Abstract
Purpose
Flexion contracture has been shown to impair function and reduce satisfaction following total knee arthroplasty (TKA). The aim of this study was to identify modifiable intra-operative variables that predict post-TKA knee extension.
Methods
Data was collected prospectively on 95 patients undergoing total knee arthroplasty, including pre-operative assessment, intra-operative computer assisted surgery (CAS) measurements and functional outcome including range of motion at one year. Patients were divided into two groups: those with mild flexion contracture (> 5°) at the one-year follow-up and those achieving full extension.
Results
The sagittal orientation of the distal femoral cut differed significantly between groups at the one-year follow-up (p = 0.014). Sagittal alignment of greater than 3.5° from the mechanical axis was shown to increase the relative risk of a mild flexion contracture at one-year follow-up by 2.9 times, independent of other variables.
Conclusion
Increasing the sagittal alignment of the distal femoral cut more than 3.5° from the mechanical axis is an independent risk factor for clinically detectable flexion contracture one year from index procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Loss of knee extension during functional activities is commonly found with advancing age [1]. However, degenerative conditions such as osteoarthritis are associated with much greater loss of knee extension. Total knee arthroplasty (TKA) is an established and highly successful surgical procedure for the treatment of knee osteoarthritis [2] and an important outcome of TKA is the restoration of full extension to the osteoarthritic knee [3]. Indeed, patients who have a flexion contracture report worse postoperative outcomes, and the degree of flexion contracture directly correlates with worse postoperative outcomes [4]. Flexion contracture in the operated limb can also lead to mechanical overload and worsening disease progression in the contralateral limb [5].
Despite the apparent importance of knee extension to function and quality of life, the majority of studies on post-TKA knee range of motion have focused on maximum flexion [6–11]. Nevertheless, a number of risk factors have been identified that potentially predict postoperative flexion contracture. These include pre-existing flexion contracture [12], pre-operative hyperextension of greater than 9° and male gender [4]. The identification of modifiable intra-operative risk factors would allow the operating surgeon to address these with a possible corresponding improvement in postoperative extension. To date, only the depth of the distal femoral cut has been shown to significantly alter flexion contracture [13, 14]. However, distal femoral cut sagittal alignment may contribute to the sagittal alignment of the prosthetic joint by determining the relationship between the femoral component and the long axis of the femur, and could be related to the degree of postoperative flexion contracture. While research has examined this relationship in the context of uni-compartmental knee arthroplasty (UKA) [15–17], there is a paucity of information for TKA.
Historically, flexion contracture has been assessed intraoperatively by visual inspection of the knee at full extension; however, Gallie et al. reported inaccuracies of 5.57° on average for this method [18]. Advances in technology have allowed for increased accuracy and improved implant alignment through the use of computer-assisted surgery for TKA (CAS-TKA) [19]. To date however, little research has been performed using the intra-operative data provided by the CAS systems to try to reduce flexion contracture.
To address the gap in the current knowledge, the aim of this study was to identify intra-operative predictors of knee flexion contracture following primary TKA. It was hypothesized that knee flexion contracture at one-year follow-up would be associated with pre-operative extension, implant size, distal femoral resection depth and distal sagittal alignment of the femoral component.
Materials and methods
A retrospective analysis of prospectively collected data was performed on patients operated on by the senior author between July 2007 and May 2009. Inclusion criteria were patients electing to undergo primary TKA with CAS (Stryker Precision® Navigation, Stryker, Kalamazoo, MI, USA), including simultaneous or sequential bilateral arthroplasties, with a minimum one-year follow-up. Exclusion criteria included inflammatory arthritis, previous arthroplasty, and inability to comply with the postoperative follow-up requirements. Of the 103 consecutive patients that underwent primary TKA with CAS, 95 were eligible for inclusion in the analysis. A fellowship-trained knee surgeon performed all arthroplasties in a fully-cemented, posterior-stabilized fashion (Genesis II, Smith Nephew ®). The data collection protocol was approved by the local ethics committee. All participation was purely voluntary and patients provided written informed consent prior to data collection.
Pre-operatively
Patients were assessed between one and three months prior to surgery by a trained research associate. Pre-operative data included sex, date of birth, height and weight. The Oxford Knee Score questionnaire was administered and a hand-held goniometer was used to measure knee range of motion. All measures were prospectively entered into a data management system (SOCRATES, Ortholink, Balmain, NSW, AUS). In total, 95 knees were examined, with mean age 69.4 years (range, 53–84 years). The sample consisted of 44 males and 51 females with an average BMI of 29.6 (range, 18–55).
Intra-operatively
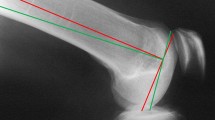
Navigated total knee arthroplasty was undertaken by the senior author according to his standard technique. Navigation active trackers were affixed to the tibia and femur of the operated limb in accordance with the manufacturer’s instructions. The hip’s centre of rotation was calculated by the navigation package prior to medial arthrotomy and registration of femoral and tibial anatomical landmarks using a hand-held digitiser [20]. Coronal, sagittal and axial alignments of the knee were measured with the surgeon cupping the heel and allowing gravity to bring the knee to maximal extension. Cemented posterior stabilised TKA was then undertaken in a standard fashion. Maximal knee extension was measured again following prosthetic implantation, after capsule and skin closure. Other intra-operative measures recorded were implant size and femoral resection depth and orientation. The sagittal orientation of the distal femoral cut was made at this time by the surgeon, based on the patient’s anatomy and the avoidance of anterior femoral notching to accommodate optimal femoral component size. The published accuracy of passive CAS is less than 1° in all axes of knee rotation and 1 mm [20, 21]; therefore, individual measurements were recorded to the nearest whole number and the mean values reported to the nearest decimal.
Clinical follow-up
During routine follow-up one year from the date of the TKA (± 1 months), patients completed an Oxford Knee score questionnaire and had their knee range of motion assessed by a trained research assistant using a manual goniometer.
Statistical analysis
The pre-operative and postoperative clinical data were extracted from the data management system, while the intraoperative measurements were recorded and stored by the navigation system. Normality of the data was assessed using the Kolmogrov-Smirnov model and a p value of 0.05 was considered significant for all tests. A threshold of 5° was used to designate clinically relevant flexion contracture where group 1 consisted of those with flexion contracture of less than 5° and group 2 had flexion contracture of 5° and above.
Baseline differences in the demographics of groups 1 and 2 were examined using Mann–Whitney U tests where appropriate. Differences in gender and operative side were examined using chi-squared cross tabulation. Possible confounders were examined using the Spearman rank correlation coefficient to assess any association with postoperative flexion contracture. Confounders examined included femoral distal resection [12, 14] and pre-operative flexion contracture [3, 11] measured by both goniometer and CAS. In addition, Oxford knee scores were compared between the two groups, specifically the Oxford pain score, Oxford climb stairs and overall knee score. Mann–Whitney U tests were also used to test for differences between groups for intraoperative CAS measurements and postoperative function scores.
Results
The group without flexion contracture (group 1) contained 63 knees while the group experiencing mild flexion contracture (Group 2) contained 32 (Table 1 and 2). There were no significant differences between groups with regards to gender (group 1 [31:32, male: female] and group 2 [13:19]; χ2 = 0.634, df = 4, P = 0.959) or operated side (group 1 [26:37, left: right] and group 2 [18:14]; χ2 = 1.915, df = 4, P = 0.751).
No statistical co-dependence was found between distal resection depth or pre-operative flexion contracture (measured both with the goniometer and with CAS) and postoperative navigation flexion contracture (Table 3).
The sagittal orientation of the distal femoral cut measured intraoperatively by the CAS system was significantly different between the two groups (P = 0.014) (Table 4). However, the difference between the group means was small, with the average femoral cut angle for group 1 being 3.15° and 3.77° for group 2. Further analysis revealed that a distal femoral cut angle of greater than 3.5° increased the relative risk of a clinically significant flexion contracture by 2.9-fold at one-year follow-up, independently of other variables (Table 5). Analysis of the postoperative Oxford knee scores failed to reveal any statistically significant differences in self-reported pain (p = 0.85), ability to climb stairs (p = 0.73) or overall score (p = 0.61) between the two groups (Table 6).
Discussion
The aim of the present study was to identify intra-operative predictors of knee flexion contracture following primary TKA, based on measures recorded by CAS. The results indicated that a relationship exists between the sagittal orientation of the distal femoral cut measured intra-operatively and flexion contracture measured with hand-held goniometry at the one-year postoperative follow-up.
This was the only variable examined in the present study to show a statistically significant relationship with flexion contracture at one-year follow-up. Performing a distal femoral cut with greater than 3.5° of flexion induces a 2.9-fold increase in the risk of having a significant flexion contracture at one-year follow-up. Oxford pain and function scores however, showed no significant difference between the two groups analysed, perhaps due to the limitation of the relatively small sample size for such a highly functional cohort.
There is little consensus in the literature regarding the amount of flexion contracture considered clinically relevant. Many studies have reported on knees with large flexion contracture [12, 22, 23] compared to a “normal” population. The original Knee Society score, prior to the Insall modification of 1993, considered flexion contracture of 0–4° as normal [24]. While this number was subsequently changed, no rationale was given and this classification was also used by a later study [13]. Groups were classified as having either no flexion contracture (4° and below) in group 1 or mild flexion contracture (5–15°) in group 2. Others have demonstrated a significant difference between maximal extension during gait between young subjects and elderly subjects with the young subjects displaying flexion of 1–4° on average and the elderly 5–8° [25]. While no patients experienced flexion contracture in excess of 15° at one-year follow-up in this study, there are problems associated with even a mild knee flexion contracture. Flexion contracture is known to increase muscular demand and associated physiological responses such as heart rate and muscle energy consumption during locomotion [26].
Previous work has shown that pre-existing flexion contracture, as well as age and gender, can lead to an increased risk of flexion contracture 12 months postoperatively [4, 12]. The present study fails to demonstrate an association between pre-operative goniometer measures or pre-operative navigation data and flexion contracture at the 12-month follow-up. Age and gender also showed no association with 12-month flexion contracture. The different results between this study and previous work [4, 12] could be attributed to differences in operative procedure or the use of CAS for the assessment of the preoperative flexion contracture. Indeed the relative accuracy of goniometer measurements has already been reported [18] and it was compared to intra-operative navigation data in our study and showed no statistical correlation (p = 0.07).
Studies have shown that using a larger femoral component could increase the patellofemoral contact force in TKA and possibly restrict knee range of motion including introducing a flexion contracture [27, 28]. However, the results of this study do not show any correlation between implant size and flexion contracture 12 months postoperatively. A possible explanation might be that the flexion contracture is more correlated to a mismatch between the distal femoral anatomy and the implant size [29, 30] than to the implant size itself.
Varying distal resection depth has previously been used to correct flexion contracture by reducing muscular tension with mixed results [31, 32]. Soft tissue tension has been demonstrated to effect both extension and stability [33]. Distal resection depth was therefore examined as a possible confounder in the present study and was not shown to be associated with loss of extension at 12 months (p = 0.31). This could be due to the use of the navigation system to balance the extension and flexion gaps.
Limitations of this study included the use of a single type of prosthesis and the length of postoperative follow-up. However, these results should be compared with other designs of prosthesis. In addition, the 12-month investigation may not have been adequate to observe resolution of flexion contracture in a majority of patients [22]. Finally, the difference between the groups for distal femoral cut angle, even if statistically significant, has to be modulated by the accuracy of the navigation system, which is less than 1° [20].
Conclusion
This is the first study to identify modifiable intra-operative variables that potentially predict post-TKA knee flexion contracture, based on intra-operative measures recorded by CAS. Of all variables examined, femoral cut angle was associated with flexion contracture at 12 months postoperative follow-up. For angles greater than 3.5°, a risk of 2.9 times for a clinically mild flexion contracture at 12 months follow-up was observed. The femoral component of the posterior stabilised Genesis II total knee arthroplasty should be implanted with no more than 3.5° of flexion to reduce the risk of flexion contracture at one year.
References
Begg RK, Sparrow WA (2006) Ageing effects on knee and ankle joint angles at key events and phases of the gait cycle. J Med Eng Technol 30(6):382–389
Dixon MC, Brown RR, Parsch D, Scott RD (2005) Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am 87(3):598–603
Scuderi GR, Kochhar T (2007) Management of flexion contracture in total knee arthroplasty. J Arthroplasty 22(4 Suppl 1):20–24
Ritter MA, Lutgring JD, Davis KE, Berend ME, Pierson JL, Meneghini RM (2007) The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplasty 22(8):1092–1096
Harato K, Nagura T, Matsumoto H, Otani T, Toyama Y, Suda Y (2010) Extension limitation in standing affects weight-bearing asymmetry after unilateral total knee arthroplasty. J Arthroplasty 25(2):225–229
Casino D, Zaffagnini S, Martelli S, Lopomo N, Bignozzi S, Iacono F, Russo A, Marcacci M (2009) Intraoperative evaluation of total knee replacement: kinematic assessment with a navigation system. Knee Surg Sports Traumatol Arthrosc 17(4):369–373
Seon JK, Park SJ, Lee KB, Li G, Kozanek M, Song EK (2009) Functional comparison of total knee arthroplasty performed with and without a navigation system. Int Orthop 33(4):987–990
Luring C, Oczipka F, Perlick L, Tingart M, Grifka J, Bathis H (2009) Two year follow-up comparing computer assisted versus freehand TKR on joint stability, muscular function and patients satisfaction. Knee Surg Sports Traumatol Arthrosc 17(3):228–232
Kawamura H, Bourne RB (2001) Factors affecting range of flexion after total knee arthroplasty. J Orthop Sc 6(3):248–252
Higuchi H, Hatayama K, Shimizu M, Kobayashi A, Kobayashi T, Takagishi K (2009) Relationship between joint gap difference and range of motion in total knee arthroplasty: a prospective randomised study between different platforms. Int Orthop 33(4):997–1000
Klein GR, Restrepo C, Hozack WJ (2006) The effect of knee component design changes on range of motion evaluation in vivo by a computerized navigation system. J Arthroplasty 21(5):623–627
Lam LO, Swift S, Shakespeare D (2003) Fixed flexion deformity and flexion after knee arthroplasty. What happens in the first 12 months after surgery and can a poor outcome be predicted? Knee 10(2):181–185
Bellemans J, Vandenneucker H, Victor J, Vanlauwe J (2006) Flexion contracture in total knee arthroplasty. Clin Orthop Relat Res 452:78–82
Ferber R, Osternig L, Gravelle D (2002) Effect of PNF stretch techniques on knee flexor muscle EMG activity in older adults. J Electromyogr Kinesiol 12(5):391–397
Campbell DG, Johnson LJ, West SC (2006) Multiparameter quantitative computer-assisted tomography assessment of unicompartmental knee arthroplasties. ANZ J Surg 76(9):782–787
Kaya Bicer E, Servien E, Lustig S, Demey G, Ait Si Selmi T, Neyret P (2010) Sagittal flexion angle of the femoral component in unicompartmental knee arthroplasty: is it same for both medial and lateral UKAs? Knee Surg Sports Traumatol Arthrosc Off J ESSKA 18(7):928–933
Muller PE, Pellengahr C, Witt M, Kircher J, Refior HJ, Jansson V (2004) Influence of minimally invasive surgery on implant positioning and the functional outcome for medial unicompartmental knee arthroplasty. J Arthroplasty 19(3):296–301
Gallie PA, Davis ET, Macgroarty K, Waddell JP, Schemitsch EH (2010) Computer-assisted navigation for the assessment of fixed flexion in knee arthroplasty. Can J Surg 53(1):42–46
Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A (2003) Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br 85(6):830–835
Lustig S, Fleury C, Goy D, Neyret P, Donell ST (2011) The accuracy of acquisition of an imageless computer-assisted system and its implication for knee arthroplasty. Knee 18(1):15–20
Doro LC, Hughes RE, Miller JD, Schultz KF, Hallstrom B, Urquhart AG (2008) The reproducibility of a kinematically-derived axis of the knee versus digitized anatomical landmarks using a knee navigation system. Open Biomed Eng J 2:52–56
Aderinto J, Brenkel IJ, Chan P (2005) Natural history of fixed flexion deformity following total knee replacement: a prospective five-year study. J Bone Joint Surg Br 87(7):934–936
Harato K, Nagura T, Matsumoto H, Otani T, Toyama Y, Suda Y (2008) Knee flexion contracture will lead to mechanical overload in both limbs: a simulation study using gait analysis. Knee 15(6):467–472
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Ostrosky KM, VanSwearingen JM, Burdett RG, Gee Z (1994) A comparison of gait characteristics in young and old subjects. Phys Ther 74(7):637–644, discussion 644–636
Jung MC, Park D, Lee SJ, Lee KS, Kim DM, Kong YK (2010) The effects of knee angles on subjective discomfort ratings, heart rates, and muscle fatigue of lower extremities in static-sustaining tasks. Appl Ergon 42(1):184–192
Kawahara S, Matsuda S, Fukagawa S, Mitsuyasu H, Nakahara H, Higaki H, Shimoto T, Iwamoto Y (2012) Upsizing the femoral component increases patellofemoral contact force in total knee replacement. J Bone Joint Surg Br 94(1):56–61
Mahoney OM, Kinsey T (2010) Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am 92(5):1115–1121
Emerson RH Jr, Martinez J (2008) Men versus women: does size matter in total knee arthroplasty? Clin Orthop Relat Res 466(11):2706–2710
Seil R, Pape D (2011) Causes of failure and etiology of painful primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1418–1432
Smith CK, Chen JA, Howell SM, Hull ML (2010) An in vivo study of the effect of distal femoral resection on passive knee extension. J Arthroplasty 25(7):1137–1142
Lu H, Mow CS, Lin J (1999) Total knee arthroplasty in the presence of severe flexion contracture: a report of 37 cases. J Arthroplasty 14(7):775–780
Asano H, Muneta T, Sekiya I (2008) Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc 16(11):999–1003
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lustig, S., Scholes, C.J., Stegeman, T.J. et al. Sagittal placement of the femoral component in total knee arthroplasty predicts knee flexion contracture at one-year follow-up. International Orthopaedics (SICOT) 36, 1835–1839 (2012). https://doi.org/10.1007/s00264-012-1580-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1580-z