Abstract
Background
Papillary microcarcinoma (PMC) of the thyroid generally follows a benign clinical course. However, treatment strategies remain controversial. According to our previous retrospective review of 178 patients with PMC who underwent surgery between 1976 and 1993, the most significant risk factors affecting cancer-specific survival were clinical symptoms at presentation due to invasion or metastasis. Distant metastasis and cancer-specific death were never seen postoperatively for 148 cases (83%) of asymptomatic PMC without clinically apparent (≥1 cm) lymph node metastasis or recurrent nerve palsy. Based on these results, we identified three biologically different types of PMC that should be treated differently. Type I comprises incidentally detected PMC without any symptoms, which is harmless and the lowest-risk cancer. Conservative follow-up with ultrasonography every 6 or 12 months is feasible. Type II involves the early stage of the usual low-risk papillary carcinoma. This can be treated by lobectomy when increasing size is noted during conservative follow-up. Type III comprises clinically symptomatic PMC, representing a high-risk cancer. Immediate wider resection followed by radioiodine treatment and suppression of thyroid-stimulating hormone is recommended.
Methods
Since 1995, we have been conducting a prospective clinical trial of nonsurgical observation for asymptomatic PMC. As of 2008, 230 of 244 candidates (94%) have decided to accept this policy, whereas 56 patients underwent surgery for symptomatic PMC between 1976 and 2006.
Results
Nonsurgical observation for a mean of 5 (range, 1–17) years for 300 lesions of asymptomatic PMC revealed that 22 (7%) had increased in size, 269 (90%) were unchanged, and 9 (3%) had decreased. No patients developed extrathyroidal invasion or distant metastasis. Three patients (1%) who developed apparent lymph node metastasis and nine patients (4%) in whom tumor increased in size eventually received surgery after 1–12 years of follow-up. No recurrences have been identified postoperatively. Conversely, 10-year cause-specific survival for symptomatic PMC was 80%. Multivariate analysis identified extrathyroidal invasion, large lymph node metastasis (≥2 cm), and poorly differentiated component as significantly related to adverse outcomes.
Conclusions
Nonsurgical observation seems to represent an attractive alternative to surgery for asymptomatic PMC. Almost 95% of asymptomatic PMC patients are type I, and another 5% are type II and can be treated with conservative surgery. A small number of PMCs with bulky lymph node metastasis or extrathyroidal invasion are high-risk type III and require aggressive treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary microcarcinoma (PMC) of the thyroid is defined as papillary thyroid carcinoma (PTC) with a diameter ≤ 1.0 cm according to the World Health Organization (WHO) histologic classification published in 1988 [1]. The recent widespread use of ultrasonography (US) and positron emission tomography (PET) for health screenings has increased the frequency of thyroid incidentalomas. In addition, the use of US-guided fine needle aspiration (FNA) has greatly facilitated the diagnosis of subclinical cancers.
Many autopsy series around the world also have shown surprisingly high prevalences of PMC, in up to 36% of patients dying from diseases other than thyroid cancer [2–6]. Similarly, the prevalence of “incidental” PMC, which had gone undetected on preoperative imaging studies but was identifiable on pathological examination of surgical specimens resected for benign thyroid diseases, ranges from 1.3% to 22% [7, 8]. In comparison, the incidence of clinically evident thyroid cancer is known to be only approximately 0.1–0.05% in the general population. PMCs are usually thought to remain harmless and asymptomatic throughout life. Indeed, many authors have reported excellent surgical outcomes for PMC [9, 10]. On the other hand, several investigators have reported that occasionally patients with PMC with bulky lymphadenopathy or with distant metastasis have experienced an unfavorable course [11–13].
Although PMC covers carcinomas with a wide range of biological malignancy, patients once diagnosed with PMC are uniformly recommended to undergo surgical treatment according to the current guidelines [14–17]. In the era of ultrasonographic diagnosis, appropriate treatment strategies are needed for individual patients with PMC, to identify patients in definite need of surgical treatment and to avoid overtreatment for the majority of patients with “innocent cancer.”
At the Cancer Institute Hospital, all patients with PMC routinely underwent surgery until 1993. In 1999, we published the results of a retrospective review of 178 patients with PMC between 1976 and 1993 to determine prognostic factors for disease mortality [18]. The most significant risk factors that affect cause-specific survival were the presence of clinically apparent (diameter ≥1 cm) lymph node metastasis and hoarseness due to recurrent nerve palsy at the time of diagnosis. All 4 cases of recurrence at the distant site and 4 cases of cancer-specific death occurred among the group of 30 patients with symptomatic PMC who showed cervical lymphadenopathy ≥1 cm, recurrent nerve invasion, or both. Conversely, neither distant metastasis nor cause-specific death was seen in the remaining 148 patients without those symptoms.
After these results, in 1995, we started a prospective clinical trial of nonsurgical observation for asymptomatic PMC based on the informed decision of the patient. The present study evaluated the validity and safety of this treatment option. On the other hand, we have continued to recommend surgery for PMC patients with symptoms due to metastasis and/or invasion.
As described previously [19–21], our initial surgical policy for PTC patients differs from most guidelines adopted recently in the United States and Europe. When a tumor was limited unilaterally, hemithyroidectomy of the affected side is the treatment of choice without postoperative radioactive iodine (RAI) ablation. This policy is based not only on the strict legal regulation of RAI in Japan, but also on the excellent postoperative outcomes of patients with low-risk PTC using this treatment modality [22]. We consider that total thyroidectomy with RAI therapy and TSH suppression therapy should be conducted only for patients with high-risk PTC. We previously proposed our own risk-group classification scheme for patients with PTC excluding PMC [19]. The present study retrospectively investigated clinical courses and risk factors for patients with symptomatic PMC, to discriminate patients who required aggressive treatment.
Materials and methods
Prospective clinical trial of nonsurgical observation for patients with asymptomatic PMC
The Cancer Institute Hospital is a tertiary oncology referral center in Tokyo, Japan. Since 1995, all patients with PMC diagnosed by US-guided FNA have been evaluated for the presence of distant metastasis, clinically apparent lymphadenopathy (≥1 cm), or extrathyroidal invasion using neck US, chest computed tomography (CT), laryngoscopy, and so on. For asymptomatic PMC patients, we provide information regarding the option of nonsurgical observation rather than immediate surgery. This information includes: (1) varieties of thyroid cancer and prognosis of PTC; (2) incidence of PMC by autopsy series or US screening tests compared with clinical PTC prevalence; and (3) risk of invasion, metastasis, and malignant transformation during nonsurgical follow-up. If the patient chooses observation, the tumor is surveyed by palpation, US, chest radiography or CT, with measurement of serum thyroglobulin (Tg) levels every 6 or 12 months. We recommend surgery during follow-up if the patient meets the following criteria: (1) change in patient preference; (2) PMC tumor has grown backward from the thyroid, toward adjacent structures, including the recurrent laryngeal nerve, trachea, and esophagus; (3) development of clinically evident lymph node metastasis or distant metastasis; or (4) increased tumor size. These protocols were approved by the ethics committee of the Cancer Institute Hospital. Written, informed consent is obtained after agreement based on the informed decision of the patient [23].
Diagnostic US was performed by a single radiologist (KY) who specializes in thyroid US using both B-mode (7.5-MHz transducer) and color-Doppler US to evaluate tumor size, multifocality, border of the tumor (regular or irregular), calcification pattern (absent, microcalcification, or coarse calcification), cervical lymph node metastasis, and blood supply to the tumor (poor or rich). Cytological diagnosis was made by a cytologist specializing in the thyroid (MK). She divided cases into two groups: common-type PTC, or suspected high-grade malignancy with characteristics, such as solid growth pattern or large nuclei.
Statistical analyses were performed by using Student’s t test or the Mann-Whitney test, as appropriate. Frequencies were compared using the χ2 test and Fisher’s exact probability test. Differences were considered significant for values of p < 0.05.
Retrospective study of treatment outcomes for patients with symptomatic PMC
During a 31-year period from 1976 through 2006, a total of 57 patients with symptomatic PMC underwent the initial thyroid surgery at the Cancer Institute Hospital. All patients had clinically apparent lymph node metastasis ≥1 cm in diameter. Eight of these patients proved to have carcinomas associated with hoarseness due to invasion of the recurrent laryngeal nerve by the primary tumor or metastatic node. In four patients, a clue to detection of the PMC was awareness of a small primary tumor. Only one patient showed distant metastasis. This 61-year-old woman initially showed distant metastasis in the brain, and metastases in the lungs and bone were subsequently identified. She also displayed a bulky (5.2 cm) lymph node metastasis from the 7-mm primary PMC at presentation and underwent resection of brain metastases, gamma knife therapy, total thyroidectomy with modified lateral neck dissection (MND), RAI therapy, TSH suppression, and periodic injection of bisphosphonate (zoledronic acid). As of the time of writing, she remains alive with the disease, 3 years after initial diagnosis. However, we excluded this case from the following analyses, because she had unusually extended symptoms at presentation.
The present series comprised 28 men and 28 women. Mean age at initial surgery was 56 (range, 19–80) years. Mean duration of follow-up was 11 (range, 2–31) years. As described earlier, we determined the extent of thyroidectomy by preoperative US, and total thyroidectomy was performed only when the tumor extended to the contralateral lobe, and/or when nodal metastasis was evident bilaterally in the neck. Lymph node dissection was performed on a selective therapeutic basis [21, 24]. Namely, limited dissection of the central compartment was conducted for patients with lymph node metastasis only in the central zone or with no metastasis at preoperative examinations. MND combined with central node dissection was performed only when the patient was diagnosed with lateral neck metastasis. Among the 56 patients, total thyroidectomy was used for 11 patients and less-than-total thyroidectomy for 45 patients. As for lymph node dissection, central zone dissection only was conducted in 9 patients, unilateral MND in 44 patients, and bilateral MND in 3 patients. All surgeries were macroscopically complete resections. No patients underwent RAI ablation as a primary treatment.
In this study, extrathyroidal invasion by the primary tumor or extranodal invasion by metastatic node was considered to be present only when the primary tumor or metastatic lymph node showed definite infiltration to surrounding organs, such as the trachea, esophagus, recurrent laryngeal nerve, jugular vein, or vagus nerve. Minimal extension to the sternothyroid muscle or perithyroid soft tissues or microscopic invasion that can be dissected sharply and can preserve the organs was not included. Because the diagnosis of PTC was based on 1988 WHO classifications [1], patients with poorly differentiated histological components at primary lesion or lymph node also were included in this series.
Survival curves were determined using the Kaplan-Meier method, and the statistical significance of differences was evaluated using the log-rank test. Statistical Analysis System software (SAS Institute, Cary, NC) was used for multivariate analysis of prognostic variables according to the Cox proportional hazards model. Values of p < 0.05 were considered statistically significant.
Results
Outcomes of nonsurgical observation for patients with asymptomatic PMC
From January 1995 to June 2008, a total of 244 patients were diagnosed to have asymptomatic PMC at our institution. Among these, 230 patients (94%) chose to undergo nonsurgical observation based on the information provided. The other 14 patients (6%) chose immediate surgery (total thyroidectomy, n = 1; hemithyroidectomy, n = 11; isthmusectomy, n = 2; central component lymph node dissection in all).
The 230 patients comprised 26 men and 204 women. Mean age was 54 (range, 23–84) years. The initial opportunity to detect PMC was cervical US in 186 patients, PET in 15 patients, neck or chest CT in 10 patients, magnetic resonance imaging (MRI) in 1 patient, and palpation in 10 patients. The remaining eight patients were diagnosed with PMC after neck dissection for other carcinoma including cancer of the esophagus (n = 3), tongue (n = 3), floor of the mouth (n = 1), and submandibular salivary gland (n = 1). These patients showed microscopic cervical lymph node metastasis of PTC and were proved to have small primary lesions in the thyroid. Including these 8 patients, 60 patients (26%) suffered from other kinds of carcinoma, such as carcinoma of the breast (n = 28), lung (n = 6), esophagus (n = 6), stomach (n = 5), colon (n = 4), tongue (n = 4) before PMC diagnosis. Among the 230 patients, 48 patients (21%) displayed multiple PMCs, with 2 lesions in 31 patients, 3 lesions in 13 patients, 4 lesions in 3 patients, and 5 lesions in 1 patient. As of June 2009, a total of 300 PMC lesions in 230 patients had been followed for 1 year or more. Because three patients have been followed since before 1995, the longest follow-up period was 17 years. The mean duration of follow-up was 5 years. Seven patients were lost to follow-up after 1–7 years of observation. Six patients died of other disease 1–8 years after the start of observation (breast cancer, n = 2; ovarian cancer, lung cancer, colon cancer, and pneumonia, n = 1 each).
Outcomes of nonsurgical observation are shown in Table 1. Increased or decreased tumor size on US was defined as a change in maximum diameter of the tumor ≥3 mm from the beginning of observation [25]. Fluctuations ≤ 3 mm were regarded as “no change.” After 1–17 years of observation, 22 of 300 lesions (7%) had increased in size. However, 269 lesions (90%) showed no change and 9 lesions (3%) had decreased in size. No patients developed extrathyroidal invasion or distant metastasis during follow-up, although three patients (1%) developed apparent nodal metastasis. We recommended surgery for these three patients and nine patients (4%) in whom tumor size increased after 1–12 years of follow-up. Four patients (2%) elected to undergo surgery 1–3 years after beginning observation, regardless of unchanged tumor status. Eventually, 16 patients (7%) underwent surgery despite initially choosing nonsurgical observation. These patients underwent total thyroidectomy in 2 cases and less-than-total thyroidectomy in 14 cases. As for lymph node dissection, unilateral MND was conducted for 2 patients and central zone dissection was performed for 14 patients. Postoperative courses were uniformly favorable. No postoperative complications (recurrent nerve palsy or permanent hypoparathyroidism), cancer recurrence, or cause-specific deaths were encountered.
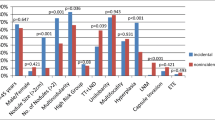
Clinical factors and US findings that affected the outcomes of nonsurgical observation were investigated (Tables 2, 3). Asymptomatic PMCs in younger patients tended to increase in size compared with those in older patients. However, sex, duration of follow-up, maximum diameter of the tumor at diagnosis, presence or absence of Hashimoto’s thyroiditis (anti-Tg and/or anti-thyroid peroxidase antibody), serum Tg at diagnosis, findings from FNA, and presence or absence of multiple lesions were not associated with outcome. As for US, 10 of 33 tumors (30%) with rich blood supply showed increased tumor size. This represented a significantly higher frequency than tumors with poor blood supply (4%). Regularity of the tumor border and calcification pattern were unrelated to outcomes.
Clinical courses and prognostic factors for patients with symptomatic PMC
Among the 56 patients with symptomatic PMC, 8 (14%) died of the disease and 8 died of other diseases (other cancer, n = 3; cerebrovascular failure, n = 2; asthma, n = 1; senility, n = 1; complications after vocal cord surgery, n = 1). Cause-specific survival rate (CSS) at 5, 10, and 20 years was 98%, 80%, and 53%, respectively (Fig. 1). Recurrence of PTC was seen in 21 patients (38%), with 1 in the remnant thyroid, 12 at the cervical lymph nodes, and 14 at distant sites. Disease-free survival rate (DFS) at 5, 10, and 20 years was 75%, 64%, and 55%, respectively (Fig. 2). In 12 patients (21%), extrathyroidal or extranodal invasion was seen at the following organs: recurrent laryngeal nerve by primary tumor in 3 cases and by metastatic lymph node in 5 cases; trachea by primary tumor in 1 case and by node in 2 cases; esophagus by primary tumor in 1 case and by node in 2 cases; jugular vein by node in 3 cases; vagus nerve by node in 1 case; and sternocleidomastoid muscle by node in 1 case.
The results of both univariate and multivariate analyses of preoperative or intraoperative (clinical) and postoperative (pathological) factors affecting DFS and CSS are shown in Tables 4 and 5. Extrathyroidal or extranodal invasion by the primary tumor or metastatic node, large lymph node metastasis (≥2 cm), and poorly differentiated component in the primary tumor or metastatic node were significantly related to adverse outcomes. Other factors, such as age, sex, primary tumor size, presence of multiple lesions, and number of metastasized lymph nodes, did not significantly affect survival. Although differences in CSS between symptomatic PMC patients with cancer invasion of adjacent organs or large nodal metastasis ≥2 cm (n = 41) and without both of these features (n = 15) were not significant (p = 0.10), none of the latter group died of the disease, whereas the 10-year CSS for the former group was 74% (Fig. 3).
Discussion
Davies et al. recently reported that the incidence of thyroid cancer in the United States increased from 3.6 per 100,000 in 1973 to 8.7 per 100,000 in 2002, representing a 2.4-fold increase [26]. The increasing incidence of thyroid cancer is predominantly due to the increased detection of small, subclinical PTCs. Indeed, mortality from thyroid cancer has remained stable during these 30 years. According to a recent meta-analysis by Roti et al., cancer-related death has rarely been reported in patients with PMC, corresponding to 32 of 9,379 patients (0.34%), and distant metastasis at diagnosis was seen in only 35 of 9,313 patients (0.37%) [27]. Furthermore, local/lymph node recurrences and recurrences at distant sites were seen in 231 (2.4%) and 26 (0.27%) of 9,379 patients with PMC, respectively. Regardless of these excellent results, most patients diagnosed with PTC in western countries now undergo total thyroidectomy, even if the cancer is microcarcinoma [27–32]. Total thyroidectomy has a small but significant risk of operative complications, such as permanent hypoparathyroidism. In addition, these policies commit the patient to a lifetime sentence of thyroid hormone replacement therapy. Cady, one of the first proponents of risk-group definitions for differentiated thyroid carcinoma, often has claimed that “punishment has to fit the crime” and has cautioned against overtreatment for low-risk PTC [33]. In the era when periodic health screening is gaining interest among the general population and sophisticated diagnostic procedures are improving, we have to establish adequate diagnostic and therapeutic strategies for patients with PTC based on individual risk of cancer-related morbidity and mortality. Particularly for patients with PMC, a more deliberate approach to avoid unnecessary investigations and surgery is needed.
Thus far, several studies have analyzed risk factors related to recurrence for patients with PMC. Roti et al. summarized that the following factors were important: younger age; clinically overt cancer; cancer multifocality; and lymph node involvement at diagnosis [27]. Few studies have been conducted to discriminate life-threatening factors in patients with PMC as of late, because very few patients die of this disease [9, 10, 28, 34, 35]. We performed a study analyzing risk factors related to 4 deaths among 178 patients with PMC and concluded that the most significant risk factors impacting cause-specific survival were symptoms resulting from metastasis and/or invasion [18]. Ito et al. also emphasized that PMC with clinically apparent metastasis, particularly in the lateral neck, shows aggressive biological behavior [36, 37]. In contrast, nodal metastasis that is only detected pathologically does not adversely affect the prognosis of PMC patients.
Combining these results with other evidence, such as the great discrepancy between the prevalence of latent or incidental PMC, we have reached the conclusion that three biologically different kinds of PMC exist and should be treated individually (Fig. 4). Type I comprises incidentally detected asymptomatic PMC, which remains harmless throughout the life of the patient. This is regarded as the lowest-risk cancer and nonsurgical observation with periodic US is feasible. Type II represents the early stage of the usual low-risk PTC and is sometimes accompanied by small lymph node metastasis and/or minimal invasion, but does not usually progress to a life-threatening cancer. Conservative surgery (hemithyroidectomy if the tumor is localized unilaterally) is recommended when an increase in size or development of clinically apparent lymph node metastasis is noted. Type III is a high-risk cancer accounting for some small proportion of clinically symptomatic PMCs. That is to say, size is not a criterion of safety; PTCs measuring ≤ 1 cm include both truly aggressive neoplasms and clinically insignificant tumors.
To confirm these hypotheses, we started a prospective clinical trial of nonsurgical observation for patients with asymptomatic PMC in 1995. As a result, 7% of patients eventually underwent surgery; however, no adverse outcomes, such as extrathyroidal invasion, distant metastasis, or anaplastic transformation, were seen among 300 lesions in 230 patients during 1–17 years of conservative follow-up. A similar trial was undertaken at Kuma Hospital in Japan. In 2003, they reported the results of an observation trial performed on 162 patients (22%) from 732 candidates [38]. The follow-up period ranged from 18 to 113 months, and >70% of patients showed no change in lesion size. In addition, no cases showing distant metastasis or extrathyroidal invasion were encountered, although 1.2% of patients developed lymph node metastasis and subsequently underwent surgery. Among patients with asymptomatic PMC, approximately 95% would be type I, and another 5% show type II and can be treated using conservative surgery. Although a much larger number of patients with longer follow-up is needed, we presently feel that nonsurgical observation based on the informed decision of the patient is feasible and seems to represent an attractive alternative to surgery, as long as the PMC remains asymptomatic.
As factors predicting outcomes of nonsurgical observation for patients with asymptomatic PMC, younger age and rich blood supply to the tumor proved to be related to increases in tumor size in our study. Among patients with PTC, an inverse correlation is usually seen between age and prognosis [19, 39–41]. However, PMC at a younger age might reserve some potential for growth to some extent. Cappelli et al. also noted the presence of intranodular vascularity as a predictor of unfavorable outcome in patients with PMC [30]. Biological aggressiveness of PMC may be reflected in not only Doppler US findings, but also in 18F-fluorodeoxyglucose (FDG)-PET uptake. Although PMCs initially detected by PET did not show significantly different courses compared with other cases (data not shown), an investigation of relationships between standard uptake value of FDG-PET in PMC and outcomes would be of great interest. Fukunaga and Yatani pointed out that the prevalence of the sclerosing variant decreases with larger tumors and suggested sclerosis as a defensive mechanism preventing tumor growth [5]. In our series, all 14 PMC lesions with completely sclerosing tumor border seen on US showed no change in tumor size. PMC with an ill-defined edge on US reportedly shows poorer DFS than PMC without such features [42]. However, our data did not show any significant relationship between appearance of the tumor border on US and outcomes of nonsurgical observation. Some investigators have stressed that intrathyroidal spread or multicentricity of PMC lesions is of considerable prognostic importance [27, 28, 34]. Our data did not show any significant relationship between this factor and changes in tumor size; however, two of three patients who developed clinically apparent lymph node metastasis during follow-up showed multiple lesions of PMC.
As for symptomatic PMC, Sanders and Rossi reported the therapeutic outcomes of 92 cases of occult well-differentiated carcinoma presenting with cervical adenopathy without palpable thyroid mass [12]. Cause-specific mortality was seen in five patients at the median follow-up of 18 years and all belonged to the older patient group (women >50 years, men >40 years). In the present series of 56 patients with symptomatic PMC, 10-year CSS was 80%, even when a patient with distant metastasis at presentation was excluded. In particular, PMCs with extrathyroidal invasion, including invasion by both primary lesion and metastatic node, bulky (≥2 cm) lymph node metastasis or poorly differentiated components correspond to Type III tumors. These PMCs definitely fall within the high-risk group of PTC, despite the small size of the primary lesion. Patients with such lesions might benefit from aggressive treatment, such as total thyroidectomy with RAI treatment and TSH suppression.
Investigations have been initiated recently to differentiate high-risk PTC from low-risk PTC using genetic markers, such as BRAF mutation [43, 44]. Before new markers can be developed to more precisely predict patients who are likely to be harmed by their disease and those who will live unaffected by the disease, our classification and individualized strategy for PMC may offer substantial clinical utility.
References
Hedinger CE, Williams ED, Sobin LH (1988) Histological typing of thyroid tumours. The WHO international histological classification of tumours, 2nd edn. Springer-Verlag, Berlin
Takahashi S (1969) Clinicopathological studies of latent carcinoma of the thyroid [in Japanese]. Nippon Naibunpi Gakkai Zasshi (Folia Endocrinol Japon) 45:65–79
Sampson RJ, Key CR, Buncher CR et al (1970) Papillary carcinoma of the thyroid gland: sizes of 525 tumors found at autopsy in Hiroshima and Nagasaki. Cancer 25:1391–1393
Sampson RJ, Woolner LB, Bahn RC et al (1974) Occult thyroid carcinoma in Olmsted country, Minnesota: prevalence at autopsy compared with that in Hiroshima and Nagasaki, Japan. Cancer 34:2072–2076
Fukunaga FH, Yatani R (1975) Geographic pathology of occult thyroid carcinomas. Cancer 36:1095–1099
Bondeson L, Ljungberg O (1981) Occult thyroid carcinoma at autopsy in Malmö, Sweden. Cancer 47:319–323
Olen E, Klinck GH (1966) Hyperthyroidism and thyroid cancer. Arch Pathol 81:531–535
Carlini M, Giovannini C, Mercadante E et al (2006) Incidental thyroid microcarcinoma in benign thyroid disease: incidence in a total of 100 consecutive thyroidectomies [in Italian]. Chir Ital 58:441–447
Noguchi S, Yamashita H, Uchino S et al (2008) Papillary microcarcinoma. World J Surg 32:747–753
Hay ID, Hutchinson ME, Gonzalez-Losada T et al (2008) Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 144:980–988
Allo MD, Christianson W, Koivunen D (1988) Not all “occult” papillary carcinomas are “minimal”. Surgery 104:971–976
Sanders LE, Rossi RL (1995) Occult well differentiated thyroid carcinoma presenting as cervical node disease. World J Surg 19:642–647
Sugitani I, Yanagisawa A, Shimizu A et al (1998) Clinicopathologic and immunohistochemical studies of papillary thyroid microcarcinoma presenting with cervical lymphadenopathy. World J Surg 22:731–737
Cobin RH, Gharib H, Bergman DA et al (2001) AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma. American Association of Clinical Endocrinologists. American College of Endocrinology. Endocr Pract 7:202–220
AACE/AME Task Force on Thyroid Nodules (2006) American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract 12:63–102
British Thyroid Association, Royal College of Physicians (2007) Guidelines for the management of thyroid cancer, 2nd edn. http://www.british-thyroid-association.org/news/Docs/Thyroid_cancer_guidelines_2007.pdf
The American Thyroid Association Guideline Taskforce (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–142
Sugitani I, Fujimoto Y (1999) Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J 46:209–216
Sugitani I, Kasai N, Fujimoto Y et al (2004) A novel classification system for patients with PTC: addition of the new variables of large (3 cm or greater) nodal metastases and reclassification during the follow-up period. Surgery 135:139–148
Sugitani I, Fujimoto Y, Yamamoto N (2008) Papillary thyroid carcinoma with distant metastases: survival predictors and the importance of local control. Surgery 143:35–42
Sugitani I, Fujimoto Y, Yamada K et al (2008) Prospective outcomes of selective lymph node dissection for papillary thyroid carcinoma based on preoperative ultrasonography. World J Surg 32:2494–2502
Sugitani I, Fujimoto Y (2009) Management of low-risk papillary thyroid carcinoma: unique conventional policy in Japan and our efforts to improve the level of evidence. Surg Today (in press)
Medical Professionalism Project (2002) Medical professionalism in the new millennium: a physicians’ charter. Lancet 359:520–522
Wada N, Duh QY, Sugino K et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Ito Y, Miyauchi A (2007) A therapeutic strategy for incidentally detected papillary microcarcinoma of the thyroid. Nat Clin Pract Endocrinol Metab 3:240–248
Davies L, Gilbert Welch H (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Roti E, degli Uberti EC, Bondanelli M et al (2008) Thyroid papillary microcarcinoma: a descriptive and meta-analysis study. Eur J Endocrinol 159:659–673
Chow SM, Law SCK, Chan JKC et al (2003) Papillary microcarcinoma of the thyroid: prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Roti E, Rossi R, Trasforini G et al (2006) Clinical and histological characteristics of papillary thyroid microcarcinoma: results of a retrospective study in 243 patients. J Clin Endocrinol Metab 91:2171–2178
Cappelli C, Castellano M, Braga M et al (2007) Aggressiveness and outcome of papillary thyroid carcinoma versus microcarcinoma: a mono-institutional experience. J Surg Oncol 95:555–560
Van den Bruel A, Moreno-Reyes R, Bex M et al (2008) Is the management of thyroid nodules and differentiated thyroid cancer in accordance with recent consensus guidelines? Results of a national survey. Clin Endocrinol 68:599–604
Mazzaferri EL (2007) Management of low-risk differentiated thyroid cancer. Endocr Pract 5:498–512
Cady B (1998) Presidential address: beyond risk groups: a new look at differentiated thyroid cancer. Surgery 124:947–957
Pelizzo MR, Boschin LM, Toniato A et al (2006) Papillary thyroid microcarcinoma: prognostic factors, management and outcome in 403 patients. Eur J Surg Oncol 32:1144–1148
Rouxel A, Hejblum G, Bernier MO et al (2004) Prognostic factors associated with the survival of patients developing loco-regional recurrences of differentiated thyroid carcinomas. J Clin Endocrinol Metab 89:5362–5368
Ito Y, Tomoda C, Uruno T et al (2004) Papillary microcarcinoma of the thyroid: how should it be treated? World J Surg 28:1115–1121
Ito Y, Tomoda C, Uruno T et al (2004) Preoperative ultrasonographic examination for lymph node metastasis: usefulness when designing lymph node dissection for papillary microcarcinoma of the thyroid. World J Surg 28:498–501
Ito Y, Uruno T, Nakano K et al (2003) An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 13:381–387
Cady B, Rossi R (1988) An expanded view of risk group definition in differentiated thyroid carcinoma. Surgery 104:947–953
Hay ID, Grant CS, Taylor WF et al (1987) Ipsilateral lobectomy versus bilateral lober resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery 102:1088–1095
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1058
Ito Y, Kobayashi K, Tomoda C et al (2005) Ill-defined edge on ultrasonographic examination can be a marker of aggressive characteristic of papillary thyroid microcarcinoma. World J Surg 29:1007–1012
Rodolico V, Cabibi D, Pizzolanti G et al (2007) BRAFV600E mutation and p27kip1 expression in papillary carcinoma of the thyroid ≤ 1 cm and their paired lymph node metastases. Cancer 110:1218–1226
Lee X, Gao M, Ji Y et al (2009) Analysis of differential BRAFV600E mutational status in high aggressive papillary thyroid microcarcinoma. Ann Surg Oncol 16:240–245
Acknowledgment
This work was supported in part by the Foundation for the Promotion of Cancer Research in Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sugitani, I., Toda, K., Yamada, K. et al. Three Distinctly Different Kinds of Papillary Thyroid Microcarcinoma should be Recognized: Our Treatment Strategies and Outcomes. World J Surg 34, 1222–1231 (2010). https://doi.org/10.1007/s00268-009-0359-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0359-x