the safety and the efficacy of the procedure. Feasibility was defined as the technical success of the procedure, i.e., the correct placement of the screw or screws, without extrusion; safety was evaluated by the screening of complications during and at the end of the procedure, as well as during the follow-up period. The efficacy was evaluated by the analgesic effect of the procedure and its impact on quality of life, by comparing patients’ self-evaluation of pain (NPRS), quality of life (EQ5D) and consumption of opioids before and after the procedure.
Results
Procedures
From July 2019 to February 2021, 11 procedures were performed 11 patients with cancer and symptomatic bone metastases with pathologic fracture were included.
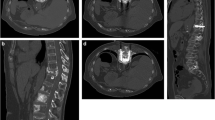
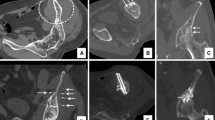
Preoperative clinical data are summarized in Table 1. One procedure example is illustrated in Fig. 1. The percutaneous procedures were performed under the control of a CT scanner and scopy. The aim of the procedure was to place one or several screw(s) across the lesions, through healthy bone on either side. The interventional radiologist positioned under direct control a wire through a coaxial needle, in order to insert titanium cannulated screw(s) of 4 mm or 6.5 mm diameter (ASNIS Stryker®). The number and diameter of the screws were defined according to the extent of the fracture, the lytic lesion and the nearby healthy bone. The use of CT guidance during the procedure allowed to check screw trajectory and to avoid possible complications.
One example. Sagittal (A) and axial (B) pre-procedure CT scan views: osteolytic lesion of the femoral neck (*) with pathologic fracture (black arrowheads); (C) sagittal CT scan view per procedure: three screws (white arrows) are positioned through the femoral neck lesion in three different orientations); sagittal (D) and axial (E) post-procedure CT scan views: the three screws (white arrows) cross the lesion and the cement (white arrowhead) is positioned around the screws; (F) 3D post-procedure reconstruction CT scan: the screws (white arrows) and cement (white arrowheads) fill the lesion and fracture
In all patients, 11-Gauge trocars were inserted (OnControl®, Teleflex; TCD®, Thiebaud), and then, the injection of polymethylmethacrylate cement (Palacos®- Heraeus Medical) was performed after screw insertion. In order to obtain optimal stabilization, cement was injected both into the lesion, at the end of the screws (in the healthy bone) and surrounding the screw. Potential adverse events and complications were also recorded with CIRSE and Clavien-Dindo classifications [27, 28]. The technical success of the procedure was defined as the correct placement of the screw(s), without any complications.
Technical success was achieved in 11/11(100%) procedures. In total, 16 screws were inserted (1.45 ± 0.7 per procedure). Iliac bone was the most frequent treated area.
Patients were able to get up within 24 h of the procedure in 90.9% of cases (10/11).
Adverse Events
Minimal cement leaks (small volume, leakage into the soft tissues) were noted in 3 procedures, which did not result in any consequences. In 2/11(18.2%) procedures, patients had complications: 1/11(9.1%) with a minor complication in the form of subcutaneous hematoma following screw insertion and 1/11(9.1%) with an asymptomatic pulmonary cruciate embolism (Clavien-Dindo 2 and CIRSE 3). The pulmonary embolism was discovered incidentally after the procedure during a usual oncological CT follow-up, and it was possibly unrelated to the procedure.
Clinical Outcomes at Initial Follow-up (4 weeks)
Clinical outcomes are summarized in Table 2. No displacement of material occurred during the follow-up. One patient died before completing the 4-week follow-up, of rapidly progressing metastatic disease. This death was unexpected and was considered to be unrelated to the procedure. All fractures were stabilized. The mean Pain Numerical Rating Scale (NPRS) dropped from 8 ± 2.7 to 1.6 ± 2.5 (p < 0.01) at the initial follow-up (4 weeks). Opioid use reduced significantly after procedure from 70.9 ± 37 to 48.2 ± 46 mg/d (p < 0.05) at 4 weeks.±
The mean EQ5D score significantly increased at the early post-procedure consultation from 42.5 ± 13.6 to 63.6 ± 10.3 (p < 0.01). One patient died before evaluation of quality of life.
Discussion
The present study showed excellent technical outcomes (100%) and a high rate of fracture stabilization (100%: 11/11). These findings are consistent with previous studies [24].
Surgical treatment exposes them to a risk of morbidity [29] and longer hospitalization [4]. Thus, for patients with comorbidities and limited life expectancy, surgical options are not suitable. The procedure was accompanied by a short period of hospitalization and early standing-up. These findings are consistent with previous studies [18]. These elements are a definite advantage for these fragile patients. Moreover, our results demonstrate a significant and rapid improvement in pain and quality of life at 4 weeks. Findings also show a significant and rapid decrease in opioid. Opioid use is common in patients with bone metastases and represents a risk of side effects [30].
The development of percutaneous osteosynthesis associated with cementoplasty has made it possible to safely and effectively treat patients who previously could not benefit from any effective surgical or interventional treatment.
This study is a prospective study to evaluate the analgesic efficacy of this intervention. Analgesic consumption was closely monitored, no patients were lost to follow-up, and there were no missing data. Quality of life was evaluated with the EQ5D scale, which is appropriate for prospective follow-up of quality of life in cancer patients [25].
The main limitations of our study include the single-center nature and the absence of a randomized control group. Furthermore, the evaluation of pain may have been affected due to other events and comorbidities related to age and treatments. Other therapies may confound pain scores in longer follow-up assessments.
Conclusions
This prospective study confirms that combination of percutaneous screw fixation and cementoplasty for pathologic bone fracture is feasible and safe. The novelty of the study results from its meticulous documentation of indicators of pain, quality of life, medication use and scan monitoring. Furthermore, it provides evidence about the procedures’ abilities to drastically reduce pain, consumption of analgesics and increase the quality of life at 4 weeks post-procedure.
Abbreviations
- CT:
-
Computed tomography
- CBCT:
-
Cone beam CT
- NPRS:
-
Numerical pain rate Score
- PS:
-
Performance status
- EQ5D:
-
EuroQol 5 dimensions
References
Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. 2006;12:6243s–9s.
van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18:1437–49.
Mastier C, Gjorgjievska A, Thivolet A, Bouhamama A, Cuinet M, Pilleul F, et al. Musculoskeletal metastases management: the interventional radiologist’s toolbox. Semin intervent Radiol. 2018;35:281–9.
Ristevski B, Jenkinson RJ, Stephen DJG, Finkelstein J, Schemitsch EH, McKee MD, et al. Mortality and complications following stabilization of femoral metastatic lesions: a population-based study of regional variation and outcome. Can J Surg. 2009;52:302–8.
Basile A, Giuliano G, Scuderi V, Motta S, Crisafi R, Coppolino F, et al. Cementoplasty in the management of painful extraspinal bone metastases: our experience. Radiol med. 2008;113:1018–28.
Anselmetti GC, Manca A, Ortega C, Grignani G, DeBernardi F, Regge D. Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Intervent Radiol. 2008;31:1165–73.
Kelekis A, Lovblad KO, Mehdizade A, Somon T, Yilmaz H, Wetzel SG, et al. Pelvic osteoplasty in osteolytic metastases: technical approach under fluoroscopic guidance and early clinical results. J Vasc Interv Radiol. 2005;16:81–8.
Lewis G. Properties of acrylic bone cement: state of the art review. J Biomed Mater Res. 1997;38:155–82.
Deschamps F, de Baere T, Hakime A, Pearson E, Farouil G, Teriitehau C, et al. Percutaneous osteosynthesis in the pelvis in cancer patients. Eur Radiol. 2016;26:1631–9.
Deschamps F, Farouil G, Hakime A, Teriitehau C, Barah A, de Baere T. Percutaneous stabilization of impending pathological fracture of the proximal femur. Cardiovasc Intervent Radiol. 2012;35:1428–32.
Deschamps F, Farouil G, Hakime A, Barah A, Guiu B, Teriitehau C, et al. Cementoplasty of metastases of the proximal femur: is it a safe palliative option? J Vasc Interv Radiol. 2012;23:1311–6.
Beckmann J, Springorum R, Vettorazzi E, Bachmeier S, Lüring C, Tingart M, et al. Fracture prevention by femoroplasty—cement augmentation of the proximal femur. J Orthop Res. 2011;29:1753–8.
Cazzato RL, Buy X, Eker O, Fabre T, Palussiere J. Percutaneous long bone cementoplasty of the limbs: experience with fifty-one non-surgical patients. Eur Radiol. 2014;24:3059–68.
Buy X, Cazzato RL, Catena V, Roubaud G, Kind M, Palussiere J. Techniques de consolidation osseuse guidée par imagerie en oncologie: cimentoplastie et vissage. Bull Cancer. 2017;104:423–32.
Cai L, Zhang Y, Zheng W, Wang J, Guo X, Feng Y. A novel percutaneous crossed screws fixation in treatment of Day type II crescent fracture–dislocation: a finite element analysis. J Orthop Transl. 2020;20:37–46.
Cornelis FH, Deschamps F. Augmented osteoplasty for proximal femur consolidation in cancer patients: biomechanical considerations and techniques. Diagn Interv Imaging. 2017;98:645–50.
Garnon J, Jennings JW, Meylheuc L, Auloge P, Weiss J, Koch G, et al. Biomechanics of the osseous pelvis and its implication for consolidative treatments in interventional oncology. Cardiovasc Intervent Radiol. 2020;43:1589–99.
Deschamps F, Yevich S, Gravel G, Roux C, Hakime A, de Baère T, et al. Percutaneous fixation by internal cemented screw for the treatment of unstable osseous disease in cancer patients. Semin Intervent Radiol. 2018;35:238–47.
Pusceddu C, Fancellu A, Ballicu N, Fele RM, Sotgia B, Melis L. CT-guided percutaneous screw fixation plus cementoplasty in the treatment of painful bone metastases with fractures or a high risk of pathological fracture. Skeletal Radiol. 2017;46:539–45.
Mavrovi E, Pialat J-B, Beji H, Kalenderian A-C, Vaz G, Richioud B. Percutaneous osteosynthesis and cementoplasty for stabilization of malignant pathologic fractures of the proximal femur. Diagn Interv Imaging. 2017;98:483–9.
Cazzato RL, Koch G, Buy X, Ramamurthy N, Tsoumakidou G, Caudrelier J, et al. Percutaneous image-guided screw fixation of bone lesions in cancer patients: double-centre analysis of outcomes including local evolution of the treated focus. Cardiovasc Intervent Radiol. 2016;39:1455–63.
Tian Q-H, He C-J, Wu C-G, Li Y-D, Gu Y-F, Wang T, et al. Comparison of percutaneous cementoplasty with and without interventional internal fixation for impending malignant pathological fracture of the proximal femur. Cardiovasc Intervent Radiol. 2016;39:81–9.
Roux C, Tselikas L, Yevich S, Sandes Solha R, Hakime A, Teriitehau C, et al. Fluoroscopy and cone-beam ct–guided fixation by internal cemented screw for pathologic pelvic fractures. Radiology. 2019;290:418–25.
Dassa M, Roux C, Tselikas L, Delpla A, Yevich S, Faron M, et al. Image-guided percutaneous fixation with internal cemented screws of impending femoral neck pathologic fractures in patients with metastatic cancer: safety, efficacy, and durability. Radiology. 2020;297:721–9.
Rabin R, de Charro F. EQ-SD: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–43.
Treillet E, Laurent S, Hadjiat Y. Practical management of opioid rotation and equianalgesia. JPR. 2018;11:2587–601.
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017;40:1141–6.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Hindiskere S, Kim H-S, Han I. Postoperative delirium in patients undergoing surgery for bone metastases. Medicine. 2020;99:e20159.
McNicol E. Opioid side effects and their treatment in patients with chronic cancer and noncancer pain. J Pain Palliat Care Pharmacother. 2008;22:270–81.
Acknowledgements
None.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
SG, SB, SM and RG elaborated the project. SG, SB and SM collected the data. SB, SG and RG performed the procedure and wrote the manuscript. All authors managed the patients, corrected and validated the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Ethical approval
This study has obtained approval from local research committee (“terre d’éthique” CHU Saint-Etienne IRBN942019/CHUSTE). The "clinical trial" document has been completed (NCT05191264).
Informed consent
Informed consent was obtained from all individual participants included.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bertholon, S., Grange, R., Thomas, T. et al. Combination of Percutaneous Screw Fixation and Cementoplasty for Lytic Bone Metastases: Feasibility, Safety and Clinical Outcomes. Cardiovasc Intervent Radiol 45, 1129–1133 (2022). https://doi.org/10.1007/s00270-022-03186-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03186-z