Abstract
Background
When surgeons decide to perform lobectomy as the treatment of papillary thyroid carcinomas (PTCs), they must consider the possibility of contralateral cancer. We wanted to determine the incidence of bilateral PTCs (bPTCs) and analyze their characteristics. We also wanted to determine how many patients with bPTC were missed preoperatively.
Methods
From January 2007 to May 2011, a total of 466 patients with PTC who were treated by total thyroidectomy at a single institution were enrolled. Patients were divided into two groups based on bilaterality. The patients with bPTCs were further investigated regarding the preoperative presence of the contralateral tumor.
Results
Bilaterality was seen in 29.8 % of PTC patients. In all, 36.8 % of PTCs ≥1 cm, and 25.7 % were papillary thyroid microcarcinomas (PTMCs). The presence of PTC in the contralateral lobe was missed in 15.8 % of bPTCs and in 21.3 % of bPTMCs. The rates of preoperatively nondetected contralateral cancer were 4.7 and 5.5 % for PTCs and PTMCs, respectively. Tumor size and multifocality were factors associated with bilaterality (p = 0.014 and p < 0.001, respectively).
Conclusions
Bilaterality is found more frequently when the tumor is large. Multifocality also can help predict the possibility of bilaterality. Therefore, total thyroidectomy may be necessary for patients with a multifocal or large tumor. It should be noted that the presence of a contralateral cancer is missed in 4.7 and 5.5 % of patients with preoperatively diagnosed unilateral PTC and PTMC, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is the most common subtype of thyroid cancer. The prognosis for patients with PTC is favorable, and disease progression is indolent. The 10-year survival rate is approximately 97 % [1]. The incidence of PTC, especially papillary thyroid microcarcinoma (PTMC)—defined by the World Health Organization (WHO) as PTC with a diameter <10 mm—is increasing worldwide because of improved imaging techniques and heightened awareness [1–3]. There is an ongoing debate about management of PTCs. Generally, clinicians choose simple lobectomy or total thyroidectomy with or without lymph node dissection. When the surgeon decides to perform lobectomy, the possibility of contralateral cancer must be considered. The true incidence of contralateral PTC that is not detected preoperatively but is diagnosed pathologically is unknown.
The aim of this study was to determine the incidence of bilateral PTC (bPTC) and analyze their characteristics. Also, we wanted to determine how many patients with bPTC were missed preoperatively.
Patients and methods
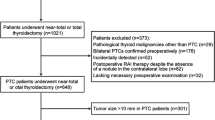
From January 2007 to May 2011, a total of 579 patients underwent surgery for PTC. Among them, 113 patients with lobectomy were excluded. Eventually this retrospective study enrolled 466 patients with PTC who were treated by total thyroidectomy at a single institution. The indication for total thyroidectomy included large tumor (usually >1 cm), advanced age (>45 years), nodule in the contralateral lobe, cervical node metastasis (including suspicious and confirmed cases), and extrathyroidal extension. However, these indications were not absolute.
The specimens were routinely sectioned every 3 mm. A single pathologist made all of the histologic diagnoses based on WHO recommendations. All patients underwent preoperative ultrasonography (IUS) evaluation for bilaterality. The data were retrospectively analyzed in relation to age, sex, central node metastasis, lymphovascular (LV) invasion, capsular invasion, extrathyroidal extension, multifocality, and bilaterality. Multifocality was defined as more than one cancer focus in the ipsilateral lobe of the primary cancer. Bilateral tumors were defined as tumors existing in both thyroid lobes. Bilaterality was diagnosed by preoperative fine-needle aspiration (FNA) or in the postoperative pathology report.
Patients were divided into two groups based on bilaterality, and the patients with bilaterality were further investigated for the preoperative presence of a contralateral nodule. Contralateral PTCs were divided into preoperatively confirmed, suspicious, and missed PTCs. We confirmed the contralateral PTCs by preoperative FNA. When patients had bilateral suspicious nodules on their first visit, they underwent FNA of both lobes. When patients were already diagnosed with ipsilateral PTC, they underwent US on the contralateral lobe to detect any contralateral tumor. When patients had a suspicious nodule in the unilateral lobe, they underwent FNA of the lobe and US to look for a contralateral tumor. A surgeon performed all of these procedures.
Suspicious US features were defined as hypoechoicity, microcalcification, increased central vascularity, infiltrative margins, and greater height than width in the transverse plane. Because most of the patients with contralateral nodules were supposed to undergo total thyroidectomy regardless of the results, FNA was skipped. PTCs not detected preoperatively were defined as “missed PTCs.”
To identify differences between groups for the clinicopathologic features, we used χ2 analysis, Fisher’s exact test, and binary logistic regression tests. A p value <0.05 was considered to represent statistical significance. The institutional review board of our hospital approved this study.
Results
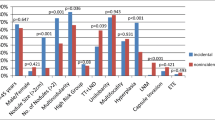
During the study period, 466 patients underwent total thyroidectomy. Among them, 139 (29.8 %) had bPTCs. Parameters were compared between the bilateral and nonbilateral groups of PTCs (Table 1). No significant difference between the groups were evident regarding age, sex, central node metastasis, capsule invasion, extrathyroidal extension, or LV invasion. A statistically significant difference was found for tumor size >1 cm (p = 0.011) and multifocality (p <0.001). Of the 292 patients with PTMC, 75 (25.7 %) had bilaterality. Tumor size >5 mm (p = 0.014) and multifocality (p < 0.001) were factors associated with bilaterality of PTMC (Table 2). On multivariate analysis, tumor size based on 1 cm and multifocality showed statistical significance with regard to bilaterality of PTC (Table 3).
Of the 466 PTC patients, 117 (25 %) had a contralateral tumor detected by preoperative US. Of the 292 patients with PTMC, 59 (20 %) had a contralateral tumor detected by preoperative US.
Of 139 patients with bPTC, 117 (84.2 %) had a contralateral tumor detected by preoperative US (Table 4). Contralateral PTC was confirmed in 42 patients (30.2 %) by preoperative FNA. In 49 patients (35.3 %), the tumor was a benign tumor; therefore, preoperative the FNA was skipped. In 26 (18.7 %), the contralateral tumor had suspicious features preoperatively. Contralateral tumor was not found in 22 (15.8 %) patients preoperatively, and PTC was the final diagnosis (Table 4). These patients represented 4.7 % (22/466) the total number of patients with PTC.
Of 75 patients with bPTMC, 59 (78.7 %) had a contralateral tumor preoperatively (Table 5). Also, 20 patients (26.7 %) had bPTMC preoperatively. In 28 patients (37.3 %), FNA was skipped because the contralateral tumor had benign features. In all, 11 patients (14.7 %) had suspicious features on US examination. Although 16 patients (21.3 %) were not diagnosed with contralateral tumor preoperatively, they were finally diagnosed as having bPTMC. They represented 5.5 % of the total patients with PTMC.
Discussion
The proper extent of surgery for PTMC has been debated. Consensus guidelines recommend total thyroidectomy for PTCs ≥1 cm and for patients with preoperatively detected bilateral PTMC [4]. However, the treatment of PTMC is still controversial. There are some indications for total thyroidectomy, but these indications are not absolute. They include large size (usually ≥1 cm), extrathyroidal extension, lymph node metastasis, presence of a contralateral tumor, and advanced age (>45 years). Despite these indications, total thyroidectomy is usually performed more often than lobectomy in our institution because of the risk of recurrence. It also provides the opportunity to give radioactive iodine therapy, address the possibility of contralateral cancer, and follow up the thyroglobulin levels. Many patients were transferred from the Department of Endocrinology to General Surgery, and the endocrinologists of our institution have asked us to perform total thyroidectomy—another reason we have chosen total thyroidectomy more often. During the study period, 80.5 % of the patients with PTC underwent total thyroidectomy.
We performed preoperative US on patients with PTC to detect the presence of a contralateral tumor. Although lobectomy was performed in a few patients with a contralateral benign tumor, most of the patients with a contralateral tumor regardless of malignancy underwent total thyroidectomy. Some of these patients underwent FNA to confirm the diagnosis of bPTC before surgery. Others with suspicious sonographic findings (including hypoechoicity, microcalcification, increased central vascularity, infiltrative margin, and greater height than width in the transverse plane) underwent total thyroidectomy without FNA preoperatively. The patients with a sonographically benign nodule in the contralateral lobe also did not undergo FNA. Even with preoperative US, however, a small PTC can be missed. Presently, the rate of missed lesions is 4.7 % for PTCs and 5.5 % for PTMCs.
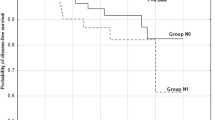
Bilaterality has clinical importance. Baudin et al. [5] found that the extent of surgery and multifocal PTMC were prognostic factors. PTMC with multifocality and tumor size >0.8 cm may be associated with a more aggressive course [6]. Wang et al. [7] reported that bPTC may be associated with more aggressive tumors, and the incidence of a BRAF mutation is significantly higher than that in unilateral PTC. In cases of PTC or PTMC with high risk, total thyroidectomy can be considered the proper treatment. However, bilaterality should be considered when a surgeon contemplates lobectomy for treatment. In particular, it is important that the final pathologic result shows bilaterality for preoperative unilateral PTMC. The studies of bilateral PTC are not well established because some patients undergo lobectomy only, and there is some inconsistency regarding the terminology. Mazeh et al. [2] divided multifocal tumors into ipsilateral, contralateral, and bilateral subgroups. Pitt et al. [8] defined multifocality as more than one tumor focus in the ipsilateral lobe of the primary tumor. Multifocality may or may not include bilaterality. In our study, we defined multifocality as more than one cancer focus in the ipsilateral lobe of the primary cancer.
Pitt et al. [8] reported that the rate of contralateral cancer was 30 % (48/158) for PTCs ≥1 cm and 26 % (18/70) for PTMCs. They demonstrated that the rate of contralateral PTC was independent of the primary tumor size, and that multifocal disease in the ipsilateral lobe of the primary tumor was a significant risk factor for a contralateral tumor. Grigsby et al. [9] also found that primary tumor size did not predict bilaterality. Mazeh et al. [2] reported rates of 57 % multifocality and 40 % bilaterality. They found that age <40 years was associated with a decreased rate of bilaterality. Other studies have reported rates of bilaterality that ranged from 13 to 56 % [10, 11]. Koo et al. [12] found that 16 % of the 132 patients with clinically unilateral PTMC had occult contralateral carcinoma. They reported that occult contralateral papillary carcinoma was significantly more frequent in patients with multifocality of the primary carcinoma in the unilateral lobe. In addition, they reported that the presence of a benign nodule in the contralateral lobe was a predictive factor for bilaterality.
Factors associated with PTC in the contralateral lobe have been reported. Lymph node metastasis found during the initial surgery, capsule invasion, the interval between lobectomy and completion thyroidectomy, and the presence of a tumor capsule have been related to bilaterality [13, 14]. Pasieka et al. [11] reported that multifocal disease in the primary resected lobe was associated with a high incidence of contralateral tumor. In our study, bilaterality occurred in 29.8 % (139/466) of PTCs, 36.8 % (64/174) of PTCs ≥1 cm, and 25.7 % (75/292) of PTMCs. These results are compatible with those in previous reports. When analyzing the association between bilaterality and other clinicopathologic features, we found that tumor size and multifocality were related to bilaterality. The same results were found on multivariate analysis.
The presence of multifocal PTC is a common clinical finding. It is not certain whether these foci are intraglandular metastases from a single primary tumor or individual tumors arising from distinct progenitor cells [15]. Iida et al. [16] reported that multiple lesions develop as a result of intraglandular dissemination. On the other hand, Shattuck et al. [15] noted that individual tumor foci in patients with multifocal PTC often arise as independent tumors.
Mazeh et al. [2] observed that the rates of multifocality and bilaterality in patients with PTMC were identical to those in patients with PTCs >1 cm. Therefore, they suggested that total thyroidectomy is required for all paitents with PTMC. Our data, however, showed a different rates of bilaterality for the PTC and PTMC subgroups (37 vs. 26 %, p = 0.011). As the tumor size enlarged, the rate of bilaterality increased. Our intention was to focus on the incidence of contralateral tumors that were missed preoperatively. The bilaterality that many studies have reported include both preoperatively confirmed cancers and missed cancers. We found that the rates of missed bilaterality were 15.8 % for bPTCs and 21.3 % for bPTMCs. The corresponding rates were 4.7 and 5.5 % for total PTCs and PTMCs, respectively. The rate of the bilateral cancers that were missed preoperatively was not very high and was not enough to change the trend of treatment. However, the problem should not be ignored. We have to consider the possibility of bilaterality before deciding the extent of surgery for PTC, especially in the case of PTMC, even though the preoperative evaluation may reveal only the presence of unilateral PTC or PTMC. Additionally, we should explain the possibility of bilaterality to the patients.
Pacini et al. [13] studied 182 patients with PTC who underwent completion thyroidectomy. They could not assess whether the tumor was present at the initial surgery or was a recurrence. However, they posited that the final outcome would probably be excellent in terms of survival. Also, they did not find any significant difference in the survival and recurrence rates between patients with unilateral or bilateral PTC. Based on the results of this study, we assume that a missed PTC does not have a strong effect on survival or recurrence.
Our study is limited by its retrospective nature and the investigation of cases from only a single institution. We think that a prospective study that includes more patients is necessary to verify our results. In addition, it is necessary to analyze long-term recurrence rates of bPTC and PTC without bilaterality. Another limitation is the fact that 19.5 % of the patients with PTC underwent lobectomy. Therefore, we do not know whether there are contralateral PTCs in those patients. To analyze the disease course of bPTC, we need longer study periods and more studies. There is an additional limitation. The specimens were routinely sectioned every 3 mm. We think that this distance is sufficient to miss small tumors.
Conclusions
Bilaterality was seen in 29.8 % of PTCs, 36.8 % of PTCs ≥1 cm, and 25.7 % of PTMCs. Bilaterality was found more frequently with large tumors. Multifocality can help predict the possibility of bilaterality. The rates of PTCs missed in the contralateral lobe were 15.8 % for bPTCs and 21.3 % for bPTMCs. Considering all PTCs and PTMCs, the rates of preoperatively missed contralateral cancers were 4.7 and 5.5 % respectively. These rates are not high enough to indicate total thyroidectomy for treatment of PTMC or PTC. However, total thyroidectomy may be necessary for patients with the aforementioned risk factors and it should be kept in mind that the presence of contralateral cancer was missed in 4.7 and 5.5 % of patients with preoperatively unilateral PTC or PTMC, respectively.
References
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Mazeh H, Samet Y, Hochstein D et al (2011) Multifocality in well-differentiated thyroid carcinomas calls for total thyroidectomy. Am J Surg 201:770–775
Hodgson NC, Button J, Solorzano CC (2004) Thyroid cancer: is the incidence still increasing? Ann Surg Oncol 11:1093–1097
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Baudin E, Travagli JP, Ropers J et al (1998) Microcarcinoma of the thyroid gland: the Gustave-Roussy Institute experience. Cancer 83:553–559
Haymart MR, Cayo M, Chen H (2009) Papillary thyroid microcarcinomas: big decisions for a small tumor. Ann Surg Oncol 16:3132–3139
Wang W, Zhao W, Wang H et al (2011) Poorer prognosis and higher prevalence of BRAF (V600E) mutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
Pitt SC, Sippel RS, Chen H (2009) Contralateral papillary thyroid cancer: does size matter? Am J Surg 197:342–347
Grigsby PW, Reddy RM, Moley JF et al (2006) Contralateral papillary thyroid cancer at completion thyroidectomy has no impact on recurrence or survival after radioiodine treatment. Surgery 140:1043–1047 discussion 1047–1049
Schonberger J, Marienhagen J, Agha A et al (2007) Papillary microcarcinoma and papillary cancer of the thyroid <or=1 cm: modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin 46:115–120 quiz N141–142
Pasieka JL, Thompson NW, McLeod MK et al (1992) The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg 16:711–716. doi:10.1007/BF02067365 discussion 716–717
Koo BS, Lim HS, Lim YC et al (2010) Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol 17:1101–1105
Pacini F, Elisei R, Capezzone M et al (2001) Contralateral papillary thyroid cancer is frequent at completion thyroidectomy with no difference in low- and high-risk patients. Thyroid 11:877–881
Miccoli P, Minuto MN, Ugolini C et al (2007) Intrathyroidal differentiated thyroid carcinoma: tumor size-based surgical concepts. World J Surg 31:888–894. doi:10.1007/s00268-006-0795-9
Shattuck TM, Westra WH, Ladenson PW et al (2005) Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med 352:2406–2412
Iida F, Yonekura M, Miyakawa M (1969) Study of intraglandular dissemination of thyroid cancer. Cancer 24:764–771
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, K.J., Cho, Y.J., Kim, J.G. et al. How Many Contralateral Papillary Thyroid Carcinomas Can Be Missed?. World J Surg 37, 780–785 (2013). https://doi.org/10.1007/s00268-013-1913-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-1913-0