Abstract
Bone resorption in the proximal femur is commonly seen after total hip arthroplasty (THA). With dual energy X-ray absorptiometry (DXA), the amount of bone mass (BMD) after implantation of a total hip stem can be precisely determined. However, prospective evaluation of the change of bone mass around the stem is only available for selected stems and short-term follow-up (up to 36 months). We analyzed BMD in patients who had undergone uncemented THA by DXA. Only patients with good clinical outcome (Merle d’ Aubigné score > 12) were included to obtain normative data for regular bone response. Two separate studies were performed: a prospective longitudinal study over 84 months with baseline values acquired within the first postoperative week (group A) (n = 26 patients) and a separate cross-sectional study, median follow-up 156 (124-178) months (group B) (n = 35 patients). Regions of interest were defined according to Gruen (ROI 1-7) and as net average ROI (net avg) for the periprosthetic femoral bone. After the initial remodeling process (12 months), BMD was compared to the 84-month (longitudinal) and the 156-month (cross-sectional) follow-up values to determine long-term periprosthetic changes of bone mineral density. The longitudinal study (group A), after the initial bone remodeling, showed no relevant further bone loss for women and men with BMD values 1.19 ± 0.15 and 1.40 ± 0.19, respectively, 12 months (women 89.8%, men 93.6%), and 1.19 ± 0.13 and 1.36 ± 0.18, respectively, after 84 months (women 90.0%, men 91.3%) (P = 0.98, P = 0.08,) respectively. The distribution of the BMD around the stem changed during the first 12 months. The ROIs around the proximal stem (ROI 1 and 7) showed the lowest absolute values at the 12-month follow-up and BMD in ROI 7 decreased most during the further follow-up until 84 months. The cross-sectional study (group B) showed no significant difference in BMD (net avg) values at a median of 156 months follow-up compared to the 12-month values (group A) (women: P = 0.77, men: P = 0.44). Initial BMD, implant diameter, and body mass index did not influence BMD loss (net avg) in this study, whereas age showed a weak correlation with BMD loss. The results show that after the initial remodeling process, no relevant further bone loss (net avg) occurs up to 84 months postsurgery, and values after a median of 156 months are similar. Normative long-term changes in the periprosthetic bone can be demonstrated in defined ROIs after implantation of a tapered corundum-blasted titanium stem with a good clinical result.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Bone resorption in the proximal femur is commonly seen after total hip arthroplasty and has been observed predominantly in uncemented THA [1, 2, 3, 4, 5, 6, 7]. Bone loss can be caused by 4 main factors: remodeling as bony response to altered strain, i.e., stress shielding of the bone by the stiffer femoral component, aging of the femur, osteolysis stimulated by particulate debris, and metabolic disturbance. Consequences of wear-induced localized osteolysis are well known [8] whereas the effect of bone loss secondary to remodeling on prosthetic longevity is less understood, especially in the long term. It seems advantageous to be able to reliably monitor changes in bone mass, especially in the regions of stress transfer, in order to predict adverse clinical outcome. For this reason normative long-term data of patients with good clinical outcome and standard osteointegration are needed for comparison and monitoring.
Changes of periprosthetic bone mass after total hip arthroplasty (THA) cannot be accurately determined in conventional X-ray imaging because of change in variability of parameters during follow-up [9]. With dual energy X-ray absorptiometry (DXA), the amount of bone mass (BMD, g/cm2) after implantation of total hip stem can be determined with high precision [4, 6, 10, 11], minimal radiation exposure [12], and negligible affection by metallic implants [13]. The initial bone remodeling process with postoperative bone loss was found to reach a steady state after 12 months [6, 11]. Prospective evaluation of the change of bone mass around the stem is only available for short-term follow-up (up to 36 months) [1, 2, 3, 4, 5, 6, 7].
We performed a prospective longitudinal follow-up study of DXA measurements with a continuous 84-month follow-up. Additionally, we present the results of a separate cross-sectional study on patients’ median 156 months after implantation to gain information about the amount of long-term changes of BMD around the same type of femoral component.
Patients and Methods
Prospective Longitudinal Study
From March 1993 to October 1994, 94 of 128 patients assigned for implantation of an uncemented THA gave informed consent for a continuous postoperative follow-up. The diagnosis leading to THA was primary osteoarthritis in all cases. Patients with consumptive disease, hormone substitution, or metabolic disturbances were excluded from this study in order to obtain normative values. We included only patients without postoperative complications (infection, hematoma, implant failure, etc) and good clinical outcome to generate normative values for regular prosthetic osteointegration. Good clinical outcome was defined at a Merle d’Aubigné score of more than 12 of 18 possible points at 12 months after surgery and at the time of measurement [14].
Fifty-three of these patients fulfilled our inclusion criteria for the longitudinal study (Table 2) and were prospectively monitored for a period of 2 years [4]. Of this group, 26 patients (group A) had continuous follow-up for 84 months after the index surgery, using the same protocol as published previously [4]. The other patients were either lost to follow-up (n = 1), died (n = 3), had a complication with involvement of the femoral stem (n = 3), or did not have continuous DXA follow-up (n = 20) according to the study protocol.
Cross-sectional Study
For a separate cross-sectional study, a subgroup of 35 out of 354 patients (Table 2) treated with uncemented THA from January 1985 to December 1989 (group B), (median 156 (range: 124–178) months postoperatively) gave informed consent for a single DXA examination at the time of their 10–15-year follow-up visit and fulfilled the above inclusion criteria. The demographic data of the longitudinal and cross-sectional study revealed no significant differences in implant diameter and BMI. However, male patients involved in the cross-sectional study were younger than those in the longitudinal study (P = 0.11).
Implant and Postoperative Regime
In all patients investigated, uncemented THA (press-fit titanium Spotorno stem [15], Sulzer Orthopedics) had been implanted at our institution. Implant size refers to the diameter at the distal third of the stem in mm.
All patients underwent the same standardized perioperative treatment (single dose or 24-h i.v. antibiotics, low-molecular-weight heparin s.c., indomethacin for 14 days, physical therapy for 3 weeks) and partial weight bearing for 6 weeks.
DXA Analysis
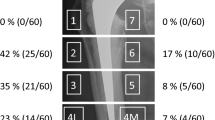
BMD measurements were performed by DXA with the QDR 2000 (Hologic Inc., Waltham, MA). The patient’s leg was fixed in 12° internal rotation and 5° flexion using a special device to achieve reproducible projection and to minimize malrotation error [3, 16]. Periprosthetic regions of interest (ROI) were placed around the stem according to Gruen [17] (Fig. 1). ROI 1-3 are lateral and ROI 5-7 are medial dividing the stem into thirds, with a distance of two pixels (P) to the external rim of the femoral cortical bone. Because of the variability of the level of the femoral neck, the proximal-medial ROI 7 was placed individually in length. ROI 4 was positioned at the tip of the stem with a standard length of 15 pixels. The overall BMD were summarized in the ROIs net average. Percentage coefficient of variation was assessed by two consecutive measurements of 5 patients at 2 days according to the following expression (Table 1):

(Variables are defined as d = difference between two measurements, n = number of measurement pairs, m1 and m 2 = means of the first and second measurements.)
Sites of BMD measurement according to Gruen et al. [17].
Results were measured as BMD [g/cm2]. The follow-up values were recorded postoperatively (within 1 week after surgery, range 2–5 days) and at 3, 6, 12, 36, 60, 84 months in the longitudinal study and at a median of 156 months in the cross-sectional study [4, 6, 11].
Radiographic Analysis
Radiographs of the affected hip were taken immediately postoperatively, at 12 months and 84 months in group A and immediately postoperatively and at long-term follow-up (156 [124-178] months) in group B. The films were analyzed according to Gruen and Engh [17, 18]. A femoral stem was regarded loose if radiolucent lines > 2 mm were present around the entire implant, or if change in the varus/valgus > 2° occurred on serial radiographs.
Statistics
Absolute BMD values were used for comparison of netavg BMD between different time points in the follow-up. All other analyses concerning BMD in the longitudinal study are based on relative BMD values, with the postoperative measurement being the reference value.
Absolute and relative BMD values, as well as demographic parameters, are described by mean and standard deviation. Normal distribution was tested by the Kolomogorov-Smirnov Test. Since no relevant deviations could be observed, mean values were compared by the one-sample t-test in cases of paired data and by the two-sample t-test in cases of unpaired data. The Pearson correlation coefficient was used to evaluate the correlation between age and initial BMD values. Univariate linear regression analysis was used to investigate the influence of several factors on bone loss. All statistical tests were carried out two-sided. Results with P-values lower than 0.05 are described as significant. However, due to multiple testing, only the primary analyses, namely, the comparisons of 12 months BMD values with 84 months values (paired design) and with median 156 months values (unpaired design), can be interpreted as confirmatory. All other analyses are exploratory and the resulting P-values have to be interpreted accordingly. The statistic software SAS (SAS Insitute; Cary, NC, USA), Version 8 for Windows, was used for data analysis.
Results
Differences Between Males and Females
Significant differences in absolute periprosthetic BMD were found after 12 months, 84 months (group A) and after a median of 156 months (group B) around the stem between males and females (P = 0.006, P = 0.003, P = 0.03), respectively. However, the relative values in the longitudinal study showed no significant differences at the two selected follow-up examinations between males and females (P = 0.18, 0.62). Furthermore, no difference in change of relative BMD values from 12 to 84 months was observed between males and females (P = 0.22) (Tables 4 and 5).
Longitudinal Study (group A)
After the initial 12-month remodeling process, absolute BMD around the stem remained nearly at a stable level until 84 months, without significant changes (women: 1.19 ± 0.15 (12 mo), 1.19 ± 0.13 (84 mo), P = 0.98; men: 1.40 ± 0.19 (12 mo), 1.36 ± 0.18 (84 mo), P = 0.08) (Fig. 2). Mean relative values at 12 months were: women 89.8%, men 93.6% and at 84 months: women 90.0%, men 91.3%.
Relative BMD values at 12 months were higher in the distal ROIs (ROI 3, 5) as compared with the proximal ROIs (ROI 1, 7). The difference in BMD between ROIs 5 and 7 became still larger during the later follow-up from 12 to 84 months.
There was a weak correlation between initial BMD and age at primary surgery in men (r = 0.50); no correlation between these parameters was found in women (r = −0.14).
Linear regression analysis revealed that age at primary surgery was also weakly correlated to later bone loss in both males and females. Other factors such as initial BMD, BMI, or implant diameter did not relate to bone loss between 12 and 84 months (Table 3).
Cross-sectional Study ( group B )
Male patients in the cross-sectional study were younger than those in the longitudinal study (P = 0.11). Other demographic parameters were equally distributed in both studies. Bone mass (net average) at a median of 156 (124–178) months (group B) revealed no significant differences compared to the 12 months postoperative values of group A (women: P = 0.77, men: P = 0.44) (Tables 4 and 5). Also in group B, lowest absolute values were observed in ROI 1 and ROI 7.
Radiographic Analysis
There was no sign of radiographic loosening in any of the stems involved in this study. No stress shielding in the proximal femur in both groups according to Engh and Bobyn [18] and no radiolucent lines according to Gruen et al. [17] were detected. Despite evidence of migration and aseptic loosening of the acetabular cup in 2 cases and acetabular revisions in 4 cases, no radiographic evidence of femoral osteolysis or migration of the stem was found. These cases were not excluded from the study because only migration led to revision and clinical symptoms were minimal with regular activity level in all patients [19].
Discussion
Dual energy X-ray absorptiometry is a precise method for quantifying bone mass and small changes in bone mineral density around femoral implants after total hip arthroplasty. To obtain baseline values for comparison, we used the postoperative values, measured within a week after the index surgery [6, 11, 20]. Short-term prospective studies have shown that maximum bone remodeling occurs until 6 months after surgery and reaches a plateau phase near the end of the first year [3]. After this period, a slow but steady decline in BMD has been described by several authors for different types of implants [3, 6, 7]. However, those studies only observed periods up to 36 months postoperatively.
All patients in our series with mid-to long-term follow-up had a good clinical outcome, so this bone response data can be regarded as typical for a well-functioning Spotorno stem. Despite excellent clinical results [21, 22], proximal femoral remodeling can occur, resulting in proximal bone loss. After the plateau had been reached, BMD in all ROIs (net average) remained stable for the whole observation period of 84 months. Despite the lack of radiographic evidence, the distribution of BMD during the observation period showed a continuous remodeling process with a slow decline of proximal BMD and stable conditions in the distal regions of the stem. This observation is somewhat in contrast to the concept of proximal load transfer advocated by the designers of the implant [15], who suggested proximal intertrochanteric press-fit. Our observations suggest that load transfer in this stem occurs mostly in the meta-diaphyseal region of the femur.
The cross-sectional long-term study after a median 156-month period (group B) showed no significant differences from the 12-month values of the longitudinal study, however, a slow decline in BMD was noticed. This phenomenon can be explained by the natural decline in BMD in the course of the natural aging process, as implant diameter and BMD showed no significant differences between the two groups [23]. If not accounted for by prospective observations (group A), individual differences (cohort effects) greatly bias interpretation of the long-term cross-sectional differences (group B) as representative of longitudinal change, because interindividual variability of BMD is high. Due to this variability, absolute normative values cannot be given and BMD changes are given in percentage of the initial value. Thus, single DXA examinations during follow-up have no prognostic value as the initial postoperative values are unknown. It should further be noted that relative individual response patterns over the whole observation period after THA were almost identical despite large differences in absolute BMD values found in both groups.
The BMD changes reported in this study were smaller than those reported by others [18, 24, 25], however, there are relevant differences between the present study and other reports. These include different techniques for determining bone loss [18], cross-sectional study design [24, 25] and design characteristics of femoral implants [18, 24, 25]. Stiff uncemented components, especially those made of cobalt-chrome, transmit load more distally and are prone to be associated with progressive bone loss proximally [18]. We suggest that the more flexible titanium stem used in this study offloads more proximally with less bone loss, because it does not fill the femoral canal distally. Our data represent longitudinally measured BMD changes in patients with this specific type of titanium stem. Similar changes were reported in a canine model, where DXA was used [25].
Variable bone response cannot be attributed to implant design until one measurement method and a standard protocol are applied across all patients. The potential predictive value of initial bone quality (i.e., bone mass) on progressive bone resorption has not been detected in our prospective study, but may yet be seen as these patients are followed in later years; at this time (84 months), however, no significant relationship was found between initial BMD and changes in bone mass following this type of femoral stem. Moreover, the absence of an observed effect may also be due to the subjective exclusion of patients as candidates for uncemented THR based on radiographic or surgical evidence of poor bone quality. Finally, the pattern of bone resorption, determined radiographically, has previously been reported to occur in a proximal to distal direction as we found in our study [18, 26]. In our protocol using the method of Gruen [17], we can reproducibly quantify the prospective long-term bone remodeling in the proximal femur.
Some limitations of this study should be considered: 40% of longitudinal patients had to be excluded mostly due to incomplete continuous DXA follow-up even though they had been radiographically and clinically followed with excellent outcome. In addition, the cross-sectional DXA group included only 10% of patients who received this stem, but > 90% of patients alive were reviewed clinically [22]. Clearly there is potential for bias. However, there was nothing to suggest that patients not included in these groups were different than the study group in terms of age, BMI and implant diameter [22]. Also, both pre- and postmenopausal women have been included in the study, most of them in their mid 50’s at the time of surgery. It is well known that the menopause is a period of rapid bone loss in women, but no significant differences were found in our study.
Furthermore, we did not use the normal contralateral hip as control for initial BMD for three reasons. First, from the available literature it would appear that up to 20% difference in the diseased side can preexist [27]. Second, there is no published evidence that preoperative pain can lead to BMD loss in patients suffering from OA, and the resumption of normal activity post-op increases bone mass around a hip stem. Nevitt et al. [27] concluded in their Study of Osteoporotic Fractures Research Group that “Elderly Caucasian women with moderate to severe radiographic hip OA had higher BMD in the hip, spine, and appendicular skeleton than did women without hip OA. Our findings are consistent with a role of elevated BMD in the pathogenesis of hip OA.” Third, some of the patients required THR on the contralateral side during the observation period thus preventing its use as a control.
DXA for the assessment of THA remains an experimental method that requires prospective observations. Its relatively high cost precludes routine examinations and the method cannot yet be recommended as part of standard follow-up. It is only of value if baseline postoperative measurements or ideally prospective follow-up are available for the individual patient. Although DXA cannot replace standard methods for diagnosis of osteointegration or subsidence and wear, we do believe that the data available with this technique will enhance our understanding of bone tissue adaptation around the hip stem. Currently, many decisions about successful implant design are based on computer simulation of bone response and in vitro testing [28, 29, 30, 31], BMD data from patients with THA will validate or refute such extrapolations.
Finally, with continued recruitment and follow-up evaluation of patients, especially when the series includes a wider range of conditions and a standard assessment protocol, DXA may become a useful tool for studying bone response for particular types of THA. Adverse remodeling can be determined earlier than with routine radiographic assessment. This would be particularly useful for the evaluation of new implants prior to widespread use.
References
KC Ang S Das De JC Goh SL Low K Bose (1997) ArticleTitlePeriprosthetic bone remodelling after cementless total hip replacement. A prospective comparison of two different implant designs. J Bone Joint Surg Br 79 675–679 Occurrence Handle10.1302/0301-620X.79B4.7410 Occurrence Handle1:STN:280:ByiA1M3lsFQ%3D Occurrence Handle9250764
BJ Kiratli JP Heiner AA McBeath MA Wilson (1992) ArticleTitleDetermination of bone mineral density by dual x-ray absorptiometry in patients with uncemented total hip arthroplasty. J Orthop Res 10 836–844 Occurrence Handle1:STN:280:ByyD3Mbns1A%3D Occurrence Handle1403298
BJ Kiratli MM Checovich AA McBeath MA Wilson JP Heiner (1996) ArticleTitleMeasurement of bone mineral density by dual-energy x-ray absorptiometry in patients with the Wisconsin hip, an uncemented femoral stem. J Arthroplasty 11 184–193 Occurrence Handle8648314
D Sabo A Reiter HG Simank M Thomsen M Lukoschek V Ewerbeck (1998) ArticleTitlePeriprosthetic mineralization around cementless total hip endoprosthesis: longitudinal study and cross-sectional study on titanium-threaded acetabular cup and cementless Spotorno stem with DEXA. Calcif Tissue Int 62 177–182 Occurrence Handle10.1007/s002239900413 Occurrence Handle1:CAS:528:DyaK1cXnslGmsQ%3D%3D Occurrence Handle9437053
C Trevisan M Bigoni G Randelli EC Marinoni G Peretti S Ortolani (1997) ArticleTitlePeriprosthetic bone density around fully hydroxyapatite coated femoral stem. Clin Orthop 340 109–117
PK Venesmaa HP Kroger HJ Miettinen JS Jurvelin OT Suomalainen EM Alhava (2001) ArticleTitleMonitoring of periprosthetic BMD after uncemented total hip arthroplasty with dual-energy X-ray absorptiometry — a 3-year follow-up study. J Bone Miner Res 16 1056–1061 Occurrence Handle1:STN:280:DC%2BD38%2FhtFKkug%3D%3D Occurrence Handle11393782
K Yamaguchi K Masuhara K Ohzono N Sugano T Nishii T Ochi (2000) ArticleTitleEvaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. The influence of the extent of porous coating. J Bone Joint Surg Am 82-A 1426–1431 Occurrence Handle1:STN:280:DC%2BD3crgsFyjug%3D%3D Occurrence Handle11057471
WH Harris (1995) ArticleTitleThe problem is osteolysis. Clin Orthop 311 46–53 Occurrence Handle7634590
JD West MB Mayor JP Collier (1987) ArticleTitlePotential errors inherent in quantitative densitometric analysis of orthopaedic radiographs. A study after total hip arthroplasty. J Bone Joint Surg Am 69 58–64 Occurrence Handle1:STN:280:BiiC3cbjslc%3D Occurrence Handle3805071
B Cohen N Rushton (1995) ArticleTitleAccuracy of DEXA measurement of bone mineral density after total hip arthroplasty. J Bone Joint Surg Br 77 479–483 Occurrence Handle1:STN:280:ByqB28zmsVM%3D Occurrence Handle7744941
H Kroger H Miettinen I Arnala E Koski N Rushton O Suomalainen (1996) ArticleTitleEvaluation of periprosthetic bone using dual-energy x-ray absorptiometry: precision of the method and effect of operation on bone mineral density. J Bone Miner Res 11 1526–1530 Occurrence Handle1:STN:280:ByiD2cvnvVY%3D Occurrence Handle8889853
WA Kalender (1992) ArticleTitleEffective dose values in bone mineral measurements by photon absorptiometry and computed tomography. Osteoporos Int 2 82–87 Occurrence Handle1:STN:280:By2C28zmvVU%3D Occurrence Handle1536984
HC Cattermole JL Cunningham (1995) ArticleTitleInfluence of metallic implants adjacent to the measurement site on DEXA measurements: a phantom study. Phys Med Biol 40 1885–1896 Occurrence Handle10.1088/0031-9155/40/11/008 Occurrence Handle1:STN:280:BymC283ns1A%3D Occurrence Handle8587938
JJ Callaghan SH Dysart CF Savory WJ Hopkinson (1990) ArticleTitleAssessing the results of hip replacement. A comparison of five different rating systems. J Bone Joint Surg Br 72 1008–1009 Occurrence Handle1:STN:280:By6D28%2Fmtlc%3D Occurrence Handle2246281
L Spotorno S Romagnoli N Ivaldo G Grappiolo E Bibbiani DJ Blaha TA Guen (1993) ArticleTitleThe CLS system. Theoretical concept and results. Acta Orthop Belg 59 IssueIDsuppl 1 144–148 Occurrence Handle8116390
ES Mortimer L Rosenthall I Paterson JD Bobyn (1996) ArticleTitleEffect of rotation on periprosthetic bone mineral measurements in a hip phantom. Clin Orthop 324 269–274 Occurrence Handle8595767
TA Gruen GM McNeice HC Amstutz (1979) ArticleTitle“Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141 17–27 Occurrence Handle477100
CA Engh JD Bobyn (1988) ArticleTitleThe influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop 231 7–28
HG Simank DR Brocai D Reiser M Thomsen D Sabo M Lukoschek (1997) ArticleTitleMiddle-term results of threaded acetabular cups. High failure rates five years after surgery. J Bone Joint Surg Br 79 366–370 Occurrence Handle10.1302/0301-620X.79B3.7273 Occurrence Handle1:STN:280:ByiA38vhsVU%3D Occurrence Handle9180310
H Kroger E Vanninen M Overmyer H Miettinen N Rushton O Suomalainen (1997) ArticleTitlePeriprosthetic bone loss and regional bone turnover in uncemented total hip arthroplasty: a prospective study using high resolution single photon emission tomography and dual-energy X-ray absorptiometry. J Bone Miner Res 12 487–492 Occurrence Handle1:STN:280:ByiB3s7hvFw%3D Occurrence Handle9076593
R Siebold G Scheller U Schreiner L Jani (2001) ArticleTitleLong-term results with the cement-free Spotorno CLS shaft. Orthopade 30 317–322 Occurrence Handle10.1007/s001320050614 Occurrence Handle1:STN:280:DC%2BD3Mzls1Glug%3D%3D Occurrence Handle11417240
PR Aldinger SJ Breusch M Lukoschek H Mau V Ewerbeck M Thomsen (2003) ArticleTitle10-15 year follow-up of the cementless Spotorno stem. J Bone Joint Surg Br 85 B
O Lofman L Larsson I Ross G Toss K Berglund (1997) ArticleTitleBone mineral density in normal Swedish women. Bone 20 167–174 Occurrence Handle9028542
DJ Kilgus EE Shimaoka JS Tipton RW Eberle (1993) ArticleTitleDual-energy X-ray absorptiometry measurement of bone mineral density around porous-coated cementless femoral implants. Methods and preliminary results. J Bone Joint Surg Br 75 279–287 Occurrence Handle1:STN:280:ByyC1cnovFI%3D Occurrence Handle8444950
CK McCarthy GG Steinberg M Agren D Leahey E Wyman DT Baran (1991) ArticleTitleQuantifying bone loss from the proximal femur after total hip arthroplasty. J Bone Joint Surg Br 73 774–778 Occurrence Handle1:STN:280:By6A2szkt1Q%3D Occurrence Handle1894664
AS Carlsson CF Gentz L Linder (1983) ArticleTitleLocalized bone resorption in the femur in mechanical failure of cemented total hip arthroplasties. Acta Orthop Scand 54 396–402 Occurrence Handle1:STN:280:BiyB38jgvFw%3D Occurrence Handle6858658
MC Nevitt NE Lane JC Scott MC Hochberg AR Pressman HK Genant SR Cummings (1995) ArticleTitleRadiographic osteoarthritis of the hip and bone mineral density. The Study of Osteoporotic Fractures Research Group. Arthritis Rheum 38 907–916 Occurrence Handle1:STN:280:ByqA3snkvVA%3D Occurrence Handle7612040
M Doblare JM Garcia (2001) ArticleTitleApplication of an anisotropic bone-remodelling model based on a damage-repair theory to the analysis of the proximal femur before and after total hip replacement. J Biomech 34 1157–1170 Occurrence Handle10.1016/S0021-9290(01)00069-0 Occurrence Handle1:STN:280:DC%2BD3Mvmt1eqsA%3D%3D Occurrence Handle11506786
R Huiskes (1990) ArticleTitleThe various stress patterns of press-fit, ingrown, and cemented femoral stems. Clin Orthop 261 27–38 Occurrence Handle2245558
R Huiskes H Weinans HJ Grootenboer M Dalstra B Fudala TJ Slooff (1987) ArticleTitleAdaptive bone-remodeling theory applied to prosthetic-design analysis. J Biomech 20 1135–1150 Occurrence Handle1:STN:280:BieC3Mrkt1E%3D Occurrence Handle3429459
J Kerner R Huiskes GH van Lenthe H Weinans B van Rietbergen CA Engh AA Amis (1999) ArticleTitleCorrelation between pre-operative periprosthetic bone density and post-operative bone loss in THA can be explained by strain-adaptive remodelling. J Biomech 32 695–703 Occurrence Handle10.1016/S0021-9290(99)00041-X Occurrence Handle1:STN:280:DyaK1MzisF2ntg%3D%3D Occurrence Handle10400357
Acknowledgements
The authors thank Dorothea Rösch, radiographic technician, for conducting the DXA measurements. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aldinger, P., Sabo, D., Pritsch, M. et al. Pattern of Periprosthetic Bone Remodeling Around Stable Uncemented Tapered Hip Stems: A prospective 84-month follow-up study and a Median 156-month Cross-Sectional Study with DXA . Calcif Tissue Int 73, 115–121 (2003). https://doi.org/10.1007/s00223-002-2036-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-002-2036-z