Abstract
The objective of this study was to investigate the range of motion (ROM) of the knee before and four years after total knee arthroplasty (TKA) with a mobile or fixed type of platform and to prospectively evaluate whether there was a difference in ligament balance between the platform types. The subjects were 68 patients involving 76 joints. The mobile type was used in 31 joints and fixed type in 45 joints by employing a prospective randomised method. The passive maximum ROM was measured using a goniometer before and four years after surgery. Also, the intraoperative knee ligament balance was measured. The postoperative extension ROM was significantly improved after TKA using a mobile bearing type compared with that employing a fixed bearing type. In TKA using the former, the intraoperative gap difference was not related to the postoperative flexion angle of the knee. However, they were related in TKA using a fixed bearing type, with a positive correlation regarding the flexion gap.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The objectives of total knee arthroplasty (TKA) are the alleviation of joint pain on standing and walking and consequent improvement in the activities of daily living (ADL), and reports of its effectiveness are numerous [3, 10, 13, 17]. However, the range of motion (ROM) of the knee is often reduced after TKA compared with the preoperative range, and this may restrict postoperative ADL. Therefore, there have been a number of reports on factors affecting the ROM of the knee after TKA. Among them, the preoperative ROM has a major effect, and patients with a good preoperative ROM have been reported to show good motion postoperatively [12]. Various other factors including the design of the prosthesis [8, 14], ratio between the patella and patellar tendon lengths [7], femoral posterior condylar offset [2, 5] and posterior cruciate ligament (PCL) stiffness [9, 18] have also been evaluated.
Recently, mobile bearing TKA, in which the platform rotates or moves anteroposteriorly, has been devised, and its clinical results are under discussion [6, 16]. The background to the introduction of this mobile type TKA arises from demands for the reduction of wear-associated debris along with the stabilisation of long-term outcomes and improvement in the flexion range of the knee [4]. However, as it has a short history of clinical application, the long-term results of this treatment, such as the frequency of loosening, remain unclear. Nor has there been a report involving a randomised comparative study between the fixed and mobile types, and the effectiveness of the mobile type is still unclear.
One of the adverse events early after mobile bearing TKA is the spinning out of the platform [11]. This condition is more likely to occur in patients with a loose balance between the varus and valgus ligaments in TKA. Appropriately balancing the varus and valgus ligaments is a basic point requiring caution in TKA, but as there is no agreed standard, it largely depends on the experience of each orthopaedic surgeon. Moreover, there has been no report in which the intraoperative ligament balance was quantitatively evaluated, and its relationship with the postoperative clinical results has not been sufficiently assessed, according to our search of the literature.
The objective of this study was to investigate the ROM of the knee before and four years after TKA with a mobile or fixed type of platform and to prospectively evaluate whether there was a difference in ligament balance, which was quantitatively evaluated during surgery, between the platform types.
Materials and methods
The study was based on a prospective randomised design. The subjects were 68 patients involving 76 joints who consented in advance. The target disease was limited to osteoarthritis of the knee, because rheumatoid arthritis often causes problems in joints other than the knee, and they were considered to affect the ROM of the knee. The patients were aged 56–81 years (mean: 68.4 years) and consisted of 19 men and 49 women. TKA was performed using the P.F.C. (DePuy Orthopaedics Inc., Warsaw, IN, USA) in all patients. Choice of the mobile or fixed type of platforms was decided preoperatively by a prospective randomised method using computer-generated random numbers. As a result, the mobile type was used in 31 joints (group M) and fixed type in 45 joints (group F). Osteotomy was performed using the independent cut method, and the PCL was conserved in all patients.
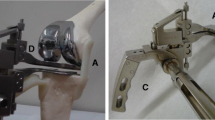
The passive maximum ROM of the knee was measured using a goniometer before and one and four years after surgery. The intraoperative knee ligament balance was measured according to previous reports [1, 15]. The joint gap (GAP) with the patella reversed was measured with a knee extension of 0˚ and flexion of 90˚ using a knee balancer (DePuy Orthopaedics Inc., Warsaw, IN, USA) (Fig. 1). A joint distraction force of 80 N was applied, and the GAP was measured in the spaces at the osteotomy sites on the medial and lateral sides of the joint. The GAP at 90˚ flexion minus the GAP at 0˚ extension was calculated as the GAP difference.
A nonparametric method, the Mann-Whitney U test, was used to calculate statistical differences between unpaired groups. The two-tailed Student’s t test was used for comparisons within and between the groups, and Pearson’s correlation coefficients were calculated. All statistical procedures were performed using StatView software. The level of significance was <0.05.
Results
The ROM of the knee improved in extension after TKA. It improved from a preoperative mean of −11.7 ± 15.2˚ to a postoperative mean of 0.3 ± 3.2˚ in group M at one year postoperatively. In group F, the extension angle also improved significantly one year after surgery. In both groups, the ROM of the knee did not change at four years after TKA. The improvement in the extension range was particularly notable in group M and was significantly greater than in group F. However, the postoperative flexion angle showed no improvement compared with the preoperative level in groups M or F (Table 1).
Concerning the relationship between the GAP difference and flexion range, no significant correlation was observed in group M at one year postoperatively. As shown in Fig. 2, the correlation coefficient between the medial GAP difference and change in the flexion angle between before and after surgery was 0.23, showing no correlation. That between the lateral GAP difference and change in the flexion angle between before and after surgery was 0.21, also revealing no correlation (Fig. 3). Also, there was no correlation between the GAP difference and flexion range at four years postoperatively.
In group F, however, a positive correlation was observed between the medial GAP difference and change in the flexion angle with a correlation coefficient of 0.51 at one year postoperatively. This indicates that the postoperative knee flexion angle tends to increase compared with the preoperative angle in patients with a large medial GAP difference (Fig. 4). The correlation coefficient between the lateral GAP difference and change in the flexion angle was 0.54, indicating an even closer correlation (Fig. 5). Also, a significant correlation was found between the GAP difference and flexion range at four years postoperatively.
Discussion
Various factors that may affect the ROM of the knee after TKA including the preoperative ROM of the knee [12], a high patellar position (Insall-Salvati ratio) [7], intraoperative ligament balance [18], femoral posterior condylar offset [2, 5] and PCL stiffness [9] have been evaluated. This study showed that mobile bearing TKA does not significantly contribute to an improvement in the postoperative knee flexion range. However, the extension range improved significantly after mobile bearing TKA compared with the preoperative extension range, maintained four years postoperatively. In addition, the improvement in the extension range was more notable after mobile bearing than after fixed bearing TKA. The patients were followed up for four years after surgery, and whether these results persist for longer is unclear. However, mobile bearing TKA appears to be a recommendable option to facilitate consistent improvements in the postoperative ROM.
Dislocation of the bearing has been reported as an adverse event after mobile bearing TKA. Ridgeway et al. described 25 cases of early bearing dislocation and reported joint instability during TKA as its cause [11]. In our study, the improvement in the knee flexion angle after mobile bearing TKA was not correlated with the intraoperative ligament balance at one to four years postoperatively. This suggests that manipulations to improve the postoperative flexion range such as increasing the flexion gap are unnecessary in mobile bearing TKA. Instead, spin out may be prevented by placing the bearing so as to equalise the extension and flexion gaps and control joint instability. In contrast, no dislocation of the bearing occurs in fixed bearing TKA. The postoperative flexion range may be increased by setting a slightly wider flexion gap. However, follow-up studies are necessary to evaluate the effects of this manipulation on the postoperative wear of polyethylene and long-term joint stability.
The following conclusion was derived from the results of this prospective study of TKA using a mobile or fixed bearing type. The postoperative extension angle of the knee was significantly improved after TKA using a mobile bearing type compared with that employing a fixed bearing type. In mobile bearing TKA, the intraoperative gap difference was not related to the postoperative flexion angle of the knee. However, they were related in TKA using a fixed bearing type, with a positive correlation regarding the flexion gap.
References
Baldini A, Scuderi GR, Aglietti P, Chalnick D, Insall JN (2004) Flexion-extension gap changes during total knee arthroplasty: effect of posterior cruciate ligament and posterior osteophytes removal. J Knee Surg 17:69–72
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84:50–53
Dennis DA, Clayton ML, O’Donnel S, Mack RP, Stringer EA (1992) Posterior cruciate condylar total knee arthroplasty. Average 11-year follow-up evaluation. Clin Orthop 281:168–176
Dennis DA, Komistek RD (2006) Mobile-bearing total knee arthroplasty: design factors in minimizing wear. Clin Orthop 452:70–77
Hanratty BM, Thompson NW, Wilson RK, Beverland DE (2007) The influence of posterior condylar offset on knee flexion after total knee replacement using a cruciate-sacrificing mobile-bearing implant. J Bone Joint Surg Br 89:915–918
Lädermann A, Lübbeke A, Stern R, Riand N, Fritschy D (2008) Fixed-bearing versus mobile-bearing total knee arthroplasty: a prospective randomised, clinical and radiological study with mid-term results at 7 years. Knee 15:206–210
Meneghini RM, Ritter MA, Pierson JL, Meding JB, Berend ME, Faris PM (2006) The effect of the Insall-Salvati ratio on outcome after total knee arthroplasty. J Arthroplasty 21:116–120
Nicholls RL, Schirm AC, Jeffcote BO, Kuster MS (2007) Tibiofemoral force following total knee arthroplasty: comparison of four prosthesis designs in vitro. J Orthop Res 25:1506–1512
Parsley BS, Conditt MA, Bertolusso R, Noble PC (2006) Posterior cruciate ligament substitution is not essential for excellent postoperative outcomes in total knee arthroplasty. J Arthroplasty 21:127–131
Rand JA, Ilstrup DM (1991) Survivorship analysis of total knee arthroplasty. Cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am 73:397–409
Ridgeway S, Moskal JT (2004) Early instability with mobile-bearing total knee arthroplasty: a series of 25 cases. J Arthroplasty 19:686–693
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 85-A:1278–1285
Schai PA, Thornhill TS, Scott RD (1998) Total knee arthroplasty with the PFC system. Results at a minimum of ten years and survivorship analysis. J Bone Joint Surg Br 80-B:850–858
Sharma A, Komistek RD, Scuderi GR, Cates HE Jr (2007) High-flexion TKA designs: what are their in vivo contact mechanics? Clin Orthop 464:117–126
Wallace AL, Harris ML, Walsh WR, Bruce WJ (1998) Intraoperative assessment of tibiofemoral contact stresses in total knee arthroplasty. J Arthroplasty 13:923–927
Watanabe T, Tomita T, Fujii M, Hashimoto J, Sugamoto K, Yoshikawa H (2005) Comparison between mobile-bearing and fixed-bearing knees in bilateral total knee replacements. Int Orthop 29:179–181
Whiteside LA (1994) Cementless total knee replacement. Nine- to 11-year results and 10-year survivorship analysis. Clin Orthop 309:185–192
Wyss T, Schuster AJ, Christen B, Wehrli U (2008) Tension controlled ligament balanced total knee arthroplasty: 5-year results of a soft tissue orientated surgical technique. Arch Orthop Trauma Surg 128:129–135
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Higuchi, H., Hatayama, K., Shimizu, M. et al. Relationship between joint gap difference and range of motion in total knee arthroplasty: a prospective randomised study between different platforms. International Orthopaedics (SICOT) 33, 997–1000 (2009). https://doi.org/10.1007/s00264-009-0772-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-009-0772-7