Abstract
Background
The decision to perform a total thyroidectomy (TT) for unilateral papillary thyroid microcarcinoma (PTMC) with nodules in the contralateral lobe remains controversial. The aim of this study was to investigate the rate of contralateral carcinomas that are preoperatively misdiagnosed as benign.
Methods
From October 2011 to October 2015, a total of 347 patients with unilateral PTMC and contralateral benign nodules who were treated with a TT at a single institution were enrolled. All patients underwent preoperative fine needle aspiration and ultrasonography (US). Clinicopathological features such as age, sex, laterality, tumor size, central lymph node metastases, capsular invasion, TgAb and TPOAb levels, Hashimoto’s thyroiditis, nodule number in both lobes according to preoperative US, and primary carcinoma number in the final postoperative pathology report were all analyzed to investigate the rate and predictive factors of contralateral carcinoma.
Results
A total of 100 patients (28.9 %) were diagnosed with papillary thyroid carcinoma in the contralateral lobe. A multivariate analysis showed that tumor size, nodule number in the contralateral lobe, and multifocality of the primary tumor were all independent predictive factors of contralateral carcinoma in patients with unilateral PTMC and contralateral benign nodules.
Conclusions
According to our findings, the rate at which contralateral carcinomas are preoperatively misdiagnosed as benign is 28.9 %. A TT is essential for unilateral PTMC with a primary tumor size >5 mm, multifocal primary carcinomas or multifocal benign nodules in the contralateral lobe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is known as the most prevalent type of thyroid cancer. In recent years, many reports have indicated that the incidence of PTC is increasing worldwide [1–3]. Whether this increase represents a true epidemic is unclear [4], because the most important explanation for the increase is improved imaging techniques such as ultrasonography (US) and US-guided fine needle aspiration (FNA). Therefore, an increasing number of cases of papillary thyroid microcarcinoma (PTMC), defined by the World Health Organization as a papillary carcinoma measuring 10 mm or less in the greatest diameter, have been detected [5]. Nevertheless, the surgical boundary and indication for treatment in patients with PTMC continue to be controversial topics. Generally, a total thyroidectomy (TT) is performed when the nodule is preoperatively confirmed to be malignant in bilateral lobes by FNA; further radioactive iodine treatment is administered for unilateral primary tumor metastases to the lateral lymph node [6, 7], and a lobectomy is usually more common for PTMC confined to the unilateral lobe. However, when a unilateral PTMC presents with benign nodules in the contralateral lobe on US, there are two choices. Most clinicians prefer a TT for fear of the risk of recurrent or persistent carcinoma in the remnant contralateral lobe. However, because PTMC is an indolent cancer with an approximately 97 % 10-year survival rate and low mortality [8], it is controversial whether all patients with PTMC confined to the unilateral lobe determined by FNA, or with benign nodules in the contralateral lobe, as determined by US, should be treated with TT. Similar studies have been previously published, but most of these reports involve heterogeneous study populations or do not provide detailed characteristics of the contralateral nodule [9–12]. The true incidence of contralateral PTC that is preoperatively considered benign by US is unknown.
The purpose of this study was to identify the prevalence of contralateral PTC and to analyze its predictive factors. We then further determined whether it is possible to avoid performing with conventional TT in some low-risk patients with PTMC.
Patients and methods
We retrospectively analyzed a total of 1608 consecutive patients who underwent initially surgery for the treatment of thyroid carcinoma at The Affiliated Taizhou Hospital, Wenzhou Medical College, between October 2011 and October 2015. The inclusion criterion was treatment with near-total thyroidectomy or TT with a tumor size ≤10 mm .Patients treated with a TT for the following reasons were excluded: pathological types of thyroid malignancies other than PTC, preoperative confirmation of bilateral PTC, incidental detection of PTC after thyroidectomy due to a large multinodular goiter, treatment with postoperative radioactive iodine 131 despite the absence of a nodule in the contralateral lobe, and lack of a preoperative examination. The detailed inclusion and exclusion criteria and selection steps are shown in the flowchart (Fig. 1). Finally, this study enrolled 347 patients with PTMC confined to a unilateral lobe with benign nodules in the contralateral lobe. All the included patients underwent preoperative ultrasonography and FNA cytology of the suspicious lesions (marked hypoechogenicity on US, taller than wide in shape, speculated margin and calcification) in both lobes. According to the 2015 ATA guidelines and the Thyroid Imaging Reporting and Data System (TI-RADS), we defined sonographic patterns of very low suspicion (spongiform or partially cystic nodules without any of the sonographic features described in the low, intermediate, or high suspicion patterns) and benign (purely cystic nodules (no solid component)) as benign, equal to TI-RADS 2, 3. Because the risk of malignancy in low suspicion nodules is 5–10 %, we generally suggest that patients with US features highly suggestive of malignancy undergo FNA to pathologically determine whether the nodule is benign or malignant. A total of 78 (22.5 %) patients had a benign FNA biopsy. The selected patients were limited to those diagnosed with PTMC in a unilateral lobe, with at least one benign nodule in the contralateral lobe and without a suspicious tumor. After surgery, all specimens were routinely sectioned at 3 mm for histopathological examination by a single head and neck pathologist according to the recommendations of the World Health Organization. The study was approved by the local Institutional Review Board.
The preoperative and postoperative clinicopathological features were retrospectively analyzed and included the following variables: age, sex, primary tumor laterality, tumor size, central lymph node metastases, capsular invasion, Hashimoto’s thyroiditis, TgAb or TPOAb level, nodule number in both lobes according to preoperative US, and number of carcinomas in the primary lobe based on the final pathology report. We defined multifocality as more than one benign or malignant nodule in the same lobe, and we defined tumor foci in the contralateral lobe that were preoperatively detected as benign nodules by US, but determined to be malignant postoperatively by pathological analysis as occult contralateral carcinoma.
To identify differences between groups for specific variables, SPSS version 16 software (SPSS Inc, Chicago, IL) was used for statistical analysis. Univariate analysis was performed using Chi-square test or Fisher exact test. Multivariate analysis was performed using binary logistic regression to determine the predictive factor for contralateral carcinoma. A p value of <0.05 was considered to represent statistical significance.
Results
In total, 347 patients who underwent a TT were included in the study, and 100 patients (28.9 %) were diagnosed with contralateral occult carcinoma. This group included 88 women and 12 men with a median age of 48 ± 10 years. The preoperative clinical features were as follows: 54(54.0 %) patients were older than 45 years, 50 (50.0 %) primary tumors were located in the left lobe, 42 (42.0 %) patients had high TgAb or TPOAb levels (TgAb > 4.11 IU/ml, TPOAb > 5.61 IU/ml) in the routine preoperative examination, and 50 (50.0 %) and 66 (66.0 %) patients exhibited multifocal nodules in the primary and contralateral lobes, respectively (Table 1). In the pathological review, a primary tumor size >5 mm, central lymph node metastases, and capsular invasion were found in 76 (76.0 %), 28 (28.0 %) and 38 (38.0 %) patients, respectively. Hashimoto’s thyroiditis and multifocal carcinoma in the primary lobe were found in 26 (26.0 %) and 38(38.0 %) patients, respectively (Table 2).
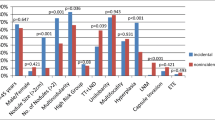
For the patients with clinically determined unilateral PTMC and benign nodules in the contralateral lobe, univariate analyses of potential preoperative and postoperative clinicopathological predictors associated with carcinoma of the contralateral lobe are shown in Tables 1 and 2. More than one benign nodule in the contralateral lobe according to preoperative US (p < 0.001), tumor size >5 mm (p = 0.002), and multifocal PTMC in the primary lobe (p < 0.001) in the final histopathology report all resulted in a significant difference in the presence of contralateral PTC. Age, sex, primary tumor laterality, central lymph node metastases, capsular invasion, Hashimoto’s thyroiditis, TgAb or TPOAb level, and nodule number in the primary lobe according to preoperative US were not significantly different between groups. The rates of occult contralateral thyroid carcinoma according to different independent predictive factors are shown in Table 3. Patients with multifocal benign nodules in the contralateral lobe exhibited a high rate of occult contralateral carcinoma compared with those with a single nodule (37.9 vs. 19.7 %, respectively). Similarly, tumor size >5 mm and multifocal PTMC in the primary lobe were also associated with a high rate of occult contralateral carcinoma.
The multivariate analysis also revealed that multifocality of the primary carcinoma in the unilateral lobe (p < 0.001, odds ratio = 3.565), tumor size (p = 0.003, odds ratio = 2.459), and the presence of multifocal benign nodules in the contralateral lobe according to the preoperative assessment (p < 0.001, odds ratio = 3292) were independent predictors of occult contralateral carcinoma in patients with clinically unilateral PTMC (Table 4).
Discussion
Although many treatment guidelines recommend that patients with PTC >1 cm and patients with bilateral PTMC according to the preoperative FNA results should undergo a TT [13], the optimal treatment for unilateral PTMC remains controversial, especially for patients with unilateral PTMC and benign nodules in the contralateral lobe as determined by US. Because the prognosis for patients diagnosed with PTMC is highly favorable [14], it is unknown whether clinicians should perform a TT for these patients.
In a previous study, researchers divided PTMCs into three different biological types that should be treated differently, and they demonstrated that almost 95 % of asymptomatic PTMC patients have type I, which encompasses incidentally detected, asymptomatic PTMCs that require only nonsurgical observation, which is an attractive alternative to surgery [15]. Moreover, the latest research from Japan showed that active surveillance might be the best choice for PTMC [16, 17]. In contrast, Wang et al. [18] indicated that bilateral PTC presented with a more advanced tumor stage and were associated with a shorter disease-free survival than unilateral PTC, and they suggested that bilateral PTC might exhibit worse biological behavior and a higher incidence of the BRAF (V600E) mutation. To identify a more appropriate treatment, further investigation of any possible predictive factors associated with contralateral carcinoma for patients with unilateral PTMC is indispensable. In our study, 28.9 % of the 347 patients who were preoperatively identified as having unilateral PTMC with benign nodule(s) in the contralateral lobe had occult contralateral carcinoma. This incidence rate was higher than the rate in other recently published studies [9–11]. This difference might have occurred because the patients in our study population all had benign nodules in the contralateral lobe according to routine US and did not have only unilateral PTMC preoperatively. From our standpoint, we can identify specific types of unilateral PTMCs that have a high risk of being contralateral carcinoma, and we can perform a TT for those high-risk cases rather than routinely performing a TT for all patients. Finally, we determined that multifocal benign nodules in the contralateral lobe according to preoperative US, tumor size, and multifocal primary carcinoma lobe in the postoperative pathological results were significant predictive factors for the risk of an occult contralateral carcinoma.
Among the preoperative indicators in our study, the presence of more than one benign nodule in the contralateral lobe according to US was significantly associated with contralateral carcinoma. Previous studies by Korean researchers determined that the presence of a likely benign nodule in the contralateral lobe was a significant predictive factor for the presence of an occult contralateral papillary carcinoma [9, 11]. Moreover, our study showed that multifocal benign nodules in the contralateral lobe were an independent risk factor for contralateral carcinoma. Although Frates et al. [19] observed that the likelihood of thyroid cancer per patient was independent of the number of nodules, and Kwong et al. [20] reported that the prevalence of clinically relevant thyroid nodules increases with advancing age despite a decreased risk that such nodules are malignant, we found that with preoperative unilateral PTMC, an increase in the number of nodules in the contralateral lobe was relevant to the increased risk of malignancy. This phenomenon might be related to intrathyroidal metastasis from a unilateral malignant focus, which has been demonstrated by several studies [21–23]. Moreover, the postoperative pathological results revealed that multifocality of the primary carcinoma was associated with a very high odds ratio in the presence of occult contralateral carcinoma, regardless of whether the multifocal lesions displayed unfavorable features in preoperative US. This finding is similar to the results of a study by Lee et al. [10], in which multifocality in the ipsilateral lobe of the primary cancer was found to help predict the possibility of contralateral carcinoma. However, we should also consider misdiagnoses by US evaluation and FNA biopsy because incorrect interpretations might lead to a failure to recognize a malignancy, including misidentifying cystic or calcified nodal metastases for nodules in a multinodular thyroid, mistaking diffusely infiltrative thyroid carcinomas and multifocal carcinomas for benign disease, and failing to recognize microcalcifications in PTC [24]. In a previous report, the sensitivity of FNA biopsy for the diagnosis of thyroid lesions was as low as the negative predictive value of 66.3 %, particularly for small lesions [25]. Because preoperative US is the most important indication for surgery but is mainly based on the radiologist’s individual subjective opinion, all clinicians should be aware of the US features that are associated with a poor outcome, thus leading to more appropriate treatment.
Eun et al. [11] reported that primary tumor size did not predict contralateral carcinoma and demonstrated that the absence of a well-defined margin in preoperative US was a significant risk factor for a contralateral carcinoma. Pitt et al. [12] also found that the risk of contralateral PTC is unrelated to the size of the primary tumor for PTC ≥ 1 cm; the risk was 30 vs. 24 % for tumors ≥1 cm and <1 cm, respectively (p = 0.43). In contrast, in our study, occult contralateral papillary carcinoma was significantly more frequent in patients with a tumor >0.5 cm according to postoperative pathology, which is consistent with the results of Lee et al. [9]. In addition, Ryu et al. [26] reported that PTC primary tumor size was significantly associated with T and N stages in the AJCC TNM staging system, which are independent predictors of multifocality and bilaterality. It has also been reported that patients with a tumor size >1 cm are more likely to have tumor recurrence in a regional lymph node [27].
In recent years, an increasing number of researchers have indicated that PTMC might be an over-treated malignancy. Ito et al. [28] found that PTMC was not associated with unacceptable characteristics regardless of patient background and clinical characteristics, and it would not be too late to perform surgical treatment after subsequent signs of progression, such as tumor enlargement and novel nodal metastasis. Therefore, a unilateral lobectomy or active observation in patients with a preoperative diagnosis of unilateral PTMC is more suitable than conventional TT, which is associated with more complications such as recurrent laryngeal nerve injury and hypoparathyroidism [29]. Considering that the rate of contralateral carcinoma was only 19.7 % (34/173) for patients with a single benign nodule in the contralateral lobe in our study, and considering patient’ needs and other extraneous factors [5], a TT is not mandatory and lobectomy might be an alternative [30, 31]. When the postoperative pathology indicates high-risk features such as multifocal carcinoma in the primary lobe, a thyroidectomy is a safe and appropriate option [32]. In our opinion, the patient’s considerations should not be ignored.
Conclusions
An occult contralateral carcinoma can be detected in only 19.7 % of PTMCs with a single nodule in the contralateral lobe, but it is detected in 37.9 % of PTMCs with multifocal nodules in the contralateral lobe. As postoperative clinical pathological indicators, multifocal primary carcinomas in the unilateral lobe and the pathological size of the primary carcinoma are also useful for predicting the risk of occult contralateral carcinoma. Consequently, to identify the optimal procedure, the significant risk factors mentioned above should be considered before surgery. In addition, the preferences of low-risk patients should be considered.
References
Leenhardt L, Grosclaude P, Cherie-Challine L (2004) Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid 14:1056–1060
Liu S, Semenciw R, Ugnat AM et al (2001) Increasing thyroid cancer incidence in Canada, 1970–1996: time trends and age-period-cohort effects. Br J Cancer 85:1335–1339
Chen AY, Jemal A, Ward EM (2009) Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer 115:3801–3807
Li N, Du XL, Reitzel LR et al (2013) Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the surveillance, epidemiology, and end results registry, 1980–2008. Thyroid 23:103–110
Schonberger J, Marienhagen J, Agha A et al (2007) Papillary microcarcinoma and papillary cancer of the thyroid ≤1 cm: modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin 46:115–120
Randolph GW, Daniels GH (2002) Radioactive iodine lobe ablation as an alternative to completion thyroidectomy for follicular carcinoma of the thyroid. Thyroid 12:989–996
Kiernan CM, Parikh AA, Parks LL et al (2015) Use of radioiodine after thyroid lobectomy in patients with differentiated thyroid cancer: does it change outcomes? J Am Coll Surg 220:617–625
Lei S, Ding Z, Ge J et al (2015) Association between prognostic factors and clinical outcome of well-differentiated thyroid carcinoma: a retrospective 10-year follow-up study. Oncol Lett 10:1749–1754
Koo BS, Lim HS, Lim YC et al (2010) Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol 17:1101–1105
Lee KJ, Cho YJ, Kim JG et al (2013) How many contralateral papillary thyroid carcinomas can be missed? World J Surg 37:780–785
Lee YC, Eun YG, Sohn YM et al (2015) Predictive factors for occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma by preoperative ultrasonographic and pathological features. World J Surg 39:1736–1741
Pitt SC, Sippel RS, Chen H (2009) Contralateral papillary thyroid cancer: does size matter? Am J Surg 197:342–347
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Sugitani I, Toda K, Yamada K et al (2010) Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J Surg 34:1222–1231
Miyauchi A (2016) Clinical trials of active surveillance of papillary microcarcinoma of the thyroid. World J Surg 40:516–522
Oda H, Miyauchi A, Ito Y et al (2016) Incidences of unfavorable events in the management of low-risk papillary microcarcinoma of the thyroid by active surveillance versus immediate surgery. Thyroid 26:150–155
Wang W, Zhao W, Wang H et al (2012) Poorer prognosis and higher prevalence of BRAF (V600E) mutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
Frates MC, Benson CB, Doubilet PM et al (2006) Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 91:3411–3417
Kwong N, Medici M, Angell TE et al (2015) The influence of patient age on thyroid nodule formation, multinodularity, and thyroid cancer risk. J Clin Endocrinol Metab 100:4434–4440
McCarthy RP, Wang M, Jones TD et al (2006) Molecular evidence for the same clonal origin of multifocal papillary thyroid carcinomas. Clin Cancer Res 12:2414–2418
Wang W, Wang H, Teng X et al (2010) Clonal analysis of bilateral, recurrent, and metastatic papillary thyroid carcinomas. Hum Pathol 41:1299–1309
Jovanovic L, Delahunt B, McIver B et al (2010) Distinct genetic changes characterise multifocality and diverse histological subtypes in papillary thyroid carcinoma. Pathology 42:524–533
Hoang JK, Lee WK, Lee M et al (2007) US features of thyroid malignancy: pearls and pitfalls. Radiographics 27:847–860
Ko HM, Jhu IK, Yang SH et al (2003) Clinicopathologic analysis of fine needle aspiration cytology of the thyroid. A review of 1,613 cases and correlation with histopathologic diagnoses. Acta Cytol 47:727–732
Baek HJ, Kim DW, Ryu JH (2015) Association between TNM staging system and histopathological features in patients with papillary thyroid carcinoma. Endocrine 48:589–594
Joo JY, Jin J, Seo ST et al (2015) Recurrence in regional lymph nodes after total thyroidectomy and neck dissection in patients with papillary thyroid cancer. Oral Oncol 51:164–169
Ito Y, Miyauchi A, Inoue H et al (2010) An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 34:28–35
Osmolski A, Frenkiel Z, Osmolski R (2006) Complications in surgical treatment of thyroid diseases. Otolaryngol Pol 60:165–170
Matsuzu K, Sugino K, Masudo K et al (2014) Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J Surg 38:68–79
Donatini G, Castagnet M, Desurmont T et al (2016) Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated? World J Surg 40:510–515
Rafferty MA, Goldstein DP, Rotstein L et al (2007) Completion thyroidectomy versus total thyroidectomy: is there a difference in complication rates? An analysis of 350 patients. J Am Coll Surg 205:602–607
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Wu, Z.G., Yan, X.Q., Su, R.S. et al. How Many Contralateral Carcinomas in Patients with Unilateral Papillary Thyroid Microcarcinoma are Preoperatively Misdiagnosed as Benign?. World J Surg 41, 129–135 (2017). https://doi.org/10.1007/s00268-016-3701-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3701-0