Abstract
Purpose
This study assessed the prognostic value of pre-operative 2-[18F] fluoro-2-deoxy-D-glucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) volumetric parameters, including metabolic tumor volume (MTV) and total lesion glycolysis (TLG), in patients with epithelial ovarian cancer.
Methods
A total of 175 patients with epithelial ovarian cancer who underwent 18 F-FDG PET/CT and subsequent cytoreductive surgery were retrospectively enrolled. Maximum standardized uptake value (SUVmax) on 18F-FDG PET/CT was measured for all patients. Because nine patients showed low tumor-to-background uptake ratios, MTV and TLG were measured in 166 patients. Univariate and multivariate analyses were performed to evaluate the prognostic significance of SUVmax, MTV, TLG, and clinicopathological factors for disease progression-free survival.
Results
Disease progressed in 78 (44.6 %) of the 175 patients, and the 2-year disease progression-free survival rate was 57.5 %. Univariate analysis showed that tumor stage, histopathological type, presence of regional lymph node metastasis, residual tumor after cytoreductive surgery, pre-operative serum carbohydrate antigen 125 (CA125) level, SUVmax, MTV, and TLG were significant prognostic factors (p < 0.05). Among these variables, tumor stage (p = 0.0006) and TLG (p = 0.008) independently correlated with disease progression-free survival on multivariate analysis. The disease progression rate was only 2.3 % in stage I-II patients with low TLG (≤100.0), compared to 80.0 % in stage III-IV patients with high TLG (>100.0).
Conclusion
Along with tumor stage, TLG is an independent prognostic factor for disease progression after cytoreductive surgery in patients with epithelial ovarian cancer. By combining tumor stage and TLG, one can further stratify the risk of disease progression for patients undergoing cytoreductive surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is the eighth most common malignancy among women and has the highest mortality rate of any gynecologic malignancy [1]. Epithelial ovarian cancers are the most common ovarian cancers and the majority of patients with epithelial ovarian cancers are diagnosed at an advanced stage [2]. Although cytoreductive surgery along with platinum and paclitaxel combination chemotherapy has improved outcomes, the prognosis of patients with epithelial ovarian cancer is still poor, with a 5-year overall survival rate less than 50 % [2, 3]. Identifying the prognostic factors for epithelial ovarian cancer is important to predict outcomes and allow the planning of the most appropriate treatment. Several factors including age, International Federation of Obstetrics and Gynecology (FIGO) stage, histopathological type, tumor grade, residual tumor after primary cytoreductive surgery, adjuvant chemotherapy, regional lymph node metastases, and serum carbohydrate antigen 125 (CA125) level have been shown to have significant predictive value [4–9].
Currently, 2-[18F] fluoro-2-deoxy-D-glucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) has been widely used in various malignant tumor types. In patients with epithelial ovarian cancer, 18F-FDG PET/CT is useful in diagnosing, staging, detecting recurrent lesions, and monitoring treatment response [10–14]. Furthermore, the degree of 18F-FDG uptake of ovarian cancer lesions, expressed as the maximum standardized uptake value (SUVmax), was found to be a significant parameter for predicting clinical outcome [15–18]. In addition to SUVmax, recent studies have demonstrated that other 18F-FDG PET/CT-based volumetric parameters such as metabolic tumor volume (MTV) and total lesion glycolysis (TLG) are also significant prognostic factors in various cancers [19–22]. However, there are few studies that have evaluated MTV and TLG as prognostic factors in epithelial ovarian cancer [23, 24]. In this study, we assessed the prognostic value of volumetric parameters on pre-operative 18F-FDG PET/CT and compare their predictive values with those of other conventional prognostic factors in patients with epithelial ovarian cancer.
Materials and methods
Patients
This retrospective study was approved by the institutional review board of our medical center, and the need for written informed consent was waived. The electronic medical records of patients with newly diagnosed epithelial ovarian cancer who underwent pre-operative 18F-FDG PET/CT and subsequent surgical staging between January 2008 and June 2012 were retrospectively reviewed, and a total of 191 patients were enrolled in the study. Patients were excluded from the study if they (1) had previous history of another malignancy, (2) received any kind of neoadjuvant treatment prior to surgery, (3) were lost to follow-up, or (4) were diagnosed with multiple primary gynecologic cancers on surgical staging. The mean interval between pre-operative 18F-FDG PET/CT imaging and cytoreductive surgery was 5.8 ± 4.5 days (median, 5.0 days). All enrolled patients also underwent conventional radiologic imaging with contrast-enhanced CT and/or magnetic resonance imaging (MRI). Furthermore, serum CA125 levels were measured prior to surgery.
All enrolled patients underwent an FIGO staging operation consisting of bilateral salpingo-oophorectomy, hysterectomy, lymphadenectomy, omentectomy, and maximal tumor reduction [2]. Moreover, biopsies were performed for all suspicious sites such as the mesentery, liver, diaphragm, pelvis, and para-aortic lymph nodes. A stage was assigned based on the operative findings and histopathological results according to the FIGO staging system for ovarian cancer [2]. Patients received platinum-based adjuvant chemotherapy after operation if indicated by their FIGO stage, and if their clinical condition permitted. All patients underwent clinical follow-up that included diagnostic imaging studies and blood tests after cytoreductive surgery. The mean duration of clinical follow-up was 31.8 ± 16.3 months (median, 30.7 months). During follow-up, clinical assessment was performed every 2–3 months, and blood tests, including serum CA125 level and imaging studies such as contrast-enhanced CT scan were performed every 6–8 months. In addition, follow-up18F-FDG PET/CT were performed in patients with advanced stage or high risk of recurrence. If the clinical assessment or studies performed during follow-up showed an abnormal finding, additional diagnostic studies and/or histopathological confirmation were performed to assess cancer recurrence or disease progression.
18F-FDG PET/CT
All 18F-FDG PET/CT scans were performed using a dedicated PET/CT scanner (Discovery STe, GE Healthcare; or Biograph TruePoint 40, Siemens Healthcare). All patients fasted for at least 6 h prior to the PET/CT imaging. PET/CT images were acquired 60 min after intravenous injection of approximately 5.5 MBq/kg 18F-FDG. First, a CT scan was performed at 30 mA and 130 kVp with the Discovery STe scanner, or at 36 mA and 120 kVp with the Biograph TruePoint scanner, without contrast-enhancement. Afterwards, a PET scan was performed extending from the skull base to the proximal thighs with an acquisition time of 3 min per bed position in 3D mode. PET images were reconstructed using ordered subset expectation maximization (OSEM) with attenuation correction.
The analysis of 18F-FDG PET/CT images was performed using an Advantage Workstation 4.4 (GE Medical Systems). First, SUVmax for each patient was calculated by placing a spheroid-shaped volume of interest (VOI) at the primary tumor lesion and metastatic lesions. The SUV was calculated as (decay-corrected activity [kBq] per milliliter of tissue volume)/(injected 18F-FDG activity [kBq] per gram of body mass). Afterwards, MTV and mean SUV of the primary tumor and metastatic lesions were measured as follows [20]; first, an elliptical VOI was drawn fully encasing the primary ovarian lesion and all metastatic lesions in the transaxial, sagittal, and coronal PET/CT images. Secondly, the boundaries of voxels, the SUV of which exceeded a threshold of 40 % of SUVmax, were automatically produced. The 40 % SUVmax threshold was shown to best fit the actual volume of simulating phantom lesions in previous studies [25, 26]. Thirdly, the voxels of normal organs such as heart, liver, kidneys, ureters, and bladder, as well as false-positive lesions such as inflammatory lesions or other benign lesions were manually subtracted. Finally, MTV and mean SUV of all primary tumors and metastatic lesions were measured. TLG was calculated as (MTV) × (mean SUV).
Statistical analysis
After surgery, the patients were classified into two groups; (i) the recurrence group included patients who had either newly developed tumors or progression of residual tumors on follow-up, and (ii) the no recurrence group included patients with no evidence of cancer recurrence or progression of residual disease on follow-up. Clinicopathological factors, SUVmax, MTV, and TLG were compared between the two groups using the Student’s t test and the chi-squared test. The mean values of SUVmax in tumors of different histopathological types were compared using the Kruskal-Wallis test. Kaplan-Meier survival analysis with a log-rank test was performed to calculate cumulative disease progression-free survival rates according to clinicopathological factors, SUVmax, MTV, and TLG. Events in the analysis of disease progression-free survival included the occurrence of new cancer lesions or progression of residual lesions. Progression-free survival time was defined as the time from surgical staging to the date of event detection or to the date of the last clinical follow-up. For statistical analyses, continuous variables, including age, serum CA125 level, SUVmax, MTV, and TLG, were grouped into two categories according to specific cutoff values. The optimal cutoff values were determined by using receiver-operating characteristic (ROC) curve analysis. The significance of the predictive values of tumor factors, SUVmax, MTV, and TLG was evaluated using the log-rank test on univariate analysis. Variables that were statistically significant on univariateanalysis were selected for multivariate analysis using the Cox proportional hazards regression test. To evaluate multi-colinearity between MTV and TLG, Spearman’s rank correlation coefficient was calculated before multivariate analysis. Moreover, the Mann–Whitney test and chi-squared test were performed to compare 18F-FDG PET/CT parameters between patients with residual cancer and without residual cancer after surgery. Statistical analyses were performed using SPSS 20.0 for Windows (SPSS Inc.), and p-values of less than 0.05 were considered statistically significant.
Results
Patient characteristics
SUVmax, MTV and TLG could not be calculated in 16 of the 191 patients because of computational or technical problems. 18F-FDG PET/CT images from the remaining patients were amenable for analysis, and finally 175 patients were enrolled in the study. MTV and TLG could not be measured in nine patients among 175 patients (mucinous carcinoma, four; serous carcinoma, three; clear cell carcinoma, one; endometrioid carcinoma, one) because of low tumor-to-background uptake ratios. Statistical analysis for MTV and TLG was performed in the remaining 166 patients. Among these nine patients, none showed a recurrence event during clinical follow-up.
The characteristics of the 175 enrolled patients are shown in Table 1. During clinical follow-up, cancer recurrence or progression of residual lesions were found in 78 patients (44.6 %). The 2-year disease progression-free survival rate was 57.5 %, and the median progression-free survival time was 30.3 months. Of the 175 patients, 166 (94.9 %) received adjuvant treatment after cytoreductive surgery. The mean values of SUVmax of serous, endometrioid, clear cell, mucinous, and mixed-type carcinomas were 10.3 ± 3.7, 12.1 ± 6.6, 8.8 ± 8.2, 6.1 ± 3.5, and 14.2 ± 7.7, respectively (p < 0.0001 for Kruskal-Wallis test). Serous and endometrioid carcinomas showed significantly higher SUVmax than mucinous carcinoma (p = 0.0004 for serous carcinoma and p = 0.002 for endometrioid carcinoma). The SUVmax, M,TV and TLG in patients with stage III and IV (11.0 ± 3.7, 54.0 ± 63.0 cm3, and 422.4 ± 514.5 g, respectively) were significantly higher than those in patients with stage I and II (8.4 ± 6.2, 19.1 ± 23.3 cm3, and 115.3 ± 139.6 g, respectively; p = 0.002 for SUVmax and p < 0.0001 for both MTV and TLG). Of the 175 patients, pre-operative 18F-FDG PET/CT detected extra-abdominal metastasis in eight patients (4.6 %) and retroperitoneal and/or abdominal lymph node metastasis in nine patients (5.1 %), which were not found on other diagnostic imaging modalities.
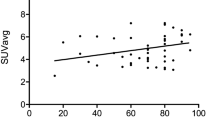
Comparison between the recurrence and no recurrence groups showed significant differences in age, histopathological type, FIGO stage, tumor grade, the presence of regional lymph node metastasis, residual tumor after cytoreductive surgery, pre-operative serum CA125 level, MTV, and TLG (p < 0.05; Table 1). The MTV and TLG in the recurrence group (Fig. 1) were significantly higher than those in the no recurrence group (p < 0.05); however, borderline significance was shown in SUVmax between the two groups (p = 0.06). The distributions of SUVmax, MTV, and TLG in the recurrence and no recurrence groups are shown in Fig. 2.
The maximum intensity projection (a) and transaxial fused (b) 18 F-FDG PET/CT images and contrast-enhanced CT image (c) of a 56-year-old woman with serous carcinoma. Intensely increased 18 F-FD uptake is shown in the right ovarian mass lesion and metastatic lesions of the pelvic cavity with maximum SUV of 6.0. MTV and TLG of primary cancer and metastatic lesions were 38.3 cm3 and 172.1 g, respectively. The patient underwent cytoreductive surgery and was surgically staged at stage III. The cancer was recurred 14 months after the surgery
Prognostic factors
Age, histopathological type, FIGO stage, tumor grade, regional lymph node metastasis, residual tumor after cytoreductive surgery, pre-operative serum CA125 level, SUVmax, MTV, and TLG were evaluated as variables in survival analysis. ROC curve analyses were performed for continuous variables, including age, serum CA125 level, SUVmax, MTV, and TLG, to specify cutoff values. The optimal cutoff values for age, serum CA125 level, SUVmax, MTV, and TLG were 55 years, 340 U/mL, 8.0, 25.0 cm3, and 100.0 g, respectively. The significance of prognostic factors on univariateanalysis and 2-year progression-free survival rates according to the variables is shown in Table 2. Among the variables, histopathological type, FIGO stage, presence of regional lymph node metastasis, residual tumor after cytoreductive surgery, serum CA125 level, SUVmax, MTV, and TLG were significant on univariate analysis (p < 0.05) and were selected for multivariate analysis. The cumulative disease progression-free survival curve according to the FIGO stage, SUVmax, MTV, and TLG by the Kaplan-Meier method is shown in Fig. 3. Because TLG is calculated by multiplying the MTV and mean SUV, multi-colinearity between MTV and TLG was evaluated before multivariate analysis. The result of the Spearman’s rank correlation test showed a significant correlation between MTV and TLG (r = 0.920, p < 0.0001), thus MTV and TLG were separately assessed with other variables on multivariate analysis. Because MTV and TLG were calculated in 166 patients, multivariate analysis was performed in those 166 patients (Table 3). On multivariate analysis, only FIGO stage and TLG were statistically significant (p < 0.05).
By combining FIGO stage with TLG, which were statistically significant variables on multivariate analysis, their predictive value could be further enhanced (Table 4). In patients with stage III-IV disease and TLG > 100.0, the disease progression rate was high at 80.0 %, while patients with stage I-II disease and TLG ≤ 100.0 g had a low disease progression rate of 2.3 %. The disease progression-free survival rates for patients with TLG ≤ 100.0 g were significantly higher than those for patients with TLG > 100.0 g in any stage of disease (p = 0.01 for stage I-II and p = 0.009 for stage III-IV; Fig. 4).
Prediction of residual tumor
The patients with residual tumor after cytoreductive surgery had significantly higher values of SUVmax (11.6 ± 3.5 vs. 9.3 ± 5.4), MTV (59.0 ± 55.0 vs. 33.4 ± 52.1), and TLG (459.8 ± 434.8 vs. 243.5 ± 424.3) than the patients with negative residual tumor (p = 0.0002 for SUVmax and p < 0.0001 for MTV and TLG). The incidence of residual tumor after operation according to the SUVmax, MTG, and TLG are shown in Table 5. There were significant differences of incidence rates of residual tumor according to the cutoff values of SUVmax, MTV, and TLG (p < 0.05). Of 45 patients with residual tumor, 88.9 % (40 patients) had TLG > 100.0 g. In patients with MTV > 25.0 cm3or TLG > 100.0 g, 39.2 % had residual tumor after surgery.
Discussion
To the best of our knowledge, this is the largest clinical study to assess the prognostic significance of volumetric parameters derived from 18F-FDG PET/CT in patients with epithelial ovarian cancer after cytoreductive surgery. Our study demonstrated that TLG of whole-body tumor burden on pre-operative 18F-FDG PET/CT is a significant independent prognostic factor, along with FIGO stage, for disease progression of epithelial ovarian cancer after cytoreductive surgery. Incorporation of TLG with FIGO stage can be more accurately prognostic than either TLG or FIGO stage alone.
SUVmax has been widely used as an indicator of metabolic activity for various malignancies. However, SUVmax only represents the highest metabolic activity within the tumor and does not take the tumor extent into account [23, 25]. In contrast, MTV takes into account the metabolic active volume of all tumor lesions, which, in our study, is the sum of voxels over 40 % of SUVmax [25]. Furthermore, TLG considers both the level of tumor glucose utilization and the volume of metabolically active tumor lesions [27]. Hence, a large TLG can reflect a small volume of tumor lesion with high 18F-FDG uptake or a large volume with low 18F-FDG uptake [21]. Because TLG reflects both the metabolic burden and disease extent, it can provide a higher predictive value than SUVmax. The results of our study also showed that TLG was the only independent prognostic factor among SUVmax, MTV and TLG, and had a higher predictive value than SUVmax. However, in nine of the enrolled patients, MTV and TLG could not be measured because of the low tumor-to-background uptake ratios. Although none of these nine patients experienced disease progression or recurrence, it could be considered as a limitation for the clinical use of the volumetric parameters as compared to SUVmax. Further investigation for developing a method of measuring MTV in tumors with low 18F-FDG uptake is needed.
To date, only one other study has investigated the predictive value of volumetric parameters on pre-operative 18F-FDG PET/CT in patients with epithelial ovarian cancer [23]. Chung et al. [23] performed pre-operative 18F-FDG PET/CT in 55 patients with epithelial ovarian cancer before surgical staging. The results of their study demonstrated that higher values of both MTV and TLG were associated with poor clinical outcome, and that MTV and TLG were statistically significant predictors of recurrence, which is similar to the results of our study. However, they showed that MTV was more predictive of recurrence than TLG, in contrast to our study. The difference in results between the two studies may be due to the different methodology of measuring MTV and TLG, and the different clinical characteristics of enrolled patients, especially the higher percentage of patients with advanced-stage disease in their study.
18F-FDG PET/CT is known to be useful for detecting lymph node metastasis and extra-abdominal distant metastasis of epithelial ovarian cancer [13, 16, 28, 29], and, in our study, additional metastatic lesions were found by 18F-FDG PET/CT in 9.7 % of enrolled patients. A recent study showed that 18F-FDG PET/CT was even better than MRI for detecting recurrent small peritoneal implants [30]. Nonetheless, because epithelial ovarian cancer is surgically staged, and also because patients with extra-abdominal lesions on 18F-FDG PET/CT also underwent cytoreductive surgery for a possible survival benefit, similar to patients negative for distant metastatic lesions, the role of pre-operative 18F-FDG PET/CT was not clear [16]. The results of our study suggest that pre-operative 18F-FDG PET/CT in epithelial ovarian cancer can provide information on prognosis after cytoreductive surgery, in addition to its original purpose of detecting metastatic lesions. Nevertheless, FIGO stage had greater predictive value for disease progression and none of the volumetric parameters on 18F-FDG PET/CT could replace FIGO staging as a prognostic factor. However, it should be pointed out that the combination of FIGO stage with TLG can improve the prognostic stratification of patients with epithelial ovarian cancer. Among patients with stage I-II disease, the disease progression rate was high at 22.7 % if TLG on PET/CT was greater than 100.0 g.
The risk of residual cancer after cytoreductive surgery can be predicted by the volumetric parameters on 18F-FDG PET/CT. The presence of residual cancer after a debulking operation has already shown to be a more powerful prognostic determinant than stage in a recent meta-analysis study [31]. According to the results of our study, 39.2 % of patients with high TLG had residual cancer, while less than 10 % of patients with low TLG had residual cancer after surgery. Hence, patients with high TLG can be considered as having high risk of residual cancer and disease progression. In addition to detecting additional metastatic lesions, 18F-FDG PET/CT could give information on the risk of residual cancer after surgery, which has a potential impact on planning treatment modality and performing adjuvant treatment.
In the present study, we measured whole-body metabolic tumor burden in the primary tumor lesion and all metastatic lesions using a threshold of 40 % SUVmax. Most previous studies evaluated MTV based on the tumor volume of the primary lesion only. Recent studies have used MTV as a measure of whole-body metabolic tumor burden and evaluated its prognostic value [20, 23, 32, 33]. Still, there is no consensus on whether whole-body metabolic tumor burden has greater predictive value than primary tumor volume. However, it stands to reason that MTV measuring whole-body metabolic tumor burden would be appropriate for epithelial ovarian cancer because most of these cancers have extensive metastatic lesions in the peritoneum or pelvic cavity at the time of diagnosis and it is often difficult to differentiate the volume of the primary tumor from that of adjacent peritoneal metastatic lesions.
Previous studies evaluating MTV mostly used three methods for defining threshold SUV to delineate metabolic tumor: (1) using a fixed SUV threshold such as 2.5 [19, 34] or 3.0 [20], (2) using a fixed ratio such as 40 % [23, 25, 26] or 50 % [33] of SUVmax as a threshold, or (3) using a threshold SUV of the mediastinal background SUV plus two standard deviations [34, 35]. There is still no established method of defining threshold SUV for clinical use. In the present study, we used a threshold of 40 % of SUVmax to define MTV. Previous studies using a phantom have demonstrated that an SUV of 40-50 % of the maximum was appropriate for contouring the actual tumor volume [25, 26]. In addition, physiologic 18F-FDG uptake of SUV more than 2.5 or 3.0 in normal tissues of the abdomen does not allow the use of a fixed threshold of 2.5 or 3.0. Therefore, further studies comparing various methods for defining the threshold SUV are needed for standardization.
There are several limitations to the present study. First, because it was a single-center study with a retrospective design, selection bias was inherent and the general applicability of our study may therefore be limited. Second, a partial-volume effect may have affected the 18F-FDG in small lesions, especially in small peritoneal lesions, resulting in underestimation of MTV and TLG values. Lastly, because of the small number of enrolled patients, subgroup analysis according to histopathology could not be performed. Although serous, endometrioid, clear cell, and mucinous ovarian carcinomas are lumped together as epithelial ovarian cancers, in reality, they are clinically, morphologically, and molecularly distinct cancers that bear little resemblance to each other [36].
In conclusion, TLG, a volumetric parameter on 18F-FDG PET/CT representing metabolically active tumor burden, was a significant independent prognostic factor for disease progression after cytoreductive surgery in patients with epithelial ovarian cancer, in addition to FIGO stage.18F-FDG PET/CT found additional metastatic lesions in 9.7 % of total patients and also showed additional value for predicting prognosis after surgery. None of the volumetric parameters on 18F-FDG PET/CT could replace FIGO staging as a prognostic factor; however, by combining TLG with stage, prognostic stratification of the patients was further improved. Further multi-center prospective studies with larger cohorts of patients are needed to validate the results of our study.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Heintz AP, Odicino F, Maisonneuve P, Quinn MA, Benedet JL, Creasman WT, et al. Carcinoma of the ovary. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006;95 Suppl 1:S161–92.
Tingulstad S, Skjeldestad FE, Halvorsen TB, Hagen B. Survival and prognostic factors in patients with ovarian cancer. Obstet Gynecol. 2003;101:885–91.
Bachmann C, Bachmann S, Fehm T, Staebler A, Becker S, Rothmund R, et al. Nodal status–its impact on prognosis in advanced ovarian cancer. J Cancer Res Clin Oncol. 2012;138:261–7.
Brun JL, Feyler A, Chene G, Saurel J, Brun G, Hocke C. Long-term results and prognostic factors in patients with epithelial ovarian cancer. Gynecol Oncol. 2000;78:21–7.
Makar AP, Baekelandt M, Trope CG, Kristensen GB. The prognostic significance of residual disease, FIGO substage, tumor histology, and grade in patients with FIGO stage III ovarian cancer. Gynecol Oncol. 1995;56:175–80.
Mury D, Woelber L, Jung S, Eulenburg C, Choschzick M, Witzel I, et al. Prognostic and predictive relevance of CA-125 at primary surgery of ovarian cancer. J Cancer Res Clin Oncol. 2011;137:1131–7.
Winter 3rd WE, Maxwell GL, Tian C, Carlson JW, Ozols RF, Rose PG, et al. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25:3621–7.
Winter 3rd WE, Maxwell GL, Tian C, Sundborg MJ, Rose GS, Rose PG, et al. Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2008;26:83–9.
Hynninen J, Kemppainen J, Lavonius M, Virtanen J, Matomaki J, Oksa S, et al. A prospective comparison of integrated FDG-PET/contrast-enhanced CT and contrast-enhanced CT for pretreatment imaging of advanced epithelial ovarian cancer. Gynecol Oncol. 2013;131:389–94.
Kim C, Chung HH, Oh SW, Kang KW, Chung JK, Lee DS. Differential diagnosis of borderline ovarian tumors from stage I malignant ovarian tumors using FDG PET/CT. Nucl Med Mol Imaging. 2013;47:81–8.
Kitajima K, Suzuki K, Senda M, Kita M, Nakamoto Y, Onishi Y, et al. FDG-PET/CT for diagnosis of primary ovarian cancer. Nucl Med Commun. 2011;32:549–53.
Kitajima K, Ueno Y, Suzuki K, Kita M, Ebina Y, Yamada H, et al. Low-dose non-enhanced CT versus full-dose contrast-enhanced CT in integrated PET/CT scans for diagnosing ovarian cancer recurrence. Eur J Radiol. 2012;81:3557–62.
Martoni AA, Fanti S, Zamagni C, Rosati M, De Iaco P. D’Errico Grigioni A, et al. [18 F] FDG-PET/CT monitoring early identifies advanced ovarian cancer patients who will benefit from prolonged neo-adjuvant chemotherapy. Q J Nucl Med Mol Imaging. 2011;55:81–90.
Risum S, Loft A, Engelholm SA, Hogdall E, Berthelsen AK, Nedergaard L, et al. Positron emission tomography/computed tomography predictors of overall survival in stage IIIC/IV ovarian cancer. Int J Gynecol Cancer. 2012;22:1163–9.
Risum S, Hogdall C, Loft A, Berthelsen AK, Hogdall E, Nedergaard L, et al. Does the use of diagnostic PET/CT cause stage migration in patients with primary advanced ovarian cancer? Gynecol Oncol. 2010;116:395–8.
Nakamura K, Hongo A, Kodama J, Hiramatsu Y. The pretreatment of maximum standardized uptake values (SUVmax) of the primary tumor is predictor for poor prognosis for patients with epithelial ovarian cancer. Acta Med Okayama. 2012;66:53–60.
Kurosaki H, Oriuchi N, Okazaki A, Tamaki T, Uki A, Izuta M, et al. Prognostic value of FDG-PET in patients with ovarian carcinoma following surgical treatment. Ann Nucl Med. 2006;20:171–4.
Hyun SH, Ahn HK, Kim H, Ahn MJ, Park K, Ahn YC, et al. Volume-based assessment by F-FDG PET/CT predicts survival in patients with stage III non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2014;41:50–8.
Oh JR, Seo JH, Chong A, Min JJ, Song HC, Kim YC, et al. Whole-body metabolic tumour volume of 18 F-FDG PET/CT improves the prediction of prognosis in small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39:925–35.
Ryu IS, Kim JS, Roh JL, Lee JH, Cho KJ, Choi SH, et al. Prognostic value of preoperative metabolic tumor volume and total lesion glycolysis measured by 18 F-FDG PET/CT in salivary gland carcinomas. J Nucl Med. 2013;54:1032–8.
Yoo J, Choi JY, Moon SH, Bae DS, Park SB, Choe YS, et al. Prognostic significance of volume-based metabolic parameters in uterine cervical cancer determined using 18 F-fluorodeoxyglucose positron emission tomography. Int J Gynecol Cancer. 2012;22:1226–33.
Chung HH, Kwon HW, Kang KW, Park NH, Song YS, Chung JK, et al. Prognostic value of preoperative metabolic tumor volume and total lesion glycolysis in patients with epithelial ovarian cancer. Ann Surg Oncol. 2012;19:1966–72.
Liao S, Lan X, Cao G, Yuan H, Zhang Y. Prognostic Predictive Value of Total Lesion Glycolysis From 18 F-FDG PET/CT in Post-Surgical Patients With Epithelial Ovarian Cancer. Clin Nucl Med. 2013;38:715–20.
Fonti R, Larobina M, Del Vecchio S, De Luca S, Fabbricini R, Catalano L, et al. Metabolic tumor volume assessed by 18 F-FDG PET/CT for the prediction of outcome in patients with multiple myeloma. J Nucl Med. 2012;53:1829–35.
Uto F, Shiba E, Onoue S, Yoshimura H, Takada M, Tsuji Y, et al. Phantom study on radiotherapy planning using PET/CT–delineation of GTV by evaluating SUV. J Radiat Res. 2010;51:157–64.
Lim R, Eaton A, Lee NY, Setton J, Ohri N, Rao S, et al. 18 F-FDG PET/CT metabolic tumor volume and total lesion glycolysis predict outcome in oropharyngeal squamous cell carcinoma. J Nucl Med. 2012;53:1506–13.
Kitajima K, Murakami K, Yamasaki E, Kaji Y, Fukasawa I, Inaba N, et al. Diagnostic accuracy of integrated FDG-PET/contrast-enhanced CT in staging ovarian cancer: comparison with enhanced CT. Eur J Nucl Med Mol Imaging. 2008;35:1912–20.
Castellucci P, Perrone AM, Picchio M, Ghi T, Farsad M, Nanni C, et al. Diagnostic accuracy of 18 F-FDG PET/CT in characterizing ovarian lesions and staging ovarian cancer: correlation with transvaginal ultrasonography, computed tomography, and histology. Nucl Med Commun. 2007;28:589–95.
Sanli Y, Turkmen C, Bakir B, Iyibozkurt C, Ozel S, Has D, et al. Diagnostic value of PET/CT is similar to that of conventional MRI and even better for detecting small peritoneal implants in patients with recurrent ovarian cancer. Nucl Med Commun. 2012;33:509–15.
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115:1234–44.
Zhang H, Wroblewski K, Liao S, Kampalath R, Penney BC, Zhang Y, et al. Prognostic value of metabolic tumor burden from (18) F-FDG PET in surgical patients with non-small-cell lung cancer. Acad Radiol. 2013;20:32–40.
Yoon HJ, Paeng JC, Kwak C, Park YH, Kim TM, Lee SH, et al. Prognostic implication of extrarenal metabolic tumor burden in advanced renal cell carcinoma treated with targeted therapy after nephrectomy. Ann Nucl Med. 2013;27:748–55.
Lee SJ, Choi JY, Lee HJ, Baek CH, Son YI, Hyun SH, et al. Prognostic value of volume-based (18) F-fluorodeoxyglucose PET/CT parameters in patients with clinically node-negative oral tongue squamous cell carcinoma. Korean J Radiol. 2012;13:752–9.
Hyun SH, Choi JY, Kim K, Kim J, Shim YM, Um SW, et al. Volume-based parameters of (18) F-fluorodeoxyglucose positron emission tomography/computed tomography improve outcome prediction in early-stage non-small cell lung cancer after surgical resection. Ann Surg. 2013;257:364–70.
Prat J. Ovarian carcinomas: five distinct diseases with different origins, genetic alterations, and clinicopathological features. Virchows Arch. 2012;460:237–49.
Acknowledgments
This study was supported by a National Research Foundation of Korea Grant funded by the Korean Government (NRF-2011–013-E00038, No. 2012027176) and the National R&D Program for Cancer Control, Ministry of Health & Welfare (1320210).
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lee, J.W., Cho, A., Lee, JH. et al. The role of metabolic tumor volume and total lesion glycolysis on 18F-FDG PET/CT in the prognosis of epithelial ovarian cancer. Eur J Nucl Med Mol Imaging 41, 1898–1906 (2014). https://doi.org/10.1007/s00259-014-2803-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2803-x