Abstract
Purpose
The study aims to analyze the incidence of 30-day mortality in elderly patients who underwent surgery for hip fractures and its associated factors.
Methods
A prospective multicentric study was performed. All patients aged ≥ 65 years, with fragility hip fractures, consecutively admitted in two Italian hospitals were included. Patients with periprosthetic or pathological fractures were excluded. Logistic regression was used to identify patient and patient care variables that independently influenced the 30-day mortality and receiver operating characteristic (ROC) curve analysis to assess their predictive capacity on the outcome.
Results
Of the patients, 728 met the inclusion criteria, of whom approximately 5% died within 30 days after admission. The 45.7% of the deceased patients died while hospitalized. Multivariate analysis showed that advancing age was the only independent predictor of 30-day mortality (OR = 1.084, 95% CI = 1.024–1.147), while a higher presence of informal caregivers was a protective factor (OR = 0.988, 95% CI = 0.979–0.997). The area under the ROC curve of the model was 0.723 (CI95% 0.676–0.770) for 30-day mortality in elderly hip fractures patients.
Conclusions
Patients with an advanced age need careful follow-up, especially within 30 days following operation for hip fracture; at the same time, the presence of informal caregivers at the patient’s bedside should be promoted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fragility hip fractures are a significant health issue in older adults, with a constantly increasing incidence worldwide, that is estimated to reach 6.3 million by the year 2050 [1]. Despite advances in peri-operative care, they have been associated with significant disability, such as inability to independently walk and/or perform Activities of Daily Living (ADLs) [2], and mortality [3]. The excess mortality after hip fracture is highest within the first month [1, 4], with a 30-day mortality reported to be as high as 13.3% in previous studies [5], but it could persist ten years [3]. The 30-day mortality has been widely considered as a quality indicator for hospital care [4]. Its association with modifiable patient care variables, such as time to surgery [4, 6,7,8,9,10], surgical technique [11], type of anaesthesia—regional versus general [11], use of clinical pathways for hip fractures [11] and/or multidisciplinary approach [12], and length of stay [13, 14] has been previously studied. Moreover, the international literature has generally agreed that patient’s characteristics, such as age, gender, and pre-existing comorbidities [1, 4, 7, 9, 15,16,17,18], and organizational factors, such as hip fracture volume [19], are non-modifiable factors contributing to early death of geriatric patients with hip fractures.
However, to our best knowledge, available studies have focused their attention mainly to one type of the above-cited factors (patient level [16,17,18, 20], patient care level [6, 8,9,10,11], organizational level [19], and used mostly retrospective data [6, 9, 10, 15,16,17,18, 21]).
In addition, given the global aging population, especially in Italy where there is one of the highest percentage of elderly people in Europe and in the world [2], and the expected increase of the total number of geriatric hip fractures [17] as well as the constant need of the National Health System (NHS) to reduce risk and improve patient outcomes, a more exhaustive analysis of 30-day mortality rates after hip fractures and possible predictors may aid our understanding and thus improve care quality.
Therefore, this study aimed to analyze the incidence of 30-day mortality in elderly patients who underwent surgery for hip fractures and its associated factors at the patient and patient care level.
Materials and methods
Study design, setting, and sample
A prospective multicentric study was performed in two Italian public hospitals: one 1500-bed university teaching hospital and one 330-bed orthopaedic specialty hospital, both with an average hip fracture surgical patient volume of 36 per month. All patients aged 65 years or older at the date of admission, with a diagnosis of fragility hip fracture (pertrochanteric, femoral neck, and subtrochanteric), consecutively admitted during the study period (October 2013–October 2014) to the Emergency Departments (EDs) of the involved hospitals, and willing to participate, were included. Those patients with periprosthetic or pathological fractures, who generally have different treatments and therefore different care needs, and/or refusing to participate in the study, were excluded.
In both involved hospitals, early surgery within 48 hours from the trauma was generally guaranteed. The included patients were admitted to an orthopaedic surgery department or to an orthogeriatric department, depending on beds’ availability. The orthopaedic surgeons, based on the patient’s age, clinical conditions, and type of fracture, established the surgical technique. During the in-hospital stay, a rehabilitation treatment was provided twice a day for six days a week, starting from the day after surgery. It aimed at allowing an early verticalization and walking. After the discharge, the rehabilitation program continued, as decided by the patient and a multidisciplinary team.
Ethics
The Ethics Committees of all the two involved hospitals approved the study protocol. Written consent was obtained from patients and from next-of-kin or legal representative for patients unable to provide consent for medical reasons. Patients were also assured that they could withdraw from the study at any time and that their anonymity was guaranteed.
Variables
The primary outcome of this study was death from any cause occurring in-and-out-of hospital within 30 days of admission.
At the patient level, the following demographic and clinical data were assessed at the patient’s admission: age (in year) and gender, prefracture activity of daily living independence (ADL) [22], presence of comorbidities as measured with the Charlson index [23], and the haemoglobin (Hb) level. During the patient’s in-hospital stay, the presence of pain, as measured using the Numerical Rating Scale (NRS) [24] or PAINAD for patients with cognitive impairment [25], of fever, intended as a body temperature > 37 °C, urinary infections (clinical evaluation), disorientation (clinical evaluation), changes in haemoglobin values, and the use of physical restraints (only bed rails), the use of diaper or urinary catheter, were assessed. Moreover, the time required to achieve, assisted or independently, the seated and static position and to walk for the first time, was measured. The average number of physiotherapist visits and the assistance required to achieve functional tasks, as measured with the Iowa Level of Assistance (ILOA) score [26], were also assessed. At discharge, the length of stay was collected.
At the patient care level, time from the occurrence of the fracture to the surgery, time from arrival in the ED to surgery, average length of surgery, and timing with respect to starting physiotherapy were measured. Moreover, the presence of an informal caregiver, such as a family member, a friend or another lay caregiver at the patient’s bedside for at least half day, was collected.
Data collectors were trained registered nurses (RNs) with experience in hip fracture care and in clinical research, not involved in patient’s care. Clarification of data was obtained if necessary from the treating staff. Each patient was assessed on admission to the ED and on a daily basis until discharge. A follow-up was also performed after 30 days from admission.
Statistical analysis
Data analysis was performed using Statistical Package for Social Sciences (SPSS v.19.0, IBM Corp., Armonk, NY, USA) for statistical analysis.
Descriptive statistical analyses were performed calculating mean and the standard deviation of the mean or median and interquartile range, when not normally distributed, for continuing variables or frequencies and percentage for categorical variables. The Kolmogorov-Smirnov test was carried out to assess the normality of the continuous variables. The Levene’s test was carried out to assess homoscedasticity. Analysis of variance (ANOVA) was carried out to assess the between-group differences of continuous, normally distributed and homoscedastic data; the Mann-Whitney test was used for all other assessments. Analysis of variance, followed by the Scheffè post hoc pairwise comparison, was also used to assess the between-group differences of continuous, normally distributed, and homoscedastic data; the Kruskal-Wallis test followed by the Mann-Whitney test with the Bonferroni correction for multiple comparisons was used for all other assessments. The Fisher exact test was carried out to investigate the relationships between the dichotomous variables. The Pearson chi-squared test, evaluated using exact methods for small samples, was carried out to investigate the relationships between group variables.
Logistic regression using the Wald backward method was utilized to find which of the studied variables independently influenced the outcome. This was repeated to select which patient care and patient care factors were significant in the univariate analysis and, corrected by the factors found with the previous analysis, influenced the outcome.
Receiver operator characteristic (ROC) curve analysis was used to check the logistic regression model.
The criterion for statistical significance was set at p < 0.05.
In this study, the sample size was based on the number of predictive parameters inserted into the multivariate analysis; therefore, it was estimated to include at least 700 patients.
Results
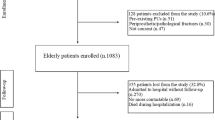
A total of 805 patients were admitted during the study period, of whom 728 were included in the study (90.4%). In the excluded patients, 30 (39%) presented periprosthetic or pathological fractures and 47 (61%) did not agree to participate in the study (Fig. 1).
Patient characteristics are summarized in Table 1.
The 30-day mortality rate was 4.9% (35/728). The 45.7% of the deceased patients died while hospitalized.
Profile of patients deceased within 30 days from hospital admission
Comparing sample’s characteristics in relation to 30-day mortality, the group of patients who died and those who survived were homogeneous in the terms of the patient care variables. With regard to the patient characteristics, a statistically significant difference was found for different variables (Table 1). In particular, those patients died within 30 days from admission were older (P < 0.005) than those who survived. During their in-hospital stay, they were more disoriented (P < 0.005) and exposed to urinary infections (P = 0.012), they experienced a higher number of days with the presence of physical restraints (P = 0.001) and diaper (P < 0.005), but fewer days with the presence of informal caregivers (P = 0.001). Furthermore, the deceased patients reported lower average percentage of days with fever (P = 0.044), lower average Hb level on admission (P = 0.029), but lower average percentage of Hb decrease during in-hospital stay (P = 0.007).
Predictive factors of 30-day mortality
In the multivariate analysis (Table 2), for each increase of one year of age over 65 years, there was a 8.4% increase in the odds of dying within 30 days from hospital admission (OR = 1.084, 95% CI = 1.024–1.147). On the contrary, experiencing the presence of informal caregivers for a higher number of days (OR = 0.988, 95% CI = 0.979–0.997) decreased the risk of 30-day mortality.
A trend toward significance was observed for experiencing disorientation for a higher number of days (OR = 2.282, 95% CI = 0.902–5.771) and the presence of urinary infection (OR = 2.183, 95% CI = 0.994–4.729).
Mapping the ROC curve to predict 30-day mortality from the multivariate model (Fig. 2), the area under the curve (AUC) was 0.723 (CI95% 0.676–0.770).
Discussion
In the present study of 728 patients who underwent surgery for hip fractures, 35 (4.9%) died within 30 days from admission to hospital. The overall death rate compares favourably to those of other developed countries, where this figure is higher, reaching up to 13.3%, as reported by a recent meta-analysis [5]. Nevertheless, differences in definition of 30-day mortality (e.g., death within 30 days after discharge [13, 21], death within 30 days after surgery [1]), in study design (retrospective—with data extracted from databases not always developed for clinical research—versus prospective), and in data collection period (e.g., more recent—with new multidisciplinary approach and implementation of guidelines for hip fractures)—versus less recent), could make the comparison difficult.
Profile of patients deceased within 30 days from hospital admission
Confirming results from previous studies, patients who died within 30 days from hospital admission were older [3,4,5, 7, 9, 15, 17, 21]; this is probably due to the reduced reserve capacity necessary to cope with the double trauma of fracture and surgery. Moreover, the number and severity of chronic diseases is generally higher in elderly patients [3]. Nevertheless, no difference in mortality have emerged about the Charlson score [23] on admission, and this result is in contrast with previous studies [1, 10].
At admission, patients who later died reported a lower average Hb level, as reported previously by other authors [20, 21]. Nevertheless, a lower Hb decrease in the post-operative period was found in this group of patients, and this could be related to a stronger/more aggressive clinical approach with blood transfusions before/during/after hip fracture surgery to correct their anaemia.
During their in-hospital stay, the deceased patients were more disoriented, exposed to urinary infections and experienced a higher number of days with the presence of physical restraints and diaper, thus suggesting their frailer condition compared to the survived patients.
Opposite to a previous Italian study [27], deceased patients received on average fewer days with the presence of an informal caregiver. The earlier study, even if conducted in medical settings and focused on in-hospital mortality, reported that those patients who died received a higher amount of care by family carers, probably because of a comfort approach required by terminally ill patients. Differently, a possible explanation for the result of this study includes the association between low social support and risk of death in the older adults [28].
Predictive factors of 30-day mortality
Unlike previous studies reporting an association between 30-day mortality and modifiable patient care factors, such as time to surgery [4, 6, 7], this relation was not found in the present study.
The only predictive factors for 30-day mortality were related to patient. For each additional year of age over 65 years, there was an 8.4% increase in risk of dying within 30 days from hospital admission. Increasing age has been previously identified as an independent risk factor for 30-day mortality in hip fracture patients because it is related to the patients’ poor physiological reserve in coping with the stress of surgery and its consequences [1, 3, 4, 7, 9, 13, 15]. On the contrary, the 30-day mortality risk was reduced by 1% for each day increase with the presence, for at least half day, of informal caregivers. This result may have important clinical implications as the presence of informal caregiver for an average length of stay of approximately 10 days may help to reduce the patient’s risk of dying up to 10%. This is a modifiable factor, thus suggesting interventions for supporting open hospital visiting policies. Indeed, a higher presence of informal caregivers may provide concrete, practical aid regarding rehabilitation process, such as helping with transfers and self-care, and psychological support [29]. Moreover, it may reflect the existence of a stronger social network and a better social support, thus reducing the risk of death in older adults [28]. Nevertheless, no previous studies associating presence of informal caregivers to 30-day mortality in hip fracture patients have been documented to date, therefore preventing comparisons. In the final predictive model, presenting a higher percentage of days with disorientation or a urinary infection retained marginal significance, thus needing to be revisited in further studies. Nevertheless, these two variables contributed to improve the predictive value of the model (AUC included between 0.7 and 0.9), in line with previous instruments developed for predict 30-day mortality in geriatric hip fracture patients, such as Sernbo score [30], HEMA model [15], and predictive model developed by Endo and colleagues [9].
Although this study is valued by its prospective design and the use of multivariate analysis, which minimized the confounding effect of covariates, some limitations affect it. No data with regard to cognitive impairment was collected on patient’s admission. Moreover, some variables, such as disorientation, were not assessed using validated instruments but with a clinical evaluation; given the pragmatic nature of the study, this was more consistent with the daily clinical practice.
Conclusions
In this study of 728 patients who underwent surgical treatment for hip fractures, the only predictive factors for 30-day mortality were related to patient’s characteristics. A higher risk of dying within 30 days after hospital admission was found for older patients; on the contrary, a higher presence of informal caregivers was a protective factor against short-term death. Patients with an advanced age need careful follow-up, especially within 30 days following operation for hip fracture; at the same time, the presence of informal caregivers at the patient’s bedside should be promoted, since they positively influence functional independence in the post-operative period. The influence of urinary infection and disorientation need to be considered and further studied.
References
Sheikh HQ, Hossain FS, Aqil A, Akinbamijo B, Mushtaq V, Kapoor H (2017) A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg 9(1):10–18. https://doi.org/10.4055/cios.2017.9.1.10
Piscitelli P, Feola M, Rao C, Celi M, Gasbarra E, Neglia C, Quarta G, Liuni FM, Parri S, Iolascon G, Brandi ML, Distante A, Tarantino U (2014) Ten years of hip fractures in Italy: for the first time a decreasing trend in elderly women. World J Orthop 5(3):386–391. https://doi.org/10.5312/wjo.v5.i3.386
Sheehan KJ, Sobolev B, Chudyk A, Stephens T, Guy P (2016) Patient and system factors of mortality after hip fracture: a scoping review. BMC Musculoskelet Disord 17:166. https://doi.org/10.1186/s12891-016-1018-7
Khan MA, Hossain FS, Ahmed I, Muthukumar N, Mohsen A (2013) Predictors of early mortality after hip fracture surgery. Int Orthop 37(11):2119–2124. https://doi.org/10.1007/s00264-013-2068-1
Hu F, Jiang C, Shen J, Tang P, Wang Y (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 43(6):676–685. https://doi.org/10.1016/j.injury.2011.05.017
Choi HJ, Kim E, Shin YJ, Choi BY, Kim YH, Lim TH (2014) The timing of surgery and mortality in elderly hip fractures: a retrospective, multicenteric cohort study. Indian J Orthop 48(6):599–604. https://doi.org/10.4103/0019-5413.144232
Bretherton CP, Parker MJ (2015) Early surgery for patients with a fracture of the hip decreases 30-day mortality. Bone Joint J 97-B(1):104–108. https://doi.org/10.1302/0301-620X.97B1.35041
Tulic G, Dubljanin-Raspopovic E, Tomanovic-Vujadinovic S, Sopta J, Todorovic A, Manojlovic R (2018) Prolonged pre-operative hospital stay as a predictive factor for early outcomes and mortality after geriatric hip fracture surgery: a single institution open prospective cohort study. Int Orthop 42(1):25–31. https://doi.org/10.1007/s00264-017-3643-7
Endo A, Baer HJ, Nagao M, Weaver MJ (2018) Prediction model of in-hospital mortality after hip fracture surgery. J Orthop Trauma 32(1):34–38. https://doi.org/10.1097/BOT.0000000000001026
Wong SHJ, Fang XC, Yee KHD, Wong TM, Pun CTT, Lau TW, Leung KLF (2018) Hip fracture time-to-surgery and mortality revisited: mitigating comorbidity confounding by effect of holidays on surgical timing. Int Orthop. https://doi.org/10.1007/s00264-017-3737-2
Neuman MD, Archan S, Karlawish JH, Schwartz JS, Fleisher LA (2009) The relationship between short-term mortality and quality of care for hip fracture: a meta-analysis of clinical pathways for hip fracture. J Am Geriatr Soc 57(11):2046–2054. https://doi.org/10.1111/j.1532-5415.2009.02492.x
Kristensen PK, Thillemann TM, Søballe K, Johnsen SP (2016) Can improved quality of care explain the success of orthogeriatric units? A population-based cohort study. Age Ageing 45(1):66–71. https://doi.org/10.1093/ageing/afv155
Nordström P, Gustafson Y, Michaëlsson K, Nordström A (2015) Length of hospital stay after hip fracture and short-term risk of death after discharge: a total cohort study in Sweden. BMJ 350:h696. https://doi.org/10.1136/bmj.h696
Sobolev B, Guy P, Sheehan KJ, Bohm E, Beaupre L, Morin SN, Canadian Collaborative Study on Hip Fractures et al (2017) Hospital mortality after hip fracture surgery in relation to length of stay by care delivery factors: a database study. Medicine (Baltimore) 96(16):e6683. https://doi.org/10.1097/MD.0000000000006683
Karres J, Kieviet N, Eerenberg JP, Vrouenraets BC (2018) Predicting early mortality after hip fracture surgery: the hip fracture estimator of mortality Amsterdam. J Orthop Trauma 32(1):27–33. https://doi.org/10.1097/BOT.0000000000001025
Lau TW, Fang C, Leung F (2016) Assessment of postoperative short-term and long-term mortality risk in Chinese geriatric patients for hip fracture using the Charlson comorbidity score. Hong Kong Med J 22(1):16–22. https://doi.org/10.12809/hkmj154451.
Man LP, WH Ho A, Wong SH (2016) Excess mortality for operated geriatric hip fracture in Hong Kong introduction. Hong Kong Med J 22:6–10. https://doi.org/10.12809/hkmj154568.
Dodd AC, Bulka C, Jahangir A, Mir HR, Obremskey WT, Sethi MK (2016) Predictors of 30-day mortality following hip/pelvis fractures. Orthop Traumatol Surg Res 102(6):707–710. https://doi.org/10.1016/j.otsr.2016.05.016
Kristensen PK, Thillemann TM, Johnsen SP (2014) Is bigger always better? A nationwide study of hip fracture unit volume, 30-daymortality, quality of in-hospital care, and length of hospital stay. Med Care 52(12):1023–1029. https://doi.org/10.1097/MLR.0000000000000234.
Praetorius K, Madsen CM, Abrahamsen B, Jørgensen HL, Lauritzen JB, Laulund AS (2016) Low levels of hemoglobin at admission are associated with increased 30-DayMortality in patients with hip fracture. Geriatr Orthop Surg Rehabil 7(3):115–120. https://doi.org/10.1177/2151458516647989
Stone AV, Jinnah A, Wells BJ, Atkinson H, Miller AN, Futrell WM, Lenoir K, Emory CL (2018) Nutritional markers may identify patients with greater risk of re-admission after geriatric hip fractures. Int Orthop 42(2):231–238. https://doi.org/10.1007/s00264-017-3663-3
Chen Q, Kane RL (2001) Effects of using consumer and expert ratings of an activities of daily living scale on predicting functional outcomes of postacute care. J Clin Epidemiol 54(4):334–342
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity: a critical review of available methods. J Clin Epidemiol 56(3):221–229
Hartrick CT, Kovan JP, Shapiro S (2003) The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract 3(4):310–316
Costardi D, Rozzini L, Costanzi C, Ghianda D, Franzoni S, Padovani A et al (2007) The Italian version of the pain assessment in advanced dementia (PAINAD) scale. Arch Gerontol Geriatr 44(2):175–180
Smith KB, Steckel SD (1995) Reliability, validity and responsiveness of functional tests in patients with total joint replacement. Phys Ther 75:169–179
Ambrosi E, Detogni S, Guarnier G, Barelli P, Zambiasi Z, Allegrini E et al (2017) In-hospital elderly mortality and associated factors in 12 Italian acute medical units: findings from an exploratory longitudinal study. Aging Clin Exp Res 29(3):517–527. https://doi.org/10.1007/s40520-016-0576-8
de Brito TRP, Nunes DP, Corona LP, da Silva Alexandre T, de Oliveira Duarte YA (2017) Low supply of social support as risk factor for mortality in the older adults. Arch Gerontol Geriatr 73:77–81. https://doi.org/10.1016/j.archger.2017.07.016
Rocha SA, Avila MA, Bocchi SC (2016) The influence of informal caregivers on the rehabilitation of the elderly in the postoperative period of proximal femoral fracture. Rev Gaucha Enferm 37(1):e51069. https://doi.org/10.1590/1983-1447.2016.01.51069.
Dawe EJ, Lindisfarne E, Singh T, McFadyen I, Stott P (2013) Sernbo score predicts survival after intracapsular hip fracture in the elderly. Ann R Coll Surg Engl 95(1):29–33. https://doi.org/10.1308/003588413X13511609954653
Acknowledgements
The authors would like to thank all individuals who participated in this study and Dr. Elettra Pignotti, expert in Biostatistics, for her contribution by performing statistical analysis.
Author information
Authors and Affiliations
Contributions
CF, PC: concept and design, acquisition of subjects and data, analysis and interpretation of data, preparation of manuscript. DG, EA: analysis and interpretation of data, preparation of manuscript. FD, AF, MM, TS: acquisition of subjects and data, analysis and interpretation of data, preparation of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Forni, C., Gazineo, D., D’Alessandro, F. et al. Predictive factors for thirty day mortality in geriatric patients with hip fractures: a prospective study. International Orthopaedics (SICOT) 43, 275–281 (2019). https://doi.org/10.1007/s00264-018-4057-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4057-x