Abstract
Purpose
Short-stem hip arthroplasty (SHA) was designed to preserve bone stock and provide an improved load transfer. To gain more evidence regarding the load transfer, this review analysed the periprosthetic bone remodelling of SHA in comparison to standard hip arthroplasty (THA).
Methods
PubMed and ScienceDirect were screened to extract dual-energy X-ray absorptiometry (DXA) studies evaluating the periprosthetic bone remodelling of SHA and two proven THA designs. From the studies included, the postoperative change in periprosthetic bone mineral density (BMD) after one year and the trend over two years was determined.
Results
Fifteen studies with four SHAs (CFP, Metha, Nanos, Fitmore) and two THAs (CLS and Bicontact) designs were included. All SHA and THA stems revealed an initial decrease at the calcar and major trochanter (Gruen 1 and 7) with the Metha, Nanos and Fitmore showing a smaller and more balanced remodelling compared to THA. The pattern after one year and the trend over two years argue for a methaphyseal anchorage of the Metha and Nanos, whereas the Fitmore and CFP seem to anchor metha-diaphyseal. Clearly different pattern of bone remodelling were observed between all four SHAs.
Conclusions
Periprosthetic bone remodelling is also present in SHA, with the main bone reduction observed proximally. However, certain SHA stems show a more balanced remodelling compared to THA, arguing for a favourable load transfer. Also, the femoral length where bone remodelling occurs is clearly shorter in SHA. As distinctively different pattern between the SHA designs were observed, they should not be judged as a single implant group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cementless anchorage of total hip arthroplasty (THA) has become a standard fixation with excellent long-term results being reported. A perquisite is sufficient bone stock with a good biological host response for osseous integration and implant fixation. However, the long-term success is also determined by the mechanical adaptation of the skeleton to the load transfer of the implant [1]. Irregular load pattern can lead to adverse bone remodelling effects, commonly referred as stress shielding. Stress shielding can cause significant bone loss around the implant and result in an early implant failure with difficult revision situations [2].
Short-stem hip arthroplasty (SHA) has recently gained popularity as it preserves femoral bone stock and is also assumed to provide a more physiological load transfer compared to conventional THA [3, 4]. Various studies have reported a good short- and medium-term outcome [5,6,7,8]. Nevertheless, long-term studies explicitly proofing the favourable load transfer are not available yet. Additionally, a variety of SHA implants has recently been introduced, most of them with distinct differences in the design regarding the stem length, levels of osteotomy and insertion techniques. Yet, the impact of these differences on bone remodelling is unknown.
The periprosthetic bone remodelling processes can be assessed by dual-energy X-ray absorptiometry (DXA) and detect the specific load transfer as well as stress shielding processes [9]. For SHA, several studies have evaluated the periprosthetic bone mineral density (BMD) and reported a reduced BMD loss in the proximal femoral regions [4, 6, 10,11,12]. Therefore, it is assumed that SHA provides a favourable load transfer compared to standard THA. However, the results of these studies also revealed distinct differences in the bone remodelling regarding the different SHA designs.
To further evaluate and compare the bone remodelling after SHA, the present study systematically reviewed the current literature and summarised the tendency of periprosthetic BMD changes. The aim was to compare the BMD changes of established SHA stems and also compare the results with those of proven conventional THA stems.
Materials and methods
Ethics statement and guidelines
This systematic review retrospectively analysed published clinical data. After contacting the Ethics Committee (Ethical Committee University of the LMU), it was stated that neither a special ethics review nor ethical approval was needed. Due to the retrospective nature using anonymous data no additional informed consent of the patients was necessary. Our study was conducted according to the preferred reporting items for systematic reviews [13].
Inclusion and exclusion criteria
Inclusion criteria were as follows: full text in English; studies including patients with primary total hip (short or conventional) replacement due to osteoarthritis, osteonecrosis, traumatic arthritis or femoral neck fracture; DXA used to evaluate the periprosthetic bone remodelling; BMD data collected within two months after surgery, which served as baseline value for the subsequent DXA examinations; the evaluated SHA stems were limited to the Metha (B.Braun, Aesculap, Tuttlingen, Germany), Nanos (Smith & Nephew, London, UK), Fitmore (Zimmer, Warsaw, IN, USA) and collum femoris preserving (CFP; Link, Hamburg, Germany) stems, and the standard stems were limited to the cementless Spotorno (CLS; Zimmer, Warsaw, IN, USA) and Bicontact (B.Braun, Aesculap, Tuttlingen, Germany) stem with proven long-term results. Exclusion criteria were as follows: non-clinical studies; no original reports on clinical outcomes such as review articles, instructional course lectures or technique articles.
Information sources and search
A comprehensive literature search was performed using the electronic medical databases PubMed and ScienceDirect until July 2017 to identify all articles reporting the bone remodelling of SHA stems and for the two conventional THA stems (CLS and Bicontact). There was no limit for the publication time. The search terms were as follows: (hip replacement OR hip arthroplasty OR THA OR THR) AND (bone remodelling OR bone remodelling OR bone resorption OR BMD OR bone mineral density OR dual-energy X-ray absorptiometry OR DXA OR DEXA) AND (short stem OR metaphyseal OR stemless OR CLS OR Spotorno Stem OR Bicontact).
Data extraction
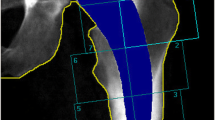
Two reviewers screened the potentially relevant literature based on titles and abstracts, and determined each eligible published study based on full text according to the inclusion criteria. Disagreements between two reviewers were judged by an additional reviewer. Unpublished studies were not searched or included. In the absence of the data of the BMD changes, they were obtained from the graphs. The periprosthetic BMD changes were extracted according to the established Gruen zones (1, greater trochanter; 2, proximal lateral; 3, distal lateral; 4, stem tip; 5, distal medial; 6, proximal medial; 7, calcar) [14]. The following data were extracted independently by two investigators from each study: author, stem type, number of female and male patients, mean age, mean body mass index (BMI), follow-up times and BMD changes. In all the studies, the BMD changes were compared to the 7-day post-operative DXA measurement.
Statistical analysis
The BMD changes (mean ± SD) for each implant were calculated from the included studies at the follow-up of one year. The overall trend of BMD changes over the study period of each single implant was revealed by the linear regression analysis.
Results
Study identification
The search strategy retrieved 238 records from PubMed/Medline and 343 from ScienceDirect. After removing 21 duplicates, 560 references were screened based on title and abstract. According to the predefined criteria, 543 reports were excluded and from 17 the full-text was screened, from which one was excluded due to repeated date and 16 studies were included (Fig. 1).
Study characteristics
The characteristics of the 16 studies are shown in Table 1. Ten studies evaluated SHA stems: three partial collum stems—Metha (n = 5, mean follow-up 21.6 months), Nanos (n = 2, mean follow-up 12 months), CFP (n = 1, follow-up 24 months)—and one trochanter sparing stem—Fitmore (n = 2, mean follow-up 12 months). Six studies evaluated conventional THA stems: CLS (n = 4, mean follow-up 48 months) and Bicontact (n = 2, mean follow-up 18 months).
Periprosthetic bone remodelling
The periprosthetic BMD changes for SHA and THA at the 1 year follow-up are summarised in Fig. 2 and Table 2. The overall trend of BMD changes in Gruen zones 1-7 for all implants are displayed in Fig. 3.
All SHA and THA stems showed a reduction in the periprosthetic BMD of the proximal regions. Also, all studies revealed a trend towards a decreased periprosthetic BMD after three or six months post-operatively, with a marked decrease at Gruen zones 1 and 7. Most of them showed that the reduced BMD in these regions did not completely recover after one year, whereas the more moderate reduction in the BMD at other Gruen zones partially recovered.
SHA implants
Metha stem
The mean BMD at 12 months post-operatively decreased in all Gruen zones except for zones 5 and 6. The highest increase was observed for Gruen zone 6 (+5.7%) and the highest decrease for zone 7 (−12.5%). In the further course until 24 months, the mean BMD increased again in all Gruen zones. The BMD even exceeded the baseline in Gruen zones 2, 5 and 6 with the highest increase observed in zone 6 (+9.2%). The BMD also recovered in the proximal femur, Gruen zones 1 and 7, but the baseline was not completely reached (−2.5% and −0.9%) (Fig. 2). Overall, a trend towards a permanently increased BMD was noted for Gruen zones 2, 5 and 6 and a slightly decreased BMD at Gruen zones 1 and 7. Gruen zones 3, 4 and 5 show a trend of holding the baseline (Fig. 3).
Nanos stem
The mean BMD decreased after 12 months for all Gruen zones except for zone 6. The highest increase was observed in Gruen zone 6 (+5.4%) and the highest decrease for zone 1 (−13.7%) and 7 (−8.4%) (Fig. 2). The Gruen zones 3, 4 and 5 (all −0.7%) showed a trend to keep the preoperative baseline, whereas Gruen zone 6 revealed a trend towards a permanent increased BMD and Gruen zones 1 and 7 for a permanent decrease (Fig. 3).
Fitmore stem
The mean BMD decreased 12 months post-operatively for all Gruen zones except for zones 3 (2.3%) and 5 (0.2%). The highest decrease was observed for Gruen zone 2 (−5.0%) as well as for Gruen zone 7 (−4.5%) and 4 (−3.2%) (Fig. 2). Overall, a trend towards a permanently increased BMD was noted for Gruen zones 3 and 5 and a slightly decreased BMD at Gruen zones 1 and 7. Gruen zones 2, 4 and 6 show a trend towards holding the baseline (Fig. 3).
CFP stem
Only one study was available for the CFP stem, which showed a decreased BMD for all Gruen zones 12 months after implantation. A highly decreased BMD was observed for the Gruen zones 7 (−30.9%), 6 (−19.2%) and 2 (−13.3%), and a moderate decrease for zone 1 (−6.8%) (Fig. 2). Overall, a trend towards a permanently decreased BMD was noted for Gruen zones 2, 6 and 7, whereas zones 3 and 5 show a trend towards holding the baseline or even increased BMD in the further course (Fig. 3).
THA implants
CLS stem
The mean BMD at 12 months post-operatively decreased in all Gruen zones, with the highest decrease seen for Gruen zone 7 (−18.3%) as well as 1 (−8.8%) and 6 (−8.7%) (Fig. 2). In the further course until 24 months the mean BMD increased again in most Gruen zones but remained decreased especially for zone 7 (−14.5%). Over the study period of 2 years, an overall trend towards a persistently and highly decreased BMD was observed for Gruen zone 7 and moderately for zones 1, 2 and 6 (Fig. 3).
Bicontact stem
The mean BMD decreased after 12 months for all Gruen zones except for zones 4 and 6. The highest decrease was seen proximally, for Gruen zones 1 (−11.4%) and 7 (−8.4%) (Fig. 2). In the further course until 24 months the mean BMD increased again in most Gruen zones but remained decreased especially for zone 1 (−14.5%). In contrast, in Gruen zones 4 and 6 the BMD exceeded the baseline. Over the study period of 2 years, an overall trend towards a persistently decreased BMD was observed for Gruen zone 1 and a moderately increase for zones 2, 6, and 4 (Fig. 3).
Discussion
This review analysis demonstrates that SHA stems should not generally be summarised as one single implant group, as the periprosthetic bone remodelling is highly dependent on the particular stem design. The data further show that SHA cannot completely avoid proximal bone remodelling and stress shielding. However, compared to the evaluated standard THA stems, some of the SHA designs seem to provide a closer physiological load transfer.
A periprosthetic BMD reduction was consistently observed for all four SHA implants in the proximal Gruen zones 1 and 7; however, with clear differences between the stems. For the Metha stem, a neck-preserving implant, the BMD decreased proximally (Gruen 1 and 7) and increased at the minor trochanteric level (Gruen 2 and 6). The increase at the minor trochanteric level is confirmed by clinical observations reporting about visible trabecular structures in Gruen zone 2 and 6 over the years, which can be considered as osseous integration due to the methapyseal load transfer [4]. In contrast, the BMD in the distal regions (Gruen 3, 4 and 5) only marginally changed and goes along with the clinical absence of thigh pain or cortical hypertrophy [5, 24, 25]. A decreased BMD was observed at the proximal level of the Metha stem, which increased in the further course, but did not completely return to the baseline. These results show that the Metha stem is able to achieve a metaphyseal load transfer, but cannot completely avoid a proximal reduction in periprosthetic BMD. Nevertheless, the Metha stem is able to avoid high rates of bone remodelling and stress shielding, which is confirmed by several studies reporting a stable implant with low rates of aseptic loosening [5, 25, 26].
The Nanos stem is designed to have an extended contact area at the calcar region. Similar to the Metha stem, the highest load transfer was found at Gruen 6 confirming the anchorage in the calcar region. The success of a stable osseous integration is confirmed by clinical migration studies [15, 27]. Only minor BMD changes were observed at the distal level in Gruen 3, 4 and 5 supporting the proximal load transfer of the Nanos stem. Nevertheless, also the Nanos stem showed postoperatively a clear primal decrease of the BMD (Gruen 1 and 7), which is in accordance with a previous finite element study [28]. Contrary to the Metha stem, the major BMD reduction was observed in the greater trochanteric region (Gruen 1) and is probably related to the higher load transfer at the calcar, striven by the implant design. Thus, similar to the Metha stem, the Nanos revealed a proximal decrease in BMD but also seems to achieve the main anchorage in the metaphyseal calcar region.
The Fitmore exhibited a completely different pattern of bone remodelling, with only a moderate decrease of the BMD at the proximal femur (Gruen 1 and 7). However, after only 12 months the BMD in Gruen 3 and 5 was increased and showed the highest tendency among the SHA designs for a further increase. This argues for a more distal anchorage and seems be related to the wider distal stem design of the Fitmore compared to the Nanos or Metha stem. This is supported by the clinical studies of Maier et al. [29], who reported about distal cortical hypertrophy (Gruen 3 and 5) in 63% of the patients. Although, no increased rate of thigh pain or loosening was observed after a mean of 3.3 years, the observations argue for a more distal fixation clearly below the lesser trochanter which might cause increased pattern of stress shielding in the further course.
For the CFP stem, a drastic BMD reduction in the proximal and calcar region (Gruen 1, 6 and 7) was noted initially, with a clear trend of a further progression. The high proximal bone loss is confirmed by Formica et al. [30], who described osteolysis in Gruen 1 and 7 in 84% of the patients and a significant cortical loss at the calcar in almost 30%. Similarly, Briem et al. [24] observed osteosclerotic bone formation in about 65% distally (Gruen 3 and 5) and none proximally (Gruen 1 and 7). A CT-based osteodensitometry study described a progressive cortical and cancellous bone loss proximally for the CFP stem and, as the bone substance did not change distally, a diaphyseal fixation was assumed [31]. In accordance with those results, we found the lowest BMD changes distally (Gruen 3 and 5), supporting the assumption that the CFP stem provides a distal load transmission. Noteworthy, despite the distal anchorage with a clear reduction of the proximal BMD, the long-term results of the CFP stem show a high rate of stability and low rate of aseptic loosing [32, 33].
Overall, the results of the analysed SHA stems impressively demonstrate that despite their uniform categorisation as short stems, highly different pattern of load transfer and periprosthetic BMD remodelling exist. For instance, the Metha and Nanos stem show a predominantly metaphyseal anchorage, while the Fitmore and CFP exhibit a more distal load transfer. Moreover, despite sharing a metaphyseal anchorage, the Metha stem shows a higher BMD reduction in the calcar region, while the Nanos revealed a higher reduction in the major trochanteric region, a phenomenon which can be related to the differing stem designs. Similarly, the CFP and Fitmore stem seem to share a more distal load transfer, but the latter did not reveal a high proximal bone loss. This impressively shows the challenge of comparing and classifying this heterogeneous group of SHA implants. In this context, several different classifications have been proposed [34, 35], but are all not satisfying in its entire.
This high variability of SHA stems aggravates a direct comparison with THA stems. In this study, the CLS and Bicontact were used for comparison as proven THA stems with low rates of aseptic loosening. The CLS stem was originally designed for a better proximal load transfer, but it is well known that a certain stress shielding tendency exist [36, 37]. This was also evident in our DXA analysis with a clear BMD reduction in Gruen 1 and 7. Accordingly, the Bicontact stem showed a proximal unloading, however to a lower degree and with a concurrent increase in Gruen 4 and 6 arguing for a combined deep metaphyseal and diaphyseal load transfer, as reported before [38]. This proximal unloading is a known phenomena for most standard THA stems [9, 11, 21, 39, 40], but as shown in this DXA review is also present in SHA. Nevertheless, the current study also shows that some of the SHA stems, such as the Metha, Nanos and Fitmore, seem to offer an overall lower rate of bone remodelling compared to the evaluated THA stems.
It also has to be noted that the Gruen zones were originally defined for standard THA and adapted to the single SHA designs [11, 41]. Due to the differences in length between SHA and THA, the Gruen zones do not correspond with regards to the femoral length but rather reflect the pattern of bone remodelling. This is an obvious advantage of the SHA stems, as they are shorter than THA stems and the bone remodelling occurs over a clear shorter femoral length.
Further limitations of this study have to be considered. First, we did not conduct a meta-analysis as the articles show certain variations in the study design. Second, up to now only a limited number of studies are available in the literature, especially considering the number of SHA designs available. Therefore the results can only account for the implants included and for a definite conclusion further studies are necessary. Third, the analysis only evaluated the bone remodelling according to the different stem designs. As patient demographics such as age, sex, BMD and body mass index (BMI) have significant impact on the outcome, these might have influenced our results. Fourth, we only included two conventional THA stems for comparison. Thus, strictly speaking the comparison only refers to those THA designs and different stem design might reveal differing pattern of bone remodelling. Finally, the follow-up of the currently available studies is relatively short, with many of them only reporting a follow-up of two years. As bone remodelling continues over time and long-term results are mandatory for definite conclusion, all SHA implants evaluated should further be monitored critically.
In conclusion, the systematic review shows that bone remodelling due to stress shielding occurs in SHA and THA stems. The calcar and greater trochanter regions exhibit the main bone loss, which is most likely related to the reduced proximal load transfer of the implants. Some, but not all evaluated SHA stems showed less periprosthetic BMD changes especially at the proximal femur (Gruen 1 and 7), arguing for a favourable and more physiological load transfer compared to conventional THA stems. Furthermore, it has to be noted that the femoral length where bone remodelling occurs is clearly shorter in SHA compared to THA. Nevertheless, the results also show that different short-stem designs lead to distinctly different patterns of bone remodelling and thus should not be judged as a single implant group.
References
Sumner DR (2015) Long-term implant fixation and stress-shielding in total hip replacement. J Biomech 48(5):797–800. https://doi.org/10.1016/j.jbiomech.2014.12.021
Kobayashi S, Saito N, Horiuchi H, Iorio R, Takaoka K (2000) Poor bone quality or hip structure as risk factors affecting survival of total-hip arthroplasty. Lancet 355(9214):1499–1504. https://doi.org/10.1016/S0140-6736(00)02164-4
Decking R, Rokahr C, Zurstegge M, Simon U, Decking J (2008) Maintenance of bone mineral density after implantation of a femoral neck hip prosthesis. BMC Musculoskelet Disord 9:17. https://doi.org/10.1186/1471-2474-9-17
Lerch M, von der Haar-Tran A, Windhagen H, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM (2012) Bone remodelling around the metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop 36(3):533–538. https://doi.org/10.1007/s00264-011-1361-0
Schmidutz F, Graf T, Mazoochian F, Fottner A, Bauer-Melnyk A, Jansson V (2012) Migration analysis of a metaphyseal anchored short-stem hip prosthesis. Acta Orthop 83(4):360–365. https://doi.org/10.3109/17453674.2012.712891
Freitag T, Hein MA, Wernerus D, Reichel H, Bieger R (2016) Bone remodelling after femoral short stem implantation in total hip arthroplasty: 1-year results from a randomized DEXA study. Arch Orthop Trauma Surg 136(1):125–130. https://doi.org/10.1007/s00402-015-2370-z
Kutzner KP, Pfeil D, Kovacevic MP, Rehbein P, Mai S, Siebert W, Pfeil J (2016) Radiographic alterations in short-stem total hip arthroplasty: a 2-year follow-up study of 216 cases. Hip Int 26(3):278–283. https://doi.org/10.5301/hipint.5000339
Wittenberg RH, Steffen R, Windhagen H, Bucking P, Wilcke A (2013) Five-year results of a cementless short-hip-stem prosthesis. Orthop Rev (Pavia) 5(1):e4. https://doi.org/10.4081/or.2013.e4
Aldinger PR, Sabo D, Pritsch M, Thomsen M, Mau H, Ewerbeck V, Breusch SJ (2003) Pattern of periprosthetic bone remodeling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int 73(2):115–121. https://doi.org/10.1007/s00223-002-2036-z
Salemyr M, Muren O, Ahl T, Boden H, Eisler T, Stark A, Skoldenberg O (2015) Lower periprosthetic bone loss and good fixation of an ultra-short stem compared to a conventional stem in uncemented total hip arthroplasty. Acta Orthop 86(6):659–666. https://doi.org/10.3109/17453674.2015.1067087
Albanese CV, Rendine M, De Palma F, Impagliazzo A, Falez F, Postacchini F, Villani C, Passariello R, Santori FS (2006) Bone remodelling in THA: a comparative DXA scan study between conventional implants and a new stemless femoral component. A preliminary report. Hip Int 16(Suppl 3):9–15
Gasbarra E, Celi M, Perrone FL, Iundusi R, Di Primio L, Guglielmi G, Tarantino U (2014) Osseointegration of Fitmore stem in total hip arthroplasty. J Clin Densitom 17(2):307–313. https://doi.org/10.1016/j.jocd.2013.11.001
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269 W264
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
Brinkmann V, Radetzki F, Delank KS, Wohlrab D, Zeh A (2015) A prospective randomized radiographic and dual-energy X-ray absorptiometric study of migration and bone remodeling after implantation of two modern short-stemmed femoral prostheses. J Orthop Traumatol 16(3):237–243. https://doi.org/10.1007/s10195-015-0335-1
Synder M, Krajewski K, Sibinski M, Drobniewski M (2015) Periprosthetic bone remodeling around short stem.Orthopedics. 38(3 Suppl):S40-S45
Jahnke A, Engl S, Seeger JB, Basad E, Rickert M, Ishaque BA (2015) Influences of fit and fill following hip arthroplasty using a cementless short-stem prosthesis. Arch Orthop Trauma Surg 135(11):1609-1614
Parchi PD, Ciapini G, Castellini I, Mannucci C, Nucci AM, Piolanti N, Maffei S, Lisanti M (2017) Evaluation of the effects of the Metha® short stem on periprosthetic bone remodelling in total hip arthroplasties: results at 48 months. Surg Technol Int 30:346-351
Zeh A, Pankow F, Röllinhoff M, Delank S, Wohlrab D (2013) A prospective dual-energy X-ray absorptiometry study of bone remodeling after implantation of the Nanos short-stemmed prosthesis. Acta Orthop Belg 79(2):174-180
Lazarinis S, Mattsson P, Milbrink J, Mallmin H, Hailer NP (2013)A prospective cohort study on the short collum femoris-preserving (CFP) stem using RSA and DXA. Primary stability but no prevention of proximal bone loss in 27 patients followed for 2 years. Acta Orthop 84(1):32-39
Wolf O, Mattsson P, Milbrink J, Larsson S, Mallmin H (2010) Periprosthetic bone mineral density and fixation of the uncemented CLS stem related to different weight bearing regimes: a randomized study using DXA and RSA in 38 patients followed for 5 years. Acta Orthop 81(3):286–291. https://doi.org/10.3109/17453674.2010.487238
Reiter A, Sabo D, Simank HG, Büchner T, Seidel M, Lukoschek M (1997) [Periprosthetic mineral density in cement-free hip replacement arthroplasty]. Z Orthop Ihre Grenzgeb 135(6):499-504
Lerch M, Kurtz A, Windhagen H, Bouguecha A, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM (2012) The cementless Bicontact stem in a prospective dual-energy X-ray absorptiometry study. Int Orthop 36(11):2211-2217
Stukenborg-Colsman CM, von der Haar-Tran A, Windhagen H, Bouguecha A, Wefstaedt P, Lerch M (2012) Bone remodelling around a cementless straight THA stem: a prospective dual-energy X-ray absorptiometry study. Hip Int 22(2):166–171. https://doi.org/10.5301/hip.2012.9227
von Lewinski G, Floerkemeier T (2015) 10-year experience with short stem total hip arthroplasty. Orthopedics 38(3 Suppl):S51–S56. https://doi.org/10.3928/01477447-20150215-57
Schnurr C, Schellen B, Dargel J, Beckmann J, Eysel P, Steffen R (2017) Low short-stem revision rates: 1-11 year results from 1888 total hip arthroplasties. J Arthroplast 32(2):487–493. https://doi.org/10.1016/j.arth.2016.08.009
Budde S, Seehaus F, Schwarze M, Hurschler C, Floerkemeier T, Windhagen H, Noll Y, Ettinger M, Thorey F (2016) Analysis of migration of the Nanos(R) short-stem hip implant within two years after surgery. Int Orthop 40(8):1607–1614. https://doi.org/10.1007/s00264-015-2999-9
Speirs AD, Heller MO, Taylor WR, Duda GN, Perka C (2007) Influence of changes in stem positioning on femoral loading after THR using a short-stemmed hip implant. Clin Biomech (Bristol, Avon) 22(4):431–439. https://doi.org/10.1016/j.clinbiomech.2006.12.003
Maier MW, Streit MR, Innmann MM, Kruger M, Nadorf J, Kretzer JP, Ewerbeck V, Gotterbarm T (2015) Cortical hypertrophy with a short, curved uncemented hip stem does not have any clinical impact during early follow-up. BMC Musculoskelet Disord 16:371. https://doi.org/10.1186/s12891-015-0830-9
Formica M, Cavagnaro L, Basso M, Zanirato A, Palermo A, Felli L (2017) What is the fate of the neck after a collum femoris preserving prosthesis? A nineteen years single center experience. Int Orthop 41(7):1329–1335. https://doi.org/10.1007/s00264-016-3350-9
Schmidt R, Gollwitzer S, Nowak TE, Nowak M, Haberle L, Kress A, Forst R, Muller LA (2011) Periprosthetic femoral bone reaction after total hip arthroplasty with preservation of the collum femoris: CT-assisted osteodensitometry 1 and 3 years postoperatively. Orthopade 40(7):591–598. https://doi.org/10.1007/s00132-011-1745-2
Briem D, Schneider M, Bogner N, Botha N, Gebauer M, Gehrke T, Schwantes B (2011) Mid-term results of 155 patients treated with a collum femoris preserving (CFP) short stem prosthesis. Int Orthop 35(5):655–660. https://doi.org/10.1007/s00264-010-1020-x
Kress AM, Schmidt R, Nowak TE, Nowak M, Haeberle L, Forst R, Mueller LA (2012) Stress-related femoral cortical and cancellous bone density loss after collum femoris preserving uncemented total hip arthroplasty: a prospective 7-year follow-up with quantitative computed tomography. Arch Orthop Trauma Surg 132(8):1111–1119. https://doi.org/10.1007/s00402-012-1537-0
Falez F, Casella F, Papalia M (2015) Current concepts, classification, and results in short stem hip arthroplasty. Orthopedics 38(3 Suppl):S6–S13. https://doi.org/10.3928/01477447-20150215-50
Khanuja HS, Banerjee S, Jain D, Pivec R, Mont MA (2014) Short bone-conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am 96(20):1742–1752. https://doi.org/10.2106/JBJS.M.00780
Schmidutz F, Woiczinski M, Kistler M, Schroder C, Jansson V, Fottner A (2017) Influence of different sizes of composite femora on the biomechanical behavior of cementless hip prosthesis. Clin Biomech (Bristol, Avon) 41:60–65. https://doi.org/10.1016/j.clinbiomech.2016.12.003
Aldinger PR, Thomsen M, Mau H, Ewerbeck V, Breusch SJ (2003) Cementless Spotorno tapered titanium stems: excellent 10-15-year survival in 141 young patients. Acta Orthop Scand 74(3):253–258. https://doi.org/10.1080/00016470310014157
Gronewold J, Berner S, Olender G, Hurschler C, Windhagen H, von Lewinski G, Floerkemeier T (2014) Changes in strain patterns after implantation of a short stem with metaphyseal anchorage compared to a standard stem: an experimental study in synthetic bone. Orthop Rev (Pavia) 6(1):5211. https://doi.org/10.4081/or.2014.5211
Merle C, Streit MR, Volz C, Pritsch M, Gotterbarm T, Aldinger PR (2011) Bone remodeling around stable uncemented titanium stems during the second decade after total hip arthroplasty: a DXA study at 12 and 17 years. Osteoporos Int 22(11):2879–2886. https://doi.org/10.1007/s00198-010-1483-z
Brodner W, Bitzan P, Lomoschitz F, Krepler P, Jankovsky R, Lehr S, Kainberger F, Gottsauner-Wolf F (2004) Changes in bone mineral density in the proximal femur after cementless total hip arthroplasty. A five-year longitudinal study. J Bone Joint Surg Br 86(1):20–26
Ercan A, Sokkar SM, Schmid G, Filler TJ, Abdelkafy A, Jerosch J (2016) Periprosthetic bone density changes after MiniHipTM cementless femoral short stem: one-year results of dual-energy X-ray absorptiometry study. SICOT J 2:40. https://doi.org/10.1051/sicotj/2016033
Acknowledgements
This study includes parts of the thesis of Y.S.G.
Funding
There was no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This systematic review retrospectively analysed published clinical data wherefore upon request of the Ethics Committee (Ethical Committee University of the LMU) neither a special ethics review nor a further ethical approval was necessary.
Informed consent
Due to the retrospective nature using anonymous data no additional informed consent of the patients was necessary.
Rights and permissions
About this article
Cite this article
Yan, S.G., Weber, P., Steinbrück, A. et al. Periprosthetic bone remodelling of short-stem total hip arthroplasty: a systematic review. International Orthopaedics (SICOT) 42, 2077–2086 (2018). https://doi.org/10.1007/s00264-017-3691-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3691-z