Abstract
Purpose
The range of motion achieved after a total knee arthroplasty (TKA) affects many daily activities and overall patients’ satisfaction. This study aims to define the determinants affecting post-operative midterm active flexion according to a specific cruciate-sacrificing prosthesis, the rotating concave–convex (ROCC®) TKA.
Method
Four hundred and eighty-four consecutive patients (584 TKAs) were prospectively followed. After baseline patient demographics and anatomical characteristics, clinical and radiological post-operative assessments were periodically recorded. The rotational alignment of the femoral component was additionally reported for 120 patients. Eligibility for final inclusion was a minimum of 5-year follow-up. Univariate analyses followed by a multivariate model were fitted to determine the independent predictors of midterm active knee flexion.
Results
Thirty-four TKA (5.8 %) were excluded for a secondary surgery before their 50 years, 69 patients died (11.8 %), and 21 (3.6 %) were lost to follow-up. Overall, 460 TKAs were included. The post-operative mean knee flexion angle was measured at 127.7° ± 9.3°. Significant factors affecting final flexion under univariate analyses were the patient height and body mass index, the absence of previous surgery, a depressive state, the preoperative flexion angle, a preoperative flexion contracture, a patellar residual subluxation, the reconstructed patellar height, and the rotation of the femoral component. The multivariate model confirmed the patient’s height, a depression, the preoperative flexion angle, a patellar residual subluxation, and the patellar height as statistically significant determinants.
Conclusion
Aside from the preoperative flexion angle, numerous predictors of flexion, both patient- and procedure-related were identified. Surgeons should take these into account both when adequately informing their patient before surgery and when performing the arthroplasty itself.
Level of evidence
Prognostic, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain relief and improved walking ability are primary objectives of total knee arthroplasty (TKA) [28]. Range of motion (ROM) is another capital post-operative target, as it influences many activities. A minimum range of knee flexion of 90° is essential to daily activities with about 67° required in swing phase, 83° in climbing stairs, 90° in descending stairs, and 93° in rising from a chair [21]. While surgeons can be confident that TKA can relieve pain, the relationship between surgery and an improved ROM is less consistently established. Numerous factors, including patient anatomy, preoperative functional status, surgical techniques, or implant designs have been in this regard investigated [20]. Among these factors, the Preoperative Active Flexion (PreAF) has been strongly and repeatedly correlated with the Postoperative Active Flexion (PostAF) [13, 18, 19]. The implication of factors such as age, weight, body mass index (BMI), Knee Society Score, and type of disease have also been reported with less robustness [19, 27]. The surgical technique and the post-operative rehabilitation protocol are likewise presumed to affect the final knee ROM [1, 25]. Each design of TKA implant has its own characteristics that may also influence the ROM. Identifying the determinants of flexion associated with each specific TKA design is therefore crucial to help surgeons in optimizing their chances to reach a satisfactory functional result.
Recently, midterm functional and survivorships results of the rotating concave–convex ®(ROCC) TKA (Biomet, Valence, France) have been published [3], yet focusing on the type of fixation. The design of this original cruciate-sacrificing implant with rotating platform is compatible with a high posterior condylar offset [2] that is meant to allow flexing kinematics closed to a physiological situation. No study has analysed yet by way of strong statistical models all the determinants of flexion according to this specific TKA implant. The aim of this study was to investigate predictors affecting post-operative midterm active flexion using the ROCC knee prosthesis.
Materials and methods
Four hundred and eighty-four consecutive patients (584 knees) receiving a ROCC between January 2001 and January 2008 were eligible for this study. Inclusion criteria were primary and secondary (rheumatoid arthritis, necrosis, trauma) knee osteoarthritis. Revisions were excluded. Baseline recorded characteristics of patients were past medical history (including a “depression” criterion, as diagnosed by the general practitioner, either based on a “mild depression” cut-off from the second version of the Beck Depression Inventory or for receiving antidepressants or anxiolytics for that purpose), physical exam, and functional impairment references.
All operative procedures were performed by one surgeon (MB), using a medial parapatellar approach (537 knees), except when a lateral approach had been previously used (47 knees), in order to reduce skin necrosis risks. No tourniquet was used. The technique consisted in both tibial and femoral measured resections perpendicular to the mechanical axis, avoiding overcorrection while closely restoring both the tibio- and patellofemoral joint lines. Collateral ligaments were carefully balanced, then rotation of the femoral component was defined parallel to the trans-epicondylar axis. Hydroxyapatite-coated femoral components were cementless press fitted whenever the primary stability was sufficient (560 knees), considering no macroscopic motion under a vigorous manipulation of the knee. A randomization designated either an HA-coated (286 knees) or a cemented tibial component (298 knees), as defined for a contemporary study. The decision to resurface the patella was based on the severity of patellofemoral symptoms [11]. It was resurfaced for 415 knees, using an anatomical rotating HA-coated component. Patellar tracking was assessed by the operator during surgery with the no thumb technique [8, 10]. Tracking was binary graded as optimal or not (defined by a lateral residual subluxation, after having received all the appropriate corrections including a lateral release). Post-operative care included daily 40 mg of enoxaparin until day 30, and painkillers represented by an immediate wound infiltration with 300 cc ropivacaine 0.2 %, in addition to ketoprofen 300 mg/day, tramadol 300 mg/day and paracetamol 3 g/day. Full weight bearing was allowed from the day of operation. Rehabilitation involved accelerated active and passive knee flexion exercises and muscle strengthening.
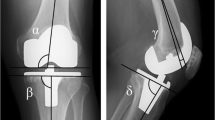
The ROCC implant is a mobile bearing TKA sacrificing the cruciate ligaments. Both the superior bearing surface and the inferior femoral surface are saddle-shaped hyperbolic paraboloids. The saddle-shaped insert fits the corresponding symmetrical intercondylar part of the femoral component, which is likewise concave–convex and spiral shaped in the sagittal plane and displays a 0.48 femoral offset (condyle/shaft ratio) in order to enhance flexion [2]. This “rider-in-saddle” socket ensures mediolateral and anteroposterior stability. A deep anatomical trochlea restores accurately the patellofemoral joint line position allowing optimal patellar tracking at every degree of flexion.
Clinical and radiological reviews were scheduled after surgery at 6 weeks, 6 months, first year, and then every 2 years. Clinical assessments included the Knee Society Score [16], the range of motion according to a manual goniometer, a dedicated 4-level Likert scale pain evaluation, focused on the whole knee but also specifically on patellar impairment (anterior pain, increasing during prolonged sitting, stairs climbing or descending, and rising from a chair) [30]. Radiological assessments based on pre- and post-operative frontal, sagittal and long-leg standing films were performed by two trained observers. The inter-observer reliability had been preliminary tested, based on 30 random measurements, allowing to calculate an intraclass correlation coefficient equal to 0.97. Patellar height was measured according to the description by Caton [7]. We additionally planned pre- and post-operative CT scans for the last 120 patients, in order to evaluate preoperatively the posterior condylar angle (between the trans-epicondylar axis and the posterior condylar line) [29] and post-operatively the rotation of the femoral component [29]. An ethical approval was delivered by the local institutional review board, the trial was registered at clinicaltrial.gov (registration number NCT02127619), and all participants gave their informed consent.
Statistical analysis
Data were entered into a database (SPSS version 19, IBM, Armonk, NJ, USA). Data were presented as mean and standard deviation for normal or median and range for non-normal distribution of variables for quantitative variables. Qualitative variables were described using number and percentage. Preoperative (demographic, clinical, and radiological), intraoperative, or immediate post-operative factors were analysed using an univariate linear mixed model taking into account correlation within subject (a patient can have a surgery of both knees). The linear mixed model was fitted to analyse the predictors that may influence post-operative active knee flexion. The predictor variables for investigation were chosen from a study of the literature. They included age, gender, height, weight, BMI, diagnosis, previous conservative surgery, functional preoperative status, and physical preoperative examination, in addition to numerous anatomical features pre- and post-operatively. Complete multivariate model included significant variable in univariate analysis (P value ≤0.05), except the rotational alignment of the femoral component, as only 120 patients had available data related to this parameter. We selected the model with the smallest Akaike information criterion. A level of P < 0.05 was considered statistically significant. Analysis are performed using R software (R Foundation for Statistical Computing, Paris, France), version 2.15.2.
Results
Patient characteristics and follow-up
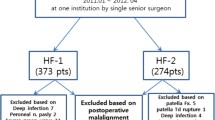
The mean age at surgery was 70.4 ± 8.7 years at the time of the surgery, including 199 men and 385 women. Preoperatively, mean active flexion was 119.4° ± 15.4°. Further baseline characteristics, clinical and functional data are displayed in Table 1. At a minimum 5 years after index surgery, 21 patients (21 knees, 3.6 %) were lost to follow-up and 69 patients (69 knees, 11.8 %) died for reasons unrelated to the replaced knee (Fig. 1). In addition, 34 knees were excluded from the analysis, as they received a second surgery before the fifth year: (1) 22 knees underwent secondary procedure without component revision (for fracture fixation, debridement for early sepsis, release for stiffness, or secondary patellar resurfacing) and (2) 12 knees underwent component revision (for late sepsis, destabilizing fracture, early fixation failure, or aseptic loosening). Thus, a total of 460 knees were available for final analysis (Fig. 1).
Surgical procedure
Overall, the surgical procedure improved the active flexion (mean 127.6° ± 9.3° at the latest follow-up, P < 0.001 compared to baseline) and the frontal knee alignment (from 21.0 to 89.6 % of “acceptable” frontal knee alignments between 178° and 182°, P < 0.001). The posterior condylar offset (post-operative–preoperative) was calculated to be 2.8 ± 4.3 mm. Further anatomical and surgical procedure details are presented in Table 2.
Linear mixed model
The univariate analyses showed no significant correlation between age, gender, weight, primary diagnosis, or patellar resurfacing with PostAF (Table 3). However, height (coefficient 0.2 ± 0.06, P < 0.0001), BMI (−0.3 ± 0.09, P < 0.0001), and the absence of previous conservative knee surgery (2.2 ± 1.1, P = 0.05) had a statistically significant association with PostAF. Depression was also found to be significantly correlated with PostAF (coefficient −4.4 ± 1.2, P < 0.0001). Among the remaining significant analyses, the parameters statistically correlated with PostAF were: the PreAF (0.2 ± 0.03, P < 0.0001), the post-operative patellar height (−6.7 ± 3.1, P = 0.04), a non-optimal patellar tracking as evaluated during surgery (−7.0 ± 1.6, P < 0.0001), and the rotational alignment of the femoral component (1.0 ± 0.3, P = 0.01). Significances were confirmed for all but two factors (history of previous surgery, preoperative contracture) after multivariate analysis (Table 3). The 120 records of rotational alignment from CT scan were not included in this multivariate step.
Discussion
The most important finding of the present study was that numerous key parameters, including patient- (height, depression, overweight, and history of knee surgery) and procedure-related (patellar tracking, patellar height, and femoral component rotation) factors have a direct influence on the final knee flexion after TKA using the ROCC implants.
We acknowledge our study had few limitations. First, a single type of TKA implant was analysed, and its use by an experienced surgeon, which participated to its design conception. Second, the surgical technique was not modified during the study period, and did not permit us to record any operative ligament balancing parameter. Our findings have consequently to be confronted to external experiences from varied centres before being definitively validated. Third, we had to deplore 3.6 % of patients lost after a minimum of 5 years of follow-up. However, as no pre-clinical mechanical testing related to the ROCC® knee implant had been published to date, this study represents one of the first picture of its clinical performance, through a prospective collection of data from a large cohort of patients, allowing solid statistical analyses.
There is no strong agreement between authors assessing factors that influence final flexion after TKA. The type of knee disease has been described by Harvey et al. [15] as the most important factor in predicting the final ROM. According to Harvey et al. [15], the final flexion angle would be greater in primary osteoarthritis, while patients with rheumatoid arthritis would have a better gain in ROM [19]. Our study is not consistent with these findings related to the influence of diagnosis. Again disagreeing with previous studies [19, 27], we found a correlation between BMI and final flexion. This might be due to soft tissue impingement between the femur and the tibia, which restricts flexion of the knee, as supported by several studies [1, 12, 22]. In addition, to our knowledge, our study is one of the first demonstrating a statistical correlation between patient height and PostAF. Our hypothesis is that a larger virgin anatomy offers less risk of oversizing the implants and high chances of low reconstructed posterior condylar offset. However, the coefficient is minimal (0.17), indicating that the actual influence is far from major. Besides, confirming previous reports, our results demonstrate no correlation between gender [15, 17, 19, 27], age [1, 27], and final flexion. Concerning depression and flexion angle, we have to acknowledge that our diagnosis criteria were large and somehow inaccurate. However, our results were perfectly consistent with Edwards et al. [9], using a validated scale [24], who confirmed depression status as a strong predictor of final flexion. While several authors argued that activity scores [1, 19, 25, 27] were the most important factors to predict final motion, our study did not demonstrate their usefulness with the ROCC prosthesis.
With little exceptions [26], increased preoperative flexion angle has previously proved [15, 27] to determine a greater post-operative flexion achieved by the patients. This statement was validated by our findings. Conclusions related to the correlation between patellar parameters and flexion are more inconsistent. Myles et al. [23] and Bindelglass et al. [4] reported no relationship among patellar maltracking and pain, flexion, or poor score result. Sancheti et al. [27] similarly found that patella resurfacing has no effect on the post-operative ROM, in agreement with Burnett et al. [6]. Their sample size might have been insufficient to reach a definitive conclusion. Operative tracking, just as post-operative patellar height, were proved to be patellar predictors to consider for a better flexion. In accordance to the capital importance of a well-“balanced” extensor mechanism, we found that the femoral component rotation was correlated with final flexion angle. This finding is in accordance with Boldt et al. publication [5], supporting the negative influence of internal femoral rotation on the definitive range of motion. As opposed to Geijsen et al. [14], no correlation was found in our study between the posterior condylar offset and knee flexion. Overall, this study suggests that a critical attention should be given to restore a satisfying femoropatellar joint in order to optimize the final flexion.
Conclusion
In conclusion, the use of the ROCC® knee prosthesis in our hands provided with final highly satisfactory range of motion of for an active daily living at a minimum of 5-year follow-up. Factors that affected final active knee flexion were demonstrated to be patient’s height, BMI, a history of knee surgery, depressive state, but also the preoperative knee flexion angle, operative patellar tracking, post-operative patellar height, and rotation of the femoral component. Surgeons should take into account these factors both before surgery when informing their patients of the potential results and during surgery in order to optimize the chances to get a satisfactory range of motion.
References
Anouchi YS, McShane M, Kelly F Jr, Elting J, Stiehl J (1996) Range of motion in total knee replacement. Clin Orthop Relat Res 331:87–92
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 1:50–53
Bercovy M, Beldame J, Lefebvre B, Duron A (2012) A prospective clinical and radiological study comparing hydroxyapatite-coated with cemented tibial components in total knee replacement. J Bone Joint Surg Br 94(4):497–503
Bindelglass DF, Cohen JL, Dorr LD (1993) Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop Relat Res 286:103–109
Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U (2006) Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty. Int Orthop 30(5):420–425
Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL (2007) A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res 464:65–72
Caton J (1989) Method of measuring the height of the patella. Acta Orthop Belg 55:385–386 French
Cho WS, Woo JH, Park HY, Youm YS, Kim BK (2011) Should the ‘no thumb technique’ be the golden standard for evaluating patellar tracking in total knee arthroplasty? Knee 18(3):177–179
Edwards RR, Haythornthwaite JA, Smith MT, Klick B, Katz JN (2009) Catastrophizing and depressive symptoms as prospective predictors of outcomes following total knee replacement. Pain Res Manag 14(4):307–311
Ewald FC (1991) Leg lift technique for simultaneous femoral, tibial and patella prosthetic cementing, rule of “no thumb” for patella tracking and “steel rod rule” for ligament tension. Tech Orthop 6(4):44–46
Feller JA, Bartlett RJ, Lang DM (1996) Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br 78-B:226–228
Franklin PD, Li W, Ayers DC (2008) The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res 466:2597–2604
Gatha NM, Clarke HD, Fuchs R, Scuderi GR, Insall JN (2004) Factors affecting postoperative range of motion after total knee arthroplasty. J Knee Surg 17:196–202
Geijsen GJ, Heesterbeek PJ, van Stralen G, Anderson PG, Wymenga AB (2014) Do tibiofemoral contact point and posterior condylar offset influence outcome and range of motion in a mobile-bearing total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 22(3):550–555
Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br 75:950–955
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Ishii Y, Matsuda Y, Sakata S, Onda N, Omori G (2005) Primary total knee arthroplasty using the Genesis I total knee prosthesis: a 5- to 10-year followup study. Knee 12:341–345
Kawamura H, Bourne RB (2001) Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci 6:248–252
Kotani A, Yonekura A, Bourne RB (2005) Factors affecting range of motion after contemporary total knee arthroplasty. J Arthroplasty 7:850–856
Kurosaka M, Yoshiya S, Mizuno K, Yamamoto T (2002) Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplasty 17(4 Suppl 1):59–62
Laubenthal KN, Smidt GL, Kettelkamp DB (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34–43
Long WJ, Scuderi GR (2008) High-flexion total knee arthroplasty. J Arthroplasty 23:6–10
Myles CM, Rowe PJ, Nutton RW, Burnett R (2006) The effect of patella resurfacing in total knee arthroplasty on functional range of movement measured by flexible electrogoniometry. Clin Biomech (Bristol, Avon) 21(7):733–739
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 85(7):1278–1285
Russell RD, Huo MH, de Jong L, Jones RE (2014) Preoperative flexion does not influence postoperative flexion after rotating-platform total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(7):1644–1648
Sancheti KH, Sancheti PK, Shyam AK, Joshi R, Patil K, Jain A (2013) Factors affecting range of motion in total knee arthroplasty using high flexion prosthesis: a prospective study. Indian J Orthop 47(1):50–56
Thomsen MG, Husted H, Otte KS, Holm G, Troelsen A (2013) Do patients care about higher flexion in total knee arthroplasty? A randomized, controlled, double-blinded trial. BMC Musculoskelet Disord 14:127
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95(5):365–372
Wevers ME, Lowe NK (1990) A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 13:227–236
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Langlois, J., Charles-Nelson, A., Katsahian, S. et al. Predictors of flexion using the rotating concave–convex total knee arthroplasty: preoperative range of motion is not the only determinant. Knee Surg Sports Traumatol Arthrosc 23, 1734–1740 (2015). https://doi.org/10.1007/s00167-014-3479-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3479-2