Abstract
Background
Cementless hemiarthroplasty is a widely used treatment for femoral neck fractures. Intra-operative femoral fracture occasionally occurs during the procedure, and the use of cerclage wire has been proposed to stabilize both the prosthesis and the bone. This study aimed to investigate the outcomes of cerclage wiring to manage intra-operative fractures occurring during cementless hemiarthroplasty in older patients with a femoral neck fracture.
Methods
Medical records and radiographs of older patients with femoral neck fractures who underwent hemiarthroplasty during 2009 to 2015 were retrospectively reviewed. Patients who received cerclage wiring were matched with a demographically matched control group that did not. Patients were followed for at least 12 months. Functional outcomes and health-related quality of life were evaluated by determining the distance of distal stem migration, Barthel Index, EuroQol-visual analog scale (VAS), and pain-VAS.
Results
Eighty-one patients were included, comprising 27 study group and 54 control group patients. A tapered wedge-shaped femoral prosthesis was implanted in all cases. No significant differences in distance of distal stem migration or rate of stem subsidence > 2 mm were observed between the case and control groups (subsidence rate 11.1 vs. 14.8%, respectively). There was also no significant difference in functional outcomes between groups.
Conclusion
Our results revealed a low mean distance of distal stem migration and a low subsidence rate. Functional outcomes and quality of life were similar between the two groups. Cerclage wiring technique is safe, and it should be routinely performed when intra-operative femoral fracture occurs during cementless hemiarthroplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a continually evolving global major public health concern. Osteoporosis leads to reduction in bone mass, which results in bone fragility [1]. Hip fracture is a common osteoporotic fracture among older adults that results in serious health consequences, including significant loss of mobility and 10–30% mortality within 1 year [2, 3]. The incidence of hip fracture in 1990 was estimated to be 1.7 million, with 72% of those fractures occurring in women. Hip fracture incidence is projected to increase to 3.9 million in 2025, and to 6.3 million in 2050 [4]. Since a large proportion of the world’s population lives in Asia and half of this population will be aged 80 years or more by 2025 (and some project that the figure could grow to 57% by 2050), the number of hip fractures is expected to progressively increase, with 37% and 45% of all hip fractures predicted to occur in Asia by 2025 and 2050, respectively [5]. In addition, certain adjustable risk factors, particularly nutritional status, are attributable to readmission following hip fracture. Models have been proposed that have shown effectiveness for mitigating the problem [6].
In general, hemiarthroplasty and total hip arthroplasty (THA) are recommended as surgical treatment options in older patients with a displaced femoral neck fracture. Hemiarthroplasty has demonstrated superior results relative to lower risk of re-operation and greater cost effectiveness [7, 8], and THA was reported to be associated with improved long-term functional outcomes [9]. However, the use of cemented and cementless prostheses remains controversial. Cemented hemiarthroplasty showed satisfying survivorship, with a cumulative incidence of revision for any reason at 20 years of only 3.5% [10]. In cemented hemiarthroplasty, acrylic bone cement is applied to reamed cancellous bone to form a mantle between the femoral component and the bone. Cemented hemiarthroplasty, however, is associated with a higher risk of complications, including fat emboli, cement emboli, and bone cement implantation syndrome (BCIS) [11, 12]. A retrospective investigation found that BCIS occurred in 25–30% of patients who underwent the cemented method, and 5–7% of patients developed severe BCIS that led to both early and late mortality [13]. The cementless technique was, therefore, introduced to minimize the risk of these associated complications [14]. The incidence of intra-operative fractures is significantly higher in cementless arthroplasty than in cemented arthroplasty [12, 15,16,17]. When this complication occurs, the use of cerclage wire is recommended for the management of intra-operative femoral fracture to maintain position and alignment of the femoral components, to ensure the stability of the prosthesis, and to prevent fracture propagation [18].
The outcomes of cerclage wire in this surgical setting remain unclear. Some studies reported post-operative subsidence, but all of those implants remained stable and no revision was required [19,20,21]. Accordingly, the aim of this study was to investigate the outcomes of cerclage wiring to manage intra-operative fracture occurring during cementless hemiarthroplasty in older patients with femoral neck fracture. Post-operative subsidence and functional outcome were specifically determined, and our findings were compared to those of a matched control group that received cementless hemiarthroplasty, but that did not have intra-operative fracture.
Materials and methods
A retrospective review of medical records and post-operative radiographs was conducted in patients with femoral neck fracture who underwent cementless hemiarthroplasty during January 2009 to December 2015 at the Department of Orthopaedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. Patients with one or more of the following conditions were excluded: femoral neck fracture caused by high-energy trauma, complex hemiarthroplasty (e.g., structural bone grafting or osteotomy), pathologic fracture, multiple fractures, and/or implantation of an earlier generation prostheses (e.g., Austin Moore or Thompson prosthesis). Patients were also excluded if there was no immediate post-operative radiograph of the operated hip. The protocol for this study was approved by the Siriraj Institutional Review Board (SIRB) (COA no. 437/2559[EC3]).
Patients who received cerclage wiring for an intra-operative femoral fracture (fracture group) while undergoing cementless hemiarthroplasty were compared with a matched control group of patients without intra-operative femoral fracture (no fracture group) at a ratio of 1:2. The case and control groups were matched according to age, gender, Dorr classification, and type of femoral prosthesis.
Surgical technique
All operations were performed via a posterolateral approach by one or more of ten surgeons (6 and 4 surgeons were arthroplasty and orthopaedic trauma surgeons, respectively). After exposure of the hip joint, the lesser trochanter was identified. Femoral neck resection was performed above the lesser trochanter based on measurement from the pre-operative template, with the aim of restoring proper leg length and femoral offset. In most cases, the femoral neck was resected approximately 1 cm above the lesser trochanter. The broach-only femoral canal preparation technique was used to prepare the canal before implantation of a tapered wedge-shaped femoral component. The femoral canal was broached to the size necessary to achieve stable fixation. Stable fixation was determined in the following three planes: axial, rotation, and flexion/extension. In this study, the following types of femoral stems were used: Corail stem (DePuy Synthes, Warsaw, IN, USA), Trilock stem (DePuy Synthes, Warsaw, IN, USA), and VerSys M/L taper stem (Zimmer, Warsaw, IN, USA). Posterior soft tissue structure was repaired in all cases. If intra-operative fracture of the femoral neck occurred, soft tissue dissection was performed to identify the extent of the fracture. After thorough evaluation of the fracture at the femoral neck, cerclage wires (1.5 mm in diameter; 316 stainless steel) were applied around the femoral neck superior to the lesser trochanter. The number of cerclage wires used was determined according to the discretion of the attending surgeon. If the fracture extended below the lesser trochanter, additional wiring was applied below the lesser trochanter to prevent fracture propagation. Patents in the control (no fracture) group were allowed full weight-bearing immediately after surgery, while those with intraoperative fracture were limited to partial weight-bearing for the first six weeks after surgery, after which they slowly progressed to full weight-bearing. All patients were followed for at least 12 months.
Data collection
Patient demographic and clinical data were collected, including age, gender, side, body mass index (BMI), Charlson comorbidity index, pre-fracture ambulatory status, and Dorr classification of the proximal femur. BMI was calculated using the formula: weight in kilograms divided by height in metres squared. Pre-fracture ambulatory status was categorized into three groups, as follows: non-ambulatory, ambulatory with assisting device, and ambulatory without assisting device. For Dorr classification, the shape and bone structure of the proximal femur were assessed and classified into one of the three following types: Type A exhibited thick cortices on the anterior-posterior radiographic view, and a large posterior cortex on the lateral view; type B exhibited bone loss from the medial and posterior cortices; and type C exhibited dramatically thin cortices with a fuzzy appearance on lateral radiographs [22]. Peri-operative data, including operative time, estimated blood loss, type of prosthesis, and length of hospital stay, were collected. Post-operative complications (e.g., fracture, dislocation, and wound complication) were also recorded. At the 12-month follow-up, the distance of distal stem migration was measured. In addition, activities of daily living, health-related quality of life, and the intensity of post-operative pain were assessed by using Barthel Index, EuroQoL, and pain-visual analog scale (VAS), respectively.
Radiographic evaluation
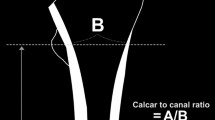
Anteroposterior radiographs were used to determine post-operative subsidence, loosening, and osteolysis. Immediate post-operative anteroposterior radiograph of both hips was evaluated as baseline information. The distance of distal stem migration was determined by the location of the tip of the greater trochanter relative to the superolateral position of the stem shoulder (Fig. 1). One assessor performed all measurements from radiographs in order to reduce measurement error. Twenty radiographs were selected to evaluate intra-observer and inter-observer reliability of this assessor’s measurement method. The intraclass correlation coefficient (r) for intra-observer reliability and inter-observer reliability was 0.999 and 0.990, respectively. The mean absolute difference between the first and second measurements by this assessor was approximately 0.3 ± 0.2 mm (range 0.05–0.74). Stem subsidence was diagnosed when the difference between the baseline and the latest follow-up distance of distal stem migration exceeded 2 mm [23]. Femoral component loosening was determined by the presence of a radiolucent line in 7 zones, as described by Gruen, et al. [24]. Failure of the femoral component was defined as a need for revision of the stem, evidence of radiographic loosening or failure, and/or severe hip or thigh pain.
Barthel Index
Barthel Index is a measurement tool that is used to rate a person’s ability to physically perform activities of daily living (ADL) [25]. The tool consists of ten items, each of which has a score that ranges from 1 to 10 (total possible score = 100). The higher the score, the greater the likelihood that a patient can live independently at home after discharge. The Thai version of the Barthel Index that was used in this study was reported to be valid and reliable [26]. Barthel Index is a validated outcome measurement tool for assessing functional recovery in elderly patients with femoral neck fracture [27].
EuroQol
EuroQol is a standardized instrument that is used for describing and evaluating health-related quality of life [28]. EuroQol contains four parts. The first two parts relate to health status (EQ-5D) and a visual analogue scale (EQ-VAS). The other two parts are specific to valuation and background information. Of those four EuroQol components, only EQ-VAS, which is a self-assessment scale, was used in this study. Each patient was asked to evaluate his or her health status on a visual analogue scale that ranged from 0 (worst health status) to 100 (best health status). The EQ-VAS was reported to be a reliable and valid tool for assessing health-related quality of life in elderly patients with femoral neck fracture [29].
Visual analogue scale
Visual analogue scale (VAS) is a commonly used tool to assess the intensity of post-operative pain. The VAS pain scale used in this study was a 10-cm vertical line labeled with “no pain” at the bottom, and “worst imaginable pain” at the top. Patients were asked to rate their pain by marking the point on the line that reflected their level of pain [30]. In this study, pain intensity was evaluated both at rest and during movement.
Statistical analysis and sample size calculation
A descriptive analysis was performed, and the results are presented as mean ± standard deviation and range for continuous variables, and as frequency and percentage for categorical variables. The Kruskal-Wallis test was used to differentiate normally distributed from non-normally distributed quantitative data. Case (intra-operative fracture) and control (no fracture) group quantitative data were compared using unpaired t test for normally distributed data and Mann-Whitney U test for non-normally distributed data. Qualitative data were compared between groups using either chi-square test or Fisher’s exact test. SPSS Statistics version 18 (SPSS, Inc., Chicago, IL, USA) was used to analyze the data. A p value less than 0.05 was regarded as being statistically significant.
To calculate the sample size, a pilot study was conducted to determine the mean distance of distal stem migration in five pairs of patients. Each pair of patients consisted of a patient with and a patient without intra-operative fracture. The mean result of that pilot study was 10.60 ± 7.08 mm and 6.50 ± 2.13 mm for the fracture group and no fracture group, respectively. Using a probability of a type I error of 0.05 and a power of 20%, a total of 36 patients (18 patients per group) was calculated. To compensate for a potentially high 1-year mortality rate among our cohort, the size of the study population was increased to at least 27 patients per group.
Results
There were 880 patients diagnosed with femoral neck fracture during the study period. Of those, 293 patients underwent cementless bipolar hemiarthroplasty. Intra-operative fracture of the femoral neck occurred in 52 patients (17.7%). Of these 52 patients, 17 patients died within one year after surgery, and eight patients were lost to follow-up. The remaining 27 patients with intra-operative fracture of the femoral neck (fracture group) were enrolled in this study. These patients were compared to a 54-patient matched control group (no fracture group) (1:2 study to control group ratio) based on age, gender, Dorr classification, and type of the femoral prostheses (Fig. 2).
The average follow-up time was 3.4 years (range 1–6) and 3.2 years (range 1–6) in the fracture group and the no fracture group, respectively. Patient demographic and baseline clinical characteristics are outlined in Table 1. The mean age was 79.3 years (range 58–93), and most (88.9%) subjects were women. Approximately 79% of patients could ambulate without the use of any assisting device before fracture, and 87.7% had a Charlson comorbidity index < 3. The most commonly used prosthesis was Corail stem (66.7%), followed by VerSys M/L taper (29.6%) and Trilock stem (3.7%). Most hips (83.9%) had a type B Dorr classification. There were no significant differences between groups for demographic or clinical characteristics, except that the right leg was significantly more often affected in the fracture group than in the no fracture group (p = 0.008) (Table 1). Most patients (74.1%) with intra-operative fracture had cerclage wiring above the lesser trochanter, whereas 11.1% and 14.8% of fracture group patients had cerclage wiring below the lesser trochanter and both above and below the lesser trochanter, respectively.
Concerning perioperative data, the mean operative time was 98.3 minutes (range 60–150) and 89.3 minutes (range 50–150) in the fracture group and the no fracture group, respectively (p > 0.05). The mean estimated total blood loss was 244.4 mL (range 50–900) in the fracture group, and 208.5 mL (range 20–700) in the no fracture group (p > 0.05). Length of hospital stay and length of postoperative stay were both significantly longer in the fracture group (both p < 0.05). No intra-operative complications other than intra-operative fracture were observed in either group (Table 2).
Evaluation of the latest post-operative radiograph of the operated hip revealed mean ± standard deviation distances of distal stem migration in the fracture and no fracture groups of 1.0 ± 0.9 mm (range 0–3.6) and 1.2 ± 1.0 mm (range 0–4.3), respectively (p = 0.58) (Fig. 3). There were three patients [11.1%, 95% confidence interval (CI) 3.9–28.1] in the fracture group that had stem subsidence greater than 2 mm, and eight patients (14.8%, 95% CI 7.7–26.6) in the no fracture group. No patients in this study had revision of the femoral stem, stem loosening, or osteolysis.
When comparing the functional outcome measure and health-related quality of life between groups, the mean Barthel Index was 78.0 ± 26.2 in the fracture group, and 83.5 ± 21.3 in the no fracture group (p = 0.10); and the EQ-VAS was 71.7 ± 16.1 in the fracture group, and 74.4 ± 17.2 in the no fracture group (p = 0.36). No significant differences were observed for pain-VAS at either rest or during activity between groups (Table 3).
Discussion
Hemiarthroplasty is a conventional treatment for older patients with a displaced femoral neck fracture [31]. However, the question whether cemented or cementless fixation is more efficacious in this surgical setting is still being debated. To date, both techniques have been widely used. Previous studies reported a preference for cementless fixation due to a shorter operative time and less blood loss, with both the cemented and cementless methods showing similar clinical results [16, 32].
Although cementless fixation has shown some distinct advantages over the cemented option, it was found to be associated with intra-operative and post-operative periprosthetic fracture [18, 33, 34]. Previous studies reported a wide range of incidence of intra-operative femoral fracture (3.7% to 19.5%) [19,20,21, 35, 36]. In the present study, the rate of intra-operative fracture of the femoral neck (17.7%) was considered high. Even though the causes of these fractures remain unclear, the authors speculate that the high rate of intra-operative fracture in this study may be related to the design of a particular femoral implant, since approximately 67% of intra-operative femoral fracture occurred in patients who received Corail stem. The Corail stem has a long femoral trunnion that creates a high vertical offset that may not be suitable for use in Asian population that normally have a small body frame and short vertical offset [37,38,39]. Devices with a long femoral trunnion may need to be driven further down into the metaphysis, potentially resulting in an intra-operative fracture of the femoral neck. This study, however, was not designed to evaluate association between the length of the femoral trunnion and the rate of intra-operative fracture. Future study to explore this issue is warranted.
All fractures in the fracture group received treatment with cerclage wiring to stabilize the implant. A biomechanical study found that placement of cerclage wiring to manage intra-operative femoral fracture in total hip arthroplasty increased the rotation and energy to failure [40]. That same study reported no significant difference between the fracture and no fracture groups for initial torsional stiffness of the prosthesis. Four previous in vitro studies reported the biomechanical properties of cerclage wires [40,41,42,43]. Prior studies investigated the subsidence rate of tapered wedge-shaped femoral stems, and the reported rates varied widely ranging from 1 to 81.6% [21, 44,45,46,47,48,49]. Barlas et al. [35] reported 5 mm subsidence in 1 out of 6 patients who received a hydroxyapatite ceramic-coated Furlong femoral component and that sustained an intra-operative femoral fracture that required fixation. Schewelov et al. [45] reported a subsidence rate of 81.6% in patients with femoral neck fracture that received total hip arthroplasty using an uncemented collarless Corail stem. In the present study, three patients (11.1%) in the fracture group and eight patients (14.8%) in the no fracture group demonstrated subsidence greater than 2 mm. Although our subsidence rate is comparable to the rates reported from those previous studies, it is difficult to compare subsidence rates due to variations in factors among studies, including patient characteristics, bone quality, definition of subsidence, and procedure (hemiarthroplasty versus total hip arthroplasty).
Our analysis of the peri-operative data revealed the length of hospital stay and the length of post-operative stay both to be significantly longer in the fracture group than in the no fracture group (p = 0.004 and p = 0.021, respectively). However, these were not unexpected results, because most surgeons tended to delay full weight-bearing and rehabilitation in the fracture group, which resulted in a longer post-operative stay. Regarding the use of cerclage wiring after intra-operative fracture, this study is the first to evaluate functional outcomes using Barthel Index, EQ-VAS, and pain-VAS. Since the outcomes were found not to be significantly different between the 2 groups, it can be inferred that the use of cerclage wiring was able to effectuate satisfactory outcomes after intra-operative fracture. This technique should, therefore, be considered a safe and effective method that should be routinely performed in all patients who receive cementless hemiarthroplasty using a tapered wedge-shaped femoral prosthesis and who develop intra-operative fracture of the femoral neck.
If intraoperative fracture of the femoral neck occurs, soft tissue dissection further down is necessary to identify the fracture extension at the femoral neck. After thorough evaluation of the fracture, one to two cerclage wires should be applied around the femoral neck superior to the lesser trochanter. If the fracture extends below the lesser trochanter, additional wires should be applied below the lesser trochanter to prevent fracture propagation. After cerclage wiring, stability of the stem should be re-evaluated. If stable fixation is not achieved with this cerclage wiring technique, change of the femoral stem to either cemented stem or full-coated cementless stem should be considered.
This study has some mentionable limitations. First and similar to all retrospective studies, this investigation was subject to some inherent biases relative to patient selection. Since the choice of femoral fixation was made at the discretion of each surgeon, it is possible that the bone quality of patients who received cemented fixation was poorer than the patients in this study that received cementless fixation. As such, it is possible that the rate of intra-operative fracture and subsidence could be much higher if cementless fixation was used in all patients with femoral neck fracture. In addition, the authors have no information or inadequate information regarding whether surgeons initially attempted to use tapered wedge-shaped cementless stem, but then changed to another type of cementless stem (full-coated) or cemented stem due to a failure to achieve immediate stability with a tapered wedge-shaped design. Nevertheless, the objective of this study was to evaluate the radiologic and functional outcomes of cerclage wiring to manage intraoperative fracture during cementless hemiarthroplasty. Second, due to the retrospective nature of this study, details regarding intra-operative fracture of the femoral neck, such as fracture location, extent of the fracture line, and at what point the fracture occurred, were not always recorded, so this information could not be included in our analysis. However, it is speculated that most fractures in this study were type AL fractures that occurred at the lessor trochanteric area according to Vancouver classification [50]. In this study, we estimated the length of intra-operative fracture based on the number of cerclage wires that were used to treat the intra-operative fracture. In most cases, cerclage wiring was applied above the lesser trochanter. If intra-operative fracture extended below the lesser trochanter, additional wires were applied below the lesser trochanter to prevent fracture propagation. In this study, the majority of patients in the fracture group (74.1%) had cerclage wiring only above the lesser trochanter. This information supports our speculation that most fractures were Vancouver type AL. However, the data limitations associated with the retrospective nature of our study limit the generalizability of our results, and we are not able to confidently conclude that cerclage wiring can be used or would be efficacious for the management all classifications of intra-operative femoral fracture. If a fracture is classified as Vancouver type B, which is a fracture that extends below the lesser trochanter, the subsidence rate and mean distance of distal stem migration may be higher.
The third limitation relates to the number of surgeons involved in this study. Because one or more of ten surgeons were involved in the treatment of these patients, the results of this study could have been affected by different surgical techniques and the level of expertise of each surgeon. However, all surgeons in this study were either an arthroplasty surgeon (6 surgeons) or an orthopaedic trauma surgeon (4 surgeons), and each of these surgeons has performed hemiarthroplasty in femoral neck fracture in more than 50 cases. We, therefore, believe the possible effect of this bias to be minimal. In addition, there was no significant difference in physician surgical specialty between the fracture and no fracture groups (p = 0.154). Moreover, since surgeons with different sub-specializations are involved in day-to-day treatment in real-world clinical settings, we feel that our data fairly and accurately reflects a real-world context. Fourth, our study had only one assessor to determine all radiographic measurements. Although we repeated radiographic assessment by two independent assessors at different time points in 20 radiographs after data collection to assess for inter-rater variability between assessors—none was identified. However, it must be acknowledged that our results could have been adversely influenced by some measurement-related bias. Last, the present study had a relatively short follow-up period. However, longer-term follow-up is difficult to study due to the short life expectancy in this patient population [51]. By way of example, 32.7% and 15.4% of patients in the intra-operative fracture group died and were lost to follow-up, respectively, during the mean three year follow-up period. Nevertheless, the mortality rate in this study is comparable to the rates reported in previous studies [52,53,54,55]. Pre-existing conditions might be the cause of the high mortality rate in geriatric hip fracture patients [56]. If all of the patients included in this study were still alive and evaluable, the subsidence rate and mean distance of distal stem migration could be higher or lower than the rates reported herein.
In conclusion, intra-operative femoral fracture is a common complication that can occur during implantation of a tapered-wedge cementless femoral prosthesis in older patients with femoral neck fracture. Cerclage wiring is required to manage this complication, to support the stability of the femoral component, and to forestall propagation of the fracture. Despite the lack of three important types of information relating to intra-operative femoral fracture (i.e., fracture location, extent of the fracture line, and at what point the fracture occurred), our results revealed a low mean distance of distal stem migration and a low subsidence rate in our study group. In addition, functional outcomes and health-related quality of life were both similar between those with and without intra-operative femoral fracture. These findings suggest the cerclage wiring technique to be safe, and that it should be routinely performed when intra-operative femoral fracture occurs during tapered-wedge cementless femoral prosthesis implantation.
References
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9(8):1137–1141. https://doi.org/10.1002/jbmr.5650090802
Millar WJ, Hill GB (1994) Hip fractures: mortality, morbidity and surgical treatment. Health Rep 6(3):323–337
Civinini R, Paoli T, Cianferotti L, Cartei A, Boccaccini A, Peris A et al (2018) Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit”. Int Orthop. https://doi.org/10.1007/s00264-018-4132-3
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2(6):285–289. https://doi.org/10.1007/BF01623184
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413. https://doi.org/10.1007/PL00004148
Stone AV, Jinnah A, Wells BJ, Atkinson H, Miller AN, Futrell WM et al (2018) Nutritional markers may identify patients with greater risk of re-admission after geriatric hip fractures. Int Orthop 42(2):231–238. https://doi.org/10.1007/s00264-017-3663-3
Wang Z, Bhattacharyya T (2017) Outcomes of hemiarthroplasty and total hip arthroplasty for femoral neck fracture: a Medicare cohort study. J Orthop Trauma 31(5):260–263. https://doi.org/10.1097/BOT.0000000000000814
Sonaje JC, Meena PK, Bansiwal RC, Bobade SS (2018) Comparison of functional outcome of bipolar hip arthroplasty and total hip replacement in displaced femoral neck fractures in elderly in a developing country: a 2-year prospective study. Eur J Orthop Surg Traumatol 28(3):493–498. https://doi.org/10.1007/s00590-017-2057-y
He JH, Zhou CP, Zhou ZK, Shen B, Yang J, Kang PD et al (2012) Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced femoral neck fractures in patients over 70 years old. Chin J Traumatol 15(4):195–200. https://doi.org/10.3760/cma.j.issn.1008-1275.2012.04.001
von Roth P, Abdel MP, Harmsen WS, Berry DJ (2015) Cemented bipolar hemiarthroplasty provides definitive treatment for femoral neck fractures at 20 years and beyond. Clin Orthop Relat Res 473(11):3595–3599. https://doi.org/10.1007/s11999-015-4462-z
Donaldson AJ, Thomson HE, Harper NJ, Kenny NW (2009) Bone cement implantation syndrome. Br J Anaesth 102(1):12–22. https://doi.org/10.1093/bja/aen328
Yli-Kyyny T, Ojanpera J, Venesmaa P, Kettunen J, Miettinen H, Salo J et al (2013) Perioperative complications after cemented or uncemented hemiarthroplasty in hip fracture patients. Scand J Surg 102(2):124–128. https://doi.org/10.1177/1457496913482249
Olsen F, Kotyra M, Houltz E, Ricksten SE (2014) Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and effect on outcome. Br J Anaesth 113(5):800–806. https://doi.org/10.1093/bja/aeu226
Bell KR, Clement ND, Jenkins PJ, Keating JF (2014) A comparison of the use of uncemented hydroxyapatite-coated bipolar and cemented femoral stems in the treatment of femoral neck fractures: a case-control study. Bone Joint J 96-B(3):299–305. https://doi.org/10.1302/0301-620x.96b3.32271
McGraw IW, Spence SC, Baird EJ, Eckhardt SM, Ayana GE (2013) Incidence of periprosthetic fractures after hip hemiarthroplasty: are uncemented prostheses unsafe? Injury 44(12):1945–1948. https://doi.org/10.1016/j.injury.2013.07.023
Ng ZD, Krishna L (2014) Cemented versus cementless hemiarthroplasty for femoral neck fractures in the elderly. J Orthop Surg (Hong Kong) 22(2):186–189. https://doi.org/10.1177/230949901402200214
Morris K, Davies H, Wronka K (2015) Implant-related complications following hip hemiarthroplasty: a comparison of modern cemented and uncemented prostheses. Eur J Orthop Surg Traumatol 25(7):1161–1164. https://doi.org/10.1007/s00590-015-1671-9
Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA (2008) Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J Bone Joint Surg Am 90(9):2000–2012. https://doi.org/10.2106/jbjs.h.00331
Berend KR, Lombardi AV Jr, Mallory TH, Chonko DJ, Dodds KL, Adams JB (2004) Cerclage wires or cables for the management of intraoperative fracture associated with a cementless, tapered femoral prosthesis: results at 2 to 16 years. J Arthroplast 19(7 Suppl 2):17–21. https://doi.org/10.1016/j.arth.2004.06.008
Capello WN, D'Antonio JA, Naughton M (2014) Periprosthetic fractures around a cementless hydroxyapatite-coated implant: a new fracture pattern is described. Clin Orthop Relat Res 472(2):604–610. https://doi.org/10.1007/s11999-013-3137-x
Unnanuntana A, Unkanawarapan H (2017) Short-term radiographic result of cementless hemiarthroplasty using taperer wedge-shaped femoral component in older patients with femoral neck fracture. J Med Assoc Thail 100(8):894–900
Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH (1993) Structural and cellular assessment of bone quality of proximal femur. Bone 14(3):231–242. https://doi.org/10.3290/j.qi.a39746
Bieger R, Cakir B, Reichel H, Kappe T (2014) Accuracy of hip stem migration measurement on plain radiographs: reliability of bony and prosthetic landmarks Orthopade 43(10): p. 934–939. https://doi.org/10.1007/s00132-014-3014-7
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res (141):17–27
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Laohaprasitiporn P, Jarusriwanna A, Unnanuntana A (2017) Validity and reliability of the Thai version of the Barthel Index for elderly patients with femoral neck fracture. J Med Assoc Thail 100(5):539–548
Unnanuntana A, Jarusriwanna A, Nepal S (2018) Validity and responsiveness of Barthel index for measuring functional recovery after hemiarthroplasty for femoral neck fracture. Arch Orthop Trauma Surg:1–7. https://doi.org/10.1007/s00402-018-3020-z
Brooks R (1996) EuroQol: the current state of play. Health Policy 37(1):53–72. https://doi.org/10.1016/0168-8510(96)00822-6
Tidermark J, Bergstrom G, Svensson O, Tornkvist H, Ponzer S (2003) Responsiveness of the EuroQol (EQ 5-D) and the SF-36 in elderly patients with displaced femoral neck fractures. Qual Life Res 12(8):1069–1079. https://doi.org/10.1023/A:1026193812514
DeLoach LJ, Higgins MS, Caplan AB, Stiff JL (1998) The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth Analg 86(1):102–106. https://doi.org/10.1213/00000539-199801000-00020
Roberts KC, Brox WT, Jevsevar DS, Sevarino K (2015) Management of hip fractures in the elderly. J Am Acad Orthop Surg 23(2):131–137. https://doi.org/10.5435/jaaos-d-14-00432
Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L (2009) Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res 467(9):2426–2435. https://doi.org/10.1007/s11999-008-0672-y
Dammerer D, Putzer D, Glodny B, Petersen J, Arrich F, Krismer M et al (2018) Occult intra-operative periprosthetic fractures of the acetabulum may affect implant survival. Int Orthop. https://doi.org/10.1007/s00264-018-4084-7
Kim SM, Han SB, Rhyu KH, Yoo JJ, Oh KJ, Yoo JH et al (2018) Periprosthetic femoral fracture as cause of early revision after short stem hip arthroplasty—a multicentric analysis. Int Orthop 42(9):2069–2076. https://doi.org/10.1007/s00264-018-3930-y
Barlas KJ, Ajmi QS, Bagga TK, Howell FR, Roberts JA, Eltayeb M (2008) Association of intra-operative metaphyseal fractures with prosthesis size during hemiarthroplasty of the hip. J Orthop Surg (Hong Kong) 16(1):30–34. https://doi.org/10.1177/230949900801600108
Kuo CL, Tan SH, Lee HC (2015) Intra-operative fractures in cementless bipolar hemiarthroplasty. J Orthop Surg (Hong Kong) 23(2):218–222. https://doi.org/10.1177/230949901502300222
Husmann O, Rubin PJ, Leyvraz PF, de Roguin B, Argenson JN (1997) Three-dimensional morphology of the proximal femur. J Arthroplast 12(4):444–450. https://doi.org/10.1016/S0883-5403(97)90201-1
Mahaisavariya B, Sitthiseripratip K, Tongdee T, Bohez EL, Vander Sloten J, Oris P (2002) Morphological study of the proximal femur: a new method of geometrical assessment using 3-dimensional reverse engineering. Med Eng Phys 24(9):617–622. https://doi.org/10.1016/S1350-4533(02)00113-3
Baharuddin MY, Kadir MRA, Zulkifly AH, Saat A, Aziz AA, Lee MH (2011) Morphology study of the proximal femur in malay population. Int J Morphol 29(4):1321–1325
ACt W, Owen JR, Wayne JS, Hess SR, Golladay GJ, Jiranek WA (2017) The effect of prophylactic cerclage wires in primary total hip arthroplasty: a biomechanical study. J Arthroplast 32(6):2023–2027. https://doi.org/10.1016/j.arth.2017.01.019
Lenz M, Perren SM, Richards RG, Muckley T, Hofmann GO, Gueorguiev B et al (2013) Biomechanical performance of different cable and wire cerclage configurations. Int Orthop 37(1):125–130. https://doi.org/10.1007/s00264-012-1702-7
Frisch NB, Charters MA, Sikora-Klak J, Banglmaier RF, Oravec DJ, Silverton CD (2015) Intraoperative periprosthetic femur fracture: a biomechanical analysis of cerclage fixation. J Arthroplast 30(8):1449–1457. https://doi.org/10.1016/j.arth.2015.02.026
Gordon K, Winkler M, Hofstadter T, Dorn U, Augat P (2016) Managing Vancouver B1 fractures by cerclage system compared to locking plate fixation—a biomechanical study. Injury 47(Suppl 2):S51–S57. https://doi.org/10.1016/s0020-1383(16)47009-9
Falez F, Santori N, Panegrossi G (1998) Intraoperative type 1 proximal femoral fractures: influence on the stability of hydroxyapatite-coated femoral components. J Arthroplast 13(6):653–659. https://doi.org/10.1016/S0883-5403(98)80009-0
Schewelov T, Ahlborg H, Sanzen L, Besjakov J, Carlsson A (2012) Fixation of the fully hydroxyapatite-coated Corail stem implanted due to femoral neck fracture: 38 patients followed for 2 years with RSA and DEXA. Acta Orthop 83(2):153–158. https://doi.org/10.3109/17453674.2011.641107
Lee YK, Joung HY, Kim SH, Ha YC, Koo KH (2014) Cementless bipolar hemiarthroplasty using a micro-arc oxidation coated stem in patients with displaced femoral neck fractures. J Arthroplast 29(12):2388–2392. https://doi.org/10.1016/j.arth.2014.04.020
Al-Najjim M, Khattak U, Sim J, Chambers I (2016) Differences in subsidence rate between alternative designs of a commonly used uncemented femoral stem. J Orthop 13(4):322–326. https://doi.org/10.1016/j.jor.2016.06.026
Kabelitz M, Fritz Y, Grueninger P, Meier C, Fries P, Dietrich M (2018) Cementless stem for femoral neck fractures in a patient’s 10th decade of life: high rate of periprosthetic fractures. Geriatr Orthop Surg Rehabil 9:2151459318765381. https://doi.org/10.1177/2151459318765381
Ries C, Boese CK, Dietrich F, Miehlke W, Heisel C (2018) Femoral stem subsidence in cementless total hip arthroplasty: a retrospective single-centre study. Int Orthop. https://doi.org/10.1007/s00264-018-4020-x
Masri BA, Meek RM, Duncan CP (2004) Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res 420:80–95. https://doi.org/10.1097/00003086-200403000-00012
Pioli G, Barone A, Giusti A, Oliveri M, Pizzonia M, Razzano M et al (2006) Predictors of mortality after hip fracture: results from 1-year follow-up. Aging Clin Exp Res 18(5):381–387
Franzo A, Francescutti C, Simon G (2005) Risk factors correlated with post-operative mortality for hip fracture surgery in the elderly: a population-based approach. Eur J Epidemiol 20(12):985–991. https://doi.org/10.1007/s10654-005-4280-9
Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J, Otto DD et al (2005) Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res 20(3):494–500. https://doi.org/10.1359/jbmr.041133
Carow J, Carow JB, Coburn M, Kim BS, Bucking B, Bliemel C et al (2017) Mortality and cardiorespiratory complications in trochanteric femoral fractures: a ten year retrospective analysis. Int Orthop 41(11):2371–2380. https://doi.org/10.1007/s00264-017-3639-3
Forni C, Gazineo D, D'Alessandro F, Fiorani A, Morri M, Sabattini T et al (2018) Predictive factors for thirty day mortality in geriatric patients with hip fractures: a prospective study. Int Orthop. https://doi.org/10.1007/s00264-018-4057-x
Bliemel C, Buecking B, Oberkircher L, Knobe M, Ruchholtz S, Eschbach D (2017) The impact of pre-existing conditions on functional outcome and mortality in geriatric hip fracture patients. Int Orthop 41(10):1995–2000. https://doi.org/10.1007/s00264-017-3591-2
Acknowledgements
The authors gratefully acknowledge Ms. Wachirapan Narktang of the Department of Orthopaedic Surgery for assistance with data collection, and Mr. Sutthipol Udompunthurak of the Division of Clinical Epidemiology, Department of Research and Development, Faculty of Medicine Siriraj Hospital, Mahidol University for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Unnanuntana, A., Saiyudthong, N. Outcomes of cerclage wiring to manage intra-operative femoral fracture occurring during cementless hemiarthroplasty in older patients with femoral neck fractures. International Orthopaedics (SICOT) 43, 2637–2647 (2019). https://doi.org/10.1007/s00264-019-04327-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04327-9