Abstract
Purpose
Due to pre-existing illnesses, elderly hip fracture patients represent a vulnerable patient population. The present study was conducted to investigate the effects of various pre-existing conditions on the outcomes of hip fracture patients.
Methods
A total of 402 surgically treated geriatric hip fracture patients were included in this prospective, single-centre study. Upon admission, patient age, gender and fracture type were documented, among other information. Patients were divided into six groups according to their pre-existing illness (neurological, cardiovascular, respiratory, gastrointestinal, renal or musculoskeletal). Outcomes in all six patient groups were measured using the following outcome parameters: length of hospital stay, mobility, functional results and mortality rate at discharge and at the one-year follow-up examination.
Results
Reduced values for the pre-fracture Barthel index (BI) were detected in patients with neurological (p < 0.001) and kidney-related diseases (p = 0.001). Neurological and kidney-related diseases were associated with reduced values on the BI (p < 0.001; p = 0.002) and Tinetti test (TT) (p < 0.001; p = 0.004) as well as an increased mortality rate (p < 0.001; p < 0.001) at the one-year follow-up. In addition, patients with respiratory (p = 0.004) and gastrointestinal disorders (p = 0.007) had an increased mortality rate in the medium term.
Conclusions
Pre-existing conditions are common among geriatric hip fracture patients. Pre-existing neurological and kidney-related diseases had the highest impact on functional outcomes and mortality rates at the end of acute care and in the medium term. In contrast to pre-existing cardiovascular disease, pre-existing neurological, kidney, respiratory and gastrointestinal disorders were also found to be associated with increased mortality rates in the medium term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to frailty and pre-existing conditions, elderly patients sustaining a hip fracture represent a vulnerable patient population. Prolonged hospital stays [1], a high rate of peri-operative complications [2] and increased mortality rates following the first post-operative year [3] are only a few indicators that support this assertion.
Many perioperative risk factors have previously been identified to improve the outcomes of hip fracture patients. Among them, the reduction of time to surgery [4], post-operative management in the intensive care unit (ICU) [5], implementation of ortho-geriatric co-management [6] and standardized relocation into rehabilitation facilities [7] represent approaches for improving the post-operative outcomes of geriatric hip fracture patients. Although such improvements in peri- and post-operative patient care have led to significant declines in complications and mortality rates, patient outcomes are still very much dependent on the pre-existing condition itself. In this context, many studies have investigated the effects of single comorbidities on outcomes in hip fracture patients. Among other pre-existing illnesses, e.g. dementia [8], Parkinson’s disease [9] and kidney failure [10] have been shown to be associated with inferior results in hip fracture patients.
The present study was performed to investigate the effects of different pre-existing diseases, categorized by organ systems, on the functional outcome and mortality rate in the peri-operative phase and at the one-year follow-up examination. The aim was to rank pre-existing conditions in regard to their impact on the outcomes of geriatric hip fracture patients.
Patients and methods
Patients aged ≥60 years who had sustained a hip fracture were included in this prospective, single-centre observational study. The criteria for exclusion was multiple trauma (Injury Severity Score (ISS) ≥ 16) and malignancy-associated fractures. All patients were surgically treated with either internal fixation or hip arthroplasty. The recruitment period was from April 1, 2009, to September 30, 2011. Approval was obtained from the local ethics committee for this study (AZ 175/08). Each patient or their legal representative gave written informed consent.
On admission to our hospital, patient age, gender, American Society of Anesthesiologists (ASA) score and fracture type were documented. Additionally, the time interval from hospital admission until surgery and the length of hospital stay were documented. The methods have previously been described in more detail in other publications including this patient cohort [11,12,13].
Assessment of pre-existing conditions
On hospital admission, previous medical conditions were recorded and classified into six different subgroups. The groups were categorized by pre-existing diseases related to the neurological system, cardiovascular system, respiratory system, gastrointestinal tract, kidneys or urinary tract and musculoskeletal system.
Diseases summarized under the term ‘neurological diseases’ included, for example, a diagnosis of Parkinson’s disease, Alzheimer’s disease, stroke, or dementia. Hypertension, myocardial infarction, heart valve damage, and pericarditis are examples of diseases that were included under the term ‘cardiovascular diseases’. Pre-existing diseases of the ‘respiratory system’ included a diagnosis of pneumonia, chronic obstructive pulmonary disease, lung cancer, or bronchial asthma. Diseases that were summarized as ‘gastrointestinal diseases’ included, for example, a diagnosis of gastrointestinal cancer, Crohn’s disease, colitis or gall bladder inflammation. Renal insufficiency, dialysis dependency, kidney cancer and urinary tract infection are examples of diseases that were classified as the ‘kidneys or urinary tract’. Pre-existing diseases summarized under the term ‘musculoskeletal system’ included a medical history of arthritis or fracture fixation, muscular dystrophy or gout.
Outcome parameters
Patient functional results were monitored using the Barthel index (BI) and Tinetti test (TT) at discharge as well as at one year postoperative. Furthermore, the overall lengths of hospital stay and the in-hospital mortality rate were documented at the time of hospital discharge and at the one-year follow-up examination.
Data entry and statistics
Data were collected in a FileMaker database® (FileMaker Inc., Santa Clara, CA, USA). Double entry with a plausibility check was performed to ensure data quality. IBM SPSS Statistics 22 (Statistical Package for the Social Sciences, IBM Cooperation, Armonk, N.Y., USA) was used for the statistical analysis.
The normality of the data distribution was determined using the Shapiro-Wilk test. Afterwards, for metric variables such as age, ASA score, BI, TT result and length of hospital stay, a Mann-Whitney U test was used to compare patients with different pre-existing comorbidities. Fisher’s exact test was performed to examine differences in categorical variables, such as gender distribution, type of surgery and the mortality rate, between patient groups. A chi-square test was conducted to determine the distribution of the different fracture types. For all tests, significance was assumed at p < 0.05.
Results
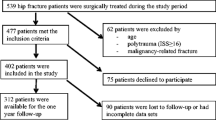
A total of 402 hip fracture patients who met the inclusion criteria participated in this study (Fig. 1). The baseline characteristics and treatment data for all patients are illustrated in Table 1. In addition, Table 1 provides patient data of the six different subgroups classified by pre-existing diseases.
Whereas, the subgroups of patients with pre-existing neurological (p = 0.002) and urinary diseases (p = 0.007) were significantly older, patients with conditions related to the respiratory (p < 0.001), gastrointestinal (p < 0.016) and urinary systems (p < 0.001) differed significantly in terms of gender distribution compared to the entire study population, with increased rates of males. No differences between the predefined subgroups and the entire study population were observed for the parameters ‘fracture location’ or ‘time to surgery’. Patients with a medical history of neurological (p = 0.002), cardiovascular (p < 0.001), respiratory (p = 0.022), gastrointestinal (p = 0.031) or kidney disease (p = 0.001) had significantly increased ASA scores compared to the entire study population. Whereas, pre-fracture functional abilities as measured by the BI were significantly worse among patients with pre-existing neurological (p < 0.001) and kidney diseases (p = 0.001), the length of hospital stay was significantly different only for patients with pre-existing neurological illness compared to the entire study population (p = 0.005).
An analysis of outcome parameters revealed pre-existing neurological and kidney diseases to be a risk factor for significantly inferior functional abilities. This was indicated by reduced values on the BI at discharge (neurological diseases, p = 0.001; kidney diseases, p = 0.001) and at the one-year follow-up examination (neurological diseases, p < 0.001; kidney diseases, p = 0.002) as well as by reduced values on the TT at discharge (neurological diseases, p = 0.001; kidney diseases, p = 0.001) and at the one-year follow-up examination (neurological diseases, p < 0.001; kidney diseases, p = 0.004) (Table 2).
Additionally, pre-existing kidney and gastrointestinal diseases were associated with an increased probability of dying during the acute care treatment (kidney diseases, p = 0.016; neurological diseases, p = 0.003). An analysis of the mortality rate at the one-year follow-up examination revealed pre-existing neurological (p < 0.001), respiratory (p = 0.007), gastrointestinal (p = 0.033) and kidney diseases (p < 0.001) to be other indicators for unfavourable clinical courses, at least in the medium term (Table 2).
Discussion
The current study aimed to analyse the impact of organ-specific, pre-existing conditions on the clinical course of geriatric hip fracture patients. The principal findings revealed that pre-existing neurological and kidney-related diseases favoured not only inferior functional results but also increased mortality rates at the end of acute care and in the medium term, respectively. Additionally, patients with pre-existing respiratory and gastrointestinal disorders had higher mortality rates in the medium term.
With 402 patients included in this prospective, observational study, the number of patients investigated was large compared to other single-centre studies on this topic [14, 15]. The predominantly female cohort included in this series is typical for a geriatric patient population with a comparatively high ASA score at hospital admission [16]. However, subgroup analysis of patients with pre-existing respiratory, gastrointestinal and kidney diseases revealed a significantly increased proportion of men compared to the total study population. As shown in cohort studies of Western industrial populations born before the year 1950, smoking is much more common among men than women [17]. This increased rate of male smokers most likely contributed to the shift in gender relations, especially in terms of pre-existing lung diseases such as chronic obstructive pulmonary disease, lung cancer and bronchial asthma, as well as in terms of gastrointestinal cancer and chronic renal failure. Regarding ASA scores, significantly elevated scores were noted in most of the subgroups with the exception of patients who presented with pre-existing musculoskeletal diseases. In this context, the musculoskeletal diseases, such as previous fractures or joint replacements, seemed not to affect the general health condition as much as diseases of other organ systems.
Interestingly, the period between trauma and surgical fixation was not affected in any of the investigated subgroups. Particularly, in the subgroup of patients with cardiovascular diseases, delays in ‘time to surgery’ were suspected to have occurred, as cardiovascular diseases are often associated with oral anticoagulation that must be compensated before hip surgery [18].
An increased average age was detected at the time of hospital admission among patients with neurological and kidney diseases. This circumstance might have contributed to the fact that in these two subgroups, patients were obviously more dependent, as indicated by significantly reduced pre-fracture BI values. For patients with pre-existing neurological illness, reduced skills in activities of daily living also led to a significant extension of the hospital stay. This effect could not be detected in patients with pre-existing renal disease.
Based on a prospective community-based study, Kisoli et al. investigated the level of functional disability, as measured with the BI, in a geriatric population including patients with different pre-existing neurological diseases [19]. Their study results indicated that patients with a diagnosis of a stroke, dementia or Parkinson’s disease were significantly more impaired than an unaffected background population. Similar results were published by Fritz et al. concerning motor impairments in patients with different types of neurological diseases [20]. In a prospective cross-sectional study, they showed that balance and gait impairments were quite common, as indicated by reduced values on the TT. Among the patients investigated, motor impairments were least severe in patients with a diagnosis of Alzheimer’s disease, more advanced in patients with a diagnosis of Parkinson’s disease and the most pronounced in those with Lewy body dementia. Therefore, the results of Kisoli et al. and Fritz et al. are consistent with our findings in terms of reduced activities of daily living and inferior motor abilities in neurologically ill patients. Additionally, reduced functional abilities were detected in the subgroup of patients with renal impairments in the present study, as measured by inferior values on the BI and the TT. Our results thus confirm the findings of Parsons et al., who published data on a population-based cohort study with more than 3000 elderly men [21]. Their study demonstrated that reduced physical activity was significantly associated with reduced chronic renal function as measured by the glomerular filtration rate. The results from a cross-sectional study published by Chao et al. further showed that acute kidney injury negatively influenced the functional status in geriatric patients, as measured by the BI [22]. In their study, the presence of an acute kidney injury was not only associated with a significantly lower BI but also increased severity of an acute kidney injury was associated with a significant decrease in the BI.
Based on our study results, patients with pre-existing kidney diseases were not only shown to be at risk for inferior functional results but also for increased mortality rates. This fatal inverse correlation between reduced scores on the BI and TT and an increased probability of dying has also been described by Morishita et al. [23]. In a review of the literature, they showed that impaired activities of daily living as well as reduced physical activities were associated with a higher mortality risk in patients with chronic kidney disease and in patients with a need for dialysis, respectively.
Similar results were observed for patients with pre-existing neurological diseases in the present study. Although the mortality rate during the acute care treatment failed to reach statistical significance, a significantly increased one-year mortality rate was discovered in this subgroup of patients. In this context, the results of the present study are consistent with those of Penrod et al. In an analysis of pooled data from three longitudinal studies on 2692 geriatric hip fracture patients, they showed that dementia had a significantly negative impact on survival at six months after hip fracture [24].
Elevated mortality rates for patients with respiratory and gastrointestinal diseases indicate the overall severity of diseases associated with these two pre-existing conditions. In contrast, musculoskeletal diseases failed to show an increased mortality rate, which is most likely due to their subordinate influence on the general disease severity as measured by the ASA score. Interestingly, cardiovascular diseases were also not associated with an increased mortality rate. This circumstance is most likely related to the fact that most of the patients were assigned to this subgroup because of pre-existing elevated blood pressure. As shown in a German population-based cohort study, the age-standardized overall prevalence of arterial hypertension is high, at 74% for men and 70% for women, respectively [25]. Nevertheless, due to an increase in anti-hypertensive medication consumption and a higher awareness of the condition itself, most of the negative effects correlated with hypertension are compensated, leading to overall insignificant mortality rates among patients in this subgroup.
Strengths and limitations
Despite a thorough study design, the results should be interpreted within the context of certain limitations. First, this was an observational study; thus, conclusions cannot be drawn in terms of causality, and the relationships described can only be interpreted as associations. Nevertheless, the present study examined and followed more than 400 prospectively enrolled patients with hip fractures, resulting in a large study compared to other single-centre studies on this topic.
Second, the conditions examined were only analysed in terms of organ systems and not in terms of single diseases, which prohibits the evaluation of the impact of each individual pre-existing disease. Although, as the purpose of the present study was to provide an organ system-based overview on the impact of pre-existing conditions on outcomes in a geriatric hip fracture population, this approach was the most applicable.
References
Motohashi T, Hamada H, Lee J, Sekimoto M, Imanaka Y (2013) Factors associated with prolonged length of hospital stay of elderly patients in acute care hospitals in Japan: a multilevel analysis of patients with femoral neck fracture. Health Policy 111:60–67. doi:10.1016/j.healthpol.2013.03.014
Bliemel C, Oberkircher L, Eschbach DA, Struewer J, Ruchholtz S, Buecking B (2013) Surgical treatment of proximal femoral fractures--a training intervention? Z Orthop Unfall 151:180–188. doi:10.1055/s-0032-1328395
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39:203–209. doi:10.1093/ageing/afp221
Morice A, Reina N, Gracia G, Bonnevialle P, Laffosse JM, Wytrykowski K, Cavaignac E, Bonnevialle N (2016) Proximal femoral fractures in centenarians. A retrospective analysis of 39 patients. Orthop Traumatol Surg Res. doi:10.1016/j.otsr.2016.09.025
Buecking B, Eschbach D, Koutras C, Kratz T, Balzer-Geldsetzer M, Dodel R, Ruchholtz S (2013) Re-admission to Level 2 unit after hip-fracture surgery — risk factors, reasons and outcome. Injury 44:1919–1925. doi:10.1016/j.injury.2013.05.012
Middleton M, Wan B, da Assunçāo R (2016) Improving hip fracture outcomes with integrated orthogeriatric care: a comparison between two accepted orthogeriatric models. Age Ageing. doi:10.1093/ageing/afw232
Ariza-Vega P, Jiménez-Moleón JJ, Kristensen MT (2014) Change of residence and functional status within three months and one year following hip fracture surgery. Disabil Rehabil 36:685–690. doi:10.3109/09638288.2013.813081
Maravic M, Ostertag A, Urena P, Cohen-Solal M (2016) Dementia is a major risk factor for hip fractures in patients with chronic kidney disease. Osteoporos Int 27:1665–1669. doi:10.1007/s00198-015-3429-y
Bliemel C, Oberkircher L, Eschbach DA, Lechler P, Balzer-Geldsetzer M, Ruchholtz S, Buecking B (2015) Impact of Parkinson’s disease on the acute care treatment and medium-term functional outcome in geriatric hip fracture patients. Arch Orthop Trauma Surg. doi:10.1007/s00402-015-2298-3
Lin ZZ, Wang JJ, Chung CR, Huang PC, Su BA, Cheng KC, Chio CC, Chien CC (2014) Epidemiology and mortality of hip fracture among patients on dialysis: Taiwan National Cohort Study. Bone 64:235–239. doi:10.1016/j.bone.2014.04.017
Bliemel C, Sielski R, Doering B, Dodel R, Balzer-Geldsetzer M, Ruchholtz S, Buecking B (2016) Pre-fracture quality of life predicts 1-year survival in elderly patients with hip fracture-development of a new scoring system. Osteoporos Int 27:1979–1987. doi:10.1007/s00198-015-3472-8
Buecking B, Struewer J, Waldermann A, Horstmann K, Schubert N, Balzer-Geldsetzer M, Dodel R, Bohl K, Ruchholtz S, Bliemel C (2014) What determines health-related quality of life in hip fracture patients at the end of acute care?--a prospective observational study. Osteoporos Int 25:475–484. doi:10.1007/s00198-013-2415-5
Eschbach DA, Oberkircher L, Bliemel C, Mohr J, Ruchholtz S, Buecking B (2013) Increased age is not associated with higher incidence of complications, longer stay in acute care hospital and in hospital mortality in geriatric hip fracture patients. Maturitas 74:185–189. doi:10.1016/j.maturitas.2012.11.003
Gordon M, Berntsson PO, Sjölund E, Demir Y, Hedbeck CJ, Stark A, Sköldenberg O (2016) Loss of offset after pertrochanteric hip fractures affects hip function one year after surgery with a short intramedullary nail. A prospective cohort study. Int Orthop 40:799–806. doi:10.1007/s00264-015-2815-6
Sharma G, Singh R, Gn KK, Jain V, Gupta A, Gamanagatti S, Farooque K, Sharma V (2016) Which AO/OTA 31-A2 pertrochanteric fractures can be treated with a dynamic hip screw without developing a lateral wall fracture? A CT-based study. Int Orthop 40:1009–1017. doi:10.1007/s00264-015-2835-2
Kannus P, Parkkari J, Sievänen H, Heinonen A, Vuori I, Järvinen M (1996) Epidemiology of hip fractures. Bone 18:57S–63S
Peters SA, Huxley RR, Woodward M (2014) Do smoking habits differ between women and men in contemporary Western populations? Evidence from half a million people in the UK Biobank study. BMJ Open 4:e005663. doi:10.1136/bmjopen-2014-005663
Ashouri F, Al-Jundi W, Patel A, Mangwani J (2011) Management of warfarin anticoagulation in patients with fractured neck of femur. ISRN Hematol 2011:294628. doi:10.5402/2011/294628
Kisoli A, Gray WK, Dotchin CL, Orega G, Dewhurst F, Paddick SM, Longdon A, Chaote P, Dewhurst M, Walker RW (2015) Levels of functional disability in elderly people in Tanzania with dementia, stroke and Parkinson’s disease. Acta Neuropsychiatr 27:206–212. doi:10.1017/neu.2015.9
Fritz NE, Kegelmeyer DA, Kloos AD, Linder S, Park A, Kataki M, Adeli A, Agrawal P, Scharre DW, Kostyk SK (2016) Motor performance differentiates individuals with Lewy body dementia, Parkinson’s and Alzheimer’s disease. Gait Posture 50:1–7. doi:10.1016/j.gaitpost.2016.08.009
Parsons TJ, Sartini C, Ash S, Lennon LT, Wannamethee SG, Lee IM, Whincup PH, Jefferis BJ (2017) Objectively measured physical activity and kidney function in older men; a cross-sectional population-based study. Age Ageing:1–5. doi:10.1093/ageing/afx091
Chao CT, Tsai HB, Wu CY, Hsu NC, Lin YF, Chen JS, Hung KY (2015) Cross-sectional study of the association between functional status and acute kidney injury in geriatric patients. BMC Nephrol 16:186. doi:10.1186/s12882-015-0181-7
Morishita S, Tsubaki A, Shirai N (2017) Physical function was related to mortality in patients with chronic kidney disease and dialysis. Hemodial Int. doi:10.1111/hdi.12564
Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, Silberzweig SB, Egol KA, Siu AL (2008) The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci 63:867–872
Lacruz ME, Kluttig A, Hartwig S, Löer M, Tiller D, Greiser KH, Werdan K, Haerting J (2015) Prevalence and Incidence of Hypertension in the General Adult Population: Results of the CARLA-Cohort Study. Medicine (Baltimore) 94:e952. doi:10.1097/MD.0000000000000952
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bliemel, C., Buecking, B., Oberkircher, L. et al. The impact of pre-existing conditions on functional outcome and mortality in geriatric hip fracture patients. International Orthopaedics (SICOT) 41, 1995–2000 (2017). https://doi.org/10.1007/s00264-017-3591-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3591-2