Abstract
Purpose
Osteoporotic hip fractures are increasing in prevalence with the growing elderly population. Morbidity and mortality remain high following osteoporotic hip fractures despite advances in medical and surgical treatments. The associated costs and medical burdens are increased with a re-admission following hip fracture treatment. This study sought to identify demographic and clinical values that may be a predictive model for 30-day re-admission risk following operative management of an isolated hip fracture.
Methods
Between January 1, 2013 and April 30, 2015 all patients admitted to a single academic medical centre for treatment of a hip fracture were reviewed. Candidate variables included standard demographics, common laboratory values, and markers of comorbid conditions and nutrition status. A 30-day, all-cause re-admission model was created utilizing multivariate logistic regression.
Results
A total of 607 patients with hip fractures were identified and met the inclusion criteria; of those patients, 67 were re-admitted within 30 days. Univariate analysis indicates that the re-admission group had more comorbidities (p < 0.001) and lower albumin (p = 0.038) and prealbumin (p < 0.001). The final, reduced model contained 12 variables and incorporated four out of five nutritional makers with an internally, cross-validated C-statistic of 0.811 (95% CI: 0.754, 0.867).
Conclusion
Our results indicate that specific nutritional laboratory markers at the index admission may identify patients that have a greater risk of re-admission after hip fracture. This model identifies potentially modifiable risk factors and may allow orthogeriatricians to better educate patients and better treat post-operative nutritional status and care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporotic hip fractures in the elderly are devastating injuries, which often lead to a substantial decline in function and independence [1,2,3]. Patients with osteoporotic hip fracture are often malnourished and have diminished physiologic reserves from multiple pre-existing comorbidities [4]. These comorbidities complicate post-operative recovery and may lead to hospital readmission [5]. Early re-admission (within 30 days of discharge) nearly doubles the one year mortality of patients who have undergone hip fracture treatment. Thus, there is substantial potential impact to outcomes if early re-admission can be prevented [5].
A multidisciplinary approach to managing hip fracture patients improves outcomes [6,7,8,9,10,11,12,13,14,15,16]. Geriatric fracture centres and orthogeriatric co-management by orthopedic surgeons and geriatricians have improved outcomes by decreasing re-admission rates, complications, length of stay, costs of care, and in-hospital mortality [15,16,17]. Despite improvements in care, the predictive factors associated with re-admission following a hip fracture are still largely unknown. Two risk models have previously been published; one using a locally-created ambulation score [18] and another examining the association between comorbidity as determined by American Society of Anesthesiologists Classification and outcomes [19]. Niether of these models accounts for a comprehensive evaluation of the patient’s admission status and identifies modifiable risk factors for re-admission.
We sought to create a predictive model incorporating markers easily collected through standard electronic medical records (EMR) including demographic characteristics, comorbidities, and markers of nutrition. We hypothesized that easily obtainable EMR variables could be used to predict risk of re-admission. Such risk stratification through this prediction model may then improve development of interventions and allocation of finite resources to the most at-risk patients. The authors also hypothesized that nutritional markers may add predictive value and help identify patients who may benefit from dietary intervention as a component of multidisciplinary in-hospital care for discharge management.
Materials and methods
The current study received Institutional Review Board approval and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients aged 50 and older admitted to our institution between January 1, 2013 and April 31, 2015 with a CPT procedure code (27,230, 27,232, 27,235, 27,236, 27,238, 27,240, 27,244, 27,245, 27,246, 27,248, 27,269) or International Classification of Diseases (ICD)-9-CM primary diagnosis code indicative of a hip fracture at the time of admission were retrospectively reviewed. Data was extracted from patients identified in the EMR with the following ICD-9 categories: “femoral neck fracture” (820.00), “subcapital fracture of hip” (820.09), “hip fracture, intertrochanteric” (820.21), “pathologic fracture of neck of femur, osteoporotic” (733.14), “hip fracture subtrochanteric” (820.22), and “other femoral hip fracture” (all other 820 codes not classified previously as these were not granular enough to distinguish different fracture types without chart review). “Open hip fractures” (820.9) were excluded. An index admission was defined for each patient based upon the first admission with presence of hip fracture according to the previously mentioned ICD-9-CM codes and inpatient or observational admission status. The final cohort was comprised of 607 patients. Patients were excluded from analysis if they did not have a primary diagnosis of a hip fracture, who sustained multiple injuries, died during index admission, or had a stay of less than one day.
Variables
All data were extracted from the EMR. The first variable identified confirmed if surgery occurred during the index hospitalization. Length of stay of index admission was defined as number of days between admission and discharge. Common demographic variables included age, gender, and race [20]. Median household income data from the 2013 American Community Survey based on patient census block group linked by geocoded address was incorporated as a marker of socioeconomic status. Smoking status was assessed by indicating whether the patient had ever or never smoked. Admission in the year prior to the index admission was coded dichotomously as experiencing or not experiencing an admission. Derived variables included the Charlson comorbidity index (CCI) [21], Glomerular filtration rate (GFR) [22], and body mass index (BMI) [20], which were calculated on the date of discharge. The last laboratory value prior to discharge was used as “baseline laboratory value” for each patient. The following laboratory markers were used as indicators of current health state at discharge: creatinine, haemoglobin, white blood cell count, alanine aminotransferase, and aspartate aminotransferase. Total protein, vitamin D, prealbumin, and albumin were considered nutritional markers. Re-admission was defined by the first all-cause observational or inpatient admission occurring within 30 days of the index admission.
Statistics
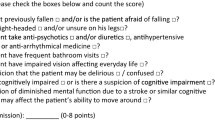
Data processing and statistical analyses were performed in R version 3.3.0. Missing data were imputed using the Multiple Imputation by Chained Equations (MICE) package for R, and included all predictors and outcomes variables used to build the regression model [23]. The imputation process was repeated five times with replacement. Logistic regression was used to model the 30-day all cause re-admissions. Continuous variables were fit using restricted cubic splines with three knots to relax normality assumptions [24]. The model that incorporated nutrition variables was reduced from 22 variables listed in Table 1 via Harrell’s model approximation method to create the most parsimonious model and to avoid overfitting [24]. This method ranks variables by order of importance, or contribution to the model’s R2, and excludes the weakest predictor until a set of predictors which account for 95% of the variance are selected and is visualized in Fig. 1 and the final model equation is provided as a Supplemental file. This model was compared to an approximated model after omitting the nutritional variables to evaluate the importance of the nutritional variables in terms of their impact on prediction accuracy. Bias-corrected performance metrics were calculated with ten-fold cross validation. Model discrimination was evaluated by calculating the concordance statistic and by plotting receiver operating characteristic (ROC) curves. Calibration curves were created by plotting predicted probabilities versus actual incidences of the outcome. Loess regression was used to smooth the calibration curves, which also included the calculation standard errors. In addition, the investigators calculated the Brier score, which is an objective measure that incorporates discrimination and calibration metrics simultaneously.
Results
A total of 607 patients with hip fractures were identified and met the inclusion criteria; of those patients, 67 (11%) were readmitted within a 30-day period. A total of 24 (4%) patients died within 30 days of index discharge.
Table 1 displays descriptive statistics and unadjusted univariate analysis of the population by 30-day re-admission status. If applicable, missing data prior to imputation is also included for each variable. Median age (79), race (89% Caucasian, 9% Black/African American, and 2% other), and gender (60% female) did not differ between groups. The fracture morphology did not significantly influence re-admission, although subtrochanteric fracture was the only type of fracture for which patients did not experience a re-admission within this data set. Patients who were re-admitted had a greater CCI (CCI of 4 vs. 2, p < 0.001) which indicates poor overall health status. Albumin (3.2 g/dL in the re-admission group vs. 3.5 g/dL, p = 0.038) and prealbumin (20.5 mg/dL in the readmission group vs. 25 mg/dL p < 0.001) levels were statistically different between groups subsequent to imputation. Normal reference values for nutritional status parameters used at our institution can be found in Table 2.
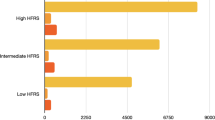
The final approximated model contained 12 variables with an internally cross-validated C-statistic of 0.811 (95% CI: 0.754, 0.867). The C-statistic indicates that this model is a good classifier and demonstrates superiority when compared to an approximated model without nutritional variables (C-statistic 0.694, 95% CI 0.624–0.763). The ROC curves displayed in Fig. 2 demonstrate an equivalent evaluation of the models’ discrimination in a graphical format. The Brier scores for the model with and without nutritional variables were respectively 0.0823 and 0.0931. Predictors selected in the final model in order of most to least importance were fracture type, prealbumin, albumin, white blood cell count, alanine aminotransferase, total protein, CCI, GFR, gender, race, creatinine, and vitamin D. Variables selected in the model without nutritional variables that underperformed with respect to the aforementioned model were fracture type, CCI, white blood cell count, alanine aminotransferase, and median income.
Discussion
The present study resulted in the derivation and validation of a model for predicting 30-day re-admission of patients hospitalized sustaining a hip fracture. The final model contained 12 variables with fields available in the EMR, including total protein, albumin, prealbumin, and vitamin D (four out of five predictors of nutrition). Our model includes nutritional factors for the prediction of re-admission risk after hip fracture, as other reports have examined causality of re-admission but not predictors. The high C-statistic suggests that the model confers good discriminative ability in identifying patients who are at high risk for re-admission. The calibration curves appear (Fig. 3) to show that both models underestimate risk among the highest risk patients, but the distributions of predicted risk are highly skewed to the left. The model likely underestimates the risk in the highest risk subset of patients, but both models appear to be sufficiently calibrated when excluding the extremely high predicted risks in the right tail of the distribution. The ROC curve demonstrates that the model with nutritional variables better discriminates between those who are re-admitted and those who are not. Our models highlight the importance of nutritional status as risk factors for re-admission. These are important modifiable risk factors because malnourished patients have substantially worse outcomes [25]. A recent randomized control trial found that oral nutritional supplementation to patients reduced post-operative complications and may be used as a template for nutritional supplementation [26]. While the nutritional laboratory markers for re-admission we identified are not sensitive enough to respond within a 30-day window, these values identify the high risk patients likely to benefit from a targeted and comprehensive nutritional intervention.
Our results show that nutritional markers were important variables in a 30-day re-admission prediction model for patients who suffered a hip fracture through selection by approximation and outperformed a model that omitted these variables on multiple measures. It may be that these variables are modifiable indicators of re-admission risk and that future models should consider their inclusion for this population. The models that omitted these variables had difficulty classifying patients into higher probabilities and appeared to perform poorly upon comparison.
Univariate analysis without adjustment shows that albumin levels were statistically different among the patients who experienced a re-admission within 30 days and those who were not re-admitted. Due to a long half-life (~20 days), albumin is essentially an indicator of a patient’s prior nutritional status and may predict if malnutrition might be a long-term issue prior to hospitalization. Low albumin can indicate that the patient is more severely ill and may need more aggressive attention after discharge to prevent complications. Prealbumin was also statistically different between re-admission and non-re-admission groups. Prealbumin is a better proxy for the patient’s status during the index hospitalization as it is sensitive to short-term nutritional changes and can identify acute malnutrition [27]. A systematic review and meta-analysis evaluating the effect of albumin levels on short-term mortality and post-operative complications identified increased odds of short-term mortality and post-operative complications with a lower serum albumin (≤ 3.4 g/dL) at admission [28]. Furthermore, a retrospective evaluation of a modified hip-multidimensional frailty score (hip-MFS) incorporating malnutrition factors in 481 patients more precisely predicted six month mortality and post-operative complications in hip fracture patients than existing tools [29]. Additionally, a previous randomized trial has shown that using a dietetic assistant in the care of hip fractures to monitor and treat nutritional deficiencies led to a decrease in mortality four months following surgical intervention [30]. However, it is important to note that the nutritional status was only a component of the hip-MFS. Despite this, with the combination of these findings and the established relationship between mortality and early re-admission we postulate that nutrition is a vital component of predicting early re-admission.
While we identified significant associations between nutritional markers and 30-day re-admission risk, a previous report of 490 hip fracture patients did not find a predictive correlation with one-year survival after hip fracture fixation [19]. Our findings do not disagree with the prior report as our study was not designed to address causal inference, but sought to identify modifiable risk factors likely to mitigate risk of re-admission. Our patient populations also differed from Donegan et al. [19] who included patients who were previously home-dwelling, ambulatory, and cognitively intact and excluded patients with significant comorbidities residing in assisted care facilities. Our study included all osteoporotic hip fractures. The most frequent reason for re-admission is reported to be non-surgical, and we postulate that nutritional status played a vital role in our investigation because co-morbid conditions frequently lead to decreased nutritional status [31].
Our study carries common limitations associated with EMR review. The type of hip fracture was not analyzed separately; however, we sought to identify potentially modifiable risk factors from the osteoporotic hip fracture population as a whole. We evaluated patients who were readmitted to our facility and may have missed patients admitted to a different facility. In addition, the data used in this study was obtained exclusively through structured fields in the patient’s medical record and may miss additional information contained in notes or free-text fields. Finally, previous investigations have identified risk factors for complications in older surgical patients that were not evaluated in this study; however, the main end point in those investigations was prevention of decubitus ulcers [32]. We do not believe that to be a relevant outcome in our investigation. Previous studies have demonstrated this to be associated with decreased reserves. Our local model reflects the operations of our hospital and the inherent characteristics of the population served; however, internal validity is salient, and it may serve to optimize patient risk stratification in its local institution.
With regard to the application of this model at the point of care, it is worth noting that a moderate percentage of patients lack nutritional laboratory values and would not be considered for risk stratification and contingent prioritization for intervention without imputation. It is important to note that a model omitting these variables did not perform as well in terms of predictive accuracy and discrimination, so one must consider the tradeoff between accurate classification and the size of the population to which this model may be applied. This can be remedied by either changing hospital practice to integrate widespread testing for the laboratory values included in the current model or by further exploring modifiable nutritional markers that are most readily available in the EMR and incorporating these into the model.
We sought to incorporate nutritional laboratory markers into a model that is functional when applied to new cases in our organization, and the authors provide the equation for those who may have similar populations. Our results indicate that laboratory markers at admission may allow us to predict which patients are at a higher risk of early re-admission after hip fracture and intervene accordingly, and that it may be beneficial to capture these variables in the EMR more often than is currently practiced. We suggest other institutions consider building their own model to accommodate laboratory values, hip fracture types, and patient demographics that may be heterogeneous across organizations.
This model may provide the foundation to direct resource intensive interventions toward high risk patients by leveraging an accurate risk prediction model. We believe that using these predictive markers, in conjunction with other established indicators, may decrease early re-admission rates [33]. Continued investigation into the peri-operative management of geriatric hip fractures utilizing similar strategies and models may lead to a reduction in patient morbidity and mortality and the healthcare expense burden.
References
Ziden L, Kreuter M, Frandin K (2010) Long-term effects of home rehabilitation after hip fracture - 1-year follow-up of functioning, balance confidence, and health-related quality of life in elderly people. Disabil Rehabil 32(1):18–32. https://doi.org/10.3109/09638280902980910
Carow J CJ, Coburn M, Kim BS, Bucking B, Bliemel C, Bollheimer LC, Werner CJ, Bach JP, Knobe M (2017) Mortality and cardiorespiratory complications in trochanteric femoral fractures: a ten year retrospective analysis. Int Orthop. https://doi.org/10.1007/s00264-017-3639-3
Bliemel C, Buecking B, Oberkircher L, Knobe M, Ruchholtz S, Eschbach D (2017) The impact of pre-existing conditions on functional outcome and mortality in geriatric hip fracture patients. Int Orthop. https://doi.org/10.1007/s00264-017-3591-2
Koren-Hakim T, Weiss A, Hershkovitz A, Otzrateni I, Anbar R, Gross Nevo RF, Schlesinger A, Frishman S, Salai M, Beloosesky Y (2016) Comparing the adequacy of the MNA-SF, NRS-2002 and MUST nutritional tools in assessing malnutrition in hip fracture operated elderly patients. Clin Nutr 35(5):1053–1058. https://doi.org/10.1016/j.clnu.2015.07.014
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP (2010) Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 210(6):901–908. https://doi.org/10.1016/j.jamcollsurg.2010.01.028
Folbert EC, Smit RS, van der Velde D, Regtuijt EM, Klaren MH, Hegeman JH (2012) Geriatric fracture center: a multidisciplinary treatment approach for older patients with a hip fracture improved quality of clinical care and short-term treatment outcomes. Geriatr Orthop Surg Rehabil 3(2):59–67. https://doi.org/10.1177/2151458512444288
Lau TW, Fang C, Leung F (2013) The effectiveness of a geriatric hip fracture clinical pathway in reducing hospital and rehabilitation length of stay and improving short-term mortality rates. Geriatr Orthop Surg Rehabil 4(1):3–9. https://doi.org/10.1177/2151458513484759
Gonzalez-Montalvo JI, Alarcon T, Mauleon JL, Gil-Garay E, Gotor P, Martin-Vega A (2010) The orthogeriatric unit for acute patients: a new model of care that improves efficiency in the management of patients with hip fracture. Hip Int 20(2):229–235
Gregersen M, Morch MM, Hougaard K, Damsgaard EM (2012) Geriatric intervention in elderly patients with hip fracture in an orthopedic ward. J Inj Violence Res 4(2):45–51. https://doi.org/10.5249/jivr.v4i2.96
Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM (2012) The medical orthopaedic trauma service: an innovative multidisciplinary team model that decreases in-hospital complications in patients with hip fractures. J Orthop Trauma 26(6):379–383. https://doi.org/10.1097/BOT.0b013e3182242678
Leung AH, Lam TP, Cheung WH, Chan T, Sze PC, Lau T, Leung KS (2011) An orthogeriatric collaborative intervention program for fragility fractures: a retrospective cohort study. J Trauma 71(5):1390–1394. https://doi.org/10.1097/TA.0b013e31821f7e60
Friedman SM, Mendelson DA, Bingham KW, Kates SL (2009) Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med 169(18):1712–1717. https://doi.org/10.1001/archinternmed.2009.321
Kammerlander C, Gosch M, Blauth M, Lechleitner M, Luger TJ, Roth T (2011) The Tyrolean Geriatric Fracture Center: an orthogeriatric co-management model. Z Gerontol Geriatr 44(6):363–367. https://doi.org/10.1007/s00391-011-0253-7
Adunsky A, Lerner-Geva L, Blumstein T, Boyko V, Mizrahi E, Arad M (2011) Improved survival of hip fracture patients treated within a comprehensive geriatric hip fracture unit, compared with standard of care treatment. J Am Med Dir Assoc 12(6):439–444. https://doi.org/10.1016/j.jamda.2010.09.003
Bracey DN, Kiymaz TC, Holst DC, Hamid KS, Plate JF, Summers EC, Emory CL, Jinnah RH (2016) An orthopedic-hospitalist comanaged hip fracture service reduces inpatient length of stay. Geriatr Orthop Surg Rehabil 7(4):171–177. https://doi.org/10.1177/2151458516661383
Marsland D, Chadwick C (2010) Prospective study of surgical delay for hip fractures: impact of an orthogeriatrician and increased trauma capacity. Int Orthop 34(8):1277–1284. https://doi.org/10.1007/s00264-009-0868-0
Kates SL, Blake D, Bingham KW, Kates OS, Mendelson DA, Friedman SM (2010) Comparison of an organized geriatric fracture program to United States government data. Geriatr Orthop Surg Rehabil 1(1):15–21. https://doi.org/10.1177/2151458510382231
Foss NB, Kristensen MT, Kehlet H (2006) Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: the cumulated ambulation score. Clin Rehabil 20(8):701–708. https://doi.org/10.1191/0269215506cre987oa
Donegan DJ, Gay AN, Baldwin K, Morales EE, Esterhai JL Jr, Mehta S (2010) Use of medical comorbidities to predict complications after hip fracture surgery in the elderly. Journal of bone and joint surgery American 92(4):807–813. https://doi.org/10.2106/JBJS.I.00571
Basques BA, Bohl DD, Golinvaux NS, Leslie MP, Baumgaertner MR, Grauer JN (2015) Postoperative length of stay and 30-day readmission after geriatric hip fracture: an analysis of 8434 patients. J Orthop Trauma 29(3):e115–e120. https://doi.org/10.1097/BOT.0000000000000222
Jou HJ, Siao RY, Tsai YS, Chen YT, Li CY, Chen CC (2014) Postdischarge rehospitalization and in-hospital mortality among Taiwanese women with hip fracture. Taiwan J Obstet Gynecol 53(1):43–47. https://doi.org/10.1016/j.tjog.2012.04.042
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
van Buuren S, Groothuis-Oudshoorn K (2011) MICE: multivariate imputation by chained equations in R. J Stat Softw 45(3):1–67
Harrell FE (2001) Regression modeling strategied with applications to linear models, logistic regression, and survival analaysis. Springer, New York
Bell JJ, Pulle RC, Crouch AM, Kuys SS, Ferrier RL, Whitehouse SL (2016) Impact of malnutrition on 12-month mortality following acute hip fracture. ANZ J Surg 86(3):157–161. https://doi.org/10.1111/ans.13429
Botella-Carretero JI, Iglesias B, Balsa JA, Arrieta F, Zamarron I, Vazquez C (2010) Perioperative oral nutritional supplements in normally or mildly undernourished geriatric patients submitted to surgery for hip fracture: a randomized clinical trial. Clin Nutr 29(5):574–579. https://doi.org/10.1016/j.clnu.2010.01.012
MacKay D, Miller AL (2003) Nutritional support for wound healing. Altern Med Rev 8(4):359–377
Laulund AS, Lauritzen JB, Duus BR, Mosfeldt M, Jorgensen HL (2012) Routine blood tests as predictors of mortality in hip fracture patients. Injury 43(7):1014–1020. https://doi.org/10.1016/j.injury.2011.12.008
Choi JY, Cho KJ, Kim SW, Yoon SJ, Kang MG, Kim KI, Lee YK, Koo KH, Kim CH (2017) Prediction of mortality and postoperative complications using the hip-multidimensional frailty score in elderly patients with hip fracture. Sci Rep 7:42966. https://doi.org/10.1038/srep42966
Duncan DG, Beck SJ, Hood K, Johansen A (2006) Using dietetic assistants to improve the outcome of hip fracture: a randomised controlled trial of nutritional support in an acute trauma ward. Age Ageing 35(2):148–153. https://doi.org/10.1093/ageing/afj011
Heyes GJ, Tucker A, Marley D, Foster A (2015) Predictors for readmission up to 1 year following hip fracture. Arch Trauma Res 4(2):e27123. https://doi.org/10.5812/atr.4(2)2015.27123
Cohen RR, Lagoo-Deenadayalan SA, Heflin MT, Sloane R, Eisen I, Thacker JM, Whitson HE (2012) Exploring predictors of complication in older surgical patients: a deficit accumulation index and the Braden scale. J Am Geriatr Soc 60(9):1609–1615. https://doi.org/10.1111/j.1532-5415.2012.04109.x
Lizaur-Utrilla A, Serna-Berna R, Lopez-Prats FA, Gil-Guillen V (2015) Early rehospitalization after hip fracture in elderly patients: risk factors and prognosis. Arch Orthop Trauma Surg 135(12):1663–1667. https://doi.org/10.1007/s00402-015-2328-1
Acknowledgements
The authors would like to thank Jan Lawlor, Section on Gerontology and Geriatric Medicine, Department of Internal Medicine, for her assistance with research coordination. The authors would also like to acknowledge the data extraction and statistical assistance of the Wake Forest Clinical and Translational Science Institute (WF CTSI), which is supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Stone has received research support from Smith & Nephew. Dr. Miller has received financial support from AO North America. Dr. Miller is a board or committee member for the American Academy of Orthopedic Surgery, the American College of Surgeons, the AOTrauma North America, and the Orthopedic Trauma Association. Dr. Miller is also on the editorial or governing board for the Journal of Orthopedic Trauma. Dr. Emory is a paid consultant for BoardVitals. Dr. Emory receives research support from IlluminOss Medical and the Muskuloskeletal Transplant Foundation. Dr. Emory is a board or committee member for the Ruth Jackson Orthopedic Society. Dr. Jinnah, Dr. Wells, Dr. Atkinson, Ms. Lenoir, and Mr. Futrell declare they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Stone, A.V., Jinnah, A., Wells, B.J. et al. Nutritional markers may identify patients with greater risk of re-admission after geriatric hip fractures. International Orthopaedics (SICOT) 42, 231–238 (2018). https://doi.org/10.1007/s00264-017-3663-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3663-3